Professional Documents
Culture Documents
J Infect Dis. 2002 Scheld S225 33
Uploaded by
Afiqah So Jasmi0 ratings0% found this document useful (0 votes)
21 views9 pagesinfection
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentinfection
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
21 views9 pagesJ Infect Dis. 2002 Scheld S225 33
Uploaded by
Afiqah So Jasmiinfection
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 9
S225
Pathophysiology of Bacterial Meningitis: Mechanism(s) of Neuronal Injury
W. Michael Scheld,
1,2
Uwe Koedel,
4
Barnett Nathan,
3
and Hans-Walter Pster
4
Division of Infectious Diseases, Departments of
1
Internal Medicine,
2
Neurosurgery, and
3
Neurology, University of Virginia School
of Medicine, Charlottesville;
4
Department of Neurology,
Ludwig Maximilians University, Munich, Germany
No bacterial disease has undergone a more dramatic change in epidemiology during the
past decade than acute bacterial meningitis. This review describes the changing epidemiology
and considers some important recent observations that contribute to our understanding of
the pathogenesis and pathophysiology of meningitis. The major focus is on the mechanisms
of neuronal injury and the pathophysiologic concepts responsible for death and neurologic
sequelae. In recent years, experimental studies have amplied our understanding of the sub-
stantial body of evidence that now implicates cytokines and chemokines, proteolytic enzymes,
and oxidants in the inammatory cascade leading to tissue destruction in bacterial meningitis.
The molecular mechanisms responsible for oxidant-induced neuronal injury in meningitis are
explored in some depth. Genetic targeting and/or pharmacologic blockade of the implicated
pathways may be a future strategy for therapeutic adjunctive measures to improve outcome
and may hold substantial promise, in concert with antimicrobial agents, in humans with acute
bacterial meningitis.
From the rst description of meningococcemia and menin-
gococcal meningitis, before identication of the etiologic or-
ganism (by Vieusseux in 1806) until the early twentieth century,
bacterial meningitis was considered a nearly uniformly fatal
disease, although some patients with meningococcal meningitis
survived without antimicrobial therapy. The advent of various
experimental procedures followed by antisera therapy directed
against meningococci reduced mortality rates during World
War I, but the introduction of sulfonamides and penicillins
along with other antimicrobial agents heralded the reduction
in morbidity and survival possible with modern antimicrobial
therapy. Despite these achievements and the introduction of
several new antimicrobial agents with in vitro activity against
the major meningeal pathogens plus some limited improvement
in diagnostic assays, bacterial meningitis remains associated
with unacceptably high morbidity and mortality [1].
Endemic meningitis is relatively unusual in developed coun-
tries although epidemic meningitis occurs with considerable fre-
quency in resource-limited settings. Explosive epidemics of me-
ningococcal meningitis have continued to affect the so-called
meningitis belt of sub-Saharan Africa. The most recent epi-
demic, which began in 1996, has resulted in over 300,000 cases
and 30,000 deaths [2]. At present, exclusive of epidemics, about
1.2 million cases of bacterial meningitis are estimated to occur
annually worldwide with 135,000 deaths [3]. Bacterial menin-
gitis is now a top 10 infectious cause of death worldwide,
Reprints or correspondence: Dr. W. Michael Scheld, University of Virginia
Health System, Dept. of Medicine, Division of Infectious Diseases, PO Box
801342, Charlottesville, VA 22908 (wms@virginia.edu).
The Journal of Infectious Diseases 2002; 186(Suppl 2):S22533
2002 by the Infectious Diseases Society of America. All rights reserved.
0022-1899/2002/18611S-0015$15.00
and about half the survivors have neurologic and other sequelae
of the disease [4].
Over the past four decades, clinical and neuropathologic
studies have documented the clear association betweenbacterial
meningitis and brain edema formation, impairments of cere-
brospinal uid (CSF) hydrodynamics, increased intracranial
pressure, seizure activity, arterial and venous cerebral vascular
insults (that may relate to death), and other neurologic sequelae.
Therefore, during the past 1520 years, emphasis has been on
a greater understanding of the pathogenesis and pathophy-
siology of bacterial meningitis in an attempt to improve out-
come [5].
It is apparent that the host immune response is incapable of
controlling infection within the central nervous system (CNS),
particularly the CSF within the subarachnoid space, and that
this host inammatory response may be responsible for many
adverse events during bacterial meningitis [6, 7]. Avery complex
and integrated series of events involving host cytokines, che-
mokines, proteolytic enzymes, and oxidants appears to be re-
sponsible for meningitis-induced brain dysfunction. This has
resulted in the search for adjunctive therapies for bacterial men-
ingitis, including corticosteroids.
In this brief review, we highlight recent epidemiologic trends
in bacterial meningitis worldwide and consider the current con-
cepts of the pathogenesis and pathophysiology of this syndrome
with an emphasis on the identication of promising targets for
adjunctive therapy. Some of these concepts have been reviewed
recently [810]. The pathogenesis of bacterial meningitis, in-
cluding colonization of the nasopharynx by the pathogen, mi-
crobial invasion into the intravascular space and survival within
the bloodstream, microbial entry mechanisms into the CNS,
survival within the subarachnoid space, and host and/or en-
b
y
g
u
e
s
t
o
n
S
e
p
t
e
m
b
e
r
6
,
2
0
1
4
h
t
t
p
:
/
/
j
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
S226 Scheld et al. JID 2002;186 (Suppl 2)
vironmental factors contributing to susceptibility to invasive
disease are reviewed more extensively elsewhere [8].
Changing Epidemiology of Acute Bacterial Meningitis
No bacterial infection worldwide has undergone a more spec-
tacular evolution in epidemiology than acute meningitis since
1990. The introduction of Haemophilus inuenzae conjugate
vaccines (Hib) in the United States and western Europe has
resulted in a decline in the incidence of invasive H. inuenzae
infections by 90% [1]. As a result, Streptococcus pneumoniae
and Neisseria meningitidis are the major causes of bacterial
meningitis in these regions. Furthermore, a dramatic change in
the epidemiology has resulted from these achievements such
that the median age of onset of acute bacterial meningitis has
increased from age 9 months to age 25 years in the United
States [1]. Similarly, the availability of conjugate pneumococcal
vaccines has led to the near total elimination of invasive pneu-
mococcal disease, including bacteremia and meningitis, in
young children in regions adopting this approach. Nevertheless,
most countries in developing regions have not added the Hib
vaccine to the standard vaccine repertoire offered to children,
because of cost. As a result, an estimated 350,000700,000 chil-
dren worldwide still die of invasive Hib disease each year.
In 1999, the Global Alliance for Vaccines and Immunization
(GAVI) was formed with the mission to ensure adequate vac-
cination of every child worldwide against preventable diseases.
Within 18 months of its inception, GAVI committed more than
$600 million to the vaccine fund in 36 developing countries
over 5 years to foster deployment of vaccines such as Hib in
susceptible populations (http://www.vaccinealliance.org). While
the ultimate effect of pneumococcal conjugate vaccines on the
epidemiology of bacterial meningitis is not known, it is hoped
that uniform vaccination, such as recently introduced into the
United States, will nearly totally eliminate this form of men-
ingitis, which is associated with the highest mortality and mor-
bidity rates. Again, cost will be an issue in resource-limited
settings.
According to criteria set forth in the 1992 Institute of Med-
icine report on emerging infectious diseases, meningococcal
meningitis and meningococcemia are emerging infectious dis-
eases [11]. The interdependence of the worldwide community
and travel have enabled the spread of meningococcal strains
from the Indian subcontinent to Saudi Arabia during the Haj
to the sub-Saharan African meningitis belt and the onset of
explosive epidemics. Clusters of meningococcal disease have
also been reported from multiple regions in recent years [12,
13]. Clusters are dened as two or more clinical or conrmed
cases of meningococcal disease arising within 12 months in the
same dened settinghousehold, nursery/playground, primary
school, secondary school, university or college [11, 13]. This
phenomenon has been reported in North America and Europe
following the introduction of new serotypes of serogroup C
(particularly serotype C:2a:P1:2) into a population in which
serogroup B strains had been the predominant causes of en-
demic disease.
As documented in Scandinavia, susceptibility to invasive me-
ningococcal disease is largely due to acquisition of a new vir-
ulent strain in a host without circulating bactericidal antibody
against the causative organism [14]. The United Kingdom in
November 1999 was the rst country to launch vaccination
against group C meningococcal disease, and a rapid decrease
in the incidence of this syndrome (including clusters) is expected
(see Public Health Laboratory Service [UK] annual report
19881999 and highlights 1999/2000). Infants and young adults
aged 1517 years are targeted, and this strategy may be ap-
plicable to other regions with clusters of meningococcal disease.
Serogroup A (/C) vaccines are currently available. Wide-
spread use of these vaccines in the meningitis belt is warranted
to reduce morbidity and mortality while more complex poly-
saccharide-protein conjugate vaccines are phased into use.
Another disturbing epidemiologic trend is the emergence of
antimicrobial resistance among meningeal pathogens. At pre-
sent the most serious is the emergence of penicillin resistance
(along with resistance to multiple other antimicrobial agents)
among S. pneumoniae. Antimicrobial usage, particularly b-lac-
tams in low concentrations for prolonged periods, leads to se-
lection for resistance among pneumococci in children and
adultsboth the carrier state and invasive disease; nevertheless,
penicillin resistance varies widely among developed countries
[15]. In addition to this selective pressure, other factors con-
tribute to the development and spread of resistant pathogens,
including an extension of their spectrum of resistance and re-
sistance genes among diverse microorganisms and mutations
in common genes [16].
Resistance to penicillin involves mutations in 1 or more pen-
icillin-binding proteins (PBP) in S. pneumoniae, reducing the
afnity for penicillin and related antibiotics. These mutations
are usually present in the transpeptidase penicillin-binding do-
main. Multiple mutations are required to result in high-level
resistance among PBP variants [17]. The genes that encode for
the altered PBP are called mosaics, since they consist of native
pneumococcal DNA mixed with fragments of foreign DNA,
presumably derived from streptococci normally resident in the
healthy human nasopharynx. This foreign DNA has been in-
corporated by the pneumococci into the chromosome. The
worldwide spread of penicillin resistance among S. pneumoniae
appears to be due to dissemination of several clones carrying
altered PBP genes. In addition, chloramphenicol resistance has
appeared among meningococci. If this trend continues on a
worldwide basis, the consequences will be devastating as chlo-
ramphenicol is widely used as the antimicrobial of choice in
resource-limited settings, especially in the sub-Saharan African
meningitis belt. Penicillin resistance among meningococci is also
spreading (e.g., from 9% of strains in 1998 to 25% of strains
b
y
g
u
e
s
t
o
n
S
e
p
t
e
m
b
e
r
6
,
2
0
1
4
h
t
t
p
:
/
/
j
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
JID 2002;186 (Suppl 2) Pathophysiology of Bacterial Meningitis S227
in 2001 in Ontario, Canada), but the impact on therapeutic
strategies is not known.
The clinical outcome of acute bacterial meningitis depends
on multiple factors including the socioeconomic status of the
patient (developed vs. developing countries), age, pathogen,
and the clinical characteristics and laboratory manifestations
of the acute infection. For example, the case fatality rate for
H. inuenzae type B meningitis in recent reviews has been about
5%, [1], a gure similar to that of meningococcal meningitis in
the same report. Conversely, the mortality rate associated with
pneumococcal meningitis is about 20% versus 15%30% for
Listeria monocytogenes in recent years [1]. About 30% of the
survivors of pneumococcal meningitis develop long-term se-
quelae such as hearing loss, neuropsychologic impairment, and
neurologic decits [18].
The case fatality rate of S. pneumoniae meningitis varies dra-
matically by agewith a case fatality rate of !10% in children
but about 40% in those 50 years old. These results apply only
to developed countries. In developing regions, 60%80%of chil-
dren and adults with pneumococcal meningitis still succumb to
the infection [18, 19]. The risk of death is greatest for those
with neurologic complications during the acute illness (e.g.,
cerebrovascular insults, hydrocephalus, brain edema, and in-
volvement of large intracranial blood vessels). Brain infarction
with severe irreversible cerebral damage and an increase of in-
tracranial pressure result from cerebrovascular involvement of
both arteries and veins. These complications may be diagnosed
by computerized tomography, magnetic resonance imaging or
angiography, or transcranial Doppler sonography, but these
modalities are not widely available in resource-limited settings.
Pathogenesis of Bacterial Meningitis
While not the focus of this review, recent studies have en-
hanced our understanding of the pathogenesis of bacterial men-
ingitis among the major pathogens. To cause disease, the path-
ogen must, in the absence of a neurosurgical procedure or CSF
leak, colonize the nasopharynx, traverse the nasopharynx into
the bloodstream, survive host defense mechanisms in the in-
travascular space, invade the blood-brain barrier (BBB), and
survive and replicate in the subarachnoid space, producing dis-
ease. Multiple interactions between the host and the organism
have been described in recent years and it is of interest that the
major meningeal pathogens have several similarities in common
(e.g., asymptomatic carriage in the nasopharynx, the ability to
cause devastating disease, phosphoryl choline moieties, poly-
saccharide capsules, IgA proteases, and certain physiologic fea-
tures such as phase variations, DNA transformation, and au-
tolysis) [2022].
Our laboratories have concentrated on S. pneumoniae; else-
where in this issue the elegant work of Kim [23] on the traversal
of Escherichia coli across the BBB is reported. A few highlights
of recent studies follow (for a more detailed discussion of path-
ogenesis, see [8]).
Pathophysiology of Bacterial Meningitis
Various bacteria including the major meningeal pathogens
(e.g., S. pneumoniae) undergo autolysis under harsh conditions
such as exposure to antimicrobial agents and/or growth to sta-
tionary phase. Autolysis consists of self-digestion of the cell
wall by peptidoglycan hydrolyases termed autolysins. At least
3 autolysins are recognized in pneumococci, but the major au-
tolysin is the N-acetyl-muramoyl-l-alanine amidase (LytA) [24].
Activation of LytA and autolysis result in the release in sub-
capsular bacterial components including peptidoglycan, lipo-
teichoic acid, bacterial DNA, and pneumolysin.
Mechanisms of immune activation. Various cell wall prod-
ucts of meningeal pathogens are well-known inducers of the
inammatory host response. The inammatory response in the
subarachnoid space characteristic of acute purulent meningitis
can be reproduced by the intracisternal challenge with whole
heat-killed unencapsulated pneumococci, their isolated cell
walls, lipoteichoic acid, or peptidoglycan, but not by the in-
jection of heat-killed encapsulated strains or isolated capsular
polysaccharide [25, 26]. Exact mechanisms of immune activa-
tion by pneumococcal cell wall products remain poorly under-
stood, but recent in vitro studies suggest that the rst step in
immune activation is binding of peptidoglycan and/or lipotei-
choic acid to the pattern recognition receptor membrane CD14
(mCD14). mCD14 is not a transmembrane molecule and thus
by itself cannot transmit the activating signal into the cell.
A second step in immune activation is necessary and this
potentially occurs through the toll-like receptor-2 (TLR-2).
Coexpression of CD14 and TLR-2 in Chinese hamster ovary
broblasts confers responsiveness to pneumococcal peptido-
glycan and heat-killed S. pneumoniae as evidenced by inducible
translocation of the nuclear transcription factor NF-kB [27].
These studies also suggest that pneumococci stimulate both a
TLR-2dependent and a TLR-2independent pathway; how-
ever, in a model of pneumococcal meningitis, TLR-2decient
mice responded to live pathogens virtually to the same extent
as wild type mice (Koedel et al., unpublished data). Leukocyte
inltration into the subarachnoid space and brain mRNA ex-
pression of proinammatory cytokines and chemokines did not
differ between TLR-2decient and wild type mice inoculated
with live pneumococci. It appears that mechanisms other than
binding of pneumococcal cell wall products to TLR-2 play a
central role in the induction of the host immune response during
pneumococcal meningitis. It appears that both TLR-2depen-
dent and independent (pneumolysin) pathways are sufcient
to cause inammation in the absence of the other, but in vivo
both are likely activated.
TLR-2independent immune activation may be mediated at
least in part by the pneumococcal toxin pneumolysin. Pneu-
b
y
g
u
e
s
t
o
n
S
e
p
t
e
m
b
e
r
6
,
2
0
1
4
h
t
t
p
:
/
/
j
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
S228 Scheld et al. JID 2002;186 (Suppl 2)
molysin stimulates the production of inammatory mediators in
vitro including tumor necrosis factor (TNF)-a, interleukin (IL)-
1b, and IL-6 [28]. Pneumolysin is also an inducer and/or activator
of enzymes such as phospholipase A
2
, COX-2, and inducible
nitric oxide synthase (iNOS). However, in a rabbit meningitis
model, a pneumolysin-decient pneumococcal strain resulted in
an inammatory response similar to that induced by injection of
the wild type strain, suggesting that pneumolysin is not essential
for the induction of meningeal inammation [29].
Another potential trigger of immune activation during acute
meningitis is bacterial DNA released during bacterial autolysis.
Bacterial DNA has substantial immune stimulatory effects on
B, NK, and dendritic cells and on monocytes and macrophages
[30, 31]. The activity of bacterial DNA is mediated by unme-
thylated CpG motifs, in particular base contexts. In fact, when
mice or rats are injected intracisternally with bacterial DNA
or unmethylated CpG oligonucleotides, meningitis developed
within 12 h. Bacterial DNA appears to initiate CNS inam-
mation by stimulation of macrophages and proinammatory
products such as TNF-a [32]. TLR-9 is absolutely required for
cellular responses to CpG DNA, and TLR-9decient mice
show no response to CpG DNA (inammatory cytokine pro-
duction from macrophages, maturation of dendritic cells, or
proliferation of splenocytes) [33]. TLR-9decient mice are also
completely resistant to the lethal effects of CpG DNA without
production of serum proinammatory cytokines. Thus, the role
of the CpG DNATLR-9 pathway for immune activation in
acute bacterial meningitis deserves further evaluation. In sum-
mary, subcapsular bacterial components act as inducers of the
host inammatory response in acute bacterial meningitis, but
the host receptor systems and downstream elements of signal
transduction are still largely unexplored.
Intracellular signal transduction pathways. For meningeal
pathogens, the major inammatory stimuli are lipopolysac-
charide (LPS) and peptidoglycan for gram-negative and gram-
positive organisms, respectively. These inammatory stimuli ac-
tivate I-kB kinase NF-kB pathways and 3 mitogen-activated
protein kinase (MAPK) pathways: extracellular signal-regu-
lated kinases (ERK) 1 and 2, c-Jun N-terminal kinase (JNK),
and p38 [34, 35]. As a result of activation of these signaling
pathways, a variety of transcription factors are activated: NF-
kB (p50/p65) and activator protein-1 (cFos/cJun), which co-
ordinate the induction of many genes encoding a variety of
inammatory mediators [36].
Soluble peptidoglycan strongly activates ERK-1 and -2 in
the mouse macrophage cell line RAW264-7 and moderately
activates JNK, while weak activation of p38 MAPK is ob-
served. In contrast, LPS strongly activates all of these kinases,
suggesting a similar but not identical activation of signal trans-
duction pathways by these major inammatory mediators of
meningeal pathogens [37].
Pneumococcal cell wall components release inammatory
mediators by mouse microglia, which is dependent on both p38
and ERK-2/ERK-1 MAPK activities [38]. These same MAPKs
are also activated when rat or human astrocytes are stimulated
with various pneumococcal cell wall fragments. In addition,
pneumococci activate NF-kB in undifferentiated human and
mature murine monocytes [39]. Although the signaling path-
ways involved in immune inactivation only recently became a
major focus of research activity, a rat model of pneumococcal
meningitis showed a marked increase in NF-kB activity. Phar-
macologic inhibition of NF-kB led to a signicant reduction of
host inammatory responses as evidenced by lower CSF leu-
kocyte and IL-6 concentrations [40]. It appears that NF-kB is
a central transcriptional activator of many genes that encode
proteins, host factors, or both involved in the pathophysiology
of pneumococcal meningitis, including cytokines, chemokines,
and adhesion molecules.
Proinammatory cytokines. Multiple cytokines play an im-
portant regulatory role in the control of inammation. TNF-
a, IL-1b, and IL-6 are major early response cytokines that
trigger, often in synergy, a cascade of inammatory mediators,
including other cytokines, arachidonic acid metabolites, che-
mokines, and reactive nitrogen and oxygen intermediates [41].
Multiple cell types within the CNS including cerebromicrovas-
cular endothelial cells, astrocytes, and microglia produce all 3
cytokines. Increased concentrations of these cytokines have
been detected in CSF samples from patients with acute bacterial
meningitis and concentrations of IL-1b, but not IL-6 and TNF-
a, are associated with signicantly worse disease outcome or
disease severity [42].
Brain mRNA and protein expression of IL-1b, IL-6, and
TNF-a are markedly up-regulated in rodents during the acute
stage of experimental pneumococcal meningitis [43, 44]. Recent
studies with genetically engineered mice provide further insight
into the role of acute phase cytokines in the pathophysiology
of pneumococcal meningitis. For example, brain bacterial titers
were not affected by either TNF-a or TNF receptor deciency
in murine models of CNS infection. Furthermore, leukocyte
recruitment into the subarachnoid space was not affected by
TNF deciency. In contrast, mice with targeted disruption of
TNF receptors p55 and p75 had decreased meningeal inam-
mation [45]. It appears that other TNF receptor ligands (e.g.,
lymphotoxin-a) must contribute to the induction and/or main-
tenance of the inammatory response during pneumococcal
meningitis. Intracisternal inoculation of pneumococci caused a
three-fold increase in CSF leukocyte concentrations in IL-6de-
cient mice when compared with wild type controls. Increased
CSF pleocytosis is thought to result from higher brain expres-
sion of the potent neutrophil chemoattractant macrophage in-
ammatory protein (MIP)-2 [8]. These observations are similar
to those in animal models of endotoxin-induced lung injury
and endotoxemia, where IL-6 appears to control the extent of
the inammatory response by down-regulating the expression
of chemokines and/or proinammatory cytokines.
No data have been presented on IL-1b or IL-1 receptor de-
b
y
g
u
e
s
t
o
n
S
e
p
t
e
m
b
e
r
6
,
2
0
1
4
h
t
t
p
:
/
/
j
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
JID 2002;186 (Suppl 2) Pathophysiology of Bacterial Meningitis S229
ciency and the pathophysiology of acute bacterial meningitis.
The role of caspase (Casp)-1 in the pathophysiology of pneu-
mococcal meningitis has been the subject of recent experiments.
Casp-1 plays a central role in the generation of mature IL-1b
and IL-18 [46]. Casp-1 mRNA and protein expression is up-
regulated in the brain during experimental pneumococcal men-
ingitis; this up-regulated activation is associated with increased
levels of IL-1b [8]. Furthermore, depletion of the Casp-1 gene
and/or pharmacologic blockade of Casp-1 attenuates the men-
ingitis-induced increase in IL-1b. A signicant reduction in NF-
kB activity, brain TNF-a, MIP-1a, and MIP-2 expression, and
CSF pleocytosis was also observed [8]. The Casp-1IL-1b sig-
naling pathways play a crucial role in the induction and am-
plication of the host inammatory response during pneu-
mococcal meningitis. TNF-a and IL-1b also stimulate the
expression of chemokines and adhesion molecules, which fur-
ther facilitate the passage of leukocytes from the circulation
into the subarachnoid space.
Chemokines. Based on the number and spacing of the con-
served N-terminal cysteines, chemokines are currently subdi-
vided into 4 distinct subfamilies: the CXC or a, CC or b, CX
3
C
or g, and C or d subfamilies [47]. The CXC chemokines are
further divided into 2 groups depending on the presence of the
ELR motif preceding the rst cysteine. Despite this classica-
tion, within each chemokine subfamily the individual members
often display overlapping chemoattractant activity. ELR-CXC
chemokines, such as IL-8 and growth related protein (Gro)-a,
are effective chemoattractants for neutrophils, but not for
monocytes. In contrast, nonELR-CXC chemokines, such as
IP-10 and, CC chemokines, such as monocyte chemotactic pro-
tein (MCP)-1 and MIP-1a, are poor chemoattractants for neu-
trophils but potent attractors of monocytes and lymphocytes.
Elevated levels of the chemokines IL-8, Gro-a, MCP-1, MIP-
1a, and MIP-1b are found in human CSF during bacterial
meningitis [48]. Furthermore, CSF from patients with bacterial
meningitis is chemotactic for neutrophils and mononuclear leu-
kocytes in an in vitro chemotaxis assay. Neutrophil chemotaxis
is reduced by antiIL-8 and antiGro-a antibodies, and mono-
nuclear cell migration is also reduced by a combination of
antiMCP-1, antiMIP-1a, and antiMIP-1b antibodies [48].
Brain mRNA and protein expression of MIP-2 and KC, the
two functional homologs of human IL-8, are markedly in-
creased during the acute phase of pneumococcal meningitis in
a murine model [43, 44]. Neutralization of MIP-2 bioactivity
reduced neutrophil inux into the CSF in an infant rat model
of Hib meningitis [8]. Thus, the available evidence suggests that
ELR-CXC chemokines play a critical role in leukocyte traversal
into the CSF during acute bacterial meningitis.
Leukocyte migration into the subarachnoid space. Leuko-
cyte migration from the circulation into the extravascular space
occurs through a multistep process governed by the sequential
activation of adhesion receptors and their ligands on both leu-
kocytes and the endothelium [49]. Four sequential steps (teth-
ering, triggering, rm adhesion, and emigration) are involved
in this adhesion cascade. The selectin family of adhesion mol-
ecules (P-, E-, L-selectin) mediates tethering and promotes leu-
kocyte rolling under ow conditions.
Firm adhesion of leukocytes to the endothelium is mediated
by a family of integrins. Integrin activation requires a triggering
step mediated by a proinammatory cytokine (e.g., IL-1b) and
chemokines (e.g., IL-8), complement products, and bacterial
cell wall components. Leukocyte integrins, once activated, bind
to endothelial cell count receptors. Macrophage antigen 1
(MAC-1; CD11b/CD18) is the predominant integrin involved
in neutrophil binding to the activated endothelial cell. Inter-
cellular adhesion molecule (ICAM)-1, an immunoglobulin-like
molecule, exhibits low constitutive levels on the cell surface of
the resting endothelium but is markedly induced by exposure
to inammatory stimuli and is the most important endothelial
ligand for MAC-1. After rm adhesion to endothelial cells,
leukocytes migrate along a chemotactic gradient, mediated by
chemokines into the subarachnoid space.
Partial inhibition of CSF leukocyte accumulation in the sub-
arachnoid space was noted in P-selectindecient mice during
experimental meningitis, whereas mice doubly decient in P-
and E-selectins showed dramatic and nearly complete inhibition
of leukocyte accumulation into the subarachnoid space [50].
Antibodies directed against the adhesion molecules MAC-1 or
ICAM-1 also reduced inux of neutrophils during experimental
meningitis and led to signicant reductions in intracranial com-
plications such as brain edema formation [51].
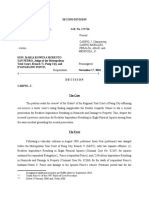
Mediators of brain damage. As shown in gure 1, by fol-
lowing the steps enumerated above, activated leukocytes can
release potentially tissue destructive agents including reactive
oxidants and proteolytic enzymes. Matrix metalloproteinases
(MMPs) have been the focus of recent investigations, both in
patients with bacterial meningitis and in experimental models
of the disease.
MMPs. MMPS are a family of zinc-dependent endopep-
tidases responsible for tissue remodeling via degradation of
extracellular matrix components [52, 53]. Collagen IV and -
bronectin are crucial components of the subendothelial basal
lamina of cerebral microvessels and contribute to the integrity
of the BBB. BBB disruption follows the intracerebral injection
of MMPs in experimental models [54]. Although it is possible
that migrating neutrophils release MMPs to facilitate traversal
from the circulation into the subarachnoid space, evidence for
this process is not available. The broad-spectrum MMP inhib-
itor BB-94 markedly attenuated BBB disruption but did not
signicantly reduce CSF pleocytosis in a rat model of menin-
gococcal meningitis [55]. Similarly, treatment with MMP in-
hibitors led to a signicant reduction of CSF TNF-a concen-
trations, BBB permeability, and the extent of neuronal injury
in an infant rat model of pneumococcal meningitis [56, 57].
MMP-9 and -8 are up-regulated in the CSF during bacterial
meningitis in humans, and higher concentrations of MMP-9
b
y
g
u
e
s
t
o
n
S
e
p
t
e
m
b
e
r
6
,
2
0
1
4
h
t
t
p
:
/
/
j
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
S230 Scheld et al. JID 2002;186 (Suppl 2)
Figure 1. Mechanisms of brain damage in experimental pneumo-
coccal meningitis. NF-kB, a transcriptional activator of many genes
involved in the pathogenesis of bacterial meningitis, encodes host fac-
tors including proinammatory cytokines, chemokines (e.g., interleukin
[IL]-8), and adhesion molecules. The proinammatory cytokines IL-
1b and tumor necrosis factor (TNF)-a are synthesized as inactive pre-
cursors that are processed to mature active forms by proteases (casbase
1 [Casp1], also known as IL-1bconverting enzyme, and TNF-a
converting enzyme [TACE]). IL-1b and TNF-a are potent activators
of NF-kB. This process may lead to the uncontrolled expression of
proinammatory mediators and the increased expression of adhesion
molecules both on the endothelium (e.g., intercellular adhesion mol-
ecule [ICAM]-1) and on neutrophils, leading to subsequent massive
inux of leukocytes into the subarachnoid space. Once present, acti-
vated leukocytes release a complex variety of potentially cytotoxic
agents including oxidants and proteolytic enzymes (e.g., matrix me-
talloproteinases [MMP]), which may contribute to tissue destruction.
Also, peroxynitrite may cause brain damage via a variety of indepen-
dent mechanisms. The best studied are attack of polyunsaturated fatty
acids, leading to lipid peroxidation, and an alternative pathway that
involves oxidant-induced DNA strand breakage and subsequent poly
(ADP ribose) polymerase (PARP) activation, which initiates an energy-
consuming intracellular cycle that ultimately results in cellular energy
depletion and cell death. Both mechanisms likely contribute to cell
injury during pneumococcal meningitis. ECM, extracellular matrix;
MIP, macrophage inammatory protein.
are associated with neurologic decits in patients with disease
compared with persons who had recovered fully, suggesting
high CSF concentrations of this MMP may signicantly in-
crease the risk for adverse outcome of bacterial meningitis in
humans [58].
Oxidants. In addition to proteolytic enzymes, several other
major effector molecules are available to the phagocyte that
may inuence pathophysiology of meningitis including reactive
oxygen species (ROS; e.g., superoxide) and reactive nitrogen
intermediates (RNIs; e.g., NO). ROS clearly play an important
role in the pathophysiology of acute bacterial meningitis. For
example, ROS generation has been detected in brain sections
of infant rats with group B streptococcal meningitis by use of
the manganese/diamino benzidine method and in vivo in a rat
model of pneumococcal meningitis by use of the lucigenin-
enhanced chemiluminescence technique [59, 60].
Meningitis-associated intracranial complications (including
cerebral hypoperfusion) increase intracranial pressure, brain
edema formation, and neuronal injury in experimental models
of bacterial meningitis and are attenuated or even prevented
by the use of antioxidants [61, 62]. NO/nitrite levels in the CSF
during meningitis are elevated in humans with bacterial men-
ingitis and in experimental animal models. NO production has
been observed uniformly in animal models of bacterial men-
ingitis, although administration of NOS inhibitors in experi-
mental models has yielded contradictory results ranging from
amelioration to deterioration of CNS complications and brain
damage [63, 64]. Unfortunately, NOS inhibitors are not selec-
tive for a single isoform of NOS and may have additional
pharmacologic effects unrelated to the NO pathway, thus con-
tributing to these contradictory results.
Knockout mice with a targeted disruption of single NOS
isoforms have been useful in dening the role of NO from
various enzymatic sources in the CNS [65, 66]. Mice decient
in the inducible NOS isoform exhibit signicantly lower levels
of inammatory mediators such as IL-1b, TNF-a, and MIP-
2 than wild type mice after challenge with pneumococci. Men-
ingitis-induced BBB disruption is signicantly reduced in par-
allel [43]. When mice with the endothelial NOS knockout were
used in similar experiments, aggravation of meningitis-induced
BBB permeability was observed. It appears that brain expres-
sion of proinammatory host factors such as IL-1b, KC, MIP,
and P-selectin may be responsible for these effects [8, 44]. It is
highly likely that NO generated by separate isoforms may have
different roles and potentially opposing effects during pneu-
mococcal meningitis. Inducible NOS seems to contribute to
some of the harmful pathophysiologic changes of the disease
while endothelial NOS-derived NO may play a protective role,
potentially through inhibition of leukocyte endothelial inter-
actions and the production of cytokines and chemokines.
Peroxynitrite is induced by various forms of inammation
and ischemia/reperfusion injury and may play a central role in
bacterial meningitis from generation of oxygen and nitrogen-
b
y
g
u
e
s
t
o
n
S
e
p
t
e
m
b
e
r
6
,
2
0
1
4
h
t
t
p
:
/
/
j
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
JID 2002;186 (Suppl 2) Pathophysiology of Bacterial Meningitis S231
Figure 2. Vicious cycle of pathophysiologic alterations leading to
neuronal injury during bacterial meningitis. BBB, blood-brain barrier;
CBV, cerebral blood volume.
centered free radicals. Nitrotyrosine concentrations, a useful
marker for the formation of peroxynitrite, which lasts only
seconds, were elevated in the CSF of patients with acute bac-
terial meningitis when compared with noninfected controls [67].
In addition, elevated concentrations of CSF nitrotyrosine are
associated with an unfavorable clinical outcome. Nitrotyrosine
residues on proteins have been detectedimmunohistochemically
in leukocytes in the subarachnoid space and in other areas such
as the leptomeninges penetrating cortical and occasionally pa-
renchymal blood vessels in both adult rats with pneumococcal
meningitis and in humans [67]. Treatment with a peroxynitrite
scavenger, uric acid, signicantly attenuates meningeal inam-
mation and meningitis-associated complications. The strong
oxidant peroxynitrite is denitely a central mediator of the
pathophysiologic alterations in bacterial meningitis [8].
Molecular mechanisms of oxidant-induced brain damage.
Peroxynitrite and other oxidants may contribute to the devel-
opment of brain damage and neuronal injury during bacterial
meningitis by a variety of mechanisms as shown in gure 1.
Lipid peroxidation through peroxynitrite inuence on poly-
unsaturated fatty acids can lead to the loss of cellular membrane
function and integrity. Malondialdehyde and 4-hydrox-2 (E-
Nonenal 4-HNE), markers of lipid peroxidation, are found in
elevated concentrations in both patients with bacterial men-
ingitis and in brain homogenates of infant rats with group B
streptococcal or pneumococcal meningitis [68, 69]. 4-HNE is
found in inammatory cells and in pial and penetrating cortical
blood vessels by immunohistochemistry techniques. Aminoste-
roids, inhibitors of lipid peroxidation, attenuate the pathophy-
siologic alterations and neuronal injury in rat models of pneu-
mococcal meningitis [70]. Clearly, lipid peroxidation in
meningitis is associated with brain injury. A similar staining
pattern for 4-HNE and nitrotyrosine suggests that RNI act as
initiators of lipid peroxidation during the disease.
Results of experiments by a group in Munich suggest that
another alternative pathway may explain oxidant-induceddam-
age during meningitis via DNA strand breakage in subsequent
poly (ADP ribose) polymerase (PARP) activation that initiates
an energy-consuming intracellular cycle that ultimately results
in cellular energy depletion and cell death [71, 72]. ADP ribose
polymer formation is a well-accepted marker for PARP cata-
lytic activity. Poly ADP-ribosylated proteins are higher in
mouse and rat brains 24 h after pneumococcal inoculation than
in uninfected control animals [73]. Knockout mice lacking the
PARP-1 gene are protected against the development of men-
ingitis-associated complications as outlined by the Munich
group. Inammatory host response is reduced in parallel. Phar-
macologic inhibition of PARP improves the clinical course of
pneumococcal meningitis. On balance, PARP activation in the
brain appears to play a crucial role in the pathophysiology of
bacterial meningitis [8, 73].
The vicious cycle of pathophysiologic alterations. Figure 2
shows that the combination of lipid peroxidation and PARP
activation may contribute substantially to endothelial cell in-
jury during bacterial meningitis. Once endothelial dysfunction
occurs, the consequences include cerebrovascular autoregula-
tion loss, loss of CO
2
reactivity of cerebral vessels, and increased
permeability of the BBB. BBB permeability disruption allows
plasma constituents to enter the brain, resulting in vasogenic
cerebral edema and an increase in intracranial pressure.
Intracranial pressure is a multifactorial process in meningitis
and is related not only to vasogenic edema but also cytotoxic
edema resulting from leukocyte inltration, interstitial edema
resulting from blockade of normal CSF pathways, and in-
creased blood volume in the brain [74, 75]. Marked increases
in intracranial pressure can be deleterious in patients with bac-
terial meningitis by causing cerebral herniation or decreasing
cerebral perfusion (a reduction in cerebral perfusion pressure
and/or loss of cerebrovascular autoregulation) and can ulti-
mately lead to irreversible brain injury or death.
Conclusions
Meningitis-associated brain injury and neuronal death is not
mediated simply by the presence of viable bacteria but occurs
as a consequence of the host reaction to bacterial components.
A wide variety of inammatory host factors involved in the
complex pathophysiologic cascade of bacterial meningitis have
been identied during the past decade, largely with experimen-
tal studies, but have also been conrmed in limited studies of
human material. The crucial role of the caspase 1IL-1b path-
way in the induction and amplication of the host inammatory
response during pneumococcal meningitis may lead to the iden-
tication of new potential therapeutic adjunctive agents. Sim-
ilarly, peroxynitrite and other important effector molecules con-
tributing to BBB disruption and neuronal injury may be
susceptible to adjunctive treatments.
Lipid peroxidation and the activation of PARP-1 are also
b
y
g
u
e
s
t
o
n
S
e
p
t
e
m
b
e
r
6
,
2
0
1
4
h
t
t
p
:
/
/
j
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
S232 Scheld et al. JID 2002;186 (Suppl 2)
central mechanisms of oxidant-induced brain damage, and
pharmacologic interference with these biochemical pathways
may be the most promising adjunctive therapeutic strategy (re-
viewed in [8]). We believe that further exploration of these path-
ways will not only be relevant to the development of therapeutic
adjunctive strategies in bacterial meningitis but may also im-
prove outcomes in other inammatory conditions of the CNS
such as meningoencephalitis, subarachnoid hemorrhage-in-
duced vasospasm, and ischemia reperfusion following stroke.
Antimicrobial agents that modulate the release of proinam-
matory bacterial compounds may also have a potential effect
on bacterial meningitis as reviewed recently [76], but systematic
study of this approach in humans has not yet been validated.
References
1. Schuchat A, Robinson K, Wenger JK, et al. Bacterial meningitis in the United
States in 1995. Active Surveillance Team. N Engl J Med 1997; 337:9706.
2. Tikhomirov E, Santamaria M, Esteves K. Meningococcal disease: public
health burden and control. World Health Stat Q 1997; 50:1707.
3. Anonymous. Epidemic meningococcal disease. World Health Organization
fact sheet 105. Geneva: WHO, 1998.
4. Grimwood K, Anderson P, Anderson V, Tan L, Nolan T. Twelve year out-
comes following bacterial meningitis: further evidence for persisting ef-
fects. Arch Dis Child 2000; 83:1116.
5. Nathan BR, Scheld WM. New advances in the pathogenesis and pathophy-
siology of bacterial meningitis. Curr Infect Dis Rep 2000; 2:3326.
6. Tunkel AR, Scheld WM. Acute bacterial meningitis. Lancet 1995; 346:
167580.
7. Pster HW, Scheld WM. Brain injury in bacterial meningitis. Curr Opin
Neurol 1997; 10:2549.
8. Koedel U, Pster HW, Scheld WM. Overview on the pathogenesis and path-
ophysiology of acute bacterial meningitis: with special emphasis on pneu-
mococcal meningitis. Lancet Infect Dis (in press).
9. Nau R, Bru ck W. Neuronal injury in bacterial meningitis: mechanisms and
implications for therapy. Trends Neurosci 2002; 25:3845.
10. Simon RP, Beckman JS. Why pus is bad for the brain. Neurology 2002; 58:
1678.
11. Zangwill KM, Schuchat A, Riedo FX, et al. School-based clusters of me-
ningococcal disease in the United States. Descriptive epidemiology and a
case-control analysis. JAMA 1997; 277:38995.
12. Austin CC, Fingar AR, Langkop C. Outbreak of serogroup Cmeningococcal
disease among preschool-aged children: Illinois, 1996. Am J Public Health
1998; 88:685.
13. Hastings L, Stuart J, Andrews N, Begg N. A retrospective survey of clusters
of meningococcal disease in England and Wales, 1993 to 1995: estimated
risks of further cases in household and educational settings. Commun Dis
Rep CDR Rev 1997; 7:R195200.
14. Gold R. Epidemiology of bacterial meningitis. Infect Dis Clin North Am
1999; 13:51525.
15. Hoban DJ, Doern GV, Fluit AC, Roussel-Delvallez M, Jones RN. Worldwide
prevalence of antimicrobial resistance in Streptococcus pneumoniae, Hae-
mophilus inuenzae, and Moraxella catarrhalis in the SENTRY antimi-
crobial surveillance program, 19971999. Clin Infect Dis 2001; 32(Suppl
2):S8193.
16. Kaye KS, Kaye D. Multidrug-resistant pathogens: mechanisms of resistance
and epidemiology. Curr Infect Dis Rep 2000; 2:3918.
17. Charpentier E, Tuomanen E. Mechanisms of antibiotic resistance and tol-
erance in Streptococcus pneumoniae. Microbes Infect 2000; 2:185564.
18. Arditi M, Mason EOJ, Bradley JS, et al. Three-year multicenter surveillance
of pneumococcal meningitis in children: clinical characteristics, and out-
come related to penicillin susceptibility and dexamethasone use. Pediatrics
1998; 102:108797.
19. Hortal M, Camou T, Palacio R, Dibarbourne H, Garcia A. Ten-year review
of invasive pneumococcal diseases in children and adults from Uruguay:
clinical spectrum, serotypes, and antimicrobial resistance. Int J Infect Dis
2000; 4:915.
20. McCullers JA, Tuomanen EI. Molecular pathogenesis of pneumococcal pneu-
monia. Front Biosci 2001; 6:D87789.
21. Marrs CF, Krasan GP, McCrea KW, Clemans DL, Gilsdorf JR. Haemophilus
inuenzaehuman specic bacteria. Front Biosci 2001; 6:E4160.
22. Tzeng YL, Stephens DS. Epidemiology and pathogenesis of Neisseria men-
ingitidis. Microbes Infect 2000; 2:687700.
23. Kim KS. Strategy of Escherichia coli for crossing the blood-brain barrier. J
Infect Dis 2002; 186(Suppl 2):S2203 (in this issue).
24. Lopez R, Garcia E, Garcia P, Garcia JL. The pneumococcal cell wall de-
grading enzymes: a modular design to create new lysins? Microb Drug
Resist 1997; 3:199211.
25. Tuomanen E, Tomasz A, Hengstler B, Zak O. The relative role of bacterial
cell wall and capsule in the induction of inammation in pneumococcal
meningitis. J Infect Dis 1985; 151:53540.
26. Tuomanen E, Liu H, Hengstler B, Zak O, Tomasz A. The induction of
meningeal inammation by components of the pneumococcal cell wall. J
Infect Dis 1985; 151:85968.
27. Yoshimura A, Lien E, Ingalls RR, Tuomanen E, Dziarski R, Golenbock D.
Cutting edge: recognition of gram-positive bacterial cell wall components
by the innate immune system occurs via toll-like receptor 2. J Immunol
1999; 163:15.
28. Braun JS, Novak R, Gao G, Murray PJ, Shenep JL. Pneumolysin, a protein
toxin of Streptococcus pneumoniae, induces nitric oxide production from
macrophages. Infect Immun 1999; 67:37506.
29. Friedland IR, Paris MM, Hickey S, et al. The limited role of pneumolysin
in the pathogenesis of pneumococcal meningitis. J Infect Dis 1995; 172:
8059.
30. Medzhitov R. CpG DNA: security code for host defense. Nat Immunol
2001; 2:156.
31. Wagner H. Toll meets bacterial CpG-DNA. Immunity 2001; 14:499502.
32. Deng GM, Liu ZQ, Tarkowski A. Intracisternally localized bacterial DNA
containing CpG motifs induces meningitis. J Immunol 2001; 167:461626.
33. Hemmi H, Takeuchi O, Kawai T, el al. Atoll-like receptor recognizes bacterial
DNA. Nature 2000; 408:7405.
34. Chang L, Karin M. Mammalian MAP kinase signaling cascades. Nature
2001; 410:3740.
35. Herlaar E, Brown Z. p38 MAPK signaling cascades in inammatory disease.
Mol Med Today 1999; 5:43947.
36. Guha M, Mackman N. LPS induction of gene expression in human mono-
cytes. Cell Signal 2001; 13:8594.
37. Dziarski R, Jin YP, Gupta D. Differential activation of extra cellular signal-
regulated kinase (ERK) 1, ERK2, p38, and c-Jun NH2-terminal kinase
mitogen-activated protein kinases by bacterial peptidoglycan. J Infect Dis
1996; 174:77785.
38. Hanisch UK, Prinz M, Angstwurm K, et al. The protein tyrosine kinase
inhibitor AG126 prevents the massive microglial cytokine induction by
pneumococcal cell walls. Eur J Immunol 2001; 31:210415.
39. Spellerberg B, Rosenow C, Sha W, Tuomanen EI. Pneumococcal cell wall
activates NFkB in human monocytes: aspects distinct from endotoxin.
Microb Pathog 1996; 20:30917.
40. Koedel U, Bayerlein I, Paul R, Sporer B, Pster HW. Pharmacological in-
terference with NF-B activation attenuates central nervous system com-
plications in experimental pneumococcal meningitis. J Infect Dis 2000;
182:143745.
41. Dinarello CA. Proinammatory cytokines. Chest 2000; 118:5038.
42. Van Furth AM, Roord JJ, Van Furth R. Roles of proinammatory and anti-
inammatory cytokines in pathophysiology of bacterial meningitis and
effect of adjunctive therapy. Infect Immun 1996; 64:488390.
b
y
g
u
e
s
t
o
n
S
e
p
t
e
m
b
e
r
6
,
2
0
1
4
h
t
t
p
:
/
/
j
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
JID 2002;186 (Suppl 2) Pathophysiology of Bacterial Meningitis S233
43. Winkler F, Koedel U, Kastenbauer S, Pster HW. Differential expression of
nitric oxide synthases in bacterial meningitis: role of the inducible isoform
for blood-brain barrier breakdown. J Infect Dis 2001; 183:174959.
44. Koedel U, Paul R, Winkler F, Kastenbauer S, Huang PL, Pster HW. Lack
of endothelial nitric oxide synthase aggravates murine pneumococcal men-
ingitis. J Neuropathol Exp Neurol 2001; 60:104150.
45. Wellmer A, Gerber J, Ragheb J, et al. Effect of deciency of tumor necrosis
factor alpha or both of its receptors on Streptococcus pneumoniae central
nervous system infection and peritonitis. Infect Immun 2001; 69:68816.
46. Los M, Wesselborg S, Schulze-Osthoff K. The role of caspases in develop-
ment, immunity, and apoptotic signal transduction: lessons fromknockout
mice. Immunity 1999; 10:62939.
47. Baggiolini M. Chemokines in pathology and medicine. J Intern Med 2001;
250:91104.
48. Spanaus KS, Nadal D, Pster HW, et al. C-X-C and C-C chemokines are
expressed in the cerebrospinal uid in bacterial meningitis and mediate
chemotactic activity on peripheral blood-derived polymorphonuclear and
mononuclear cells in vitro. J Immunol 1997; 158:195664.
49. Kubes P, Ward PA. Leukocyte recruitment and the acute inammatory re-
sponse. Brain Pathol 2000; 10:12735.
50. Tang T, Frenette PS, Hynes RO, Wagner DD, Mayadas TN. Cytokine-in-
duced meningitis is dramatically attenuated in mice decient in endothelial
selectins. J Clin Invest 1996; 97:248590.
51. Wever JR, Angstwurm K, Bu rger W, Einhaupl KM, Dirnagl U. Anti ICAM-
1 (CD 54) monoclonal antibody reduces inammatory changes in exper-
imental bacterial meningitis. J Neuroimmunol 1995; 63:638.
52. Leppert D, Lindberg RL, Kappos L, Leib SL. Matrix metalloproteinases;
multifunctional effectors of inammation in multiple sclerosis and bac-
terial meningitis. Brain Res Brain Res Rev 2001; 36:24957.
53. Yong VW, Power C, Forsyth P, Edwards DR. Metalloproteinases in biology
and pathology of the nervous system. Nat Rev Neurosci 2001; 2:50211.
54. Lukes A, Mun-Bryce S, Lukes M, Rosenberg GA. Extracellular matrix deg-
radation by metalloproteinases and central nervous system diseases. Mol
Neurobiol 1999; 19:26784.
55. Paul R, Lorenzl S, Keodel U, et al. Matrix metalloproteinases contribute to
the blood-brain barrier disruption during bacterial meningitis. AnnNeurol
1998; 44:592600.
56. Leib SL, Leppert D, Clements J, Tauber MG. Matrix metalloproteinases
contribute to brain damage in experimental pneumococcal meningitis.
Infect Immun 2000; 68:611520.
57. Leib SL, Clements JM, Lindberg RL, et al. Inhibition of matrix metallo-
proteinases and tumour necrosis factor alpha converting enzyme as ad-
juvant therapy in pneumococcal meningitis. Brain 2001; 124:173442.
58. Leppert D, Leib SL, Grygar C, Miller KM, Schaad UB, Hollander GA.
Matrix metalloproteinase (MMP)-8 and MMP-9 in cerebrospinal uid
during bacterial meningitis: association with blood-brain barrier damage
and neurological sequelae. Clin Infect Dis 2000; 31:804.
59. Leib SL, Kim YS, Chow LL, Sheldon RA, Tauber MG. Reactive oxygen
intermediates contribute to necrotic and apoptotic neuronal injury in an
infant rat model of bacterial meningitis due to group B streptococci. J
Clin Invest 1996; 98:26329.
60. Dirnagl U, Koedel U, Pster HW, Villringer A, Schleinkofer L, Einhaupl
KM. Detection of brain free radical generated photons in vivo: prelimi-
nary results. Adv Exp Med Biol 1993; 333:20312.
61. Koedel U, Pster HW. Protective effect of the antioxidant N-acetyl-l-cysteine
in pneumococcal meningitis in the rat. Neurosci Lett 1997; 225:336.
62. Auer M, Pster LA, Leppert D, Tauber MG, Leib SL. Effects of clinically
used antioxidants in experimental pneumococcal meningitis. J Infect Dis
2000; 182:34750.
63. Koedel U, Bernatowicz A, Paul R, Frei K, Fontana A, Pster HW. Exper-
imental pneumococcal meningitis: cerebrovascular alterations, brain
edema, and meningeal inammation are linked to the production of nitric
oxide. Ann Neurol 1995; 37:31323.
64. Buster BL, Weintrob AC, Townsend GC, Scheld WM. Potential role of nitric
oxide in the pathophysiology of experimental bacterial meningitis in rats.
Infect Immun 1995; 63:38359.
65. Bolanos JP, Almeida A. Roles of nitric oxide in brain hypoxia-ischemia.
Biochim Biophys Acta 1999; 1411:41536.
66. Huang PL. Lessons learned from nitric oxide synthase knockout animals.
Semin Perinatol 2000; 24:8790.
67. Kastenbauer S, Loedel U, Becker BF, Pster HW. Oxidative stress in bacterial
meningitis in humans. Neurology 2002; 58:18691.
68. Koedel U, Pster HW. Superoxide production by primary rat cerebral en-
dothelial cells in response to pneumococci. J Neuroimmunol 1999; 96:
190200.
69. Christen S, Schaper M, Lykkesfeldt J, et al. Oxidative stress in brain during
experimental bacterial meningitis: differential effects of alpha-phenyl-tert-
butyl nitrone and N-acetylcysteine treatment. Free Radic Biol Med
2001; 31:75462.
70. Lorenzl S, Koedel U, Frei K, Bernatowicz A, Fontata A, Pster HW. Pro-
tective effect of a 21-aminosteriod during experimental pneumococcal
meningitis. J Infect Dis 1995; 172:1138.
71. Ha HC, Snyder SH. Poly (ADP-ribose) polymerase-1: in the nervous system.
Neurobiol Dis 2000; 7:22539.
72. Shall S, De Murcia G. Poly (ADP-ribose) polymerase-1: what have we learned
from the decient mouse model? Mutat Res 2000; 460:115.
73. Hausmann EH, Berman NE, Wang YY, Meara JB, Wood GW, Klein RM.
Selective chemokine mRNA expression following brain injury. Brain Res
1998; 788:4959.
74. Kempski O. Cerebral edema. Semin Nephrol 2001; 21:3037.
75. Scheld WM, Dacey RC, Winn HR, Welsh JE, Jane JA, Sande MA. Cere-
brospinal uid outow resistance in rabbits with experimental meningitis.
J Clin Invest 1980; 66:24353.
76. Nau R, Eiffert H. Modulation of release of proinammatory bacterial com-
pounds by antibacterials: potential impact on course of inammation and
outcome in sepsis and meningitis. Clin Microbiol Rev 2002; 15:95110.
b
y
g
u
e
s
t
o
n
S
e
p
t
e
m
b
e
r
6
,
2
0
1
4
h
t
t
p
:
/
/
j
i
d
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
You might also like
- Anatomy of Long Bone and Classification of Joints: Prepared by DR Dipendra Maharjan 1 Yr Resident, NAMSDocument32 pagesAnatomy of Long Bone and Classification of Joints: Prepared by DR Dipendra Maharjan 1 Yr Resident, NAMSAfiqah So JasmiNo ratings yet
- Growth Charts For Children With Down Syndrome CanDocument12 pagesGrowth Charts For Children With Down Syndrome CanAfiqah So JasmiNo ratings yet
- Imm 922Document1 pageImm 922Afiqah So JasmiNo ratings yet
- Growth Charts For Down's Syndrome From Birth To 18 Years of AgeDocument7 pagesGrowth Charts For Down's Syndrome From Birth To 18 Years of AgeAfiqah So JasmiNo ratings yet
- Summary of New Recommendations: HIV Testing and CounsellingDocument9 pagesSummary of New Recommendations: HIV Testing and CounsellingAfiqah So JasmiNo ratings yet
- Iron Deficiency Anaemia in Toddlers: Learning PointsDocument8 pagesIron Deficiency Anaemia in Toddlers: Learning PointsAfiqah So JasmiNo ratings yet
- Barb Melo SkyDocument17 pagesBarb Melo SkyAfiqah So JasmiNo ratings yet
- Improve Your Hands-On Nutrition Physical Exam SkillsDocument27 pagesImprove Your Hands-On Nutrition Physical Exam SkillsAfiqah So JasmiNo ratings yet
- Theories OutlineDocument16 pagesTheories Outlineapi-242756158No ratings yet
- CI Mar2012 Growth Charts en - Rev2013Document13 pagesCI Mar2012 Growth Charts en - Rev2013Afiqah So JasmiNo ratings yet
- Pathophysiology Infants: of inDocument4 pagesPathophysiology Infants: of inAfiqah So JasmiNo ratings yet
- Overview07 WebDocument34 pagesOverview07 WebAfiqah So JasmiNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Chapter 9 - PPT (New)Document43 pagesChapter 9 - PPT (New)Syarifah NourazlinNo ratings yet
- Multicutural LiteracyDocument3 pagesMulticutural LiteracyMark Alfred AlemanNo ratings yet
- Invitation 2023Document10 pagesInvitation 2023Joanna Marie Cruz FelipeNo ratings yet
- Crime Scene Manual FullDocument19 pagesCrime Scene Manual FullMuhammed MUZZAMMILNo ratings yet
- Pathfinder CharacterSheet.1.8InterActiveDocument3 pagesPathfinder CharacterSheet.1.8InterActiveJessica AlvisNo ratings yet
- The Biofloc Technology (BFT) Water Quality, Biofloc Composition, and GrowthDocument8 pagesThe Biofloc Technology (BFT) Water Quality, Biofloc Composition, and GrowthHafez MabroukNo ratings yet
- Rosenberg Et Al - Through Interpreters' Eyes, Comparing Roles of Professional and Family InterpretersDocument7 pagesRosenberg Et Al - Through Interpreters' Eyes, Comparing Roles of Professional and Family InterpretersMaria AguilarNo ratings yet
- German Monograph For CannabisDocument7 pagesGerman Monograph For CannabisAngel Cvetanov100% (1)
- Papadakos PHD 2013Document203 pagesPapadakos PHD 2013Panagiotis PapadakosNo ratings yet
- CV Michael Naughton 2019Document2 pagesCV Michael Naughton 2019api-380850234No ratings yet
- 1027 12Document3 pages1027 12RuthAnayaNo ratings yet
- A/L 2021 Practice Exam - 13 (Combined Mathematics I) : S.No Name Batch School Ad No. Marks RankDocument12 pagesA/L 2021 Practice Exam - 13 (Combined Mathematics I) : S.No Name Batch School Ad No. Marks RankElectronNo ratings yet
- BhattacharyaDocument10 pagesBhattacharyavoraciousvNo ratings yet
- Ancestral Healing PrayersDocument4 pagesAncestral Healing Prayerssuperhumannz100% (13)
- Motivational Speech About Our Dreams and AmbitionsDocument2 pagesMotivational Speech About Our Dreams and AmbitionsÇhärlöttë Çhrístíñë Dë ÇöldëNo ratings yet
- Dan 440 Dace Art Lesson PlanDocument4 pagesDan 440 Dace Art Lesson Planapi-298381373No ratings yet
- Ivler vs. Republic, G.R. No. 172716Document23 pagesIvler vs. Republic, G.R. No. 172716Joey SalomonNo ratings yet
- CH Folk Media and HeatlhDocument6 pagesCH Folk Media and HeatlhRaghavendr KoreNo ratings yet
- Bagon-Taas Adventist Youth ConstitutionDocument11 pagesBagon-Taas Adventist Youth ConstitutionJoseph Joshua A. PaLaparNo ratings yet
- The Idea of Multiple IntelligencesDocument2 pagesThe Idea of Multiple IntelligencesSiti AisyahNo ratings yet
- A Lei Do Sucesso Napoleon Hill Download 2024 Full ChapterDocument23 pagesA Lei Do Sucesso Napoleon Hill Download 2024 Full Chapterdavid.brown752100% (12)
- Stockholm KammarbrassDocument20 pagesStockholm KammarbrassManuel CoitoNo ratings yet
- Site Master S113C, S114C, S331C, S332C, Antenna, Cable and Spectrum AnalyzerDocument95 pagesSite Master S113C, S114C, S331C, S332C, Antenna, Cable and Spectrum AnalyzerKodhamagulla SudheerNo ratings yet
- The John Molson School of Business MBA 607 Final Exam June 2013 (100 MARKS)Document10 pagesThe John Molson School of Business MBA 607 Final Exam June 2013 (100 MARKS)aicellNo ratings yet
- Effect of Intensive Health Education On Adherence To Treatment in Sputum Positive Pulmonary Tuberculosis PatientsDocument6 pagesEffect of Intensive Health Education On Adherence To Treatment in Sputum Positive Pulmonary Tuberculosis PatientspocutindahNo ratings yet
- India: SupplyDocument6 pagesIndia: SupplyHarish NathanNo ratings yet
- CSEC Eng A Summary ExerciseDocument1 pageCSEC Eng A Summary ExerciseArisha NicholsNo ratings yet
- Dark Witch Education 101Document55 pagesDark Witch Education 101Wizard Luxas100% (2)
- F3 Eng Mid-Term 2023Document5 pagesF3 Eng Mid-Term 2023Mwinyi BlogNo ratings yet
- Bgs Chapter 2Document33 pagesBgs Chapter 2KiranShettyNo ratings yet