Professional Documents
Culture Documents
ANTI HYPERTENSIVE DRUGS
Uploaded by
Gabriella Chafrina0 ratings0% found this document useful (0 votes)
22 views7 pagesA useful classification of these anti hypertensive agents categorizes them according to the principal regulatory site or mechanism on which they act. Diuretics lower blood pressure by depleting the body of sodium and reducing blood volume. Sympathoplegic agents reduce blood pressure by reducing peripheral vascular resistance.
Original Description:
Original Title
GUS4 Antihypertensive Drugs
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentA useful classification of these anti hypertensive agents categorizes them according to the principal regulatory site or mechanism on which they act. Diuretics lower blood pressure by depleting the body of sodium and reducing blood volume. Sympathoplegic agents reduce blood pressure by reducing peripheral vascular resistance.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
22 views7 pagesANTI HYPERTENSIVE DRUGS
Uploaded by
Gabriella ChafrinaA useful classification of these anti hypertensive agents categorizes them according to the principal regulatory site or mechanism on which they act. Diuretics lower blood pressure by depleting the body of sodium and reducing blood volume. Sympathoplegic agents reduce blood pressure by reducing peripheral vascular resistance.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 7
ANTI HYPERTENSIVE DRUGS | Tutorial B-1 GUS
130110110177|Gabriella Chafrina| 05/05/13
A useful classification of these anti
hypertensive agents categorizes them
according to the principal regulatory site or
mechanism on which they act. Because of
their common mechanisms of action, drugs
within each category tend to produce a similar
spectrum of toxicities. The categories include
the following:
1. Diuretics, which lower blood pressure by
depleting the body of sodium and reducing
blood volume and perhaps by other
mechanisms.
2. Sympathoplegic agents, which lower
blood pressure by reducing peripheral
vascular resistance, inhibiting cardiac
function, and increasing venous pooling in
capacitance vessels. (The latter two
effects reduce cardiac output.) These
agents are further subdivided according to
their putative sites of action in the
sympathetic reflex arc (see below).
3. Direct vasodilators, which reduce
pressure by relaxing vascular smooth
muscle, thus dilating resistance vessels
andto varying degreesincreasing
capacitance as well.
4. Agents that block production or action of angiotensin and thereby reduce peripheral vascular
resistance and (potentially) blood volume.
VASODILATORS
- Mechanism and Site of Action
Class of drugs Used for
Oral vasodilators (hydralazine and minoxidil) long-term outpatient therapy of hypertension
Parenteral vasodilators (nitroprusside, diazoxide,
and fenoldopam)
treat hypertensive emergencies
Calcium channel blockers long-term outpatient therapy of hypertension and
treat hypertensive emergencies
Nitrates in angina
ANTI HYPERTENSIVE DRUGS | Tutorial B-1 GUS
130110110177|Gabriella Chafrina| 05/05/13
Vasodilators work best in
combination with other
antihypertensive drugs that oppose
the compensatory cardiovascular
responses
- Drugs
Hydralazine
Hydrazine derivative
Hydralazine + nitrates effective in heart failure
Pharmacokinetic and Dosage
Well absorbed and rapidly metabolized by liver during 1
st
pass, so low bioavailability (+25%) and
variable among individuals
Metabolized in part by acetylation at a rate that appears to be bimodally distributed in the population.
As a consequence, rapid acetylators have greater 1
st
-pass metabolism, lower blood levels, and less
antihypertensive benefit from a given dose than do slow acetylators
Half life: 1.5-3 hours, but vascular effects persist longer than do blood concentrations, possibly due to
avid binding to vascular tissue
Usual dosage ranges from 40 mg/d to 200 mg/d, but higher dosages result in greater vasodilation and
may be used if necessary
Dosing two or three times daily provides smooth control of blood pressure
Toxicity
Most common adverse effects: headache, nausea, anorexia, palpitations, sweating, and flushing
In patients with ischemic heart disease, reflex tachycardia and sympathetic stimulation may provoke
angina or ischemic arrhythmias
Dosages of 400 mg/d or more, there is a 1020% incidencechiefly in persons who slowly acetylate
the drugof a syndrome characterized by arthralgia, myalgia, skin rashes, and fever that resembles
lupus erythematosus
ANTI HYPERTENSIVE DRUGS | Tutorial B-1 GUS
130110110177|Gabriella Chafrina| 05/05/13
Minoxidil
Efficacious orally active vasodilator
Minoxidil sulfate (the active metabolite) cause opening of potassium channels in
smooth muscle membranes Increased potassium permeability stabilizes
the membrane at its resting potential and makes contraction less likely
Dilates arterioles but not veins
Minoxidil can replaced hydralazine in patients with renal failure and severe
hypertension, who do not respond well to hydralazine
Pharmacokinetics and Dosage
Associated with reflex sympathetic stimulation and sodium and fluid retention
Must be used in combination with a blocker and a loop diuretic
Toxicity
Tachycardia, palpitations, angina, and edema are observed when doses of blockers and diuretics are
inadequate
Headache, sweating, and hypertrichosis are relatively common
Topical minoxidil (as Rogaine) is used as a stimulant to hair growth for correction of baldness
Sodium nitroprusside
Powerful parenterally administered vasodilator that is used in treating
hypertensive emergencies as well as severe heart failure
dilates both arterial and venous vessels, resulting in reduced peripheral
vascular resistance and venous return
activation of guanylyl cyclase (either via release of nitric oxide or by
direct stimulation of the enzyme) increased intracellular cGMP
relaxes vascular smooth muscle
Pharmacokinetics and Dosage
Nitroprusside: complex of iron, cyanide groups, and a nitroso moiety
rapidly metabolized by uptake into red blood cells with liberation of cyanide. Cyanide in turn is
metabolized by the mitochondrial enzyme rhodanase, in the presence of a sulfur donor, to the less
toxic thiocyanate. Thiocyanate is distributed in extracellular fluid and slowly eliminated by the kidney
rapidly lowers blood pressure, and its effects disappear within 110 minutes after discontinuation
given by intravenous infusion and should be changed after several hours
in aqueous solution is sensitive to light and must therefore be made up fresh before each
administration and covered with opaque foil
Dosage typically begins at 0.5 mcg/kg/min and may be increased up to 10 mcg/kg/min as necessary to
control blood pressure
Toxicity
Most common: excessive blood pressure lowering
Most serious: accumulation of cyanide, metabolic acidosis, arrhythmias, excessive hypotension, and
death
ANTI HYPERTENSIVE DRUGS | Tutorial B-1 GUS
130110110177|Gabriella Chafrina| 05/05/13
Diazoxide
An and relatively long-acting parenterally administered arteriolar dilator
that is occasionally used to treat hypertensive emergencies
Effect: rapid fall in systemic vascular resistance and mean arterial blood
pressure associated with substantial tachycardia and increase in cardiac
output and prevents vascular smooth muscle contraction by opening
potassium channels and stabilizing the membrane potential at the resting
level
Pharmacokinetics and Dosage
Similar chemically to the thiazide diuretics but has no diuretic activity
Bound extensively to serum albumin and to vascular tissue
Partially metabolized, metabolic pathways are not well characterized
The remainder is excreted unchanged
Half life: approx. 24 hours, but the relationship between blood concentration and hypotensive action is
not well established
The blood pressure-lowering effect after a rapid injection is established within 5 minutes and lasts for
412 hours
Toxicity
Most significant: excessive hypotension, resulting from the recommendation to use a fixed dose of 300
mg in all patients
Hypotension has resulted in stroke and myocardial infarction
Diazoxide inhibits insulin release from the pancreas (probably by opening potassium channels in the
beta cell membrane) and is used to treat hypoglycemia secondary to insulinoma hyperglycemia
complicates diazoxide use, particularly in persons with renal insufficiency
Rarely caused renal salt and water retention
Fenoldopam
A peripheral arteriolar dilator used for hypertensive emergencies and postoperative
hypertension
Acts primarily as an agonist of dopamine D
1
receptors, resulting in dilation of peripheral
arteries and natriuresis
Pharmacokinetics and Dosage
Rapidly metabolized, primarily by conjugation
Half life: 10 minutes
Administered by continuous IV infusion
Initiated at a low dosage (0.1 mcg/kg/min), and the dose is then titrated upward every 15 or 20
minutes to a maximum dose of 1.6 mcg/kg/min or until the desired blood pressure reduction is
achieved
Toxicity
Major toxicities: reflex tachycardia, headache, and flushing
Cause increases intraocular pressure
Calcium Channel Blockers
Have antianginal effects, antiarrhythmic effects, and reduce peripheral resistance and blood pressure
Verapamil, diltiazem, and the dihydropyridine family (amlodipine, felodipine, isradipine, nicardipine,
nifedipine, and nisoldipine) are all equally effective in lowering blood pressure
Clevidipine is a newer member of this group that is formulated for intravenous use only
Hemodynamic differences among calcium channel blockers may influence the choice of a
particular agent
ANTI HYPERTENSIVE DRUGS | Tutorial B-1 GUS
130110110177|Gabriella Chafrina| 05/05/13
Nifedipine and the other dihydropyridine agents are more selective as vasodilators and have less
cardiac depressant effect than verapamil and diltiazem
Reflex sympathetic activation with slight tachycardia maintains or increases cardiac output in most
patients given dihydropyridines
Verapamil has the greatest depressant effect on the heart and may decrease heart rate and cardiac
output
Diltiazem has intermediate actions
Intravenous nicardipine and clevidipine are available for the treatment of hypertension when oral
therapy is not feasible; parenteral verapamil and diltiazem can also be used for the same indication
Nicardipine is typically infused at rates of 215 mg/h. Clevidipine is infused starting at 12 mg/h and
progressing to 46 mg/h
Oral short-acting nifedipine has been used in emergency management of severe hypertension
INHIBITORS OF ANGIOTENSIN
- Renin, angiotensin, and aldosterone play important roles in at least some people with essential
hypertension
- Approximately 20% of patients with essential hypertension have inappropriately low and 20% have
inappropriately high plasma renin activity
- Mechanism and Sites of Action
Renin release from the kidney cortex is stimulated by reduced renal arterial pressure, sympathetic
neural stimulation, and reduced sodium delivery or increased sodium concentration at the distal
renal tubule
Renin acts upon angiotensinogen to split off the inactive precursor decapeptide angiotensin I
Angiotensin I is then converted, primarily by endothelial ACE, to the arterial vasoconstrictor
octapeptide angiotensin II angiotensin II which is in turn converted in the adrenal gland to
angiotensin III Angiotensin II and III both stimulate aldosterone release
Angiotensin II has vasoconstrictor and sodium-retaining activity
Angiotensin may contribute to maintaining high vascular resistance in hypertensive states
associated with high plasma renin activity, such as renal arterial stenosis, some types of intrinsic
renal disease, and malignanthypertension, as well as in essential hypertension after treatment with
sodium restriction, diuretics, or vasodilators
ANTI HYPERTENSIVE DRUGS | Tutorial B-1 GUS
130110110177|Gabriella Chafrina| 05/05/13
A parallel system for angiotensin generation exists in several other tissues (eg, heart) and may be
responsible for trophic changes such as cardiac hypertrophy
The converting enzyme involved in tissue angiotensin II synthesis is also inhibited by ACE inhibitors
Three classes of drugs act specifically on the renin-angiotensin system:
ACE inhibitors; the competitive inhibitors of angiotensin at its receptors, including losartan and other
nonpeptide antagonists; and aliskiren, an orally active renin antagonist
A fourth group of drugs, the aldosterone receptor inhibitors eg, spironolactone, eplerenone)
-blockers, can reduce renin secretion
Angiotensin-Converting Enzyme (ACE) Inhibitors
Captopril and other drugs in this class inhibit the converting enzyme peptidyl dipeptidase that hydrolyzes
angiotensin I to angiotensin II and (under the name plasma kininase) inactivates bradykinin, a potent
vasodilator, which works at least in part by stimulating release of nitric oxide and prostacyclin
The hypotensive activity of captopril results both from an inhibitory action on the renin-angiotensin system
and a stimulating action on the kallikrein-kinin system
Bradykinin receptor antagonist, icatibant, blunts the blood pressure-lowering effect of captopril
Enalapril is an oral prodrug that is converted by hydrolysis to a converting enzyme inhibitor, enalaprilat,
with effects similar to those of captopril
Enalaprilat itself is available only for intravenous use, primarily for hypertensive emergencies
Lisinopril is a lysine derivative of enalaprilat. Benazepril, fosinopril, moexipril, perindopril, quinapril,
ramipril, and trandolapril are other long-acting members of the class. All are prodrugs, like enalapril, and
are converted to the active agents by hydrolysis, primarily in the liver
Angiotensin II inhibitors lower blood pressure principally by decreasing peripheral vascular resistance.
These agents do not result in reflex sympathetic activation may be due to downward resetting of the
baroreceptors or to enhanced parasympathetic activity
ACE inhibitors have a particularly useful role in treating patients with chronic kidney disease because they
diminish proteinuria and stabilize renal function
ACE inhibitors have also proved to be extremely useful in the treatment of heart failure, and after
myocardial infarction, and there is recent evidence that ACE inhibitors reduce the incidence of diabetes in
patients with high cardiovascular risk
Pharmacokinetics and Dosage
Captopril
Enalapril:
Peak concentrations of enalaprilat, the active metabolite of enalapril, occur 34 hours after dosing
with enalapril
Half life: 11 hours
Typical doses of enalapril are 1020 mg once or twice daily
Lisinopril
Half life: 12 hours
Doses of 1080 mg once daily are effective in most patients
All of the ACE inhibitors except fosinopril and moexipril are eliminated primarily by the kidneys; doses
of these drugs should be reduced in patients with renal insufficiency
Toxicity
Severe hypotension can occur after initial doses of any ACE inhibitor in patients who are hypovolemic
as a result of diuretics, salt restriction, or gastrointestinal fluid loss
Other adverse effects common to all ACE inhibitors include acute renal failure (particularly in patients
with bilateral renal artery stenosis or stenosis of the renal artery of a solitary kidney), hyperkalemia,
dry cough sometimes accompanied by wheezing, and angioedema
ANTI HYPERTENSIVE DRUGS | Tutorial B-1 GUS
130110110177|Gabriella Chafrina| 05/05/13
Hyperkalemia is more likely to occur in patients with renal insufficiency or diabetes
ACE inhibitors are contraindicated during the second and third trimesters of pregnancy because of the
risk of fetal hypotension, anuria, and renal failure, sometimes associated with fetal malformations or
death
Captopril, particularly when given in high doses to patients with renal insufficiency, may cause
neutropenia or proteinuria. Minor toxic effects seen more typically include altered sense of taste,
allergic skin rashes, and drug fever, which may occur in up to 10% of patients
Important drug interactions include those with potassium supplements or potassium-sparing diuretics,
which can result in hyperkalemia
Nonsteroidal anti-inflammatory drugs may impair the hypotensive effects of ACE inhibitors by blocking
bradykinin-mediated vasodilation, which is at least in part, prostaglandin mediated
Angiotensin ReceptorBlocking Agents
Losartan and valsartan were the first marketed blockers of the angiotensin II type 1 (AT1) receptor
Candesartan, eprosartan, irbesartan,telmisartan, and olmesartan have no effect on bradykinin metabolism
and are therefore more selective blockers of angiotensin effects than ACE inhibitors and have the
potential for more complete inhibition of angiotensin action compared with ACE inhibitors because there
are enzymes other than ACE that are capable of generating angiotensin II
Angiotensin receptor blockers provide benefits similar to those of ACE inhibitors in patients with heart
failure and chronic kidney disease
Pharmacokinetics and Dosage
Toxicity
Similar to ACE inhibitors, including the hazard of use during pregnancy
You might also like
- Drug Recipes IndexDocument72 pagesDrug Recipes IndexEka Kusyanto50% (4)
- Pharmacology 3 - Management of Heart FailureDocument59 pagesPharmacology 3 - Management of Heart Failurealbatros000No ratings yet
- Drugs For Congestive Heart FailureDocument46 pagesDrugs For Congestive Heart Failuresultan khabeeb100% (1)
- Vasoconstrictors & VasodilatorsDocument37 pagesVasoconstrictors & VasodilatorsDrVarun Menon100% (1)
- Vasodilators by Hiren PatelDocument28 pagesVasodilators by Hiren PatelHiren_Patel_2427No ratings yet
- 1 Drugs For HypertensionDocument62 pages1 Drugs For HypertensionSaniNo ratings yet
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Preps 4-61Document57 pagesPreps 4-61fianaNo ratings yet
- ObjectionableDocument9 pagesObjectionabledmtalbhogeNo ratings yet
- Business Plan To Start An Online Pharmacy BusinessDocument32 pagesBusiness Plan To Start An Online Pharmacy BusinessDiriba Alemu100% (1)
- Antihypertensive DrugsDocument37 pagesAntihypertensive Drugsleiann_jessicaNo ratings yet
- Capital Budgeting Hetero DrugsDocument100 pagesCapital Budgeting Hetero DrugsDasari Anilkumar100% (1)
- Vasodilators 1233318450814478 3Document29 pagesVasodilators 1233318450814478 3Nehal AmjadNo ratings yet
- Friabilator Operation Cleaning Handling Standard Operating ProcedureDocument8 pagesFriabilator Operation Cleaning Handling Standard Operating ProcedureKumar Galipelly100% (1)
- Foreign Body EarDocument34 pagesForeign Body EarGabriella ChafrinaNo ratings yet
- 8D - HypertensionDocument58 pages8D - Hypertensionmashe1No ratings yet
- Cardiotronic MedicationsDocument13 pagesCardiotronic MedicationsTee WoodNo ratings yet
- Calcium Channel Blockers: Mechanisms, Types, Uses & Side EffectsDocument6 pagesCalcium Channel Blockers: Mechanisms, Types, Uses & Side EffectsManyal Kutin KoakNo ratings yet
- Managing Hypertension with Drug TherapyDocument39 pagesManaging Hypertension with Drug TherapykiranstNo ratings yet
- Cardiovascular PharmacologyDocument61 pagesCardiovascular PharmacologyTeeOne920% (1)
- Thiazide and Thiazide-Like DiureticsDocument3 pagesThiazide and Thiazide-Like DiureticsYohanes SutrisnoNo ratings yet
- Cardiovascular System Pharmacology: Pharmacology Ii DR E KeziaDocument15 pagesCardiovascular System Pharmacology: Pharmacology Ii DR E KeziaJohnNo ratings yet
- Emergency Cardiac Medications for ArrhythmiasDocument14 pagesEmergency Cardiac Medications for ArrhythmiasRomzy BasañesNo ratings yet
- Anti Hypertensive 20191211Document35 pagesAnti Hypertensive 20191211helloitsmenadNo ratings yet
- Cardiac ArrhythmiaDocument101 pagesCardiac ArrhythmiaYuvraj ChauhanNo ratings yet
- عرض تقديمي2Document18 pagesعرض تقديمي2Sabrina ShalhoutNo ratings yet
- HTN EmergencyDocument11 pagesHTN EmergencyKaran ChhabraNo ratings yet
- Antihypertensive AgentsDocument52 pagesAntihypertensive Agentssameena ramzanNo ratings yet
- Heat Failure DrugsDocument8 pagesHeat Failure DrugsDaniel MwiluNo ratings yet
- Skema HipertensiDocument4 pagesSkema HipertensiAndri wijayaNo ratings yet
- Cardiotonic DrugsDocument67 pagesCardiotonic DrugsLady Mae Ramos100% (1)
- Hypertensive Emergencies: BY: Dr. Imtiyaz Hashim (PGR) Dr. Khalida Baloch (Ho)Document31 pagesHypertensive Emergencies: BY: Dr. Imtiyaz Hashim (PGR) Dr. Khalida Baloch (Ho)امتیاز ہاشم بزنجوNo ratings yet
- CVS PharmacologyDocument60 pagesCVS PharmacologyGølà Sèèñàà–baale irraaNo ratings yet
- 1 Antihypertensive DrugsDocument14 pages1 Antihypertensive DrugsReda SoNo ratings yet
- 2nd - Semester.lecture 3.1-Drugs Used in HypertensionDocument40 pages2nd - Semester.lecture 3.1-Drugs Used in HypertensionToader SilviaNo ratings yet
- Obat Yang Bekerja Pada Sistem KardiovaskulerDocument18 pagesObat Yang Bekerja Pada Sistem KardiovaskulerMuhammad IkbalNo ratings yet
- HCL Clonipress: 75 MCG & 150 MCG TabletDocument1 pageHCL Clonipress: 75 MCG & 150 MCG TabletShyden Taghap Billones BordaNo ratings yet
- Emergency Drugs Review: Oxygen, Epinephrine, Atropine and MoreDocument71 pagesEmergency Drugs Review: Oxygen, Epinephrine, Atropine and Moredodong skyroseNo ratings yet
- Anti HypertensionDocument62 pagesAnti HypertensionHazazi Jr Love LoverpoolNo ratings yet
- Journal 3 Diuretic in Heart FailureDocument6 pagesJournal 3 Diuretic in Heart FailureClara Nur RamadhaniNo ratings yet
- 10-11 Treatment of HypertensionDocument11 pages10-11 Treatment of HypertensionHanif GandohNo ratings yet
- Pharm CH 11 AntihypertensivesDocument42 pagesPharm CH 11 AntihypertensivesDaniel AdamsNo ratings yet
- FARMAKOGNOSI - Obat AntihipertensiDocument7 pagesFARMAKOGNOSI - Obat AntihipertensiTrianisa FebyNo ratings yet
- Antihypertensive Drugs ٠١١٦٥٨Document10 pagesAntihypertensive Drugs ٠١١٦٥٨mohnad806mNo ratings yet
- Bihs PDFDocument4 pagesBihs PDFFredrikus Lay Berkh MansNo ratings yet
- Review of Advancements in Heart Failure 81220Document65 pagesReview of Advancements in Heart Failure 81220Dr MustafaNo ratings yet
- Antihypertension: Prajogo WibowoDocument45 pagesAntihypertension: Prajogo WibowoDesti Ratna PutriNo ratings yet
- NCP and DSDocument6 pagesNCP and DSfranzcatchie100% (1)
- Heart Failure and DHF PDFDocument31 pagesHeart Failure and DHF PDFMahamed Wefkey OmranNo ratings yet
- Ecart For PrintingDocument10 pagesEcart For PrintingbluennaNo ratings yet
- Anti Hypertensive Drugs .Document6 pagesAnti Hypertensive Drugs .Baqir BroNo ratings yet
- Spironolactone: Generic Name Brand Name ClassificationDocument5 pagesSpironolactone: Generic Name Brand Name ClassificationShermalyn SalahuddinNo ratings yet
- Prepared By: Shukri Yusuf ElmiDocument17 pagesPrepared By: Shukri Yusuf ElmiabdishakurNo ratings yet
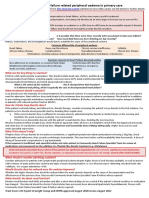
- Heart Failure Managing HF Related Peripheral Oedema in Primary CareDocument1 pageHeart Failure Managing HF Related Peripheral Oedema in Primary CareParth VinaypatilNo ratings yet
- Drugs Affecting The Cardiovascular System (Antihypertensive - Part-1)Document6 pagesDrugs Affecting The Cardiovascular System (Antihypertensive - Part-1)alialahmedy24No ratings yet
- PEDRIATICDocument17 pagesPEDRIATICMaxxdlc 16No ratings yet
- Faculty of Physical TherapyDocument15 pagesFaculty of Physical TherapyDr Abdallah BahaaNo ratings yet
- Congestive Heart FailureDocument25 pagesCongestive Heart Failureemman122392No ratings yet
- Diuretics in The Treatment of Hypertension: Michael E. Ernst, Pharmd, and Samuel J. Mann, MDDocument8 pagesDiuretics in The Treatment of Hypertension: Michael E. Ernst, Pharmd, and Samuel J. Mann, MDWawan NNo ratings yet
- 7,8 - Antihypertensive DrugsDocument10 pages7,8 - Antihypertensive DrugsHusniya MehamedNo ratings yet
- Generic NameDocument8 pagesGeneric NameRosaree Mae PantojaNo ratings yet
- LECTURE 8 AntihypertensiveDocument18 pagesLECTURE 8 AntihypertensiveanaNo ratings yet
- PharmaDocument8 pagesPharma2022105340No ratings yet
- Lecture 24-25 - Antihypertensive AgentsDocument30 pagesLecture 24-25 - Antihypertensive AgentsJedoNo ratings yet
- Heart Failure: Causes, Treatments, and Dental ImplicationsDocument8 pagesHeart Failure: Causes, Treatments, and Dental Implicationsمحمد علي حميدNo ratings yet
- Pathogenesis of LeprosyDocument13 pagesPathogenesis of LeprosyNurul AinNo ratings yet
- Soal Mde Tropmed 2007Document4 pagesSoal Mde Tropmed 2007Gabriella ChafrinaNo ratings yet
- Cvs4-Clinical Aspects of Serum Cholesterol LevelDocument2 pagesCvs4-Clinical Aspects of Serum Cholesterol LevelGabriella ChafrinaNo ratings yet
- ECG Arrhythmia GraphsDocument3 pagesECG Arrhythmia GraphsGabriella ChafrinaNo ratings yet
- Rs6 Extrapulmonary TuberculosisDocument4 pagesRs6 Extrapulmonary TuberculosisGabriella ChafrinaNo ratings yet
- RS7 InfluenzaDocument6 pagesRS7 InfluenzaGabriella ChafrinaNo ratings yet
- TM3-Diagnosis and DD of MalariaDocument3 pagesTM3-Diagnosis and DD of MalariaGabriella ChafrinaNo ratings yet
- Rs6-Cervical Lymph NodeDocument6 pagesRs6-Cervical Lymph NodeGabriella ChafrinaNo ratings yet
- Lab PharmacologyDocument2 pagesLab PharmacologyGabriella ChafrinaNo ratings yet
- Rs6 Pleural TuberculosisDocument5 pagesRs6 Pleural TuberculosisGabriella ChafrinaNo ratings yet
- RS7-Acid Base BalanceDocument4 pagesRS7-Acid Base BalanceGabriella ChafrinaNo ratings yet
- RS5 PiDocument9 pagesRS5 PiGabriella ChafrinaNo ratings yet
- Rs4-Gas Exchange and TransportDocument5 pagesRs4-Gas Exchange and TransportGabriella ChafrinaNo ratings yet
- Rs4 Phop CRPDocument2 pagesRs4 Phop CRPGabriella ChafrinaNo ratings yet
- RS3 PiDocument5 pagesRS3 PiGabriella ChafrinaNo ratings yet
- Iccu (Tachycardia) : - Tutorial D-1 CVSDocument2 pagesIccu (Tachycardia) : - Tutorial D-1 CVSGabriella ChafrinaNo ratings yet
- RS5-Defense Mech of LungDocument3 pagesRS5-Defense Mech of LungGabriella ChafrinaNo ratings yet
- Macroscopic Hematuria GuideDocument3 pagesMacroscopic Hematuria GuideGabriella ChafrinaNo ratings yet
- RS1 ManagementDocument3 pagesRS1 ManagementGabriella ChafrinaNo ratings yet
- Group A Β-Hemolytic Streptococcus: - Tutorial B-1 RSDocument2 pagesGroup A Β-Hemolytic Streptococcus: - Tutorial B-1 RSGabriella ChafrinaNo ratings yet
- Iccu (Tachycardia) : - Tutorial D-1 CVSDocument2 pagesIccu (Tachycardia) : - Tutorial D-1 CVSGabriella ChafrinaNo ratings yet
- CVS5-Conduction of Cardiac Action PotentialsDocument1 pageCVS5-Conduction of Cardiac Action PotentialsGabriella ChafrinaNo ratings yet
- Lab PharmacologyDocument2 pagesLab PharmacologyGabriella ChafrinaNo ratings yet
- Deep Vein Thrombosis (DVT) : - Tutorial D-1 CVSDocument1 pageDeep Vein Thrombosis (DVT) : - Tutorial D-1 CVSGabriella ChafrinaNo ratings yet
- CVS6 Heart SoundsDocument3 pagesCVS6 Heart SoundsGabriella ChafrinaNo ratings yet
- CVS6 Page InterpretationDocument2 pagesCVS6 Page InterpretationGabriella ChafrinaNo ratings yet
- Advanced Life Support Algorithm GuideDocument1 pageAdvanced Life Support Algorithm GuideGabriella ChafrinaNo ratings yet
- Advance Life Support (American Heart Association 2010) : - Tutorial D-1 CVSDocument1 pageAdvance Life Support (American Heart Association 2010) : - Tutorial D-1 CVSGabriella ChafrinaNo ratings yet
- List of high alert medications at Husada HospitalDocument5 pagesList of high alert medications at Husada HospitalCHRISTINE EriskaNo ratings yet
- Antibiotics in OMFSDocument20 pagesAntibiotics in OMFSAmit GaurNo ratings yet
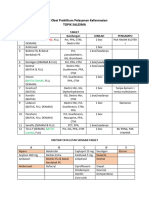
- Daftar Obat Praktikum Pelayanan Kefarmasian OretDocument4 pagesDaftar Obat Praktikum Pelayanan Kefarmasian OretRiza AsariNo ratings yet
- 5.1.4. Microbiological Quality of Non-Sterile Pharmaceutical Preparations and Substances For Pharmaceutical UseDocument1 page5.1.4. Microbiological Quality of Non-Sterile Pharmaceutical Preparations and Substances For Pharmaceutical UseCik ApaiNo ratings yet
- Medicine List by AmirDocument39 pagesMedicine List by AmirNomAn JuTtNo ratings yet
- Diabetic Foot Infections: by Scott Bergman, Pharm.D., BCPS-AQ ID and Punit J. Shah, Pharm.D., BCPSDocument20 pagesDiabetic Foot Infections: by Scott Bergman, Pharm.D., BCPS-AQ ID and Punit J. Shah, Pharm.D., BCPSPrashant LokhandeNo ratings yet
- Harga Prolanis (Data Dari Apotek Online)Document74 pagesHarga Prolanis (Data Dari Apotek Online)Orin Tri WulanNo ratings yet
- Tablet and CapsulesDocument101 pagesTablet and CapsulesTamer HassanNo ratings yet
- Cipla General Overview & SWOT AnalysisDocument5 pagesCipla General Overview & SWOT Analysisakanksha morghadeNo ratings yet
- AN ALTERNATIVE TO CODEINE AND HYDROCODONE - Management of Persistent CoughDocument2 pagesAN ALTERNATIVE TO CODEINE AND HYDROCODONE - Management of Persistent CoughAnna LiachenkoNo ratings yet
- NemeraDocument5 pagesNemeraFransisca FortunataNo ratings yet
- Hilton - Maher - SeltoDocument21 pagesHilton - Maher - Seltoareep94No ratings yet
- IT 10 - Farmakologi Obat - Obat Di Bidang Endokrin - TEODocument34 pagesIT 10 - Farmakologi Obat - Obat Di Bidang Endokrin - TEOtattosssNo ratings yet
- CephalexinDocument4 pagesCephalexinCHIEF DOCTOR MUTHUNo ratings yet
- Maharashtra Board Pharmacology Model AnswerDocument19 pagesMaharashtra Board Pharmacology Model AnswerJyoti MangtaniNo ratings yet
- 16 10 25 Decarboxylation of THCA To Active THC PDFDocument3 pages16 10 25 Decarboxylation of THCA To Active THC PDFRafael Ignacio Leal QuijónNo ratings yet
- Alims - Approved Terminology - Routes and Methods of Administration - October 2014Document2 pagesAlims - Approved Terminology - Routes and Methods of Administration - October 2014Katarina R.M.No ratings yet
- Chapter 1. Intro To DrugsDocument10 pagesChapter 1. Intro To DrugsLyka Milo AvilaNo ratings yet
- Jujube FruitDocument5 pagesJujube FruitnasmiNo ratings yet
- Gina Shenoda, BS, MBADocument3 pagesGina Shenoda, BS, MBACristian RamirezNo ratings yet
- Brain O MaticDocument5 pagesBrain O MaticshemoomiNo ratings yet
- Lozenges Troches Sticks and SuppositoriesDocument21 pagesLozenges Troches Sticks and SuppositoriesABC.DEFNo ratings yet
- Clinical Pharmacology and Clinical PharmacyDocument8 pagesClinical Pharmacology and Clinical PharmacyRowena Concepcion Penafiel100% (1)
- Phytochemical and Antibacterial Studies On Peperomia Pellucida (L.) H.B.KDocument3 pagesPhytochemical and Antibacterial Studies On Peperomia Pellucida (L.) H.B.KSonia Virgawati PratiwiNo ratings yet