Professional Documents
Culture Documents
Glaucoma
Uploaded by
beia210 ratings0% found this document useful (0 votes)
35 views59 pagesdiseases of the eye
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentdiseases of the eye
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
35 views59 pagesGlaucoma
Uploaded by
beia21diseases of the eye
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 59
Glaucoma
ANATOMY AND PHYSIOLOGY
APPLIED ANATOMY
Ciliary body- aqueous poduction
Angle of anterior chamber
Gonioscopic grading of the angle width
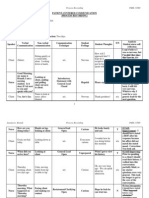
Grade Angle witdth Configuration Chances of closure Structures visible
on gonioscopy
IV 35-45 Wide open Nil SL, TM, SS, CBB
III 20-35 Open angle Nil SL, TM, SS
II 20 Moderately
narrow
Possible SL, TM
I 10 Very narrow High SL only
0 0 Closed Closed None of the angle
structures visible
APPLIED ANATOMY
Aqueous outflow system
APPLIED PHYSIOLOGY
Aqueous humour and its production
Volume
Anterior chamber: o.25 mL
Posterior chamber: 0.06 mL
Functions:
Maintains a proper intraocular pressure
Metabolic role
Maintains optical transparency
Takes place of lymph that is absent within the eyeball
APPLIED PHYSIOLOGY
Aqueous humour and its production
Refractive index: 1.336
Composition
Water: 99.9%
Solids: 0.1%
Proteins
Amino acid
Non-colloid constituents
Oxygen
Note: composition of aqueous is similar to plasma
except:
High concentrations of ascorbate, pyruvate and lactate
Low concentration of protein, urea and glucose
APPLIED PHYSIOLOGY
Aqueous humour and its production
Anterior chamber VS. posterior chamber
HCO in posterior chamber is higher than in the
anterior chamber
Cl concentration in posterior chamber is lower than in
the anterior chamber
Ascorbate concentration of posterior aqueous is
slightly higher than that of anterior chamber aqueous
APPLIED PHYSIOLOGY
Aqueous humour and its production
Production
2.3 l/min
Three mechanisms
Ultrafiltration
Secretion
Diffusion
Control of aqueous formation
APPLIED PHYSIOLOGY
Drainage of aqueous humour
Trabecular (conventional) outflow
Uveoscleral (unconventional) outflow
APPLIED PHYSIOLOGY
Maintenance of intraocular pressure
Normal IOP: 10-21 mmHg
Local factors
Rate of aqueous formation
Resistance to aqueous outflow (drainage)
Increased episcleral venous pressure
Dilatation of pupil
APPLIED PHYSIOLOGY
Maintenance of intraocular pressure
General factors
Heredity
Age
Sex
Diurnal variation of IOP
Postural variations
Blood pressure
Osmotic pressure of blood
General anaesthetics
GENERAL CONSIDERATIONS
DEFINITION OF GLAUCOMA
It is not a single disease process
Group of disorders
Characterized by a progressive optic
neuropathy
Characteristic apperance of the optic disc
Specific pattern of irreversible visual field
defects
Associated with raised IOP
CLASSIFICATION OF GLAUCOMA
Congenital and developmental glaucomas
Primary congenital glaucoma (w/o associated
anomalies)
Developmental glaucoma (w/associated
anomalies)
Primary adult glaucomas
Primary open angle glaucomas (POAG)
Primary angle closure glaucoma (PACG)
Primary mixed glaucoma
Secondary glaucomas
PATHOGENESIS OF GLAUCOMATOUS
OCULAR DAMAGE
Progressive optic neuropathy
Death of retinal ganglion cells (RGCs)
Blockage of neurothrophins from the brain
RGCs are unable to maintain normal function and
undergo apoptosis and also trigger apoptosis of
adjacent vells
RGC death is associated with loss of retinal nerve
fibers
PATHOGENESIS OF GLAUCOMATOUS
OCULAR DAMAGE
Etiology
Primary insults
Raised IOP (Mechanical theory)
Pressure independent factors (Vascular insufficiency
theory)
Failure of autoregulatory mechanism of blood flow
Vasospasm
Systemic hypotension
Other factors: e.g. acute blood loss
Secondary insults (Excitotoxicity theory)
CONGENITAL/DEVELOPMENTAL
GLAUCOMAS
TERMINOLOGY
Group of diverse disorders in which abnormal
high intraocular pressure results due to
developmental abnormalities of the angle of
anterior chamber obstructing the drainage of
aqueous humour
Types:
Primary developmental/congenital glaucoma
Developmental glaucoma with associated ocular
anomalies
PRIMARY DEVELOPMENTAL/
CONGENITAL GLAUCOMA
Abnormally high IOP which results due to
developmental anomaly of the angle of the
anterior chamber
Not associated with any other ocular or
systemic anomaly
PRIMARY DEVELOPMENTAL/
CONGENITAL GLAUCOMA
True congenital glaucoma
IOP is raised during intrauterine life and child is
born with ocular enlargment
40% of cases
Infantile glaucoma
Disease manifests prior to the childs 3
rd
birthday
50% of cases
Juvenile glaucoma
Develop pressure rise between 3-16 years of life
10% of cases
PRIMARY DEVELOPMENTAL/
CONGENITAL GLAUCOMA
Prevalence and genetic pattern
Sporadic
10% of cases exhibit an autosomal recessive
inheritance with incomplete penetrance
65% of patients are males
Diseases is bilateral in 75% cases
Disease affects only 1 child in 10,000 births
PRIMARY DEVELOPMENTAL/
CONGENITAL GLAUCOMA
Pathogenesis
Trabeculodysgenesis
Flat iris insertion
more common
Iris inserts flatly and abruptly into the thickened
trabeculum either at or anterior to scleral spur or
posterior to scleral spur
Concave iris insertion
Less common
Superficial iris tissue sweeps over the iridotrabecular
junction and the trabecululm and thus oscures the scleral
spur and ciliary body
PRIMARY DEVELOPMENTAL/
CONGENITAL GLAUCOMA
Clinical features
Photophobia, blepharospasm, lacrimation and eye
rubbing
Corneal signs:
Oedema
Enlargement
Tears and breaks in Descemets membrane
Sclera becomes thin and appears blue
Anterior chamber becomes deep
Iris may show iridodonesis and atrophic patches
PRIMARY DEVELOPMENTAL/
CONGENITAL GLAUCOMA
Clinical features
Lens becomes flat and may even subluxate
Optic disc may show variable cupping and atrophy
IOP is raised
Axial myopia
PRIMARY DEVELOPMENTAL/
CONGENITAL GLAUCOMA
Examination (Evaluation)
Measurement of IOP
Schiotz tonometer
Perkins applanation tonometer
Measurement of corneal diameter
Ophthalmoscopy
Gonioscopic examination
PRIMARY DEVELOPMENTAL/
CONGENITAL GLAUCOMA
Differential diagnosis
Cloudy cornea
Trauma, mucopolysaccharidosis, interstitial keratitis and corneal
endothelial dystrophy
Large cornea
Megalocornea
Lacrimation
Congenital nasolacrimal duct blockage
Photophobia
Keratitis or uveitis
Raised IOP in infants
Retinoblastoma, retinopathy of prematurity, persistent primary
hyperplastic vitreous, traumatic glaucoma and secondary
congenital glaucomas
PRIMARY DEVELOPMENTAL/
CONGENITAL GLAUCOMA
Treatment
Surgical but IOP must be lowered by use of
medications
Surgical procedures:
Goniotomy
Trabeculotomy
Combined trabeculotomy and trabeculectomy
DEVELOPMENTAL GLAUCOMAS WITH
ASSOCIATED ANOMALIES
Glaucoma associated with iridocorneal
dysgenesis
Glaucoma associated with aniridia
Glaucoma associated with ectopia lentis
syndromes
Glaucoma associated with phakomatosis
Miscellaneous conditions
PRIMARY OPEN ANGLE GLAUCOMA
AND RELATED CONDITIONS
PRIMARY OPEN ANGLE GLAUCOMA
No obvious systemic or ocular cause of rise in
the intraocular pressure
Eyes with open angle of the anterior chamber
Chronic simple glaucoma of adult onset
Slowly progressive raised IOP associated with
optic disc cupping and specific visual field
defects
POAG
PRIMARY OPEN ANGLE GLAUCOMA
Etiopathogenesis
Predisposing and risk factors
Heredity
Age
Race
Myopes
Diabetics
Cigarette smoking
High blood pressure
Thyrotoxicosis
PRIMARY OPEN ANGLE GLAUCOMA
Etiopathogenesis
Pathogenesis of rise in IOP
Due to decrease in the aqueous outflow facility due to
increased resistance to aqueous outflow caused by
age-related thickening and sclerosis of the trabeculae
and an absent of giant vacuoles in the cell lining the
canal of Schlemm
Corticosteroid responsiveness
More likely to respond to 6 weeks topical steroid
therapy with a significant rise of IOP
PRIMARY OPEN ANGLE GLAUCOMA
Incidence of POAG
1 in 100 of the general population above the age
40 years
PRIMARY OPEN ANGLE GLAUCOMA
Clinical features
Symptoms
Insidious and usually asymptomatic until it has caused a
significant loss of visual field
Mild headache and eyeache
Defect in the visual field
Reading and close work often present increasing
difficulties
Delayed dark adaptation
PRIMARY OPEN ANGLE GLAUCOMA
Clinical features
Signs
Anterior segment
Intraocular pressure changes
Optic disc changes
Examinations techniques
Direct ophthalmoscopy and indirect ophthalmoscopy
Slit-lamp biomicroscopy using a + 90D lens, Hruby lens
or Goldmann contact lens
Recording and documentation techniques
Serial drawings, photography and photogrammertry
Confocal scanning laser topography i.e., Heidelberg
retinal tomograph (HRT)
Optical coherence tomography
Scanning laser polarimetry i.e., Nerve fibre analyser
(NFA)
PRIMARY OPEN ANGLE GLAUCOMA
Clinical features
Early glaucomatous changes
Vertically oval cup
Asymmetry of the cups
Large cup
Splinter hemorrhages
Pallor areas on disc
Atrophy of retinal nerve fibre layer
PRIMARY OPEN ANGLE GLAUCOMA
Clinical features
Advanced glaucomatous changes in the optic disc
Marked cupping
Thinning of neuroretinal rim
Nasal shifting of retinal vessels
Pulsations of the retinal arterioles
Lamellar dot sign
PRIMARY OPEN ANGLE GLAUCOMA
Clinical features
Glaucomatous optic atrophy
All the neural tissue is destroyed and the optic nerve
head appears white and deeply excavated
Pathphysiology of disc changes
Mechanical effect
Raised IOP forces the lamina criborosa backwards and
squeezes the nerve fibres
Vascular factors
Contribute in ischemic atrophy of the nerve fibres
Cavernous optic atrophy
PRIMARY OPEN ANGLE GLAUCOMA
Visual field defects
Anatomical basis of field defects
Distribution of retinal nerve fibres
Superior and inferior radiating fibres (srf and irf)
Papillomacular bundle (pmb)
Superior and inferior arcuate fibres (saf and iaf)
Arrangement of nerve fibres within optic nerve head
PRIMARY OPEN ANGLE GLAUCOMA
Visual field defects
Progression of field defects
1. Isopter contraction
2. Baring of blind spot
3. Small wing-shaped paracentral scotoma
4. Seidels scotoma
5. Arcuate or Bjerrums scotoma
6. Ring or double arcuate scotoma
7. Roennes central nasal step
8. Peripheral field defects
9. Advanced glaucomatous field defects
PRIMARY OPEN ANGLE GLAUCOMA
Diagnosis of glaucoma field defects on HGA
single field prinout
Criteria to grade glaucomatous field defects:
Sr. Parameter Criteria for glaucomatous field defects
No. Early defects Moderate defects Severe defects
1 Mean deviation (MD) < -6 dB -6 dB 12 dB > - 12 dB
2 Corrected pattern
standard deviation
(CPSD)
Depressed to
the p<5%
Depressed to the
p <5%
Depressed to the p
<5%
3 Pattern deviation plot
Points depressed
below the p < 5%
or
Points decreased
below the p <1%
< 18 (25%)
< 10
< 37 (50%)
< 20
> 37 (>50%)
> 20
4 Glaucoma Hemifield
Test (GHT)
Outside normal
limits
Outside normal
limits
Outside normal
limits
5 Sensitivity in central 5
degree
No point <
15dB
One hemifield
may have point
sensitivity <15dB
No point has 0 dB
Both hemifield have
points with
sensitivity <15dB
Any point has 0 dB
PRIMARY ANGLE-CLOSURE
GLAUCOMA
SECONDARY GLAUCOMAS
SURGICAL PROCEDURES FOR
GLAUCOMA
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Community Medicine Learning ObjectivesDocument4 pagesCommunity Medicine Learning Objectivesbeia21No ratings yet
- Approach To The Diagnosis of A Cancer PatientDocument52 pagesApproach To The Diagnosis of A Cancer Patientbeia21No ratings yet
- Chapter 1Document14 pagesChapter 1beia21No ratings yet
- GlaucomaDocument59 pagesGlaucomabeia21No ratings yet
- 5pediatrics2.1 Neuro Exam Uerm2015bDocument6 pages5pediatrics2.1 Neuro Exam Uerm2015bbeia21No ratings yet
- Floor plan layout registration buffet entrance exitDocument1 pageFloor plan layout registration buffet entrance exitbeia21No ratings yet
- Breast AnatomyDocument53 pagesBreast AnatomyShriniwas RushiNo ratings yet
- 3PEDIA6 - Childhood Cancer UERM2015BDocument15 pages3PEDIA6 - Childhood Cancer UERM2015Bbeia21No ratings yet
- Test Taking StrategiesDocument17 pagesTest Taking Strategiesbeia21No ratings yet
- Med Ethics Report - KissingerDocument7 pagesMed Ethics Report - Kissingerbeia21No ratings yet
- Cestodes 2Document3 pagesCestodes 2beia21No ratings yet
- Psychiatric History ImdDocument17 pagesPsychiatric History Imdunno hiquianaNo ratings yet
- Pharma Sales HandbookDocument16 pagesPharma Sales Handbookbeia21No ratings yet
- Goldmining PDFDocument7 pagesGoldmining PDFbeia21No ratings yet
- 225 Primary Biliary CirrhosisDocument3 pages225 Primary Biliary Cirrhosisbeia21No ratings yet
- Epidemiology Case ReportDocument5 pagesEpidemiology Case Reportbeia21No ratings yet
- Bright Future Invest 2013Document1 pageBright Future Invest 2013beia21No ratings yet
- Diseases of Thyroid and Parathyroid GlandDocument60 pagesDiseases of Thyroid and Parathyroid Glandbeia21No ratings yet
- AT&T AGENT'S GUIDE TO VALUING CUSTOMERSDocument4 pagesAT&T AGENT'S GUIDE TO VALUING CUSTOMERSbeia21No ratings yet
- Interconversion of Sugar From Aldose To KetoseDocument7 pagesInterconversion of Sugar From Aldose To Ketosebeia21No ratings yet
- The Antimicrobial Effects of Centella Asiatica CreamDocument1 pageThe Antimicrobial Effects of Centella Asiatica Creambeia21No ratings yet
- Elem Trad CdsDocument2 pagesElem Trad Cdsbeia21No ratings yet
- Love Different Week 1Document2 pagesLove Different Week 1Suzaine AmbayecNo ratings yet
- Philam Life ProductsDocument3 pagesPhilam Life Productsbeia21No ratings yet
- 1200 Calorie Diet Menu PlanDocument12 pages1200 Calorie Diet Menu PlanJanet SanchezNo ratings yet
- We BoundariesDocument1 pageWe Boundariesbeia21No ratings yet
- 1200 Calorie Diet Menu PlanDocument12 pages1200 Calorie Diet Menu PlanJanet SanchezNo ratings yet
- Abundance Plus Client Presentation PDFDocument20 pagesAbundance Plus Client Presentation PDFbeia21No ratings yet
- Low Back PainDocument3 pagesLow Back Painbeia21No ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Contemporary Buddhism Volume Issue 2019 (Doi 10.1080 - 14639947.2018.1576292) Lee, Kin Cheung (George) Chez Kuang, Ong - The Satipa Hāna Sutta - An Application of Buddhist Mindfulness For CounselloDocument16 pagesContemporary Buddhism Volume Issue 2019 (Doi 10.1080 - 14639947.2018.1576292) Lee, Kin Cheung (George) Chez Kuang, Ong - The Satipa Hāna Sutta - An Application of Buddhist Mindfulness For Counsellosugianto zhong YanfengNo ratings yet
- NICU ReportDocument7 pagesNICU ReportoapsdoaksdokaNo ratings yet
- Neuromodulation NotesDocument7 pagesNeuromodulation NotesShashankChaurasiaNo ratings yet
- Application of Attachment Theory To The Study of Sexual AbuseDocument11 pagesApplication of Attachment Theory To The Study of Sexual AbuseBea100% (3)
- Heritage Village ProjectDocument24 pagesHeritage Village ProjectHaindava Keralam50% (2)
- 360 Process Recording TemplateDocument13 pages360 Process Recording Templateapi-252910411100% (9)
- Uterine Fibroids: Causes, Symptoms and Treatment OptionsDocument25 pagesUterine Fibroids: Causes, Symptoms and Treatment OptionssyifasfNo ratings yet
- Cord Blood Banking Opening New Avenues for India's Growing Medical Tourism IndustryDocument29 pagesCord Blood Banking Opening New Avenues for India's Growing Medical Tourism IndustryPreeti KashyapNo ratings yet
- ADHD Screening Test PDFDocument20 pagesADHD Screening Test PDFdcowan94% (17)
- Schizoaffective With Bipolar DisordersDocument14 pagesSchizoaffective With Bipolar DisordersNaomi MasudaNo ratings yet
- Medical-Surgical Nursing Course OverviewDocument89 pagesMedical-Surgical Nursing Course OverviewMusa yohanaNo ratings yet
- Skin Test Procedure For UVRDocument4 pagesSkin Test Procedure For UVRVenice Camille PatricioNo ratings yet
- Flexor Tendon Injuries. Hand Clinics. 2005Document152 pagesFlexor Tendon Injuries. Hand Clinics. 2005k2rojo100% (2)
- Significance of History Taking Oral SurgeryDocument32 pagesSignificance of History Taking Oral SurgeryFourthMolar.com0% (1)
- Functional Gastrointestinal Disorders in ChildrenDocument3 pagesFunctional Gastrointestinal Disorders in ChildrenEsosa ObakpolorNo ratings yet
- CounselingDocument23 pagesCounselingrashmi patooNo ratings yet
- Assessing A Couple Relationship and Compatibility Using MARI Card Test and Mandala DrawingDocument7 pagesAssessing A Couple Relationship and Compatibility Using MARI Card Test and Mandala DrawingkarinadapariaNo ratings yet
- Test Bank For Abnormal Psychology 17 e Jill M Hooley James N Butcher Matthew K Nock Susan MinekaDocument4 pagesTest Bank For Abnormal Psychology 17 e Jill M Hooley James N Butcher Matthew K Nock Susan MinekaLucretia Hoffer100% (33)
- Understanding AuriculotherapyDocument4 pagesUnderstanding AuriculotherapyFelipe de Jesus HernandezNo ratings yet
- HeartsInHarmony PDFDocument103 pagesHeartsInHarmony PDFVanessa100% (9)
- ChemoDocument32 pagesChemoJehannah Dayanara HayudiniNo ratings yet
- KELOMPOK I Dexrazoxane (SHINee Farma)Document24 pagesKELOMPOK I Dexrazoxane (SHINee Farma)yustirahayuNo ratings yet
- 2014 Fokke GBS Brighton Brain 2014Document11 pages2014 Fokke GBS Brighton Brain 2014Hikmat SatriaNo ratings yet
- Peritoneal DialysisDocument5 pagesPeritoneal DialysisLisette TupasNo ratings yet
- Guideline for Hepatitis C in Chronic Kidney DiseaseDocument107 pagesGuideline for Hepatitis C in Chronic Kidney DiseaseAndreea Livia DumitrescuNo ratings yet
- European PRM Board ExamDocument23 pagesEuropean PRM Board ExamAmer WasimNo ratings yet
- Lumbar Traction Review2Document9 pagesLumbar Traction Review2Phooi Yee LauNo ratings yet
- ACCP Anticoagulation Guidelines SummaryDocument11 pagesACCP Anticoagulation Guidelines Summaryd40sithui100% (3)
- CV Iptec LDocument9 pagesCV Iptec Lapi-457833798No ratings yet
- Clinical Pharmacology in Healthcare, Teaching and ResearchDocument80 pagesClinical Pharmacology in Healthcare, Teaching and ResearchVNcomer100% (1)