Professional Documents
Culture Documents
Lewis COPD Case Study
Uploaded by
atarisgurl08Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lewis COPD Case Study
Uploaded by
atarisgurl08Copyright:
Available Formats
COPD (Ch. 29 p.
607)
1. What classic manifestations indicate the patient had a COPD exacerbation?
Increased dyspnea and increased volume and purulence of sputum.
2. What are some likely causes of her COPD?
Smoking and air pollution as a traffic patrolwoman
3. What symptoms indicate the overuse of inhalers, and which drug would cause the symptoms described?
Jitters and racing heart; the Ventolin HFA would be the cause.
4. What is the only way H.M. can affect the natural history or progression of COPD?
Stop smoking
5. Why would H.M. feel full fast when eating? What could you do to minimize this issue?
The food eaten enlarges the abdomen and this presses on the flat diaphragm. Thus the muscle is
further inhibited from participating in respiration in addition to the already hyperinflated lungs.
6. Interpret the ABGs. What pattern do you see?
pH: 7.34: low, thus acidosis (normal 7.35 to 7.45)
PaCO
2
:
49 mm Hg: high, thus the cause of the acidosis (normal 35 to 45 mm Hg)
HCO
3
:
27 mEq/L (normal 19 to 24): high, thus the kidneys are compensating by conserving bicarbonate
and trying to bring the pH to normal. H.M. had partially compensated respiratory acidosis on
admission.
Also with PaO
2
70 mm Hg, she is hypoxemic.
7. What are nursing priorities for discharge planning and teaching?
Nutrition:
5 to 6 meals, small, per day with lower carbohydrate and calories from protein/fats.
Nutritional supplements if tolerated.
Weigh weekly; if weight trends downward, contact health care provider.
Activity:
Confer with health care provider about pulmonary rehab order or at least one time consult with PT to
develop home exercise program for patient.
Encourage daily walking with increasing time and distance.
Confer with health care provider if patient qualifies for oxygen during exercise. Suggest a 6-minute
walk test.
Medications:
Explain the action of the Ventolin HFA and how the symptoms she had were a direct result of too
much. Explain how it should be dosed and reinforce the use of the counter on the MDI. Ask the patient
to demonstrate how she uses and cleans her MDI and how she tells if it is empty (i.e., look at the
counter).
Explain the Advair DPI discus and have the patient demonstrate use. Explain the difference between
the DPI and MDI. Explain why mouth rinses are important after the Advair and provide written points
on the difference. Explain that the Advair will prevent her from having as many exacerbations. Also
explain that the long-acting
2
-adrenergic agonists (LABA) should prevent night-time dyspnea.
Explain how prednisone works and why it is tapered. Explain that the azithromycin needs to be taken
until all pills are gone, despite improvement in symptoms.
Discuss the cardinal symptoms of COPD exacerbation including increased dyspnea, increased volume
and purulence of sputum, and what and when she should report to the health care provider.
Teach the patient huff coughing and pursed lip breathing and give written materials on these
techniques and have her return the demonstration
8. Based on the assessment data presented, what are your priority nursing diagnoses? Are there any
collaborative problems?
Altered nutrition: less than body requirements related to poor nutritional intake.
Activity intolerance related to hypoxemia, deconditioning as evidenced by difficulty climbing one flight
of stairs.
Deficient knowledge related to overuse of MDI and new medications ordered at discharge.
9. H.M.s son has been trying to convince his mother to quit smoking for many years without success. He asks
you to tell his mother the results of her pulmonary function tests to convince her it is time to quit. Will this
approach work?
Analysis of evidence has determined that the use of spirometry or communication of the results does
not independently increase smoking cessation or the likelihood that a person would maintain smoking
abstinence.
You might also like
- NRSG 115 CCL CDL Spring 2020 Lab Information SheetDocument7 pagesNRSG 115 CCL CDL Spring 2020 Lab Information SheetSethNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanAl RizkyNo ratings yet
- VSim SARAH LIN For Nursing - Health Assessment POST QUIZDocument5 pagesVSim SARAH LIN For Nursing - Health Assessment POST QUIZWen RodsaNo ratings yet
- Nursing Case CadDocument26 pagesNursing Case CadShield DalenaNo ratings yet
- Case StudyPainDocument1 pageCase StudyPainlovesalad100% (1)
- Cardiovascular ADocument3 pagesCardiovascular AAutumn AllisonNo ratings yet
- Chapter 24 Management of Patients With Chronic Pulmonary DisordersDocument3 pagesChapter 24 Management of Patients With Chronic Pulmonary DisordersPeej Reyes100% (1)
- Nursing Concept MapDocument2 pagesNursing Concept MapMary Mann100% (1)
- STUDENT Sepsis Rapid ReasoningDocument6 pagesSTUDENT Sepsis Rapid Reasoningghodghod123No ratings yet
- Assignmen 1 AnswersDocument3 pagesAssignmen 1 AnswersAlasl BobyNo ratings yet
- ANEMIADocument48 pagesANEMIAjomcy0% (2)
- Activity Intolerance Care Plan For CFDocument8 pagesActivity Intolerance Care Plan For CFapi-314197645No ratings yet
- Pneumonia Causative Agent: 1. Infectious - Bacteria (Streptococcus Pneumonia) Virus FungiDocument2 pagesPneumonia Causative Agent: 1. Infectious - Bacteria (Streptococcus Pneumonia) Virus FungiFreeNursingNotes100% (1)
- Nursing DiagnosisDocument7 pagesNursing DiagnosisMariya Mikaela Garcia SoledadNo ratings yet
- NURSING CARE OF ADULTS I: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS I: Passbooks Study GuideNo ratings yet
- EvalDocument3 pagesEvalapi-433857993No ratings yet
- The Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseFrom EverandThe Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseNo ratings yet
- Concept MapDocument6 pagesConcept Mapapi-499028250No ratings yet
- COPD SimDocument10 pagesCOPD Simbarbara60% (5)
- Assessment of Respiratory Function Chpt.20Document32 pagesAssessment of Respiratory Function Chpt.20Maricar RosasNo ratings yet
- Chapter - 037 - 1 Infective Endocarditis ClassDocument41 pagesChapter - 037 - 1 Infective Endocarditis ClassWisdomIsMiseryNo ratings yet
- Life and DeathDocument23 pagesLife and DeathJea Joel MendozaNo ratings yet
- CH 32Document8 pagesCH 32Elizabeth PetersenNo ratings yet
- NUR1213L May2013 FinalDocument23 pagesNUR1213L May2013 FinalOzzy Viadnes MalanaNo ratings yet
- Chapter 3 Fluids and Electrolytes - Acid-Base BalanceDocument8 pagesChapter 3 Fluids and Electrolytes - Acid-Base BalanceDiony CruzNo ratings yet
- Mental Health - PsychopharmacologyDocument4 pagesMental Health - PsychopharmacologyRenetria DrakeNo ratings yet
- Nur411 Syllabus Part 1 Fall 2011Document21 pagesNur411 Syllabus Part 1 Fall 2011bmccsnresources0% (1)
- BloodDocument27 pagesBloodRagda AhmedNo ratings yet
- Status Epilepticus Case Study Kristopher Kirby.Document4 pagesStatus Epilepticus Case Study Kristopher Kirby.KrisNo ratings yet
- ETOH Case StudyDocument5 pagesETOH Case StudyCharme Jean RaygonNo ratings yet
- Atelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesFrom EverandAtelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesNo ratings yet
- Bronchospasm PR 1Document41 pagesBronchospasm PR 1teklayNo ratings yet
- Acetaminophen PDFDocument1 pageAcetaminophen PDFmp1757No ratings yet
- Management of Patients With Gastric and Duodenal DisordersDocument47 pagesManagement of Patients With Gastric and Duodenal DisordersJor GarciaNo ratings yet
- Case Study Multiple Organ Dysfunction and ShockDocument3 pagesCase Study Multiple Organ Dysfunction and ShockJrBong SemaneroNo ratings yet
- EBP Poster Template 2019Document1 pageEBP Poster Template 2019Momina ArshadNo ratings yet
- Impaired Gas ExchangeDocument4 pagesImpaired Gas ExchangeNuraini Hamzah100% (1)
- Nursing Process Overview: Health Assessment NotesDocument40 pagesNursing Process Overview: Health Assessment NotesEliakim III InsongNo ratings yet
- NandaDocument28 pagesNandaAmit MartinNo ratings yet
- Ati Codes Cont'Document1 pageAti Codes Cont'm1k0eNo ratings yet
- Learning Log of Reflective Practice FormDocument8 pagesLearning Log of Reflective Practice FormTomii HajiNo ratings yet
- Clinical 2Document2 pagesClinical 2Jonathan100% (1)
- Metoprolol Teaching PlanDocument18 pagesMetoprolol Teaching Planapi-419091662No ratings yet
- Flashcards 2601-2800Document191 pagesFlashcards 2601-2800kkenNo ratings yet
- Part I: Emergency Department (ED) : SKINNY ReasoningDocument6 pagesPart I: Emergency Department (ED) : SKINNY ReasoningUzumaki KNo ratings yet
- Types of Seizure & Status Epilepticus: Prepared By: Ivy Joy A. Benitez, BSN 4-ADocument28 pagesTypes of Seizure & Status Epilepticus: Prepared By: Ivy Joy A. Benitez, BSN 4-AyviyojNo ratings yet
- COPD Acute Management ABCDEDocument11 pagesCOPD Acute Management ABCDESSNo ratings yet
- Cirrhosis Case StudyDocument20 pagesCirrhosis Case StudyJodi Schaefer100% (1)
- Alterations in VentilationDocument10 pagesAlterations in VentilationCharisma Pastor100% (1)
- A. Cardiac Failure: Biologic CrisisDocument11 pagesA. Cardiac Failure: Biologic CrisisJillian CaumbanNo ratings yet
- Cardiac Arrest, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCardiac Arrest, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Concept Map SepsisDocument4 pagesConcept Map SepsisSavanna ChambersNo ratings yet
- Ams 11Document702 pagesAms 11CrazyNo ratings yet
- Nursing Care of PlanDocument16 pagesNursing Care of PlanDbyNo ratings yet
- Professional Development PowerpointDocument12 pagesProfessional Development Powerpointapi-400385739No ratings yet
- CaseStudy CAN2Document4 pagesCaseStudy CAN2Weng RamojalNo ratings yet
- Asthma and COPD NCLEXDocument17 pagesAsthma and COPD NCLEXPotchiee PfizerNo ratings yet
- The Biological Perspective 2Document11 pagesThe Biological Perspective 2Radhey SurveNo ratings yet
- CCD 25132Document3 pagesCCD 25132bharattaneja017023No ratings yet
- q3 Week 3 Stem g11 Genbio Aaron Anicieto DurianDocument13 pagesq3 Week 3 Stem g11 Genbio Aaron Anicieto Durianaaronjeruel100% (1)
- Liberation From Mechanical VentilationDocument21 pagesLiberation From Mechanical VentilationRins Chacko50% (2)
- Urinalysis 2023 08 29T00 - 00 - 00Document1 pageUrinalysis 2023 08 29T00 - 00 - 00Michamiel SerratoNo ratings yet
- Retained Neonatal Reflexes PDFDocument4 pagesRetained Neonatal Reflexes PDFkapczuk0% (1)
- Individual Assignment - SwimmingDocument9 pagesIndividual Assignment - Swimminghaafiz5arisNo ratings yet
- Final Poly 1Document44 pagesFinal Poly 1kimberlyn odoñoNo ratings yet
- Organophosphorus PoisoningDocument15 pagesOrganophosphorus PoisoningtaufiAmaneeNo ratings yet
- Craniofacial Biology Notes Unit 1Document37 pagesCraniofacial Biology Notes Unit 1nohacksNo ratings yet
- Medtronic Physio Control Lifepak 10 DefibrillatorDocument2 pagesMedtronic Physio Control Lifepak 10 DefibrillatorCarlos RomeroNo ratings yet
- Zincum ValerianicumDocument3 pagesZincum ValerianicumKamalNo ratings yet
- Introduction To Clinical Neurology - 2018Document68 pagesIntroduction To Clinical Neurology - 2018Alberto MayorgaNo ratings yet
- DLL - Science 6 - Q2 - W1Document7 pagesDLL - Science 6 - Q2 - W1Kaye Goc-ongNo ratings yet
- Bleuler Psychology PDFDocument666 pagesBleuler Psychology PDFRicardo Jacobsen Gloeckner100% (2)
- Apnea of PrematurityDocument8 pagesApnea of PrematuritypatriaindraNo ratings yet
- The Inorganic Side of Chemical Biology: CommentaryDocument4 pagesThe Inorganic Side of Chemical Biology: CommentarySilloAntonioNo ratings yet
- Residency: Called - To.See - Patient V1.1Document111 pagesResidency: Called - To.See - Patient V1.1Glen OngNo ratings yet
- Pex 05 05Document4 pagesPex 05 05Lesly Castellano50% (2)
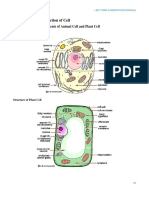
- Cell Types SeDocument16 pagesCell Types SeKendallNo ratings yet
- Genetics in Blood BankingDocument47 pagesGenetics in Blood BankingMandy A. Delfin100% (3)
- 67Document57 pages67Neeruam Ellehcim Aled ZurcNo ratings yet
- 4 - Ditta - BIO173 - Unity of Life - 20204Document13 pages4 - Ditta - BIO173 - Unity of Life - 20204John ChoiNo ratings yet
- PHARMACOLOGYDocument36 pagesPHARMACOLOGYjanr123456100% (1)
- 083 41 Final Biologi T4 DLP-30-60Document31 pages083 41 Final Biologi T4 DLP-30-60Farhan DarwisyNo ratings yet
- Nigel Fong's MRCP NotesDocument66 pagesNigel Fong's MRCP Noteslucas0% (1)
- Dna Replication, Translation, and TranscriptionDocument43 pagesDna Replication, Translation, and TranscriptionMaria VisitacionNo ratings yet
- An Estimation of The Number of Cells in The Human BodyDocument11 pagesAn Estimation of The Number of Cells in The Human BodysedilotNo ratings yet
- Foreign Pharmacy Graduate Equivalency ExaminationDocument26 pagesForeign Pharmacy Graduate Equivalency Examinationnewfakeemail100% (2)
- 86 Normal Low Tension Glaucoma PDFDocument4 pages86 Normal Low Tension Glaucoma PDFSherZalattha KuchikiElfNo ratings yet