Professional Documents
Culture Documents
Kasus Asma
Uploaded by
Hananun Zharfa0%(3)0% found this document useful (3 votes)
1K views5 pagesASMA
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentASMA
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0%(3)0% found this document useful (3 votes)
1K views5 pagesKasus Asma
Uploaded by
Hananun ZharfaASMA
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
ASMA AKUT
My boy has trouble breathing and he keeps coughing. His albuterol
isnt helping.
_ HPI
Peyton Harrison is a 3-year-old African-American boy who presents
to the emergency department with a 3-day history of cough and
congestion. The mother was giving him albuterol, 2.5 mg via
nebulization twice a day since the cough started. She was also giving
him an allergy medicine. He did have a fever 3 days prior to
admission, and he was given ibuprofen. The previous night before
admission, he seemed to be gasping for air and during the day
today, he has had an increased work of breathing. Mother also notes
that he has been fussy, not eating well, and has had only two to three
urinations in the past 24 hours. His assessment in the emergency
department revealed him to have labored breathing that was more
difficult with activities. He had mild retractions with tachypnea at
52 breaths per minute. His other vital signs were a heart rate of 137
beats per minute, blood pressure of 100/68, temperature of 38.9C,
and a weight of 14.4 kg. The initial oxygen saturation was 88%, and
he was started on oxygen at 1.5 liter/min via nasal cannula. His
breath sounds were noted to have fair air exchange but with
expiratory wheezes. His chest x-ray revealed patchy infiltrates consistent
with pneumonia. Peyton was complaining of a runny nose
and sore throat. He did not have any ear pain. While in the
emergency department, he was given three albuterol/ipratropium
nebulizations and one dose of prednisolone 15 mg orally. He
received one dose of acetaminophen 210 mg. His breath sounds and
oxygenation did not improve so he was started on hourly albuterol
nebulizations at 5 mg. Peyton was then transferred to the Pediatric
Intensive Care Unit for further treatment and monitoring.
_ PMH
Asthma, unknown if previous hospitalizations
S/P tonsillectomy/adenoidectomy at 2 years of age
_ FH
Unknown
_ SH
Lives with foster mother and two siblings. Birth mother has visitations.
Unclear as to reason for foster placement. Positive tobacco
exposure in current home.
_ Meds
Albuterol 2.5 mg via nebulizer as needed
Phenylephrine/chlorpheniramine/methscopolamine (Dallergy), dose
unknown
_ All
NKA
_ ROS
(+) Fever, cough, congestion, increased work of breathing
_ Physical Examination
Gen
NAD, moderate increase in work of breathing
VS
BP 103/55, P 154, T 36.4C, R 29, O2 sat 94% at 1.5 L/min nasal
cannula
Skin
No rashes, no bruises
HEENT
NC/AT, PERRLA
Neck/Lymph Nodes
Soft, supple, no cervical lymphadenopathy
Chest
Slight decrease in breath sounds bilaterally, minimal wheezing
CV
RRR, no MRG
Abd
Soft, NT/N
Ext
No clubbing or cyanosis
Neuro
A & O, no focal deficits
_ Labs
Respiratory viral panel nasal swab: positive for parainfluenza 3
Na 134 mEq/L WBC 6.5 103/mm3
K 3.0 mEq/L RBC 3.84 106/mm3
Cl 103 mEq/L Hgb 10 g/dL
CO2 19 mEq/L Hct 34%
BUN 6 mg/dL Plt 252 103/mm3
SCr 0.4 mg/dL
Glu 140 mg/Dl
_ Chest X-Ray
Patchy infiltrates throughout lung fields
_ Assessment
Asthma exacerbation with pneumonia and dehydration
QUESTIONS
Problem Identification
1.a. Create a list of the patients drug-related problems.
1.b. What information (signs, symptoms, laboratory values) indicates
the severity of the acute asthma attack?
Desired Outcome
2. What are the acute goals of pharmacotherapy in this case?
Therapeutic Alternatives
3.a. What nondrug therapies might be useful for this patient?
3.b. What feasible pharmacotherapeutic alternatives are available
for the treatment of acute asthma?
Optimal Plan
4.a. What drug, dosage form, dose, schedule, and duration of
therapy are best for this patients acute asthma exacerbation?
4.b. What other pharmacotherapy would you recommend in the
acute treatment of this patient?
CLINICAL COURSE
Within 72 hours of initiation of the treatment plan for management
of the acute exacerbation, Peyton was stable enough to transfer to
the general pediatric floor. His vital signs were BP 111/67, P 108, R
26, T 36.7C, O2 sat 99% on 0.5 L/min nasal cannula. Mother states
that he is more like his normal self and doesnt seem to have much
trouble breathing now.
4.c. What drug, dosage form, dose, schedule and duration of
therapy are best for this patients discharge plan?
Outcome Evaluation
5.a. Once the patient has transferred to the general medical floor
and his vitals have improved (see Clinical Course), what
clinical and laboratory parameters are necessary to evaluate the
therapy for achievement of the desired therapeutic outcome
and to detect or prevent adverse effects at that point in the
patients care?
5.b. What clinical parameters are necessary to evaluate the efficacy
of the patients asthma therapy after hospital discharge?
Patient Education
6.a. Describe the information that should be provided to the family
regarding nebulization technique, the differences between quickrelief
and controller medications, and possible asthma triggers.
6.b. What should the family monitor for regarding the potential
adverse effects from the drug therapy?
FOLLOW-UP QUESTIONS
1. Should any cough and cold products be used for asthma symptoms?
Why or why not?
2. What methods could be used to help a pediatric patient and the
family to be compliant with nebulization treatments?
3. What information can be given to families who are concerned
about giving their child steroids for asthma treatment (either
in an acute asthma exacerbation or for controller therapy)?
SELF-STUDY ASSIGNMENTS
1. Research the efficacy of systemic corticosteroids for treatment of
acute asthma exacerbation when given intravenously versus orally
(enterally).
2. Discuss the differences in acute asthma exacerbation symptoms
in an adult patient versus a pediatric patient, and describe when
you would refer a patient (or family) to the physician or
emergency department based on his or her asthma action plan.
3. Discuss the appropriate use of ipratropium bromide in an acute
asthma exacerbation.
CLINICAL PEARL
For proper treatment of an acute asthma exacerbation, the patient (or
family) needs to be aware of the first symptoms of an exacerbation and
possible triggers. At this point, the patient (family) should initiate his
or her asthma action plan to minimize the symptoms, duration of
drug therapy, and severity of the exacerbation. This in turn, should
decrease the number of severe exacerbations and hospital admissions.
(Jennifer A. Donaldson, PharmD)
ASMA KRONIS
_ Chief Complaint
I cantbreatheand my albuteroldoesnt seem to be helping!
_ HPI
Madison Bradley is a 29-year-old woman who presents to the ED for
an acute visit due to shortness of breath. She reports feeling especially
short of breath since awakening this morning. She states that she has
been using her albuterol every hour for the past 6 hours and that it
doesnt seem to be helping. Her peak flows have been running
between 180 L/min and 200 L/min today (personal best = 400 L/
min). In addition to her albuterol MDI, which she uses PRN, she also
has a fluticasone MDI, which she uses most days of the week. She
reports having to use her albuterol inhaler approximately 34 times
per week over the past 2 months, but over the past week she admits
to using albuterol almost daily. She reports being awakened by a
cough three times over the past month. She states she especially
becomes short of breath when she exercises; although she admits that
her shortness of breath is not always brought on by exercise and
sometimes occurs when she is not actively exercising. She indicates
that her morning peak flows have been running around 300 L/min
(personal best = 400 L/min) over the past several weeks.
_ PMH
Asthma (previously documented as mild persistent) since childhood;
no prior history of intubations; hospitalized twice in the
past year for poorly controlled asthma; three visits to the ED in
the past 6 months; treated with oral systemic corticosteroids
during both hospitalizations and at each ED visit.
Migraine headache disorder (diagnosed at age 21); currently taking
prophylactic medication; has had only one migraine attack in the
past year.
_ FH
Both parents living; mother 52-years-old with HTN, osteoporosis;
father 54-years-old with COPD (33 pack-year smoking history) and
Type 2 DM; brother, age 34 (smoker); sister, age 32 (non-smoker)
_ SH
No alcohol or tobacco use. Married, sexually active. Lives with
husband (cabinetmaker; non-smoker) and two cats.
_ Meds
Fluticasone HFA 110 mcg, 2 puffs BID
Albuterol HFA 2 puffs Q 46 h PRN shortness of breath
Ortho-Tri-Cyclen 1 po daily
Propranolol 80 mg po BID
Maxalt-MLT 5 mg po PRN acute migraine
_ All
Sulfa (rash)
_ Physical Examination
Gen
Anxious-appearing Caucasian female; moderate respiratory distress
with audible wheezing noted; unable to speak in complete sentences;
suprasternal muscle retractions noted; hunched forward
VS
BP 134/78, HR 110, RR 22, T 37C; Wt 68 kg, Ht 5'5''; Pulse Ox 88%
on RA
HEENT
PERRLA; mild oral thrush; TMs intact
Neck/Lymph Nodes
Supple; no lymphadenopathy or thyromegaly
Lungs/Thorax
High-pitched, diffuse expiratory wheezes bilaterally, two-thirds of
the way up
Breasts
Nontender without masses
CV
Tachycardia; Regular rhythm; no MRG
Abd
Soft, NTND; (+) BS
Genit/Rect
Deferred
Ext
Normal ROM; peripheral pulses 3+; no CCE
Neuro
No motor deficits; CN IIXII grossly intact; A & O 3
_ Labs
_ Chest X-Ray
Hyperinflated lungs; no infiltrates
Na 134 mEq/L Hgb 12 g/dL WBC 8.0 103/mm3
K 3.0 mEq/L Hct 36% PMNs 56%
Cl 99 mEq/L RBC 5.0 106/mm3 Bands 1%
CO2 28 mEq/L MCH 28 pg Eosinophils 3%
BUN 22 mg/dL MCHC 34 g/dL Basophils 2%
SCr 0.7 mg/dL MCV 90 m3 Lymphocytes 33%
Glu 117 mg/dL Plts 192 103/mm3 Monocytes 5%
_ Assessment
29 yo woman with moderate to severe exacerbation of asthma;
uncontrolled chronic asthma
_ Clinical Course
The patient is admitted overnight for treatment with oxygen, inhaled
bronchodilators, and oral prednisone 60 mg daily. She is discharged
home with her previous regimen plus nebulized albuterol 2.5 mg
every 8 hours for 5 days and prednisone 60 mg orally once daily to
complete a 10-day burst. She was also given nystatin swish and
swallow for treatment of her oral thrush infection. On follow-up at
day 4 in the clinic, her lungs are clear without wheezing; her respiratory
rate is 16 breaths per minute; and her pulse oximetry is 97% on
room air. Her peak flow readings have improved to 300 L/min.
QUESTIONS
Problem Identification
1.a. Create a list of the patients drug therapy problems.
1.b. What information indicates the presence of uncontrolled
chronic asthma and an acute asthma exacerbation?
1.c. What factors may have contributed to this patients poorly
controlled asthma and acute exacerbation?
1.d. How would you classify this patients level of asthma control
(well controlled, not well controlled, or very poorly controlled),
according to NIH guidelines?
Desired Outcome
2. What are the goals of pharmacotherapy in this case?
Therapeutic Alternatives
3.a. What nonpharmacologic therapies might be useful for this
patient?
3.b. What feasible pharmacotherapeutic alternatives are available
for treatment of this patients chronic asthma?
Optimal Plan
4.a. Outline an optimal plan of treatment for this patients chronic
asthma.
4.b. What alternatives would be appropriate if the initial therapy fails?
Outcome Evaluation
5. What clinical parameters are necessary to evaluate the therapy for
achievement of the desired therapeutic effect and to detect or
prevent adverse effects?
Patient Education
6. What information should be provided to the patient regarding
the use of her asthma medications and how she can use her peakflow
readings to better manage her disease?
SELF-STUDY ASSIGNMENTS
1. Review the NIH guidelines on the management of asthma during
pregnancy, and develop a pharmacotherapeutic treatment plan
for this patients asthma if she were to become pregnant.
2. Review the literature on the impact of chronic inhaled corticosteroid
use on the risk for development of osteoporosis, and
write a two-page paper summarizing the available published
literature on this topic.
CLINICAL PEARL
Patients with asthma who report that taking aspirin makes their
asthma symptoms worse may respond well to leukotriene modifiers.
Aspirin inhibits prostaglandin synthesis from arachidonic acid
through inhibition of cyclooxygenase. The leukotriene pathway may
play a role in the development of asthma symptoms in such patients,
as inhibition of cyclooxygenase by aspirin may shunt the arachidonic
acid pathway away from prostaglandin synthesis and toward leukotriene
production. Although inhaled corticosteroids are still the preferred
anti-inflammatory medications for patients with asthma and
known aspirin sensitivity, leukotriene modifiers may
(Julia M. Koehler, PharmD ; Carrie Maffeo, PharmD, BCPS, CDE)
Pharmacotherapy Case File, Terry L. Schwinghammer, 2009
You might also like
- Psychiatric Assessment ToolDocument53 pagesPsychiatric Assessment ToolLori100% (4)
- Lecture Notes On PsychiatryDocument38 pagesLecture Notes On PsychiatryMing Wang50% (6)
- Hypnotherapy Scripts 6 Steve G Jones Ebook PDFDocument66 pagesHypnotherapy Scripts 6 Steve G Jones Ebook PDFjohannes2212100% (10)
- Physical Changes With AgingDocument8 pagesPhysical Changes With Agingjanna mae patriarcaNo ratings yet
- AO 56 S 1989 LTODocument13 pagesAO 56 S 1989 LTOmikan2No ratings yet
- NSP2 PDFDocument92 pagesNSP2 PDFIrene C. CruzNo ratings yet
- Administrative Order No 56 S 1989Document7 pagesAdministrative Order No 56 S 1989Anne Marion Perez67% (3)
- Generic DispensingDocument30 pagesGeneric Dispensingshervintancruzado83% (6)
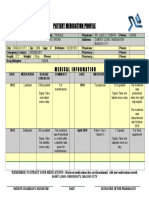
- Medication ProfileDocument1 pageMedication ProfileKlendle Leigh Revocal100% (1)
- Unit 1. Clinical PharmacyDocument5 pagesUnit 1. Clinical PharmacyAashish BhattaraiNo ratings yet
- Dispensing Lecture Reviewer - MidtermDocument26 pagesDispensing Lecture Reviewer - Midtermapi-306968266No ratings yet
- Hospital FormularyDocument27 pagesHospital FormularyMarvin BernalesNo ratings yet
- Aiims Hospital Disaster PlanDocument6 pagesAiims Hospital Disaster PlanSujatha J JayabalNo ratings yet
- Four Humors Theory in Unani MedicineDocument4 pagesFour Humors Theory in Unani MedicineJoko RinantoNo ratings yet
- TR-Pharmacy Services NC IIIDocument135 pagesTR-Pharmacy Services NC IIIAljon Fortaleza Balanag100% (2)
- Community Pharmacy Internship Reflection PaperDocument2 pagesCommunity Pharmacy Internship Reflection PaperPeter Paul Recabo100% (2)
- Páginas Desdepharmacotherapy Casebook 10th Ed.Document61 pagesPáginas Desdepharmacotherapy Casebook 10th Ed.Glo VsNo ratings yet
- Standard Patient Counseling ScriptDocument22 pagesStandard Patient Counseling ScriptElleason Joshua G. FranciscoNo ratings yet
- Philippine Practice Standards For PharmacistsDocument8 pagesPhilippine Practice Standards For PharmacistsAgatha Rose100% (1)
- Storage of Dosage FormsDocument20 pagesStorage of Dosage FormsMeredith Kerr50% (2)
- Ao 55 1988Document10 pagesAo 55 1988Ella Riva100% (2)
- Briefer On RA 10918Document3 pagesBriefer On RA 10918Eugene UC100% (1)
- Philippine Pharmacists Advocacy Programs PDFDocument4 pagesPhilippine Pharmacists Advocacy Programs PDFFaith Gabriel100% (1)
- Standard Operating Procedure Good Storage PracticeDocument2 pagesStandard Operating Procedure Good Storage PracticeDaniel Yves IV Paez100% (1)
- Jurisprudence and EthicsDocument22 pagesJurisprudence and EthicsRozamae Magnanao100% (1)
- Dispensing and Medication CounselingDocument12 pagesDispensing and Medication CounselingLei100% (3)
- Hospital Pharmacy QA and Inventory ControlDocument9 pagesHospital Pharmacy QA and Inventory ControlChristian Rey Abuan80% (10)
- Hospital Information Management System - Cover PageDocument15 pagesHospital Information Management System - Cover Pageapi-1946401583% (6)
- Organization of NICU ServicesDocument45 pagesOrganization of NICU ServicesMonika Bagchi84% (64)
- PALS Helpful Hints 2015 Guidelines Posted Nov 2016Document5 pagesPALS Helpful Hints 2015 Guidelines Posted Nov 2016Mj Teate100% (1)
- Asthma - Case PresentationDocument56 pagesAsthma - Case Presentationsarooah199467% (6)
- Pharmaceutical Jurisprudence - Ethics Answer Key-RED PACOPDocument20 pagesPharmaceutical Jurisprudence - Ethics Answer Key-RED PACOPArk Olfato ParojinogNo ratings yet
- The Philippine Pharmacy Act: RA 10918 Submitted By: Emerald Shaine P. SamozaDocument49 pagesThe Philippine Pharmacy Act: RA 10918 Submitted By: Emerald Shaine P. Samozaemerald shaine samozaNo ratings yet
- Dr. Nelson T. TubonDocument29 pagesDr. Nelson T. TubonBS50% (2)
- (BLUE PACOP) Pharmaceutical Jurisprudence & EthicsDocument31 pages(BLUE PACOP) Pharmaceutical Jurisprudence & EthicsDenise Yanci Demiar100% (1)
- CentralVenousCatheters PDFDocument77 pagesCentralVenousCatheters PDFHarold De Leon Malang100% (1)
- Code of Ethics and PPhADocument12 pagesCode of Ethics and PPhARaymond Godfrey DagwasiNo ratings yet
- OutputDocument1 pageOutputmsenthamizharasaNo ratings yet
- BFAD GUIDELINES LABELING DRUG PRODUCTSDocument35 pagesBFAD GUIDELINES LABELING DRUG PRODUCTSDaya Mavi Tura Gabuyo100% (2)
- Basic Iv Fluid PDFDocument77 pagesBasic Iv Fluid PDFDesi AdiyatiNo ratings yet
- Associate Professor:Ivan Bonet. Obstetric and Gynecology Associate Professor:Ivan Bonet. Obstetric and GynecologyDocument31 pagesAssociate Professor:Ivan Bonet. Obstetric and Gynecology Associate Professor:Ivan Bonet. Obstetric and Gynecologyivan0% (1)
- Ra 9711-FDA Act of 2009Document34 pagesRa 9711-FDA Act of 2009Shehana Tawasil Musahari0% (1)
- Pharmaceutical Jurisprudence and Ethics ManualDocument51 pagesPharmaceutical Jurisprudence and Ethics ManualYap JackyNo ratings yet
- Damasco - Cpi - Activity No.9Document5 pagesDamasco - Cpi - Activity No.9LDCU - Damasco, Erge Iris M.No ratings yet
- Ra 10918Document23 pagesRa 10918Colleen Ariel SandovalNo ratings yet
- Space Management in Pediatric DentistryDocument37 pagesSpace Management in Pediatric DentistryAlshammary Freah100% (3)
- (Dispensing 1 Laboratory) Review NotesDocument12 pages(Dispensing 1 Laboratory) Review NotesZen HeartNo ratings yet
- Addition and DeletionDocument10 pagesAddition and DeletionNikkaMontilNo ratings yet
- Exam PrelimDocument4 pagesExam PrelimRochelle Anne Abad BandaNo ratings yet
- Ao 99 S 1990Document2 pagesAo 99 S 1990taengoo2180% (1)
- Tablet FriabilityDocument25 pagesTablet FriabilityJean Florencondia67% (3)
- Ethical Standards for Health Product PromotionDocument14 pagesEthical Standards for Health Product PromotionKitkat CasacopNo ratings yet
- Name: Eyah Ifeanyi Godfrey Score: Year Level: 3 Date: 12/7/2020Document14 pagesName: Eyah Ifeanyi Godfrey Score: Year Level: 3 Date: 12/7/2020Jeyma Dacumos100% (1)
- PX CDocument1 pagePX CMich TolentinoNo ratings yet
- Advocacy in PharmacyDocument3 pagesAdvocacy in PharmacyZofia RanadaNo ratings yet
- Nica Chua - Hospital Pharmacy Internship Daily Activity Report-Day 33 MajorDocument5 pagesNica Chua - Hospital Pharmacy Internship Daily Activity Report-Day 33 MajorMa Victoria ChuaNo ratings yet
- Dispensing CA NotesDocument16 pagesDispensing CA NotesJohn TecsonNo ratings yet
- Clinical Pharmacy Answer Key-PINK PACOPDocument29 pagesClinical Pharmacy Answer Key-PINK PACOPKaguraNo ratings yet
- INTERN-3 Community Pharmacy ProfileDocument34 pagesINTERN-3 Community Pharmacy ProfilejadeNo ratings yet
- Republic Act No 6675Document4 pagesRepublic Act No 6675JenilynM.ChuNo ratings yet
- Internship5 12Document7 pagesInternship5 12Jerel MarquezNo ratings yet
- Exercises 8-10 (By Dr. N. Tubon) PDFDocument25 pagesExercises 8-10 (By Dr. N. Tubon) PDFLoren100% (1)
- Iinternship 13Document35 pagesIinternship 13Darwin MangabatNo ratings yet
- PhenacetinDocument16 pagesPhenacetinJericSalcedoNo ratings yet
- Apply for FDA License to Operate (LTO) in the PhilippinesDocument3 pagesApply for FDA License to Operate (LTO) in the Philippinesarkina_sunshine0% (1)
- Ra 3720 - Safety and Purity of Foods, and CosmeticsDocument70 pagesRa 3720 - Safety and Purity of Foods, and CosmeticsShehana Tawasil MusahariNo ratings yet
- Case 2Document4 pagesCase 2Patrícia Martins25% (4)
- Bronchial AsthmaDocument3 pagesBronchial AsthmaSabrina Reyes0% (1)
- CasesDocument25 pagesCasesfatemaNo ratings yet
- Cases Resp - SystemDocument12 pagesCases Resp - SystemJerin XavierNo ratings yet
- By Nawal GaletDocument54 pagesBy Nawal GaletSoia NeriyaniNo ratings yet
- Osce PDFDocument18 pagesOsce PDFMahamed Wefkey OmranNo ratings yet
- NCM 112 Rle Case Analysis: Care of Client With Alterations in Oxygenation (ASTHMA)Document2 pagesNCM 112 Rle Case Analysis: Care of Client With Alterations in Oxygenation (ASTHMA)Joegie ArioNo ratings yet
- Pediatric Asthma TBL QuestionsDocument4 pagesPediatric Asthma TBL QuestionsVladimir BasurtoNo ratings yet
- JNC 8Document14 pagesJNC 8amiwahyuniNo ratings yet
- Hipertensi AND Kemoterapi PDFDocument11 pagesHipertensi AND Kemoterapi PDFHananun ZharfaNo ratings yet
- Ich Q3C (R4)Document25 pagesIch Q3C (R4)Ravishankar NagarajanNo ratings yet
- Click To Edit Master Subtitle StyleDocument4 pagesClick To Edit Master Subtitle StyleRobertoArandaNo ratings yet
- Internasional PDFDocument10 pagesInternasional PDFHananun ZharfaNo ratings yet
- Stifar Komplemen2013Document44 pagesStifar Komplemen2013Hananun ZharfaNo ratings yet
- 232 439 1 SMDocument10 pages232 439 1 SMHananun ZharfaNo ratings yet
- 14 13 1 PB PDFDocument9 pages14 13 1 PB PDFRizki PuspitasariNo ratings yet
- How to Get Scholarships for Studying AbroadDocument15 pagesHow to Get Scholarships for Studying AbroadHananun ZharfaNo ratings yet
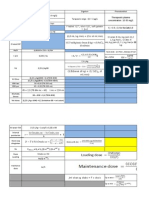
- Rumus Cp maks Cp min C toksik farmasiDocument4 pagesRumus Cp maks Cp min C toksik farmasiHananun ZharfaNo ratings yet
- Fast Dissolving Oral Films An Innovative DrugDocument8 pagesFast Dissolving Oral Films An Innovative DrugHananun ZharfaNo ratings yet
- How to Get Scholarships for Studying AbroadDocument15 pagesHow to Get Scholarships for Studying AbroadHananun ZharfaNo ratings yet
- Pembuatan Fase Gerak KKT: KarbohidratDocument4 pagesPembuatan Fase Gerak KKT: KarbohidratHananun ZharfaNo ratings yet
- Rumus Cp maks Cp min C toksik farmasiDocument4 pagesRumus Cp maks Cp min C toksik farmasiHananun ZharfaNo ratings yet
- GrafikDocument7 pagesGrafikHananun ZharfaNo ratings yet
- How to Get Scholarships for Studying AbroadDocument15 pagesHow to Get Scholarships for Studying AbroadHananun ZharfaNo ratings yet
- Analisis ParetoDocument1 pageAnalisis ParetoHananun ZharfaNo ratings yet
- Dept. of Pulmonology expertise in lung careDocument7 pagesDept. of Pulmonology expertise in lung carerohit6varma-4No ratings yet
- AtherosclerosisDocument7 pagesAtherosclerosisFaris Mufid Madyaputra100% (1)
- Emergency Contact ListDocument1 pageEmergency Contact ListthubanNo ratings yet
- Dental BS Delta 1500 PPO Benefit Summary 2018Document4 pagesDental BS Delta 1500 PPO Benefit Summary 2018deepchaitanyaNo ratings yet
- Major & Mild NCD Terminology UpdatesDocument30 pagesMajor & Mild NCD Terminology Updatesrachelle anne merallesNo ratings yet
- Health Apps - A ToolkitDocument3 pagesHealth Apps - A ToolkitAlexandra WykeNo ratings yet
- Cae Linking WordsDocument8 pagesCae Linking Wordsapi-19975062No ratings yet
- Assessment 7Document5 pagesAssessment 7api-525782290No ratings yet
- 4-5TH JANUARY 2023: Organized byDocument3 pages4-5TH JANUARY 2023: Organized byvivien kate perixNo ratings yet
- Nursing Diagnosis and Plan of Care for Anemia with Chronic DiseaseDocument6 pagesNursing Diagnosis and Plan of Care for Anemia with Chronic DiseaseChristine Joy FloresNo ratings yet
- Qip ProjectDocument13 pagesQip Projectapi-534216481No ratings yet
- Chapter 10Document45 pagesChapter 10Hannah BuquironNo ratings yet
- ATT Induced Hepatotoxicity: Dr. K. K. SharmaDocument36 pagesATT Induced Hepatotoxicity: Dr. K. K. SharmaSucharita Ray100% (1)
- Malnutrition in Critical Illness and Beyond A Narrative Review PDFDocument9 pagesMalnutrition in Critical Illness and Beyond A Narrative Review PDFEsteban DavidNo ratings yet
- F-I Drug HandbookDocument55 pagesF-I Drug HandbookGeanieveve ElnasNo ratings yet