Professional Documents
Culture Documents
RS5 Pi
Uploaded by
Gabriella Chafrina0 ratings0% found this document useful (0 votes)
30 views9 pagesDYSPNEA Definition: Breathlessness or shortness of breath, difficult or labored breathing. Usually attributed to congestive heart failure with pulmonary edema and sometimes in patients with chronic pulmonary disease. Common causes of dyspnea: a) Upper airway: foreign body / mass, allergic reaction, airway stenosis, pulmonary embolism, interstitial lung disease, COPD, asthma, mass.
Original Description:
Original Title
RS5-PI
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDYSPNEA Definition: Breathlessness or shortness of breath, difficult or labored breathing. Usually attributed to congestive heart failure with pulmonary edema and sometimes in patients with chronic pulmonary disease. Common causes of dyspnea: a) Upper airway: foreign body / mass, allergic reaction, airway stenosis, pulmonary embolism, interstitial lung disease, COPD, asthma, mass.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
30 views9 pagesRS5 Pi
Uploaded by
Gabriella ChafrinaDYSPNEA Definition: Breathlessness or shortness of breath, difficult or labored breathing. Usually attributed to congestive heart failure with pulmonary edema and sometimes in patients with chronic pulmonary disease. Common causes of dyspnea: a) Upper airway: foreign body / mass, allergic reaction, airway stenosis, pulmonary embolism, interstitial lung disease, COPD, asthma, mass.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 9
PAGE INTERPRETATION (CASE 5)| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 27/11/13
DYSPNEA
Definition: Breathlessness or shortness of breath, difficult or labored breathing
Types of dyspnea:
a) Dyspnea on exertion: dyspnea provoked by physical effort or exertion
b) Cardiac dyspnea: caused by cardiac disease
c) Expiratory dyspnea: caused by hindrance to the free exhalation of air from lungs
d) Inspiratory dyspnea: caused by hindrance to the free inhalation of air into lungs
e) Functional dyspnea: often associated into anxiety status
f) Nocturnal dyspnea: minimal in the morning and gradually and become severe at night
g) Non-expansional dyspnea: caused by inadequate expansion of chest
h) Paroxysmal nocturnal dyspnea: respiratory distress that awakens patients from sleep and is
related to posture. Usually attributed to congestive heart failure with pulmonary edema and
sometimes in patients with chronic pulmonary disease
i) Orthostatic dyspnea: occurs in erect position
j) Renal dyspnea: anemia/volume overload associated with kidney disease
Common causes of dyspnea:
a) Upper airway: foreign body/mass, allergic reaction, airway stenosis, tracheomalacia
b) Lung/lower airway: pneumonia, pneumothorax, pleural effusion, pulmonary embolism,
pulmonary hypertension, interstitial lung disease, adult respiratory distress syndrome, COPD,
asthma, mass
c) Cardiac: myocardial ischemia, CHF, pericardial effusion, valvular disease, arrhythmia
d) Metabolic/hematologic: Thyrotoxicosis, Hb abnormality, anemia, disorder of phosphate/K
+
/Ca
2+
,
sepsis/fever, acidosis
e) Neuromuscular: GBS, myasthenia gravis, myopathy, neuropathy
f) Psychogenic: panic disorder, hyperventilation, deconditioning
g) Massive ascites
h) Drug withdrawal
Mechanism of dyspnea in chronic obstructive
pulmonary disease (COPD). Airways narrow on
expiration but, in normal individuals, the elasticized
alveolar attachments prevent closure so the alveoli
empty. In COPD there is a loss of elastin fibers as a
result of elastases, which means that even in mild
COPD small airways close to a greater extent. As
COPD becomes more severe, the thickness of small
airways increases and alveolar attachments may be
disrupted so that a peripheral airway may close
during expiration, which results in air trapping and
hyperinflation that leads to dyspnea and a reduced
exercise capacity
PAGE INTERPRETATION (CASE 5)| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 27/11/13
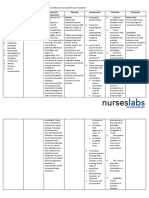
COUGH Adult (chronic)
DIAGNOSTIC ISSUES HISTORY PHYSICAL EXAM
Cigarette smoking Minimal sputum Usually normal but eventually leads
to abnormalities
Chronic lung disease
(chronic bronchitis and
emphysema)
Dyspnea; cough and sputum production
tend to be wose after arising from sleep.
Patient is usually a heavy cigarette smoker
or has had chronic exposure to industrial
dusts
Hyperresonant lung fields, distant
breath sounds, scattered rhonchi or
wheezes, prolonged expiration
Secondary to medication Captopril or other angiotensin converting
enzyme inhibitor; beta-blockers may
aggravate an asthmatic cough
Normal
Gastrointestinal reflux Heartburn occasionally noted Normal exam
Psychogenic Mostly in daytime Barking, loud cough; normal exam
Lung tumor Change in cough pattern. Hemoptysis and
chest ache may occur. Patient is usually a
cigarette smoker
Usually normal. Enlarged
supraclavicular nodes may be
palpated
Tuberculosis Fever, night sweats, weight loss; chronic
cough and occasional hemoptysis. Some
patients note a recent exposure to active
tuberculosis or a history of a positive
tuberculin test
Exam is usually normal; apical
rales/crackles, weight loss, and fever
may be present
Congestive heart failure or
mitral stenosis
Nocturnal coughing, orthopnea, dyspnea,
paroxysmal nocturnal dyspnea
Moist rales/crackles at both bases;
ankle edema. Heart exam may
reveal an S
3
gallop, a diastolic
murmur, or a loud pulmonic
component of the second heart
sound
SPUTUM
Also called mucus or phlegm, is a protective substance produced by the lungs to aid in the trapping and
removal of foreign particles. It is expelled by coughing or clearing of the throat. Patients with COPD
usually produce small amounts of tenacious sputum when they cough. A copious amount of thick
sputum is often associated with a bacterial lung infection, which can exacerbate COPD symptoms. The
color and consistency of sputum may change when a bacterial infection is present.
1. Bloody (Hemoptysis)
1. blood-streaked sputum - inflammation of throat, bronchi; lung cancer;
2. Pink sputum - sputum evenly mixed with blood, from alveoli, small bronchi;
3. massive blood - cavitary tuberculosis of lung, lung abscess, bronchiectasis, infarction, embolism.
2. Rusty colored - usually caused by pneumococcal bacteria (in pneumonia)
3. Purulent - containing pus. The colour can provide hints as to effective treatment in Chronic
Bronchitis Patients:
1. a yellow-greenish (mucopurulent) color suggests that treatment with antibiotics can reduce
symptoms. Green color is caused by Neutrophil Myeloperoxidase
2. a white, milky, or opaque (mucoid) appearance often means that antibiotics will be ineffective in
treating symptoms. (This information may correlate with the presence of bacterial or viral
infections, though current research does not support that generalization)
4. Foamy white - may come from obstruction or even edema.
5. Frothy pink - pulmonary edema
PAGE INTERPRETATION (CASE 5)| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 27/11/13
AMINOPHYLLINE
SALBUTAMOL
FUROSEMIDE
BMI
In our patient: BMI = 48/((1.65)
2
) = 17.63
From WHO 2000 BMI and Protein Energy Malnutrition (PEM) Category
BMI Grade
<16 Grade III PEM
16.0-16.9 Grade II PEM
17.0-18.5 Grade I PEM (Underweight)
18.5-24.9 Normal
25.0-29.9 Overweight
30.0-34.9 Class I Obese
35.0-39.9 Class II Obese
>40 Class III Severe Obesity
PAGE INTERPRETATION (CASE 5)| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 27/11/13
VITAL SIGN (ADULT)
BLOOD PRESSURE
CATEGORY SYSTOLIC (mmHg) DIASTOLIC (mmHg)
HYPERTENSION
STAGE 3 (SEVERE) >180 >110
STAGE 2 (MODERATE) 160-179 100-109
STAGE 1 (MILD) 140-159 90-99
HIGH NORMAL 130-139 85-59
NORMAL <130 <85
OPTIMAL <120 <80
HEART AND PULSE RATE TEMPERATURE RESPIRATORY RATE
Normal: 60-100 beats/minute Normal: 36.5-37.5
o
C Normal: 16-24 breath/minute
PROLONGED EXPIRATION
Respiratory condition wherein there is an increase in the expiratory time of a person compared to the
inspiratory time which is often characterized by a person's difficulty in breathing.
In COPD, expiration is prolonged as the patient forces his breath out through obstructed airways
PURSED LIPS BREATHING
The act of exhaling through tightly pressed,
pursed lips. Doctors and respiratory
therapists teach the technique to their
patients to ease shortness of breath and to
promote deep breathing, also referred to as
abdominal or diaphragmatic breathing. The
purpose of PLB is to create back-pressure
inside airways to splint them open; moving
air thus then takes less work.
Spontaneous breathing through pursed lips,
especially after physical exercise, is also one
of the signs that health workers use to
detect possible chronic obstructive
pulmonary disease (COPD) in patients.
Some therapists say that using PLB has
positive effects in treating stress and anxiety related disorders.
JUGULAR VENOUS PRESSURE
A. Normal: 4 cm or less
B. Increased >4 cm (Jugular Venous Distention)
1. Right-sided Heart Failure (most common)
a. Increased right atrial pressure
2. Constrictive Pericarditis
3. Tricuspid stenosis
4. Superior Vena Cava Obstruction
5. Valsalva phenomenon (laughing, coughing)
PAGE INTERPRETATION (CASE 5)| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 27/11/13
BARREL SHAPED CHEST
- Increase in the anterior posterior diameter of the
chest wall resembling the shape of a barrel, most
often associated with emphysema
- Characteristic: round and bulging chest, large ribcage,
very round torso, large lung capacity, and can
potentially have great upper body strength
- In COPD: lungs chronically overinflated with air rib
cage stays partially expanded all the time
breathing less efficient and aggravates any existing
shortness of breath
LUNG LIVER BORDER
The upper border of liver dullness is defined by:
o 5th intercostal space in the midclavicular line
o 7th intercostal space in the midaxillary line
o 9th intercostal space in the scapular line
Note: 9th intercostal space is located approximately at the inferior border of the scapula
HYPERSONAR
Also called hyperresonant. In percussion, heared tympanic or drum-like, as
opposed to dull
Resonant sounds are low pitched, hollow sounds heard over normal lung tissue.
Hyperresonant sounds that are louder and lower pitched than resonant sounds are
normally heard when percussing the chests of children and very thin adults.
Hyperresonant sounds may also be heard when percussing lungs hyperinflated with air,
such as may occur in patients with COPD, or patients having an acute asthmatic attack.
An area of hyperresonance on one side of the chest may indicate a pneumothorax.
PAGE INTERPRETATION (CASE 5)| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 27/11/13
WHEEZING AND CRACKLES
Crackles are discontinuous, explosive, "popping" sounds that
originate within the airways. They are heard when an obstructed
airway suddenly opens and the pressures on either side of the
obstruction suddenly equilibrates resulting in transient, distinct
vibrations in the airway wall. The dynamic airway obstruction can
be caused by either accumulation of secretions within the airway
lumen or by airway collapse caused by pressure from inflammation
or edema in surrounding pulmonary tissue. Crackles can be heard
during inspiration when intrathoracic negative pressure results in
opening of the airways or on expiration when thoracic positive
pressure forces collapsed or blocked airways open. Crackles are
heard more commonly during inspiration than expiration. They are
significant as they imply either accumulation of fluid secretions or
exudate within airways or inflammation and edema in the
pulmonary tissue.
Wheezes are continuous musical tones that are most
commonly heard at end inspiration or early expiration. They
result as a collapsed airway lumen gradually opens during
inspiration or gradually closes during expiration. As the
airway lumen becomes smaller, the air flow velocity increases
resulting in harmonic vibration of the airway wall and thus the
musical tonal quality. Wheezes can be classified as either high
pitched or low pitched wheezes. It is often inferred that high
pitch wheezes are associated with disease of the small
airways and low pitch wheezes are associated with disease of
larger airways. However, this association has not been
confirmed. Wheezes may be monophonic (a single pitch and
tonal quality heard over an isolated area) or polyphonic
(multiple pitches and tones heard over a variable area of the
lung). Wheezes are significant as they imply decreased airway
lumen diameter either due to thickening of reactive airway
walls or collapse of airways due to pressure from surrounding
pulmonary disease.
CLUBBING FINGER
Also called drumstick finger or watch-glass nails.
Clubbing finger is a deformity of
the fingers and fingernails associated with a number of
diseases, mostly of the heart and lungs
PAGE INTERPRETATION (CASE 5)| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 27/11/13
NORMAL LABORATORY TEST (IN PAGE)
Hemoglobin
WBC
DIFFERENTIAL COUNT
PLATELET
EMPHYSEMATOUS LUNG
Emphysema is a chronic lung condition in which the lungs'
natural airspaces, called alveoli, become larger but
decrease in number. The tissue surrounding the alveoli loses
elasticity so that the airspaces can no longer expand and
shrink as usual. This reduces the amount of oxygen
transferred by the
lungs to the
bloodstream,
making it more
difficult for you to
breathe
PAGE INTERPRETATION (CASE 5)| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 27/11/13
SPIROMETRY
BLOOD GAS ANALYSIS
ECHOCARDIOGRAPHY
PAGE INTERPRETATION (CASE 5)| Tutorial B-1 RS
130110110177|Gabriella Chafrina| 27/11/13
BOHR EFFECT
A shift of the oxygen hemoglobin dissociation curve to the
right in response to increases in blood carbon dioxide and
hydrogen ions has a significant effect by enhancing the
release of oxygen from the blood in the tissues and
enhancing oxygenation of the blood in the lungs. As the
blood passes through the tissues, carbon dioxide diffuses
from the tissue cells into the blood. This increases the blood
Po2, which in turn raises the blood H
2
CO
3
(carbonic acid) and
the hydrogen ion concentration. These effects shift the
oxygen-hemoglobin dissociation curve to the right and
downward, forcing oxygen away from the hemoglobin
and therefore delivering increased amounts of oxygen to the
tissues. Exactly the opposite effects occur in the lungs,
where carbon dioxide diffuses from the blood into the
alveoli. This reduces the blood Pco2 and decreases the hydrogen ion concentration, shifting the oxygen-
hemoglobin dissociation curve to the left and upward. Therefore, the quantity of oxygen that binds with
the hemoglobin at any given alveolar Po2 becomes considerably increased, thus allowing greater oxygen
transport to the tissues.
FACTOR INFLUENCE O
2
BIND TO Hb
- pH H
+
and O
2
both compete for binding to the Hb molecule
- CO
2
concentration influences intracellular pH and CO
2
accumulation causes carbamino compounds to be generated
through chemical interactions, which bind to Hb forming
carbaminohemoglobin
- blood temperature when will weaken and denature bond
between oxyhemoglobin
- 2,3-biphosphoglycerate (BPG) an organophosphate which is
created in erythrocytes during glycolysis
You might also like
- Pathogenesis of LeprosyDocument13 pagesPathogenesis of LeprosyNurul AinNo ratings yet
- Rs4 Phop CRPDocument2 pagesRs4 Phop CRPGabriella ChafrinaNo ratings yet
- Foreign Body EarDocument34 pagesForeign Body EarGabriella ChafrinaNo ratings yet
- Soal Mde Tropmed 2007Document4 pagesSoal Mde Tropmed 2007Gabriella ChafrinaNo ratings yet
- RS3 PiDocument5 pagesRS3 PiGabriella ChafrinaNo ratings yet
- Rs6 Pleural TuberculosisDocument5 pagesRs6 Pleural TuberculosisGabriella ChafrinaNo ratings yet
- ECG Arrhythmia GraphsDocument3 pagesECG Arrhythmia GraphsGabriella ChafrinaNo ratings yet
- Cvs4-Clinical Aspects of Serum Cholesterol LevelDocument2 pagesCvs4-Clinical Aspects of Serum Cholesterol LevelGabriella ChafrinaNo ratings yet
- Lab PharmacologyDocument2 pagesLab PharmacologyGabriella ChafrinaNo ratings yet
- Rs6 Extrapulmonary TuberculosisDocument4 pagesRs6 Extrapulmonary TuberculosisGabriella ChafrinaNo ratings yet
- RS7 InfluenzaDocument6 pagesRS7 InfluenzaGabriella ChafrinaNo ratings yet
- Group A Β-Hemolytic Streptococcus: - Tutorial B-1 RSDocument2 pagesGroup A Β-Hemolytic Streptococcus: - Tutorial B-1 RSGabriella ChafrinaNo ratings yet
- TM3-Diagnosis and DD of MalariaDocument3 pagesTM3-Diagnosis and DD of MalariaGabriella ChafrinaNo ratings yet
- RS7-Acid Base BalanceDocument4 pagesRS7-Acid Base BalanceGabriella ChafrinaNo ratings yet
- Rs6-Cervical Lymph NodeDocument6 pagesRs6-Cervical Lymph NodeGabriella ChafrinaNo ratings yet
- RS5-Defense Mech of LungDocument3 pagesRS5-Defense Mech of LungGabriella ChafrinaNo ratings yet
- ANTI HYPERTENSIVE DRUGSDocument7 pagesANTI HYPERTENSIVE DRUGSGabriella ChafrinaNo ratings yet
- RS1 ManagementDocument3 pagesRS1 ManagementGabriella ChafrinaNo ratings yet
- Macroscopic Hematuria GuideDocument3 pagesMacroscopic Hematuria GuideGabriella ChafrinaNo ratings yet
- Deep Vein Thrombosis (DVT) : - Tutorial D-1 CVSDocument1 pageDeep Vein Thrombosis (DVT) : - Tutorial D-1 CVSGabriella ChafrinaNo ratings yet
- Rs4-Gas Exchange and TransportDocument5 pagesRs4-Gas Exchange and TransportGabriella ChafrinaNo ratings yet
- Lab PharmacologyDocument2 pagesLab PharmacologyGabriella ChafrinaNo ratings yet
- CVS6 Page InterpretationDocument2 pagesCVS6 Page InterpretationGabriella ChafrinaNo ratings yet
- CVS6 Heart SoundsDocument3 pagesCVS6 Heart SoundsGabriella ChafrinaNo ratings yet
- Iccu (Tachycardia) : - Tutorial D-1 CVSDocument2 pagesIccu (Tachycardia) : - Tutorial D-1 CVSGabriella ChafrinaNo ratings yet
- Iccu (Tachycardia) : - Tutorial D-1 CVSDocument2 pagesIccu (Tachycardia) : - Tutorial D-1 CVSGabriella ChafrinaNo ratings yet
- CVS5-Conduction of Cardiac Action PotentialsDocument1 pageCVS5-Conduction of Cardiac Action PotentialsGabriella ChafrinaNo ratings yet
- Advance Life Support (American Heart Association 2010) : - Tutorial D-1 CVSDocument1 pageAdvance Life Support (American Heart Association 2010) : - Tutorial D-1 CVSGabriella ChafrinaNo ratings yet
- Advanced Life Support Algorithm GuideDocument1 pageAdvanced Life Support Algorithm GuideGabriella ChafrinaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- HISTORY TAKING FINAL Sumanyu258@gmail - Com 01092014 PDFDocument111 pagesHISTORY TAKING FINAL Sumanyu258@gmail - Com 01092014 PDFMohit BiswalNo ratings yet
- Viva Questions of Final Professional ExaminationDocument48 pagesViva Questions of Final Professional ExaminationFaisol KabirNo ratings yet
- Chronic Congestive Heart FailureDocument10 pagesChronic Congestive Heart FailureEllappa GhanthanNo ratings yet
- In Re Briggs A WLS Employee 12-22560Document107 pagesIn Re Briggs A WLS Employee 12-22560NevadaGadflyNo ratings yet
- COPD Case Study Reveals Mechanisms of DyspneaDocument27 pagesCOPD Case Study Reveals Mechanisms of DyspneaMelissa MakhoulNo ratings yet
- Asthma Ineffective Airway ClearanceDocument2 pagesAsthma Ineffective Airway ClearanceEdmr SlzarNo ratings yet
- EmpisemaDocument11 pagesEmpisemaVIRGIL ZELINDRAHNo ratings yet
- Emrgency Guidelines 3 RD EditionDocument123 pagesEmrgency Guidelines 3 RD EditionMitz MagtotoNo ratings yet
- Evaluation of Dyspneic PatientDocument15 pagesEvaluation of Dyspneic Patientcamila perillaNo ratings yet
- Problem List Assessment Nursing Diagnosis Planning ImplementationDocument2 pagesProblem List Assessment Nursing Diagnosis Planning ImplementationJai GoNo ratings yet
- NUR 2115 Final Exam Fundamentals of Professional Nursing Final Exam Concept Review Fall 2020 Rasmussen College - RemovedDocument5 pagesNUR 2115 Final Exam Fundamentals of Professional Nursing Final Exam Concept Review Fall 2020 Rasmussen College - RemovedJudy DurkinNo ratings yet
- COPDDocument54 pagesCOPDSushmaNo ratings yet
- Respiratory DisordersDocument17 pagesRespiratory DisordersVallesh ShettyNo ratings yet
- Chest PhysiotherapyDocument12 pagesChest Physiotherapysenthilkumar100% (2)
- ABC Lecture NotesDocument7 pagesABC Lecture NotesLady Shayne YapNo ratings yet
- LCP Asthma Club Seminar Teaches Patients to Manage AsthmaDocument2 pagesLCP Asthma Club Seminar Teaches Patients to Manage AsthmaEliseo RamirezNo ratings yet
- Case Study Hematology I 2Document1 pageCase Study Hematology I 2Mark SyNo ratings yet
- Midterm Review 1Document39 pagesMidterm Review 1Beverly ManaloNo ratings yet
- NGNTestPacket 110322Document64 pagesNGNTestPacket 110322romeliza romeliza0% (1)
- Imss Registration FormatDocument2 pagesImss Registration FormatScribdTranslationsNo ratings yet
- Nitrofurantoin 50 and 100 MF UKPARDocument30 pagesNitrofurantoin 50 and 100 MF UKPARdivyenshah3No ratings yet
- Cebu (Velez) General Hospital Department of PediatricsDocument4 pagesCebu (Velez) General Hospital Department of PediatricsJanelle Estrabela GargaritanoNo ratings yet
- Copd 8 439Document13 pagesCopd 8 439alNo ratings yet
- Indications For Common Rlung Formulas in Tibetan MedicineDocument8 pagesIndications For Common Rlung Formulas in Tibetan MedicineErikjampaNo ratings yet
- Exercise in PregnancyDocument7 pagesExercise in PregnancynirchennNo ratings yet
- GNG Health Screening FormDocument2 pagesGNG Health Screening FormGeorge NakojaNo ratings yet
- Physiological Integrity Oxygenation RN RespDocument13 pagesPhysiological Integrity Oxygenation RN RespAaLona RobinsonNo ratings yet
- 1800 MCQ Revised VersionDocument606 pages1800 MCQ Revised VersionFarah FarahNo ratings yet
- Jessica Crish Youngstown State University NURS 4852 Senior Capstone Dr. Kim Ballone & Wendy Thomas February 28, 2022Document6 pagesJessica Crish Youngstown State University NURS 4852 Senior Capstone Dr. Kim Ballone & Wendy Thomas February 28, 2022api-592372682No ratings yet
- COVID-19 Outpatient Department RequirementsDocument10 pagesCOVID-19 Outpatient Department RequirementsJustine CagatanNo ratings yet