Professional Documents
Culture Documents
9 - Reviews in Gynaecological and Perinatal Practice Volume 6 Issue 3-4 2006 (Doi 10.1016/j.rigapp.2006.04.001) Sarah Vause Stelios Christodoulou - Repeat Caesarean Section or Induction of Labour
Uploaded by
Stefani LarasatiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
9 - Reviews in Gynaecological and Perinatal Practice Volume 6 Issue 3-4 2006 (Doi 10.1016/j.rigapp.2006.04.001) Sarah Vause Stelios Christodoulou - Repeat Caesarean Section or Induction of Labour
Uploaded by
Stefani LarasatiCopyright:
Available Formats
Repeat Caesarean section or induction of labour
Sarah Vause
a,
*
, Stelios Christodoulou
b
a
Department of Obstetrics, St Marys Hospital, Hathersage Road,
Manchester M13 OJH, United Kingdom
b
Department of Obstetrics and Gynaecology, Royal Preston Hospital,
Sharoe Green Road, Preston, United Kingdom
Received 21 December 2005; accepted 3 April 2006
Available online 30 May 2006
Abstract
Obstetricians frequently need to decide whether to induce a woman who has previously been delivered by Caesarean section (LSCS).
There is very little evidence from randomised controlled trials to aid their decision making. Observational studies, with their inherent
aws, suggest a 3.6%maternal complication rate in women undergoing repeat elective LSCS, and approximately 66%vaginal delivery rate
and 1% uterine rupture rate in women who were induced. There is little evidence to guide the choice of induction agent. Various factors
have been suggested to predict a successful vaginal delivery, but a previous vaginal delivery appears to be strongly predictive of a good
outcome. Alternative strategies, such as stretching and sweeping the membranes or awaiting spontaneous labour, may reduce the need for
induction. If labour is induced in a woman with a scarred uterus we should ensure that the high risk situation is not compounded by poor
care in labour.
# 2006 Elsevier B.V. All rights reserved.
Keywords: Induction of labour; Vaginal birth after Caesarean section; Uterine rupture
1. The clinical dilemma
What should the obstetrician advise a woman whose
pregnancy has reached 41 weeks gestation? The evidence
suggests that she should be offered induction of labour as
this reduces the risk of perinatal mortality compared with
conservative management [1]. But what should that
obstetrician advise if the woman has previously had a
lower segment Caesarean section? Does the evidence still
apply, or has the balance of risk changed?
The clinician and woman have three options. They may
choose to perform a repeat Caesarean section; or they may
opt for induction by whatever method; or await spontaneous
onset of labour. What does the evidence show?
1.1. Randomised controlled trials of elective repeat
LSCS versus induction of labour
Unfortunately there are no randomised controlled
clinical trials comparing these options in women with a
previous Caesarean section and any comparative data come
from observational studies with all their inherent dis-
advantages.
1.2. Induction of labour versus awaiting spontaneous
labour
There is only one randomised trial of induction of labour
versus awaiting spontaneous labour in women with a
previous LSCS scar [2]. This trial used 200 mg mifepristone
on 2 successive days and showed a signicant increase in the
number of women who laboured within 4 days and a
reduction in oxytocin usage. The trial was too small (n = 32)
to assess maternal or fetal morbidity.
www.elsevier.com/locate/rigapp
Reviews in Gynaecological and Perinatal Practice 6 (2006) 233239
* Corresponding author. Tel.: +44 161 276 6426; fax: +44 161 276 6143.
E-mail addresses: sarah.vause@cmmc.nhs.uk (S. Vause),
stchristodoulou@hotmail.com (S. Christodoulou).
1871-2320/$ see front matter # 2006 Elsevier B.V. All rights reserved.
doi:10.1016/j.rigapp.2006.04.001
Faced with this lack of evidence from randomised
controlled trials obstetricians have to advise based on the
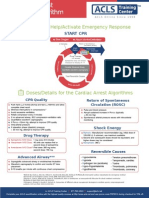
perceived balance of risks (Fig. 1).
2. What is the morbidity from elective repeat
Caesarean section?
The morbidity from elective repeat Caesarean section is
difcult to assess, as many of the large observational studies
include women who would not be suitable for a trial of
labour or induction of labour [3].
A large (n = 33,699) prospective multicentre observa-
tional study described a 3.6% maternal complication rate in
women undergoing a repeat elective LSCS and compared
this to women having a trial of labour [4]. Another
observational study by McMahon et al. has suggested that
8.4% of women would experience some morbidity (0.8%
major morbidityhysterectomy or operative visceral injury
and 7.6% minor morbiditypyrexia, transfusion or wound
infection) [5]. Rates of complications are detailed in Table 1
with gures for women having trials of labour after previous
LSCS as comparison (not all were induced).
None of the studies have examined the length of
convalescence, a factor likely to be of great importance to
a mother with a small baby who probably has at least one
other child at home.
As the risk of placenta previa, placenta accreta and
hysterectomy increase with the number of repeat LSCS, it
has recently been suggested that the number of future
pregnancies a woman is planning should be taken into
account when making the decision whether to repeat a LSCS
or induce labour [6].
3. What about the morbidity in women with a
previous LSCS who are induced?
The overall rate of morbidity in women with a previous
LSCS who are induced will depend on:
(i) the relative proportions which deliver vaginally or by
LSCS;
(ii) the rate of uterine rupture in the women who are
induced.
3.1. The relative proportions which deliver vaginally or
by LSCS
Obtaining accurate gures from the literature is difcult
because there may be
Reporting bias with authors more willing to report series
where there are high rates of vaginal delivery and low
rates of uterine rupture.
Majority of papers have relatively small numbers of
women.
Dosage regimes vary.
Several different methods of induction can be used in the
same study [710].
The choice of induction agent may be inuenced by
cervical status, the women with a less favourable cervix
receiving prostaglandin and those with the more favour-
able cervix being induced by amniotomy.
Failure to discriminate whether oxytocin is used as an
induction agent or to augment labour [11,12].
Failure to differentiate between women who have and
have not had previous vaginal deliveries [13].
Differences in cultural context [14].
Given above, it is hardly surprising that there is wide
variation in the vaginal delivery rates between studies
which range from 53% to 89% [3,1523]. In a large study
from Switzerland the vaginal delivery rate in a group of
2459 women with a scarred uterus who were induced was
65.6%, compared to a rate of 75.1% in women with a
scarred uterus who laboured spontaneously [3]. In a large
prospective multicentre observational study from the
United States the respective gures were 67% and 80%
[20].
3.2. The rate of uterine rupture in the women who are
induced
It is again difcult to obtain accurate gures from the
literature for the rate of uterine rupture in women who are
S. Vause, S. Christodoulou / Reviews in Gynaecological and Perinatal Practice 6 (2006) 233239 234
Fig. 1. Which carries more risk elective repeat LSCS or induction of
labour?
Table 1
Morbidity in women undergoing an elective repeat LSCS compared with
trial of labour
Elective
repeat
LSCS
Successful
trial of
labour
Failed
trial of
labour
Wound infection (%) [5] 2.2 0 3.3
Pyrexia (%) [5] 6.4 3.5 8.0
Operative visceral
injury (%) [5]
0.6 0.1 3.0
Transfusion (%) [4] 1.0 1.2 3.2
Thromboembolism (%) [4] 0.1 0.02 0.1
Hysterectomy (%) [4] 0.3 0.1 0.5
Maternal death (%) [4] 0.04 0.01 0.04
Mean hospital stay
(days) [6]
5.0 2.3 5.3
induced, for the same reasons outlined in the list above.
Some studies do not differentiate between asymptomatic
dehiscence and symptomatic rupture.
If the results of 14 observational studies [4,15,20,2226]
are pooled a total of 91 ruptures were described in 8841
women with a previous LSCS who were induced (1.0%).
This compares with 75 ruptures in 16,814 women (0.4%) in
these studies who laboured spontaneously. Some of the
studies did not include a spontaneous labour group. These
gures must therefore be interpreted extremely cautiously
bearing in mind the potential problems with the data
described above.
In the largest study (a multicentre prospective cohort
study from the United States) the uterine rupture rate in the
women who were induced was signicantly higher than in
those labouring spontaneously [4]. The uterine rupture rate
in women who were induced (n = 4708) was 1.0%, in those
augmented (n = 6009) was 0.9% and in the spontaneous
labour group (n = 6685) was 0.4%. In the previously quoted
large Swiss study the rate of uterine rupture in the 2459
women who were induced was 0.65% [3].
3.3. Perinatal mortality in women who are induced
In a retrospective population based study, there was no
signicant difference in perinatal mortality between women
with a scarred uterus induced with prostaglandin (3/2398),
and those with a scarred uterus undergoing a trial of labour
who did not have prostaglandins (17/13,120). Overall this
was approximately 11 times greater (odds ratio [OR], 11.6;
95% CI, 1.686.7) than the risk associated with planned
repeat Caesarean delivery (1/9014) [27].
4. How should we induce labour after previous
LSCS?
Many trials comparing different methods of induction of
labour have excluded women with a scarred uterus [28,29].
It may therefore be inappropriate to extrapolate ndings
from these trials to women who have previously been
delivered by LSCS.
There have only been two randomised controlled trials of
different methods of induction in women with previous
LSCS and both were extremely small [30,31].
One trial compared prostaglandin E2 with amniotomy
and oxytocin [30]. There was no signicant difference in
vaginal delivery rates (prostaglandin 17/21 81% versus
ARM and oxytocin 15/21 71%), and one uterine rupture in a
woman in the prostaglandin group who was also augmented
with oxytocin.
Another trial compared misoprostol with amniotomy and
oxytocin was terminated prematurely after only 38 women
had been recruited, when two uterine ruptures occurred in
the group of women treated with misoprostol [31]. The
authors recommended that misoprostol should not be used in
women with a scarred uterus.
As the numbers of women in both of these randomised
controlled trials was small (n = 42 and 38) it is impossible to
draw from them any conclusions as to which method of
induction to use.
No case control studies evaluating the relative risk of scar
rupture with different methods of induction have been
published, and therefore obstetricians can only base their
advice on observational studies.
Several papers describe cohorts of women induced by a
variety of methods after a previous LSCS [810]. However,
the outcomes described for the various methods of induction
could be prone to bias. For example, a woman with a soft
favourable cervix would be more likely to be induced with
amniotomy and oxytocin and go on to deliver vaginally, than
a woman with a long rm closed cervix who may be given
prostaglandin. The two treatment groups may therefore be
dissimilar and it would not be appropriate to compare
outcomes from the two groups.
One frequently cited study exemplies the need for
critical appraisal of the evidence [32]. It appeared to show
that compared with elective repeat LSCS, spontaneous
labour had a relative risk of 3 for uterine rupture, induction
without the use of prostaglandin had a relative risk of 5,
and induction with prostaglandin a relative risk of 16.
However no description was given of cervical status,
dosage regimes, augmentation or vaginal delivery rates.
The data for this study were obtained from computerised
administrative records such as the clinical coding on
hospital discharge summaries, with the authors acknowl-
edging frequent inaccuracies [32]. Unfortunately, the
gures from this paper are quoted in the current NICE
guideline, with no reference being made to the poor
methodology [33].
4.1. Amniotomy and oxytocin for induction after
previous LSCS
A vaginal delivery rate of 72% was achieved in an
observational study n = 32 which is comparable to that
found in the previously mentioned randomised controlled
trial [34]. In these studies no uterine ruptures were
reported in the groups induced with oxytocin. However
Zelop et al. reported nine uterine ruptures (2%) among 458
women in whom labour was induced with oxytocin alone
[35]. Unfortunately, they failed to report vaginal delivery
rates.
4.2. Prostaglandin for induction after previous LSCS
Eight studies have been identied where the use of
prostaglandin to induce women with a previous scar is the
main focus [3643]. In three studies there are no comparison
groups and three studies have fewer than 30 cases. The rates
of vaginal delivery in these studies ranged from 5084%,
S. Vause, S. Christodoulou / Reviews in Gynaecological and Perinatal Practice 6 (2006) 233239 235
with an overall vaginal delivery rate of 63% if the studies are
combined. The overall symptomatic rupture rate if all the
studies were combined was 0.6%.
5. Prostaglandins or poor care?
In the CESDI 5th annual report a focus group examined
the care of 42 women in whom a ruptured uterus was
associated with the death of the baby [44]. A disproportio-
nately large number of these women (18almost half) had
previous LSCSs and had been induced with prostaglandin.
Whilst this may initially raise concerns about the relation-
ship between prostaglandin and scar rupture, examination of
the antenatal and intrapartum care of these women revealed
that in most cases inappropriate decisions had been made or
inappropriate care given. Aspects of care criticised by the
CESDI panel were inadequate recognition of risk, inap-
propriate decisions regarding induction, inappropriate
settings for induction of a woman with a scarred uterus,
lack of involvement of senior staff, inadequate intrapartum
surveillance and lack or recognition of the overall picture as
a high risk situation.
When a woman with a previous LSCS is induced it is
important that there is ongoing recognition of the level of
risk by all members of the clinical team, and whilst we
should think carefully before starting the induction process,
we should also continue to think carefully about when to
stop the process.
6. Can we select women better?
6.1. Predicting vaginal delivery
If it were possible to predict accurately which women
would achieve a vaginal delivery the number of emer-
gency LSCS and their associated morbidity would be
reduced. Predictive features may assist the clinician and
the woman in reaching a decision about whether to
embark on induction.
Using a population of 23,286 women with one prior
LSCS, Smith et al. developed and validated a model for
predicting the risk of delivery by LSCS antenatally [45].
Factors associated with emergency LSCS were maternal
age, maternal height, male fetus, no previous vaginal birth,
prostaglandin induction of labour and birth at or after 41
weeks. Non prostaglandin induction was not predictive of
emergency LSCS. Unlike other studies the risk of Caesarean
section is estimated only using information available in the
antepartum period and therefore can aid counselling in
relation to induction of labour. Other papers have included
variables which are only available when the woman is
admitted in labour, such as cervical status and at this point
the opportunity for elective LSCS has passed and induction
is no longer necessary.
When Smith validated his model he found that 36% of
women had a predicted risk of Caesarean section of less than
20% and their overall Caesarean section rate was 10.9%.
Conversely 16.5% of women had a predicted risk of
Caesarean section of greater than 40% and their overall
Caesarean section rate was 47.7% [45]. However, more than
50% of those predicted to be high risk still achieved a
vaginal delivery.
In women with a previous LSCS who are induced, a
previous vaginal delivery and greater cervical effacement at
commencement of induction appear to positively predict a
successful outcome [25], whilst the need for augmentation is
associated with a poorer outcome [46]. Although the indica-
tion for the previous LSCS appears to predict outcome in
women who labour spontaneously, [47] it does not seem to
be predictive in women who are induced in a subsequent
pregnancy [46]. However, this may reect some degree of
selection bias as women who are considered to have had a
signicant degree of cephalopelvic disproportion previously
may not be considered suitable for induction, and therefore
do no feature in the published series.
In McNally and Turners series 64% of women with an
unfavourable cervix and no previous vaginal delivery were
delivered by LSCS, whilst in women with a previous vaginal
delivery the incidence of a repeat Caesarean section in labour
was only 4% [46]. In a series by Kayani and Alrevic, where
the majority of women were induced with prostaglandin, the
vaginal delivery rate was 44% in women with no previous
vaginal delivery and 83% in women who had delivered
vaginally [20]. In a series by Grinstead and Grobman, where
the majority of women had non prostaglandin inductions,
prior vaginal delivery was independently associated with an
increased chance of vaginal delivery (OR3.795%CI 1.97.1)
[15].
6.2. Predicting uterine rupture
In Smiths model described above the risk of uterine
rupture and the risk of uterine rupture with perinatal death
were associated with an increased predicted risk of
Caesarean section [45]. In women predicted to be at low
risk of LSCS the observed incidence of uterine rupture was
0.2% and in those predicted to be at high risk the incidence
of uterine rupture was 0.9%.
Ultrasonographic measurement of scar thickness has
been proposed as a method of predicting uterine rupture or
scar dehiscence [48]. Whilst it has been found that scar
thickness is inversely related to the frequency of defective
scars, the positive predictive value is low (11.8% for a cut
of value of 3.5 mm). No trials have been done where
women are randomised to either revealing or concealing
the results of scar thickness measurements, and therefore it
is difcult to assess the effect of this intervention on
outcome. One prospective open study with historical
controls showed no change in the overall repeat Caesarean
section rate, but more elective Caesarean sections were
S. Vause, S. Christodoulou / Reviews in Gynaecological and Perinatal Practice 6 (2006) 233239 236
performed with a compensatory reduction in emergency
procedures [49].
Avoidance of overstimulation of the uterine contractions
during induction or augmentation of labour by using
intrauterine pressure monitoring has been suggested as a
way of preventing uterine rupture. However, a series of 10
ruptures has been described in which intrauterine pressure
was monitored [50].
In 6 of the 10 cases scar rupture occurred when the uterine
activity was within normal limits, presumably reecting a
weak scar rather than an overstimulated uterus.
A recent observational cohort study has suggested that
there may be an increased incidence of uterine rupture in
women whose previous uterine incision was closed using a
single-layer technique rather than a double layer closure
[51]. However, other confounding factors may inuence
this, and the current Caesar study will address this issue in
the context of a randomised controlled trial.
7. Are there any alternatives?
As this is obviously a high risk situation to which there
are no easy or evidence based answers, it is worth
considering whether there are ways to reduce the numbers
of women for whom this decision arises.
The recent National Sentinel Caesarean Section Audit
study highlights the numbers of LSCS performed for fetal
distress without scalp pH being done, and the numbers of
LSCS performed for failure to progress without oxytocin
augmentation being used [52]. An active policy of external
cephalic version can reduce the number of LSCS performed
for malpresentation [53]. Minimising the incidence of
primary LSCS minimises the number of women where
decisions about induction or repeat LSCS have to be made in
subsequent pregnancies.
Postmaturity is the most common indication for induction
in women with a previous LSCS [52]. Evidence suggests
that the number of women requiring induction for
postmaturity can be reduced by using ultrasound scanning
to accurately date pregnancies [1].
Stretching and sweeping the membranes has been shown
to increase the number or women labouring spontaneously,
and hence reducing the numbers requiring formal induction
[54]. For every seven women who have a stretch and sweep
one induction is prevented. This is a cheap and easy evidence
based intervention which can be performed in any antenatal
clinic.
In women with a scarred uterus the wisdom of established
interventions should be critically questioned as the balance
of risks may have changed. For example, the evidence shows
that induction of labour beyond 41 weeks gestation reduces
perinatal mortality and has become an established inter-
vention [1]. However, the number needed to treat is large
(NNT = 476) which means that 476 women would need to
be induced to prevent one perinatal death. If 476 women
with a previous LSCS are induced then, based on the above
gures, it is likely that there would be four or ve uterine
ruptures with the possible death of a fetus. Under such
circumstances it appears that the balance is fairly evenly
poised!
8. Conclusion
Patient choice becomes more important when obstetri-
cians are unable to base their counselling on evidence and
very little evidence is available in relation to induction of
labour after previous LSCS.
Further research is needed to compare the alternatives
of elective repeat LSCS, induction of labour and
conservative management. Research is also needed to
determine the most appropriate method of induction in
women with a scarred uterus. However, as outcomes such
as uterine rupture are rare any such trial would need large
numbers.
Until such evidence becomes available we should
actively use interventions to reduce the number of women
in whom these decisions need to be made, and if we do
decide to induce labour should ensure that the high risk
situation is not compounded by poor care in labour.
Practice points
Patient choice becomes more important
when obstetricians are unable to base their
counselling on evidence. Very little evidence
is available in relation to induction of labour
after previous LSCS.
Evidence based interventions to reduce the
incidence of the rst LSCS should be
employed, for example external cephalic
version.
Evidence based interventions to reduce the
need for induction in women with a previous
LSCS should be employed, for example
sweeping the membranes.
Senior involvement and ongoing recogni-
tion of the level of risk are important to
ensure that a high risk situation is not
compounded by poor care in labour.
Research directions
Consideration of a randomised controlled
trial, or case control study of induction of
labour versus await spontaneous labour
versus elective repeat LSCS. The very large
numbers required may be prohibitive.
Consideration of a randomised controlled
trial of different methods of induction in
women with a previous LSCS scar. Again
S. Vause, S. Christodoulou / Reviews in Gynaecological and Perinatal Practice 6 (2006) 233239 237
recruitment of sufcient numbers of women
may make this impractical.
Prospective use of the model suggested by
Smith, and an observational study of how
this inuenced patient choice and outcome.
Comparative observational study of length
of convalescence in women who chose
repeat LSCS versus induction of labour.
References
[1] Crowley P. Interventions for preventing or improving the outcome of
delivery at or beyond term. Cochrane Database Syst Rev )2001;(2).
[2] Lelaidier C, Baton C, Benia JL, Fernandez H, Bourget P, Frydman R.
Mifepristone for labour induction after previous caesarean section.
BJOG 1994;101:5013.
[3] Rageth JC, Juzi C, Grossenbacher H, for the Swiss Working Group of
Obstetric and Gynecologic Institutions. Delivery after previous Cesar-
ean: A risk evaluation. Obstet Gynecol 1999;93:3327.
[4] Landon MB, Hauth JC, Leveno KJ, et al., for the National Institute of
Child Health and Human Development Maternal-Fetal Medicine Units
Network. Maternal and Perinatal outcomes associated with a trial of
labor after prior Cesarean delivery. N Engl J Med 2004;351:25819.
[5] McMahon MJ, Luther ER, Bowes WA, Olshan AF. Comparison of a
trial of labor with an elective second cesarean section. N Engl J Med
1996;335:68995.
[6] Pare E, Quinones J, Macones G. Vaginal birth after caesarean section
versus elective repeat caesarean section: assessment of maternal
downstream health outcomes. BJOG 2006;113:758.
[7] Hibbard JU, Ismail MA, Wang Y, Te C, Karrison T, Ismail MA. Failed
vaginal birth after a cesarean section: How risky is it? 1. Maternal
morbidity. Am J Obstet Gynecol 2001;184:136573.
[8] Sims EJ, Newman RB, Hulsey TC. Vaginal birth after cesarean: to
induce of not to induce. Am J Obstet Gynecol 2001;184:11224.
[9] Lao TT, Leung FH. Labor induction for planned vaginal delivery in
patients with previous cesarean section. Acta Obstet Gynecol Scand
1987;66:4136.
[10] Adair CD, Sanchez-Romos L, Gaudier FL, Kaunitz AM, McDyer DC,
Briones D. Labor induction in patients with previous cesarean section.
Am J Perinat 1995;12:4504.
[11] Ravasia DJ, Wood SL, Pollard JK. Uterine rupture during induced trial
of labor among women with previous cesarean delivery. Am J Obstet
Gynecol 2000;183:11769.
[12] Leung AS, Farmer RM, Leung EK, Medearis AL, Paul RH. Risk
factors associated with uterine rupture during trial of labor after
cesarean delivery: a case control study. Am J Obstet Gynecol 1993;
168(5):135863.
[13] Sakala EP, Kaye S, Murray RD, Munson LJ. Oxytocin use after
previous Cesarean: Why a higher rate of failed labor trial? Obstet
Gynecol 1990;75:3569.
[14] Cunha M, Bugalho A, Bique C, Bergstrom S. Induction of labor by
vaginal misoprostol in patients with previous cesarean delivery. Acta
Obstet Gynecol Scand 1999;78:6534.
[15] Grinstead J, Grobman WA. Induction of labor after one prior Cesarean:
predictors of vaginal delivery. Obstet Gynecol 2004;103:5347.
[16] Chattopadhyay SK, Sherbeeni MM, Anokute CC. Planned vaginal
delivery after two previous caesarean sections. BJOG 1994;101:498
500.
[17] Chattopadhyay K, Senfupta BS, Edrees YB, Lambourne A. Vaginal
birth after cesarean section: Management debate. Int J Gynecol Obstet
1988;26:18996.
[18] Del Valle GO, Adair CD, Sanchez-Ramos L, Gaudier FL, McDyer DC,
Delke I. Cervical ripening in women with previous cesarean deliveries.
Int J Obstet Gynecol 1994;47:1721.
[19] Al Suleiman SA, El Yahia AR, Al Najashi S, Rahman J, Rahman MS.
Outcome of labour in patients with a lower segment Caesarean scar. J
Obstet Gynaecol 1989;9:199202.
[20] Kayani SI, Alrevic Z. Uterine rupture after induction of labour in
women with previous caesarean section. BJOG 2005;112:4515.
[21] Landon MB, Leindecker S, Spong CY, Hauth JC, et al., for the
National Institute of Child Health and Human Development Mater-
nal-Fetal Medicine Units Network. The MFMU Cesarean Registry:
Factors affecting the success of trial of labor after previous cesarean
delivery. Am J Obstet Gynecol 2005;193:101623.
[22] Locatelli A, Regalia AL, Ghidini A, Ciriello E, Bif A, Pezzullo JC.
Risks of induction of labour in women with a uterine scar from
previous low transverse caesarean section. BJOG 2004;111:13949.
[23] Chilaka VN, Cole MY, Habayeb OMH, Konje JC. Risk of uterine
rupture following induction of labour in women with a previous
caesarean section in a large UK teaching hospital. J Obstet Gynaecol
2004;24:2645.
[24] McDonagh MS, Osterweil P, Guise JM. The benets and risks of
inducing labour in patients with prior caesarean delivery: a systematic
review. BJOG 2005;112:100715.
[25] Bujold E, Blackwell SC, Hendler I, Berman S, Sorokin Y, Gauthier RJ.
Modied Bishops score and induction of labor in patients with a
previous caesarean delivery. Am J Obstet Gynecol 2004;191:16448.
[26] Lin C, Raynor BD. Risk of uterine rupture in labor induction of
patients with prior caesarean section: An inner city hospital experi-
ence. Am J Obstet Gynecol 2004;190:14768.
[27] Smith GCS, Pell JP, Cameron AD, Dobbie R. Risk of perinatal death
associated with labor after previous Cesarean delivery in uncompli-
cated term pregnancies. JAMA 2002;287:268490.
[28] Tan BP, Kelly AJ. Intravenous oxytocin alone for induction of labour.
Cochrane Database Syst Rev )2001;(3).
[29] Botha DJ, Howarth GR. Oxytocin and amniotomy for induction of
labour. Cochrane Database Syst Rev )2001;(2).
[30] Taylor AVG, Sellers S, Ah-Moye M, MacKenzie IZ. A prospective
random allocation trial to compare vaginal prostaglandin E
2
with
intravenous oxytocin for labour induction in women previously deliv-
ered by caesarean section. J Obstet Gynaecol 1993;12:3336.
[31] Wing DA, Lovett K, Paul RH. Disruption of prior uterine incision
following misoprostol for labor induction in women with previous
cesarean delivery. Obstet Gynecol 1998;91:82830.
[32] Lydon Rochelle M, Holt VL, Easterling TR, Martin DP. Risk of uterine
rupture during labor among women with a prior Cesarean delivery. N
Engl J Med 2001;345:38.
[33] National Institute for Clinical Excellence. Caesarean section. NICE
Clinical Guideline, vol. 13. London: National Institute for Clinical
Excellence; 2004.
[34] Horenstein JM, Phelan JP. Previous cesarean section: the risks and
benets of oxytocin usage in a trial of labor. Am J Obstet Gynecol
1985;151:5649.
[35] Zelop CM, Shipp TD, Repke JT, Cohen A, Caughey AB, Lieberman E.
Uterine rupture during induced or augmented labor in gravid women
with one prior cesarean delivery. AmJ Obstet Gynecol 1999;181:8826.
[36] Yamani TY, Rouzi AA. Induction of labor with vaginal prostaglandin
E
2
in grand multiparous women with one previous cesarean section.
Int J Gyn Obstet 1999;65:2513.
[37] Flamm BL, Anton C, Goings JR, Nerman J. Prostaglandin E
2
for
cervical ripening: a multicenter study of patients with prior cesarean
delivery. Am J Perinat 1997;14:15760.
[38] Blanco JD, Collins M, Willis C, Prien S. Prostaglandin E
2
gel
induction of patients with a prior low transverse cesarean section.
Am J Perinat 1992;9:803.
[39] Goldberger SB, Rosen DJD, Michaeli G, Markow S, Ben-Nun I, Fejgin
MD. The use of PGE
2
for inductionof labor inparturients witha previous
cesarean section scar. Acta Obstet Gynaecol Scand 1989;68:5236.
S. Vause, S. Christodoulou / Reviews in Gynaecological and Perinatal Practice 6 (2006) 233239 238
[40] MacKenzie IZ, Bradley S, Embrey MP. Vaginal prostaglandins and
labour induction for patients previously delivered by Caesarean sec-
tion. BJOG 1984;91:710.
[41] Norman M, Ekman G. Preinductive cervical ripening with prosta-
glandin E
2
in women with one previous cesarean section. Acta Obstet
Gynaecol Scand 1992;71:3515.
[42] Stone JL, Lockwood CJ, Berkowitz G, Alvarez M, Lapinski R,
Valcamonico A, et al. Use of cervical prostaglandin E
2
gel in patients
with previous cesarean section. Am J Perinat 1994;11:30912.
[43] Williams MA, Luthy DA, Zingheim RW, Hickok DE. Preinduction
Prostaglandin E
2
gel prior to induction of labor in women with a
previous Cesarean section. Gynecol Obstet Invest 1995;40:8993.
[44] CESDI, 5th Annual Report, London; 1998, p. 6371
[45] Smith GCS, White IR, Pell JP, Dobbie R. Predicting caesarean section
and uterine rupture among women attempting vaginal birth after one
prior caesarean section. PLoS Med 2005;2(9):e252.
[46] McNally OM, Turner MJ. Induction of labour after one previous
Caesarean section. Aust NZ J Obstet Gynaecol 1999;39(4):4259.
[47] Lavin JP, Stephens RJ, Miodovnik M, Barden TP. Vaginal delivery in
patients with a prior Cesarean section. Obstet Gynecol 1982;59:13548.
[48] Rozenberg P, Gofnet F, Phillippe HJ, Nisand I. Ultrasonographic
measurement of lower uterine segment to assess risk of defects of
scarred uterus. Lancet 1996;347:2814.
[49] Rozenberg P, Gofnet F, Phillippe HJ, Nisand I. Thickness of the lower
uterine segment: its inuence in the management of patients with
previous cesarean sections. Eur J Obstet Gynecol Reprod Biol
1999;87:3945.
[50] Beckley S, Gee H, Newton JR. Scar rupture in labour after previous
lower uterine segment caesarean section: the role of uterine activity
measurement. BJOG 1991;98:2659.
[51] Bujold E, Bujold C, Hamilton EF, Harel F, Gauthier RJ. The impact of
single-layer or double-layer closure on uterine rupture. Am J Obstet
Gynecol 2002;186:132630.
[52] Thomas J, Paranjothy S. Royal College of Obstetricians and Gynae-
cologists Clinical Effectiveness Support Unit. National Sentinel Cae-
sarean Section Audit Report. RCOG Press; 2001
[53] Hofmeyer GJ. External cephalic version for breech presentation at
term. Cochrane Database Syst Rev )2001;(3).
[54] Boulvain M, Stan C, Irion O. Membrane sweeping for induction of
labour. Cochrane Database Syst Rev )2001;(2).
S. Vause, S. Christodoulou / Reviews in Gynaecological and Perinatal Practice 6 (2006) 233239 239
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Distillation ApparatusDocument2 pagesDistillation ApparatusStefani LarasatiNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Laporan 1Document2 pagesLaporan 1Stefani LarasatiNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Supermarket CendawanDocument3 pagesSupermarket CendawanStefani LarasatiNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Molecules 18 09933 3Document16 pagesMolecules 18 09933 3Stefani LarasatiNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Supermarket CendawanDocument3 pagesSupermarket CendawanStefani LarasatiNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Absen NeuroDocument6 pagesAbsen NeuroStefani LarasatiNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- GWK / Uluwatu Pura??: (Jumpsuit Polkadot) (Tanktop Pink)Document1 pageGWK / Uluwatu Pura??: (Jumpsuit Polkadot) (Tanktop Pink)Stefani LarasatiNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Molecules 18 09933 3Document16 pagesMolecules 18 09933 3Stefani LarasatiNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shout For Help/Activate Emergency Response: CPR StartDocument2 pagesShout For Help/Activate Emergency Response: CPR StartdavpierNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Confirm Booking Le Pirate Beach Club Gili Trawangan: Booking Reference NO:LPG1131Document1 pageConfirm Booking Le Pirate Beach Club Gili Trawangan: Booking Reference NO:LPG1131Stefani LarasatiNo ratings yet
- Dapus RKP Kitis 4Document1 pageDapus RKP Kitis 4Stefani LarasatiNo ratings yet
- Up Date in Head Injury ManagementDocument63 pagesUp Date in Head Injury ManagementStefani LarasatiNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Tamba HanDocument3 pagesTamba HanStefani LarasatiNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Journal Reading Tinea CapitisDocument22 pagesJournal Reading Tinea CapitisStefani LarasatiNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Physical Paper +1ANNUALDocument5 pagesPhysical Paper +1ANNUALprabhnoorprimeNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Bio SafetyDocument57 pagesBio SafetySatyaveer SinghNo ratings yet
- Congenital SyphilisDocument28 pagesCongenital SyphilisMeena Koushal100% (4)
- MNT For Sucrase Isomaltase DeficiencyDocument14 pagesMNT For Sucrase Isomaltase DeficiencySarah DresselNo ratings yet
- Ranula: A Review of LiteratureDocument6 pagesRanula: A Review of LiteratureNicco MarantsonNo ratings yet
- Urolithiasis PDFDocument4 pagesUrolithiasis PDFaaaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 4446 16364 1 PBDocument8 pages4446 16364 1 PBSafira Rosyadatul AissyNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Zbornik Limes Vol 2Document354 pagesZbornik Limes Vol 2Morrigan100% (1)
- Nettle Rash Symptoms, Causes, TreatmentDocument2 pagesNettle Rash Symptoms, Causes, TreatmentArdave Laurente100% (1)
- Important Uses of Neem ExtractDocument3 pagesImportant Uses of Neem ExtractAbdurrahman MustaphaNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Sas 1# - CHNDocument16 pagesSas 1# - CHNZymer Lee Perez AbasoloNo ratings yet
- Hydrocephalus IDocument52 pagesHydrocephalus IVlad Alexandra50% (2)
- Test-11 (Current Affair-2)Document86 pagesTest-11 (Current Affair-2)Pavansaikumar DasariNo ratings yet
- Angina Pectoris: Dr. Naitik D Trivedi & Dr. Upama N. TrivediDocument15 pagesAngina Pectoris: Dr. Naitik D Trivedi & Dr. Upama N. TrivediNaveen KumarNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Pharmacology ReviewerDocument21 pagesPharmacology ReviewerCzairalene QuinzonNo ratings yet
- HSSC Paper PDF (8) - WatermarkDocument15 pagesHSSC Paper PDF (8) - WatermarkJitender TanwarNo ratings yet
- Epstein Barr VirusDocument13 pagesEpstein Barr VirusDianaLorenaNo ratings yet
- JUUL Labs, Inc. Class Action Complaint - January 30, 2019Document384 pagesJUUL Labs, Inc. Class Action Complaint - January 30, 2019Neil MakhijaNo ratings yet
- Vicente vs. Employees' Compensation CommissionDocument7 pagesVicente vs. Employees' Compensation CommissionAlexNo ratings yet
- BPJ Vol 9 No 2 P 827-828Document2 pagesBPJ Vol 9 No 2 P 827-828MayerNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaAlmira PutriNo ratings yet
- Envis Newsletter April 2014Document16 pagesEnvis Newsletter April 2014Mikel MillerNo ratings yet
- MeningitisDocument21 pagesMeningitisSonya GodwinNo ratings yet
- 5388 Tech ManualDocument198 pages5388 Tech ManualMichal SzymanskiNo ratings yet
- Progestin-Only Injectables: Characteristics and Health BenefitsDocument11 pagesProgestin-Only Injectables: Characteristics and Health BenefitsRazaria DailyneNo ratings yet
- Basics of DentistryDocument65 pagesBasics of DentistryHiba Shah100% (1)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Information Bulletin A FMC Mbbs 2021Document27 pagesInformation Bulletin A FMC Mbbs 2021Bidyut Bikash BaruahNo ratings yet
- بنك طب نفسيDocument19 pagesبنك طب نفسيمحمد نادر100% (1)
- FCA (SA) Part I Past PapersDocument72 pagesFCA (SA) Part I Past PapersmatentenNo ratings yet
- Science Magazine, Issue 6657 (August 4, 2023)Document175 pagesScience Magazine, Issue 6657 (August 4, 2023)Kim LevrelNo ratings yet