Professional Documents
Culture Documents
2009-07-24 Musculoskeletal Simulation Webinar
Uploaded by
Mounesh7Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2009-07-24 Musculoskeletal Simulation Webinar
Uploaded by
Mounesh7Copyright:
Available Formats
1
Musculoskeletal Webinar
Musculoskeletal Simulation Webinar
David Wagner, PhD
Ozen Engineering
July 24, 2009
Please visit:
http://www.ozeninc.com/default.asp?ii=273
for upcoming webinars
Welcome to the Webinar
Welcome to the Webinar. Please make sure
your audio is working
Feel free to use
computer speakers
or telephone
Type any questions
you have here
2
Summary
Coupling musculoskeletal modeling and finite element analysis
Extracting and incorporating 3D geometry and material properties
from tomographic medical image data
A Proposed workflow for incorporating musculoskeletal modeling
Modeling the human body Musculoskeletal simulation of activities
of daily living
Prevalent uses of simulation in the orthopedic industry
Uses of Simulation in the Orthopedic Industry
Replicating Physical Test Research (Internal/University)
Kim et al. 2008,
SBC2008-193023
Li et al. 2008, SBC2008-192776
Design of Orthopedic Devices and Prosthetics
ASME Summer Bioengineering Conference (2008)
Finding out what went wrong
Finite-element
analysis of
failure of the
Capital Hip
designs
Janssen et al.
2005
3
Benets of Simulation
The use of computational simulation can be beneficial if it:
accurately represents and replicates the physics of the system
increases the number of possible design iterations (within a fixed
time)
decreases the cost associated with each design iteration
improves the fidelity of analysis as related to making design
decisions
is integrated in the design process
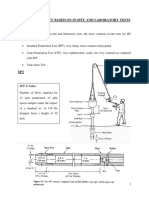
Replicating Standardized Physical Tests
For example
ASTM F384 -06 Standard Specifications and Test Methods for Metallic Angled Orthopedic
Fracture Fixation Devices (no associated ISO standard)
Methods for bending fatigue testing
Fatigue life over a range of maximum bending moment levels
Estimate the fatigue strength for a specified number of fatigue cycles
Not intended to define levels of performance of case-specific
ASTM F1264 Standard Specification and Test Methods for Intramedullary Fixation Devices
performance definitions
test methods and characteristics determined to be important to in-vivo performance
of the device (bending fatigue test, static torsion test, static four-point bend test)
It is not the intention of this specification to define levels of performance or case-
specific clinical performance of these devices, as insufficient knowledge to predict
the consequences of the use of any of these devices in individual patients for
specific activities of daily living is available
4
From Kojic 2008
Comparison of Fracture Fixation Devices
Fixed Plate
Internal compression
resulting from screw +
fixation plate geometry
Intramedullary nail
Bending stiffness:
K
b
= ExI
E, Youngs Modulus of Elasticity
I, the second moment of inertia
for bending of the nail cross
section
Torsional stiffness:
K
t
= ExI
t
G, Shear Modulus
I
t
, the second moment of inertia
for torsion
From Kojic 2008
Example Analysis - Fixed Plate Boundary Conditions
Fixed
Constraint
~ approximating
of axial load
during human
walking (single
stance phase of
70 kg
individual)
5
From Kojic 2008
Example Analysis Results - Effective Stresses
No slip
condition
modeled
between
screws, plate,
and bone =>
i.e. bonded
contacts
MPa
From Kojic 2008
Example Analysis Results - Fixed Plate Stresses
Stainless steel
used for plate
and screws
E = 2.1x10
5
Mpa
Poissons ratio = 0.3
Maximum effective stress
less than critical values for
stainless steel. However,
cyclic loading leading to
material fatigue must also
be considered
6
From Kojic 2008
Example Analysis - Intramedullary Nail
Same bone geometry,
material properties, and
boundary conditions as in
the neutralization plate
analysis
From Kojic 2008
Example Analysis - Intramedullary Nail Stresses
Effective stress concentrations in the nail near the screw regions => However, stress values
are significantly lower than the corresponding neutralization plate regions (~80 MPa).
Implication is that risk of intramedullary nail failure is significantly lower when compared to
neutralization plate.
7
From Kojic 2008
Example Analysis - Intracapsular Fractures
Parallel Screws Dynamic Hip Implant
Comparison of implant designs for internal fixation of intracapsular fractures of the
femoral neck
From Kojic 2008
Example Analysis - Parallel Screws BCs
Positive correlation
between
intraoperative
stability and
femoral neck
fractures that have
healed (versus did
not heal),
Rehnberg et al.
1989
Fixed Boundary
Condition
F
R
: Pelvis to femur head reaction force, 199 daN
F
A
: Force generated by gluteal muscles, 137 daN
Body weight: 70 daN
8
Can we use
simulation in a
more pro-active
way to develop
better products?
Doing More with Simulation (one idea)
Summary
Coupling musculoskeletal modeling and finite element analysis
Extracting and incorporating 3D geometry and material properties
from tomographic medical image data
A Proposed workflow for incorporating musculoskeletal modeling
Modeling the human body Musculoskeletal simulation of activities
of daily living
Prevalent uses of simulation in the orthopedic industry
9
Help understand what is going on inside the human body
We use simulation for many other engineering analyses,
why not for the human body as well
Design/redesign safe working environments
Teaching
Functional assessments (neuromusculoskeletal system)
Create/Mimic realistic movement
Sometimes the only way to understand and learn more
about complex systems (like people!)
Simulation for !Biomechanics" - Why?
Musculoskeletal Analysis
AnyBody
LifeMod
Opensim/SIMM/SimTK
Madymo (TNO)
ESI Group
Marlbrook
Motek
Digital Manikins
RAMSIS (Human
Solutions)
Jack (UGS/Siemens)
HumanBuilder/Delmia
(Dassault)
HumanCAD (NexGen)
SANTOS (U. Iowa)
Some others
Motion Capture
BodyBuilder (Vicon)
Simi
Qualisys
SIMM (Motion Analysis)
XSENS
Many others
CAE tools (FE/CAD)
ANSYS
LS-DYNA (ANSYS)
Abacus (Dassault)
AutoCAD (AutoDesk)
NASTRAN & ADAMS (MSC)
COMSOL
Other tools
Matlab (Mathworks)
Mathematica
Simulation Software for !Biomechanics"
10
The Holy Grail
Task + Environment + Population
Unique
Simulation
from Parkinson and Reed (2008)
Working Within the Connes of the Current Technology
Library of activities
Cant rely (yet) on the musculoskeletal models to adapt to new
task/environment conditions => particularly for novel (~non-cyclic)
tasks
Global Assessments vs. Better Products/Designs
Models that match measured results are great, but models that
exhibit realistic trends may be sufficient (and as useful)
Better incorporation/understanding of variability
E.g. Within subject variability as indicator of model performance
Will we ever be able to use Musculoskeletal Simulation
without a corresponding validation study
Cant ALWAYS be expected to conduct a validation study for a new activity
Must have confidence in the tools (e.g. Finite Element Models)
11
Expanding the Use of Activities of Daily Living with a
Library of Musculoskeletal Simulations
Long-term stability of hip-
implants have been
evaluated using normal
walking, sit to stand, stair
climbing, and combinations
of those activities.
Traditionally used as
pass/fail tests to identify
whether a particular design
performs to a set of
minimum specifications
Significantly Underutilized
Musculoskeletal Models Used Here
80
14.6
35
5.2
549
121
709
782
804
17
121
121
(b)
Popular class of musculoskeletal
models based on rigid body
dynamics:
Bones and objects from the
environment are rigid
Muscles and ligaments are
mass-less actuators
Soft tissue wobbly
masses are not taken into
account (mass is
concentrated in bones)
Phenomenological muscle
models
Easily scalable
Suited for simulating internal body forces (muscle,
joint, ligament) for prescribed activities
Static 2D
Dynamic 3D (AnyBody
Modeling System)
12
} ,.., 1 { , 0
] , [ where ,
) ( ) (
) ( ) (
M M
i
n i f ! "
= =
M R
f f f d Cf
Muscle
forces
Joint
reactions
Internal
forces
Applied
forces
The matrix C is rectangular. This means that there are
infinitely many solutions to the system of equations.
How to pick the right one?
Formulating Dynamic Equilibrium
Using Optimization to Get a Solution
!
Minimize
G(f
(M)
)
Subject to
Cf = d
f
i
(M )
" 0, i #{1,.., n
(M )
}
Objective function. Different
choices give different muscle
recruitment patterns.
What should be used for ?
!
G(f
(M)
)
13
Musculoskeletal Models for Commercial Use
No gold-standard, just like with other pieces of engineering
software
Commercially available (including open source) software
packages demand a knowledgeable user
Not traditionally incorporated in current design/engineering
methodologies
Always room for improvement (I.e. improved validation, better
accuracy, scaling to populations or patient specific, etc.)
Still must demonstrate where/how this arena of modeling can
improve specific processes (I.e. $$$)
Summary
Coupling musculoskeletal modeling and finite element analysis
Extracting and incorporating 3D geometry and material properties
from tomographic medical image data
A Proposed workflow for incorporating musculoskeletal modeling
Modeling the human body Musculoskeletal simulation of activities
of daily living
Prevalent uses of simulation in the orthopedic industry
14
Bridging the Gap with Simulation
Physical Testing
Simulated
Physical Testing
Simulated In-
Vivo Performance
All the necessary pieces:
Geometry
Mesh
Material Properties
Boundary Conditions
Solve
Post-Processing
Setting up an FE Simulation Using Boundary Conditions Derived from a
Musculoskeletal Model
15
Selected Arenas of Simulation (by Device)
The use of computational simulation can be beneficial if it:
accurately represents and replicates the physics of the system
increases the number of possible design iterations (within a fixed
time)
decreases the cost associated with each design iteration
improves the fidelity of analysis as related to making design
decisions
Starting with Geometry
16
Incorporating Musculoskeletal Modeling
Implant Evaluation
17
Implant Optimization
Associated Software
18
Summary
Coupling musculoskeletal modeling and finite element analysis
Extracting and incorporating 3D geometry and material properties
from tomographic medical image data
A Proposed workflow for incorporating musculoskeletal modeling
Modeling the human body Musculoskeletal simulation of activities
of daily living
Prevalent uses of simulation in the orthopedic industry
Geometry, Mesh, and Material Properties
Realistic geometries and material properties are practical ways to
improve the accuracy of the simulations
A NIH (National Institute of
Health) Project
Goal is anatomically detailed,
3D representation of the
human body
CT, MRI, Cryosection taken of
cadavers
Male specimen released 1994
Female specimen in 1995
Publicly available with an
application to National Library
of Medicine
CT
MRI
Cryosection
19
Tool for working with segmented
medical data
Provides a GUI environment to
apply various segmentation
methods
Creates and exports advanced 3D
geometries
Can be used to export Finite
Element Mesh (if desired)
Can be used to dene iso-tropic
material denitions from apparent
density relationships
Using Medical Data as Simulation Input
Deriving Material Properties From Scan Data
In Ansys, the mesh can be changed by a number of
operations, such as applying different boundary conditions or
for purposes of convergence
Deferring the material property assignment until the simulation
is fully set up ensures versatility
Bonemat is a public domain program originally written by
Cinzia Zannoni et al. at The Rizzoli Institute*
Uses a voxel data integration algorithm to determine material
properties for nte elements regardless of relative voxel size
*Zannoni C, Mantovani R, Viceconti M. Material properties
assignment to nite element models of bone structures: a new
method. Med Eng Phys 1998;20(10):73540.
20
Bonemat Workow
Bonemat takes 2 inputs:
A mesh in patran neutral le format (*.ntr)
Volumetric CT data in a vtk le format(rectilinear grid or point cloud)
Bonemat outputs:
An identical patran neutral mesh le with material properties assigned
An informational frequency le on material property distribution
Solution
Geometry Mimics
Commercially available software packages with
tomographic reconstruction capabilities
(Mimics, Analyze, Osiris) can also be used to
define material properties (isotropic) suitable for
FEA => using Hounsfield Units relationships
The material property of each
tetrahedral element was defined
using a procedure similar to that
used by Peng et al. (2006).
HU =
HU are normalized units associated with CT image
scans
- based on the linear attenuation coefficient ()
- based on scale -1000 (air) : + 1000 (bone), 0 (water)
Material properties from imaging data
21
Material properties from imaging data
The Hounsfield Units (HU) of each voxel in the CT scan indicates the radiodensity of the
material, distinguishing the different bone tissue types. There exist an approximate linear
relationship between apparent bone density and HU (Rho et al. 1995).
The maximum HU of the CT
scan, 1575, was defined to be
the hardest cortical bone of
density (2000 kg/m
3
) and the
HU value of 100 was defined to
be the minimum density of
cortical bone (100 kg/m
3
).
Density
100 kg/m
3
2000 kg/m
3
Material properties from imaging data
Elements were assigned elastic
moduli calculated from apparent
densities using axial loading
equations developed by Lotz et al.
(1991):
There exist an approximate power relationship between bone material properties and apparent
densities (Wirtz et al. 2000).
Elastic Moduli
A Poisson's ratio of 0.30 was
used for all materials.
HU >= 801, cortical bone (E = 2065!
3.09
MPa)
HU <= 800, cancellous bone (E = 1904!
1.64
MPa)
HU < 100, intramedullar tissue (E = 20 MPa)
22
Summary
Coupling musculoskeletal modeling and finite element analysis
Extracting and incorporating 3D geometry and material properties
from tomographic medical image data
A Proposed workflow for incorporating musculoskeletal modeling
Modeling the human body Musculoskeletal simulation of activities
of daily living
Prevalent uses of simulation in the orthopedic industry
All the necessary pieces:
Geometry
Mesh
Material Properties
Boundary Conditions
Solve
Post-Processing
Setting up the FE Simulation
23
Cycling Data
Cyclist Data
24
Musculoskeletal Simulation
Single Revolution
Observed Cadence of 62 rpm
5 points of support (pelvis, feet,
hands)
Anthropometry Matched to
Subject
Simulated Crank Torque =>
MechOutput = 170 (avg.
mechanical output over a
cycle in Watts)
Musculoskeletal Simulation
Force and Moment ! Free Body Diagram"
1 revolution = 0.97 seconds
Cut Plane (vector
lengths correspond to
force magnitudes)
25
Muscle Force Boundary Conditions at a Single Time Step
FE Model in Dynamic Equilibrium
- Matched mass and inertia
properties between rigid and
flexible body simulations
- Matched points of force
application
- No arbitrary constraints (i.e.
nodal position fixed in space)
- Inertia loads applied
- Model supported by weak springs
(~1e-3 Newtons), to prevent rigid
body motion
- Assumption of small deflections
26
Tested Fracture Fixation Plate (Distal Femur)
Geometry with 3 plate
thicknesses
3.25mm
4.0mm
4.75mm
Fatigue Life Results
Fatigue Life Minimum Cycles:
3.25 mm => 178,000 cycles
4.0 mm => 335,000 cycles
4.75 mm => 14.7 million cycles
Plots are depicted at
97% of cycle (t = 0.9704)
4.75 mm
3.25 mm
4.00 mm
Stress Life
Fully Reversed
t= 0.9409
Stress Life
Fully Reversed
t= 0.9409
Stress Life
Fully Reversed
t= 0.9409
27
Stress Contour Plots
Maximum Stress:
3.25 mm => 855 MPa
4.0 mm => 692 MPa
4.75 mm => 584 MPa
Plots are depicted at
97% of cycle (t = 0.9704)
4.75 mm
3.25 mm
4.00 mm
Yield Stress of Titanium Alloy => 930 MPa
Deformation Mode
Deformation from musculoskeletal forces @ 0.02 s, 18x scale
28
Equivalent Stresses for Three Plate Thicknesses
3.25mm
4.00mm
4.75mm
Summary of Simulation Capabilities
1. Replicating physical tests using
simulation
2. Compare performance of new
implant design to current on the
market device
3. Replicate implant failure
conditions associated
with clinical and/or case-specific
performance criteria
4. Evaluate implant performance
criteria (i.e. total deformation,
maximum stress, maximum
strain, and/or fatigue life)
for physiologically realistic
boundary conditions associated
with a single or library of
activities of daily living
29
Summary of Simulation Capabilities
5. Evaluate implant performance criteria
(i.e. total deformation, maximum
stress, maximum strain, and/or fatigue
life) for different populations (i.e. bone
size/geometry, bone quality/strength)
performing relevant activities of daily
living
6. Perform shape optimization of
parametrically defined implant to
maximize or satisfy
one/multiple performance objectives or
criteria
7. Perform sensitivity analysis on screw
placement and/or implant variations
with respect to performance criteria
8. Evaluate internal bone stresses
at/around implant-bone and bone-
bone interfaces for laboratory and
activity of daily living criteria
Thank you for your attention
Thank You For Your Attention
lor furLher lnformauon, please conLacL:
CZLn LnClnLL8lnC, lnC.
1210 L. A8CuLS AvL. Sul1L: 207
Sunn?vALL, CA 94083
(408) 732-4663
lnfo[ozenlnc.com
www.ozenlnc.com
lease leL us know lf you have any quesuons on speclc Loplcs presenLed here
(musculoskeleLal[ozenlnc.com)
Weblnars relaLed Lo musculoskeleLal slmulauon every monLh
(hup://www.ozenlnc.com/defaulL.asp?ll=273)
Cur 8uslness:
Collaborauon (l.e. granLs, Lralnlng)
Consulung
Soware
Some 8ecenL news (!uly 23, 2009)
hup://www.clemson.edu/newsroom/arucles/2009/[uly/Czen_gl_res.php3
30
You might also like
- LM50 23B12R2Document5 pagesLM50 23B12R2Mounesh7No ratings yet
- Kitab Ul-AquaidDocument32 pagesKitab Ul-AquaidMounesh7No ratings yet
- Updated On Board Team LoginDocument20 pagesUpdated On Board Team LoginMounesh7No ratings yet
- PLM - Indishtech PVT Ltd-Corporate ProfileDocument16 pagesPLM - Indishtech PVT Ltd-Corporate ProfileMounesh7No ratings yet
- Hayat e AlaHazratDocument138 pagesHayat e AlaHazratMounesh7No ratings yet
- The Real Reasons You Procrastinate PDFDocument15 pagesThe Real Reasons You Procrastinate PDFMounesh7No ratings yet
- M Tech Design EngineeringDocument22 pagesM Tech Design EngineeringMounesh7No ratings yet
- Madina Book1 Arabic TextDocument120 pagesMadina Book1 Arabic TextTewhid-islamNo ratings yet
- 1150 1Document58 pages1150 1Mounesh7No ratings yet
- Product Design 01Document6 pagesProduct Design 01Mounesh7No ratings yet
- Product Design 01Document6 pagesProduct Design 01Mounesh7No ratings yet
- Product Design 01Document6 pagesProduct Design 01Mounesh7No ratings yet
- HIFZDocument3 pagesHIFZMounesh7No ratings yet
- Gear Tooth DesignDocument18 pagesGear Tooth DesignMounesh7100% (1)
- Learn UrduDocument56 pagesLearn UrduSunilkumar Dubey86% (7)
- DisDocument1 pageDisMounesh7No ratings yet
- Learn UrduDocument56 pagesLearn UrduSunilkumar Dubey86% (7)
- Learn Urdu and English at HomeDocument39 pagesLearn Urdu and English at Homeapi-27152512100% (2)
- Urdu Ka Muallim Level1Document55 pagesUrdu Ka Muallim Level1Mounesh7No ratings yet
- LoadDocument1 pageLoadMounesh7No ratings yet
- ZakathDocument1 pageZakathMounesh7No ratings yet
- ThesisDocument1 pageThesisMounesh7No ratings yet
- Seven Qirats of The QurDocument11 pagesSeven Qirats of The Qurslavequadir1No ratings yet
- Book of SarfDocument263 pagesBook of SarfNasrin AktherNo ratings yet
- UrduDocument1 pageUrduMounesh7No ratings yet
- Models NewDocument2 pagesModels NewMounesh7No ratings yet
- Ishariya Fatwa Razviya Nusra Thul Haq, Rahmathe Kuha VandiDocument1 pageIshariya Fatwa Razviya Nusra Thul Haq, Rahmathe Kuha VandiMounesh7No ratings yet
- Kufic: Nabataean ScriptDocument11 pagesKufic: Nabataean ScriptMounesh7No ratings yet
- Urdu Ka Muallim Level1Document55 pagesUrdu Ka Muallim Level1Mounesh7No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 6 4rate of Plate MovementDocument5 pages6 4rate of Plate Movementapi-245872444No ratings yet
- Identifying VariablesDocument25 pagesIdentifying Variablesapi-236248022No ratings yet
- 15IPST024Document217 pages15IPST024Roland BagiNo ratings yet
- Gears and How Their World Is ChangingDocument69 pagesGears and How Their World Is Changingjohn doeNo ratings yet
- AP 101 SyllabusDocument3 pagesAP 101 SyllabusTamandeep SinghNo ratings yet
- Beginner Ansys TutorialDocument114 pagesBeginner Ansys TutorialNGUYEN92% (12)
- Product Safety Commission (Afps) : Management: Federal Institute For Occupational Safety and HealthDocument12 pagesProduct Safety Commission (Afps) : Management: Federal Institute For Occupational Safety and HealthFabricio AmorimNo ratings yet
- Determination of The Electron Specific MassDocument2 pagesDetermination of The Electron Specific MassAdina BlazeNo ratings yet
- Nonlinear AnalysisDocument8 pagesNonlinear Analysisstrawberry8320No ratings yet
- Trig EssayDocument4 pagesTrig Essayapi-265366548No ratings yet
- Investigating The Effect of Light Intensity On The Rate of PhotosynthesisDocument2 pagesInvestigating The Effect of Light Intensity On The Rate of PhotosynthesisIzwahaneIbrahim83% (12)
- Separation of Plant Pigments by Paper Chromatography PDFDocument3 pagesSeparation of Plant Pigments by Paper Chromatography PDFJade EncarnacionNo ratings yet
- Awdaw Aw Da Wda WDDocument6 pagesAwdaw Aw Da Wda WDebrown7No ratings yet
- Galata CFA Properties GuideDocument12 pagesGalata CFA Properties GuideToniHospitalerNo ratings yet
- Problems and Solutions To The MIChO Selection Camp 2015: Third PhaseDocument38 pagesProblems and Solutions To The MIChO Selection Camp 2015: Third PhaseYau Ching Koon100% (1)
- API GravityDocument1 pageAPI Gravityscribd_thakurNo ratings yet
- MTM Metro Expt1 ManualDocument10 pagesMTM Metro Expt1 ManualBhargav DindukurthiNo ratings yet
- Gypsum Moisture LossDocument3 pagesGypsum Moisture LossbyronvaughanNo ratings yet
- Determination of Synthesis Route of 1 - 3 4-Methylenedioxyphenyl - 2-Propanone Mdp-2-p Based On Impurity Profiles of MdmaDocument12 pagesDetermination of Synthesis Route of 1 - 3 4-Methylenedioxyphenyl - 2-Propanone Mdp-2-p Based On Impurity Profiles of Mdmagluebom69No ratings yet
- CP504Lecture - 06 - OK (Enzyme Reactor Design)Document12 pagesCP504Lecture - 06 - OK (Enzyme Reactor Design)Yurri Hutami ZarraNo ratings yet
- Molecular Energy Levels NotesDocument5 pagesMolecular Energy Levels Notesskrim2No ratings yet
- Heat Transfer Excel Calculations 1Document39 pagesHeat Transfer Excel Calculations 1Sharon LambertNo ratings yet
- Design of Concrete Airport PavementDocument64 pagesDesign of Concrete Airport Pavementaeroalan100% (4)
- Sediment Transport in Mountain Rivers: Christophe Ancey, Patricio Bohorquez, and Eric BardouDocument16 pagesSediment Transport in Mountain Rivers: Christophe Ancey, Patricio Bohorquez, and Eric BardouomeaveNo ratings yet
- 02 Mirski Czudak-Fem Used For Strength-Related Calculations of Adhesive Joints in The Making of Rail Vehicles PDFDocument9 pages02 Mirski Czudak-Fem Used For Strength-Related Calculations of Adhesive Joints in The Making of Rail Vehicles PDFAbhey DograNo ratings yet
- HeyWhatsThat Path ProfilerDocument2 pagesHeyWhatsThat Path ProfilerCharles VolkoffNo ratings yet
- Benzil SynthesisDocument2 pagesBenzil SynthesisVineeth GopalNo ratings yet
- Bearing Capacity From Other Methods-KFCDocument14 pagesBearing Capacity From Other Methods-KFCmazharNo ratings yet