Professional Documents
Culture Documents
Cytokine Gene Polymorphism and Immunoregulation in Periodontal Disease
Uploaded by
kochikaghochiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cytokine Gene Polymorphism and Immunoregulation in Periodontal Disease
Uploaded by
kochikaghochiCopyright:
Available Formats
Cytokine gene polymorphismand
immunoregulationinperiodontal
disease
John J. Taylor, Philip M. Preshaw & Peter T. Donaldson
It has long been appreciated that the key to under-
standing the pathogenesis of periodontal disease lies
in understanding the details of host immune
responses to oral bacteria. It is equally rmly estab-
lished that cytokines play a central role in the inam-
matory processes associated with gingivitis and
initial tissue destruction in periodontal disease as
well as regulation of the adaptive immune responses
that might govern disease progression and clinical
outcome (64, 139). Understanding what triggers
inappropriate tissue destructive host responses is
central to providing rational diagnostic and thera-
peutic strategies for this condition. It is clear that
there is signicant individual variation in the develop-
ment and progression of periodontitis. Periodontitis
is initiated by a pathogenic subgingival microora
(37), but the presence of a pathogenic microora
alone is insufcient to cause disease. There are sig-
nicant variations in the disease experience of
individuals with the same periodontal pathogens,
as well as variation in the microbial composition
between individuals and between affected sites in
the same individual. Cluster analyses have revealed
that certain bacterial species frequently occur
together in complexes (169) and it is now recognized
that the relative balance between different bacterial
species is the important determinant in the develop-
ment of disease (73).
In addition to inter-individual variations in period-
ontal microbiology, the nature of the host immune
inammatory response to the presence of subgingi-
val plaque varies signicantly between individuals
(137). The concept of high- and normal-responders
has been postulated (138) in which high-responders
produce elevated quantities of inammatory media-
tors and destructive cytokines as part of their host
inammatory response to the presence of plaque
(hyper-responsive individuals). Consequently, these
individuals are more susceptible to periodontitis
than normal-responders, who produce minimal
levels of inammatory mediators for a given bacterial
challenge and do not demonstrate signicant period-
ontal breakdown. Thus, the concept of individual
disease susceptibility has emerged as a focus for
understanding disease pathogenesis (1). Further-
more, several comprehensive and detailed recent
reviews have presented convincing evidence for a
heritable component to both susceptibility and pro-
gression or severity in periodontal diseases (10, 75
77, 86, 130, 156). Our understanding of the pathogen-
esis of periodontal disease will be greatly enhanced
by investigating the role of inherited variability in the
host immune responses.
Inter-individual variations in host immune
responses to both self and non-self antigen are well
described in immunology. There is an established
literature on inter-individual variation in the major
histocompatibility complex (MHC) and how genetic
differences in immune-cell development and antigen
presentation may contribute to susceptibility to
autoimmune and infectious diseases (84, 124). More
recently, attention has focused on inherited variation
in immunoregulatory genes which map outside the
MHC, especially the cytokine genes (34, 85). The
central concept for this research has been that inher-
ited variations in cytokine genes determine the var-
iation in the biological response to stimulation with
antigen. Inherited variation in cytokine levels may
predispose to events favoring the development of
disease. If such polymorphism inuences cytokine
production, then the natural corollary is that it may
also determine inter-individual variation in outcome
158
Periodontology 2000, Vol. 35, 2004, 158182 Copyright
#
Blackwell Munksgaard 2004
Printed in Denmark. All rights reserved
PERIODONTOLOGY 2000
following exposure to infectious agents. Since these
polymorphisms are inherited through the germ-line,
this genetic variation may form the heritable compo-
nent of periodontal disease (107). It is important,
however, that we appreciate from the outset that
the presence or absence of a particular cytokine poly-
morphism may not directly translate into a detect-
able clinical phenotype. Periodontal diseases are
complex diseases in which genetic factors, microbial
factors, and the presence of environmental and
acquired systemic and local risk factors all play a role
in determining disease progression. The challenge
for researchers in this area is not, therefore, limited
to demonstrating associations between genetic poly-
morphism and periodontal disease but extends to
understanding how these genetic factors might inter-
act with other risk factors. The human genome pro-
ject and the immediate post-genomic era has
brought an explosion of new information about
genetic variation in man and the real promise that
we will be able to add new dimensions to our under-
standing of complex diseases such as periodontal
disease. It is therefore timely that we review the cur-
rent state of our knowledge with respect to cytokine
gene polymorphism and immunoregulation in peri-
odontal disease.
Cytokines and periodontal disease
Cytokines have a pivotal role in the
initiation of periodontitis
The central role of cytokines in focal immunopathol-
ogies such as periodontal disease is reected by their
properties: they are effective in very low concentra-
tions, are produced transiently and act locally in the
tissue where they are produced (141). They are often
self-regulatory, able to induce their own expression
in an autocrine or paracrine fashion and have pleio-
tropic actions on a number of cell types. Cytokines
act on their target cells by binding to specic recep-
tors and initiating intracellular second messengers
resulting in phenotypic changes in the cell via altered
gene regulation (15). There is signicant overlap and
redundancy between the function of individual cyto-
kines. The consequence of this is that individual
cytokines do not act in isolation but rather as a ex-
ible, complex network bringing together elements of
both innate and adaptive immunity in the defense
against infection and disease (12). The analysis of the
function of individual cytokines, the determination
of the inuence of factors such as genetic poly-
morphism which may affect cytokine regulation,
and the interpretation of these data in the context
of immune responses represent signicant chal-
lenges.
A large body of work from in vivo and in vitro ana-
lyses of human tissues as well as studies in animal
models strongly supports the notion that cytokines
play a key role at all stages of the immune response
in periodontal disease (64, 117, 139). Periodontal
disease has all the immunologic and pathologic
features of a persistent infection in which a progres-
sion from acute to chronic inammation is a key
feature; the cytokines which have important roles in
periodontal pathogenesis reect this fact. Therefore,
proinammatory cytokines such as interleukin-1b
(IL-1b) and tumor necrosis factor-a (TNF-a) have a
key role in the initiation, regulation and perpetuation
of innate responses in the periodontium (3, 15, 36,
64). This results in vascular changes and migration of
effector cells such as neutrophils into the period-
ontium commensurate with an appropriate immune
response aimed at containing and eradicating
periodontal pathogens. However, the chronic persis-
tence of subgingival plaque bacteria coupled with
inappropriate cytokine responses can lead to inam-
mation and concomitant tissue damage. Certainly,
it is well established that both IL-1b and TNF-a have
a variety of biological activities that are known to
underpin tissue damage in chronic inammation,
including periodontitis (139).
Cytokine responses are elicited by bacterial cell
surface molecules and secreted products which
penetrate the gingiva (36). Thus a variety of cell types
have been shown to secrete IL-1b and TNF-a in
response to periodontal bacteria (41). Macrophages
are likely to be the most important source of these
mediators in the early stages of gingival inamma-
tion, although other leukocytes such as the B cell
may be the primary source in advanced periodontal
disease (160). The central importance of IL-1b and
related cytokines is evidenced by data clearly asso-
ciating elevated levels of these cytokines with the
inammatory processes in periodontal disease. Thus
tissue IL-1b levels are higher in the gingiva of
patients with periodontal disease than in tissue from
healthy subjects (88) and higher in active periodon-
titis sites than in stable sites (171). Furthermore,
there are increased levels of IL-1b in gingival crevice
uid (GCF) of periodontitis patients (122, 146)
and IL-1b is rapidly elevated in the GCF during
experimental gingivitis (79). TNF-a from monocytes
and macrophages has synergistic effects with IL-1
cytokines, although TNF-a is somewhat less potent
Cytokine gene polymorphism and immunoregulation
159
than IL-1 (139). Also, there are increased numbers of
IL-1b-containing cells in periodontitis as compared
to both TNF-a and IL-1a-containing cells (172).
IL-1b is a potent stimulator of connective tissue
destruction, including breakdown of both periodon-
tal ligament and alveolar bone (109, 175). IL-1b also
induces cells such as broblasts and neutrophils to
secrete matrix metalloproteinases and prostaglan-
dins which further enhance destructive processes
in the inamed periodontium (137, 138).
Other cytokines have a proinammatory role in
periodontitis. Thus IL-6 is expressed by a wide vari-
ety of cells in the periodontal lesion and, in common
with IL-1 and TNF-a, enhances bone resorption (92,
139). IL-8 is a chemoattractant cytokine (chemokine)
with a proinammatory role in periodontal disease
serving as a potent chemoattractant and activator of
neutrophils (182). There is, as yet, no direct evidence
for a role of other recently described proinamma-
tory cytokines such as IL-18 in periodontal disease
(160).
It is important to emphasize that these proinam-
matory cytokines play other roles in immune
responses. For example IL-1a and IL-1b regulate
immunoglobulin G2 (IgG2) synthesis which may be
of critical importance in immune responses to car-
bohydrate antigens from certain periodontal bacteria
(94). IL-6 is an important regulator of B-cell
responses (92, 139). It is well-established that proin-
ammatory cytokines such as those of the IL-1 family
have a primary role in periodontal inammation, but
discovery of cytokines able to downregulate these
mediators will also be of central importance in
understanding immunoregulatory circuits and the
processes that mediate disease susceptibility and
progression. In this regard, both IL-10 and IL-11
are able to downregulate IL-1 production (160).
The importance of proinammatory cytokines in
periodontal health and disease has recently been
reinforced by studies in animal models demonstrat-
ing the therapeutic value of IL-1 inhibitors (40).
Cytokine networks underpin disease
progression and chronic inflammation
in periodontal disease
The progression of gingivitis to established period-
ontal disease is of primary clinical importance and
elucidation of the immunopathogenesis is central to
our understanding. In the early stages of inamma-
tion, proinammatory cytokines secreted by acti-
vated monocytes, macrophages and other cells (e.g.
broblasts, epithelial and endothelial cells) will
predominate. The macrophage is a key cell in the
progress of periodontal disease from an acute ina-
mmatory condition to a chronic pathology mediated
by elements of the adaptive immune response (109).
Local tissue macrophages secrete chemokines such
as IL-8 and macrophage/monocyte chemoattractant
protein (MCP-1) that encourage the recruitment of
additional monocytes (which develop into tissue
macrophages) as well as lymphocytes, which are
directly activated by macrophages. It is clear from
histologic studies of established periodontal lesions
that the predominant cell type of the chronic lesion is
the lymphocyte (140, 159). These cells are the source
of a variety of cytokines that have a central role in
local immunoregulatory circuits and in perpetuating
the destructive aspects of chronic inammation.
Indeed, the nature of the cytokine response is
considered critical in determining the progression
of periodontal disease; an appropriate cytokine
response will lead to a protective immune response
and stable periodontal disease, whereas an inap-
propriate cytokine response will lead to destructive
immune responses and disease progression (64, 160).
The cytokine milieu can inuence the development
of particular subsets of T cells and dendritic cells and
can direct immune responses towards tolerance or
immunity.
Much research has focused on T-cell subsets and a
central paradigm of immunoregulation to emerge in
the last decade is based on the recognition that dur-
ing immune responses to infection, distinct subpo-
pulations of T cells develop and that these subsets
can be distinguished by their cytokine secretion pro-
le (119). The dogma that has emerged is that the
cytokine secretion proles of Thl and Th2 cells are
related to their function. Type 1 cytokines (IL-2, IL-12,
IL-15, interferon (IFN)-g) mediate Th1 responses and
are primarily involved in cell-mediated immunity.
Type 2 cytokines (IL-3, IL-4, IL-6, IL-10, IL-13) med-
iate Th2 responses and are primarily involved in
humoral (antibody-mediated) immunity. There is
also reciprocal regulation of the development of
Th1 and Th2 cells through the action of IFN-g and
IL-10 (119).
There is evidence that one or other of these subsets
predominate in immune responses mediated by par-
ticular functions (39). However, if these effector
responses become dysregulated, damaging patholo-
gic reactions can ensue. This model has been
extended to periodontal disease and evoked to
explain the immunologic differences between stable
and progressive lesions (64, 160). IFN-g secretion is a
key feature of Thl responses serving to promote a
160
Taylor et al.
cell-mediated response elicited by the phagocytic
activity of macrophages and neutrophils. Develop-
ment of T cells into a Thl phenotype is stimulated
by IL-12. There is an analogy with delayed-type
hypersensitivity, often associated with chronic infec-
tions, in which a macrophage/T-cell-dominated
pathology leads to a contained lesion. In theory,
IFN-g secretion by T cells and the presence of IL-
12 would be key features of a stable periodontal
lesion (160). IL-4 secretion is central to the activity
of Th2 cells, activating B cells and enhancing the
antibody-mediated immune response. IL-4 secretion
by Th2 T cells would lead to B-cell activation and
possibly to the excessive and chronic production of
IL-1, leading to tissue destruction. A Th2 response
could therefore be a feature of a progressive, destruc-
tive lesion (160).
Entirely consistent results supporting a role for
Thl- or Th2-dominated regulatory circuits in all
forms of periodontal disease have proved difcult
to obtain (160). The reasons for this may be technical
issues or the variable cytokine secretion prole of T
cells isolated from periodontal lesions may reect a
dynamic property of immunoregulatory circuits
mediated by T cells and the synthesis of immune
responses to different antigens (26). Nevertheless,
the weight of evidence suggests that a cytokine pro-
le reecting a dominance of Th2 T cells is present in
the majority of progressive periodontal lesions and
supports a central role for T-cell-derived cytokines in
determining disease activity (102, 160, 198).
A further subset of T cells has been described on
the basis of a cytokine secretion prole and function
distinct from that of either Thl or Th2 cells; these T
regulatory (Tr) cells have a role in maintaining peri-
pheral tolerance and immune homeostasis in muco-
sal tissues (71). There is also increasing evidence that
they are induced against bacterial antigens (128).
Their development and function is mediated mainly
through the action of IL-10 and a role in suppression
of Th1-mediated immune responses has been pro-
posed (128). Tr cells may therefore inuence Thl/Th2
effector functions and a role for this T-cell subset in
local immunosuppression contributing to chronic
infection has been proposed (128). Although there is
no direct evidence for a role of Tr cells in periodontal
pathogenesis, it is reasonable to propose that a cyto-
kine milieu in the periodontium including IL-10 from
Th2 cells would promote Tr-cell activity with conco-
mitant suppression of cell-mediated responses. More
recently, it has been recognized that dendritic cells
also exist in subsets inuenced by and secreting
either type 1 or type 2 cytokines (11). It is reasonable
to propose that a network of immunoregulation in
chronic infections may develop with T cells and den-
dritic cells as the key cellular elements driven by the
action of particular groups of pleiotropic cytokines.
Understanding the extent to which variation in the
genome determines inter-individual variation in
cytokine-mediated immune responses may be the
key to understanding individual disease susceptibil-
ities. An overview of cytokines and immunoregula-
tion in periodontal disease would have to conclude
that numerous cytokines are involved in a complex
network of interactions. However, it is possible to
identify cytokines which seem to be of fundamental
and central importance to the initiation and regula-
tion of immune responses in periodontal disease.
This list includes the IL-1 cytokines, TNF-a and
IL-10 and there are already published studies of the
role of the genes encoding these cytokines in period-
ontal disease.
IL-1 cytokines are regulated at a
number of levels
Cytokines are regulated at the level of synthesis,
secretion and biological activity. Much is known
about the regulation of the IL-1 cytokines and these
serve as a useful paradigm, although our knowledge
is far from complete. The three cytokines originally
described as the members of the IL-1 family were
IL-1a and IL-1b, which have agonist activity, and
IL-1Ra, a physiologic antagonist to the other IL-1
cytokines (43, 44). IL-1 cytokines are of fundamental
importance in health and disease as evidenced by
their wide-ranging roles in innate and adaptive
immune responses and in the generation of inam-
matory reactions and by the variety of target cells
that are responsive to IL-1. The IL-1 cytokines are
made by a variety of cells and, in particular, stimu-
lated monocytes, macrophages and epithelial cells.
These functionally similar molecules are encoded on
separate genes in the same region of chromosome 2
(134). More recently, six novel proteins have been
identied from cDNA databases and the genes
encoding these IL-1 family-members map to the
same 400 kb region of the genome (48, 135, 167,
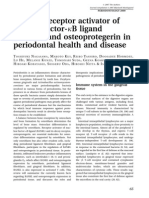
176) (Fig. 1). Although these new members have
yet to be fully characterized, they include proteins
with agonist and antagonist activities and the
restricted expression of some members indicates
potentially specialized function in particular tissues
(48, 135, 167, 176).
Analysis of the biochemical processes governing
IL-1 synthesis, secretion and biological activity reveals
161
Cytokine gene polymorphism and immunoregulation
many proven and potential opportunities for regula-
tion (6, 164). In contrast to IL-1b, IL-1a is generally
not found in the circulation or tissue uids but is
retained by the cell in intracellular and membrane-
bound forms and is active in both the pro-IL-1a and
mature IL-1a forms (44). Our knowledge of the tran-
scriptional regulation of IL-1a is by no means com-
plete. A regulatory site between positions 73 to 24
in the IL1A promoter was identied (60). Also, two
binding sites for the transcription factor AP-1 exist in
the IL1A promoter (between bases at positions 63
and 49 and 12 to 6); the former regulates basal
promoter activity and the latter is bound by nuclear
protein induced by lipopolysaccharide. although its
role in transcriptional control is not clear (4, 9, 44).
There are two nuclear factor kB (NFkB) binding sites
in the IL1A locus, at 1065/1056 and 646/655
(133). Recently, two GCC motifs in the 65 to 41
region of the IL1A promoter have been shown to
contribute to IL-1a regulation but the transcription
factors which bind these structures have not yet been
characterized (199). In summary, although our
knowledge is incomplete, several studies indicate
that the 65 to 41 region of the IL1A promoter is
important in transcriptional regulation.
Transcriptional regulation of IL-1b is dependent
on the activity of a series of transcription factors
exerting their effects at the proximal promoter of
IL1B and the region between 131 and 12 is suf-
cient to direct cell-type-specic expression of a
reporter gene (164). The myeloid specic transcrip-
tion factor Spi-l/PU.1 binds to at least two sites (50/
39 and 115/97) in the IL1B promoter and reg-
ulates tissue specic gene transcription (106).
Nuclear factor of IL-6 (NFIL6) is another transcrip-
tion factor which inuences IL1B transcription.
NFIL6 is constitutively expressed by monocytes
and is activated by lipopolysaccharide and cytokines
such as TNF-a, exerting its activity by binding to the
IL1B promoter at two separate sites (90/82 and
40/32) (200). NFIL6 and Spi1/PU.1 act synergis-
tically in the transcriptional regulation of IL1B (197).
Signicantly, a third transcription factor, HSF-1,
appears to repress IL1B transcription by binding to
NFIL6 (195). Other transcription factors associated
with IL1B modulation include CREB, lipopolysac-
charide/IL-1-inducible STAT and NF-kB (132, 183).
At the post-transcriptional level, there is a transi-
ent accumulation of IL-1b mRNA in response to cell
stimuli, and regulation of mRNA activity is thought to
occur by a transcriptional repressor and regulation of
mRNA half-life (58, 95). Certain stimuli (e.g. lipo-
polysaccharide) will promote translation of proIL-1b
mRNA by stabilizing mRNA (157, 158). Unlike
proIL-1a, proIL-1b only has marginal biological
activity and needs to be cleaved to yield the active
IL-1b peptide, which is transported out of the cell
where it exerts its biological activity. In addition to
lipopolysaccharide, cytokines such as TNF-a and IL-
1b itself stimulate IL-1 cytokine release. Therefore a
positive feedback loop contributes to the regulation
of IL-1 (45).
The antagonist IL-1Ra exists in two forms. The
intracellular form icIL-1Ra functions to modulate
IL-1a activity. The extracellular, secreted form
sIL-1Ra binds to IL-1 receptors (principally IL-1R1)
Fig. 1. The Interleukin-1 gene cluster. Diagram of the IL-1
cluster (after Nicklin et al. (135)) illustrating the position
of known genes (shaded boxes) and genetic polymorph-
isms within a 500 kb region of chromosome 2. The chev-
rons with the gene symbols indicate the direction of
transcription. Detailed descriptions of the IL1 polymorph-
isms and technical details relating to their analysis are
described elsewhere (13, 14, 65, 78, 135).
50Kb
<IL1A <IL1B
IL1F6>
IL1F7> IL1F9>
IL1F10> IL1RN> <IL1F8
IL1F5>
SNP -889 promoter
Trinucleotide repeat intron 4
SNP +4854 exon 5
Dinuculeotide repeat intron 5
46bp VNTR intron 6
SNP -31 promoter
SNP -511 promoter
SNP +3954 exon 5
2 other SNPs
SNP +2018 exon 2
86bp VNTR intron 2
9 other SNPs
gaat.p33330
tetranucleotide
repeat
Y31
Dinucleotide repeat
162
Taylor et al.
without inducing signal transduction thereby acting
as an antagonist to IL-1b. This is highlighted by in
vivo studies in man which reveal that although as
little as 1 ng.kg
1
IL-1a elicits symptoms, as much
as 10 mg.kg
1
IL-1Ra has no agonistic effect (67,
179).
Two IL-1 receptors are found on the surface of
responsive cells, IL-1RI and IL-1RII (166). Signi-
cantly, the genes for these receptors are located
downstream of the IL-1gene cluster on chromosome
2. IL-1RI is the primary signal transducing receptor;
IL-1RII binds IL-1b but lacks a cytosolic signal trans-
duction domain. It is thought that IL-1RII acts as a
`decoy' receptor binding IL-1b, preventing activation
of the signal transducing IL-1RI (28). There are only
low numbers of these receptors on target cells, as few
as 50 molecules per cell in some instances. It is
thought that the low numbers of receptors are
explained by the high afnity of IL-1b for IL-1RI,
augmented by the presence of the IL-1 receptor
accessory protein (IL-1R-AcP) (68). There are soluble
forms of both IL-1 receptors and the circulating
levels of these molecules increase in inammatory
conditions (6). IL-1R, the IL-18 receptor and the Toll-
like receptors share highly conserved cytoplasmic,
Toll/IL-1R (TIR) domains (136). Stimulation of cells
via these receptors has common features including
formation of complexes with accessory proteins (e.g.
IL-1RAcP) and interaction with cytoplasmic adap-
tor molecules (e.g. TNFR-associated factors (TRAFs)),
which subsequently oligomerize, leading to signal
transmission of the inammatory response via the
mitogen-activated protein kinase (MAPK) and NF-kB
pathways (111). The signaling pathways activated by
IL-1RI are a complex network of interacting elements
and therefore provide many further opportunities for
physiologic (and therapeutic) regulation of the bio-
logical activity of IL-1. An example of this is the anti-
inammatory action of glucocorticoids which mod-
ulates proinammatory signaling pathways at a
number of levels (111).
Regulation of IL-1 is a critical element of immune
responses in health and disease; it is established that
low levels of IL-1 are benecial in host responses to
infection, but that elevated levels can be detrimental
and that the margin between benecial effects of
these cytokines and pathologic effects is very small.
This is evidenced by data relating circulating levels of
IL-1 to disease severity in conditions associated with
dysregulated inammatory responses (20). In sum-
mary, there is accumulating but incomplete data on
the molecular genetic elements which regulate IL-1
production. However these are only one level at
which IL-1 cytokines are regulated. It is in this con-
text that the effects of genetic polymorphism on
cytokine regulation must be considered.
Cytokine gene polymorphism
Inter-individual genomic variations are
mainly encoded by single nucleotide
polymorphisms (SNPs)
Genetic polymorphisms have historically been used
as genetic markers to locate disease-causing genes
through linkage studies. However, there is increasing
appreciation that they may directly inuence com-
plex common diseases via a direct effect on gene
function. By denition, a genetic polymorphism is
a nucleotide sequence at a particular position in
DNA molecules exhibiting at least two structural var-
iants (alleles) that occur in the population at a fre-
quency of greater than 1%. There are a number of
different types of nucleotide structure in the human
genome that t this denition.
Minisatellitevariablenumber tandemrepeat (VNTR)
polymorphisms are highly polymorphic and there-
fore potentially informative as genetic markers (96).
However, minisatellite VNTRs are not evenly dis-
persed in the genome, tending to be concentrated
in discreet regions such as the telomeres. Further-
more, due to their size they are not easily detected by
polymerase chain reaction and therefore are not
amenable to high throughput technologies.
Microsatellite polymorphisms are small arrays of
tandem repeats of simple, short sequences of nucleo-
tides (most frequently 14 bases), e.g. CA
n
(190).
Microsatellites occur more evenly throughout the
genome and are more numerous than minisatellites,
forming up to 0.5% of the total genome sequence.
Although they are highly polymorphic and have been
popular as genetic markers, their use is limited by the
fact that, on average, they only occur at a frequency
of 1 every 30 kb in the genome.
A single nucleotide polymorphism (SNP) is a varia-
tion in the identity of a single nucleotide at a parti-
cular site in the genome. The SNP denes two alleles
for which there could be three genotypes amongst
individuals in a given population. SNPs include, but
are not limited to, restriction fragment length poly-
morphisms (RFLPs), i.e. nucleotide changes that cre-
ate or destroy sites for restriction endonucleases in
the DNA molecule.
There is a wealth of information in the literature
revealing the presence of SNPs in and around most
163
Cytokine gene polymorphism and immunoregulation
genes and they are therefore considered to be the
primary source of functional sequence variation
between genomes (22). Data generated by the Inter-
national SNP Consortium as well as information
from the analysis of overlapping clones by the Inter-
national Human Genome Sequencing Consortium
reveal that there is an SNP every 1.91 kb in the entire
genome sequence (23, 151). Signicantly, SNPs are
even more frequent in coding sequences (1 per
1.08 kb in genes); 93% of genes have a SNP and
98% are within 5 kb of a SNP. Furthermore, detection
of SNPs is compatible with high throughput technol-
ogies (115, 189). To date, some 1.8 million SNPs have
been identied within the human genome. SNPs are
easily detectable using both traditional polymerase
chain reaction-based methods and evolving high-
throughput technologies. SNPs in promoter regions
or enhancer sequences may encode difference in
gene transcription, and those in exons may alter
the protein sequence and thereby inuence biologi-
cal function. Thus, SNPs constitute excellent candi-
dates as genome-wide markers in linkage and
association studies and variation encoded by SNPs
may relate to phenotypic diversity and susceptibility
to complex polygenic disease (23). Detailed informa-
tion relating to SNPs in the human genome can be
found in several WWW-based resources (Table 1).
SNPs are widespread in cytokine
gene loci
Cytokine genes have been particularly well studied
by immunogeneticists for two reasons: rst, cytokine
genes play a very signicant role in orchestrating the
immune response and second, the rst cytokine gene
to be scrutinized in disease, TNFA, maps within the
MHC. This initial interest in TNFA led to investiga-
tions of other cytokine loci found outside the MHC,
for example IL-1. Bidwell and colleagues provide a
useful catalogue of cytokine gene polymorphism
and their relation to disease (13, 14, 78) that is also
available as a WWW-based resource (Table 1). The
polymorphisms listed therein include SNPs, micro-
satellites and microsatellites in the promoter regions,
introns, and 5
0
untranslated regions (5
0
UTR) as well
as SNPs in coding regions. Many of the SNPs listed
involve amino acid substitutions (nonsynonymous);
others inuence promoter and enhancer activity.
However, not all SNPs are functional. Indeed, we
have no knowledge of the functional correlates for
much of the diversity in the human genome.
The ever-growing list of cytokines provides ample
opportunity to relate genetic variation at individual
cytokine gene loci to modied function. This will be
assisted by an understanding of cytokine structure
and function using the tools of structural biology and
bioinformatics. For instance, although there are now
some 27 cytokines termed interleukins they seem to
fall within a limited number of structural families
(49). IL-1 cytokines, and IL-1b in particular, have
central roles in the initiation and progression of
periodontal disease. These cytokines are very well
characterized in terms of their molecular genetic
and immunologic properties. Furthermore, much
information exists relating to the association of IL-
1 genotypes with common complex diseases such as
periodontal disease. Therefore, IL-1 serves as a useful
paradigm for the relationship between cytokine gene
polymorphism and immunoregulation in periodon-
tal disease.
Table 1. Table of useful WWW sites for gene polymorphisms
WWW resource Description URL Comments
NCBI dbSNP database `One-stop shop' for
SNP resources
http://www.ncbi.nlm.nih.gov/
SNP/index.html
Comprehensive and detailed
information. Interpretation
requires some expertise.
Integrated with NCBI's
other genomic resources.
The SNP consortium A public/private
collaboration dedicated
to SNP discovery and
application
http://snp.cshl.org/ Similar level of information
to the NCBI site but dedicated
to SNPs. Both these sites are
likely to be more useful for
gene mapping studies.
Cytokine gene
polymorphism
data base
Descriptions of
polymorphisms,
phenotypic effects and
association study data
http://bris.ac.uk/pathandmicro/
services/GAI/cytokine4.htm
User-friendly format but
information last updated
March 2002. Most useful
for designing candidate
gene studies.
164
Taylor et al.
Numerous polymorphisms exist in the
IL-1 gene cluster
There are multiple polymorphic sites within the
human IL-1 gene cluster which include microsatel-
lites, VNTRs and numerous SNPs (Fig. 1). These are
conveniently catalogued in the Cytokine Gene Poly-
morphism in Human Disease database (13, 14, 78)
(Table 1). A detailed review of polymorphism in IL-1
gene cluster (and the TNF gene locus) has recently
been published (65). The linkage disequilibrium
across the IL-1 cluster is described as `moderate'
and there is a correlation between physical distance
and the degree of linkage disequilibrium which exists
(29). There is strong linkage disequilibrium within
the IL1A locus and between the 31 IL1A SNP and
the 86 bp VNTR polymorphism in intron 2 of that
gene (29, 51). Although linkage disequilibrium
between IL1B 31 and 3954 IL1B SNP has been
demonstrated, this was not consistent in different
populations (72, 51). No signicant linkage disequi-
librium between 3954 IL1B SNP and the IL1RN
intron 2 VNTR has been found (29, 51). Furthermore,
linkage disequilibrium between polymorphic sites
within the IL1B locus may be weak (29, 72).
Giventhe complex biologyof IL-1regulationandthe
extensive polymorphism in the IL-1 gene cluster, it is
likely that if IL-1 genes inuence disease, then combi-
nations of specic alleles will be important rather than
individual alleles. Therefore, it isconsideredthat know-
ledge of linkage disequilibriumand population haplo-
types in the IL-1 cluster will greatly aid rational design
of experiments, e.g. genetic association studies to test
the role of genetic polymorphismindisease pathogen-
esis(29). For example, populationstudieshaverevealed
the presence of at least one common haplotype com-
prisingalleles of eight polymorphicloci of theIL-1gene
cluster present at a frequency seven times greater than
expected (29). Nonetheless, association studies of IL-1
gene polymorphism and periodontal disease have
focused on individual SNPs or limited combinations
of SNPs rather than extended haplotypes.
Cytokine gene polymorphismand
periodontal disease
Cytokine gene polymorphisms may
encode inter-individual variation in
periodontal disease experience
There have been a considerable number of studies
demonstrating inter-subject variation in cytokine
production by peripheral blood mononuclear cells
(35, 53, 54, 94, 131). A number of parameters inu-
ence cytokine secretion levels, including cell type, in
vitro culture conditions, nature of the stimulus and
genetic background of the source cells (35, 54, 94).
These studies emphasize the multifactorial nature of
cytokine regulation. Furthermore, cells from indivi-
duals with immune-mediated diseases often exhib-
ited different cytokine secretion proles compared to
healthy controls and this might be explained by
genetic differences between affected and unaffected
individuals (84, 94, 124).
Hints that susceptibility to periodontal disease
might relate to individual differences in cytokine
secretions have come from data demonstrating that
peripheral blood mononuclear cells from periodon-
titis patients secrete increased levels of proinam-
matory cytokines in response to standard stimuli (63,
126, 162). Observations have been made supporting
the hypothesis that a hyper-inammatory phenotype
in certain individuals accounts for susceptibility to
chronic inammatory conditions such as periodon-
titis and possibly for shared susceptibility for certain
systemic conditions such as cardiovascular disease
and diabetes (137). Polymorphisms in the IL-1 clus-
ter have been the main focus of attention in recent
studies because of the fundamental role of IL-1b in
the pathogenesis of periodontal disease and the fact
that the genetic structures of the IL-1 gene cluster
and its associated polymorphisms are well estab-
lished.
When investigating the role of cytokine gene poly-
morphisms in the pathogenesis of periodontal dis-
eases, researchers have used two general approaches.
The majority of studies involving comparison of
allele and genotype frequencies between patients
with periodontal diseases and `healthy' controls have
been population-based studies of genetic association
(summarized in Tables 2 and 3). Other studies have
analyzed cytokine responses in immune cells iso-
lated from individuals of dened genotype and some
have sought correlation between cytokine genotype
and cytokine levels in various biological uids.
The role of cytokine genes in periodontal
disease has mainly been investigated in
genetic association studies of IL-1 SNPs
Interest in the role of cytokine gene polymorphisms
in the pathogenesis of periodontal disease expanded
signicantlyfollowing publicationof data by Kornman
et al. that suggested that non-smokers with period-
ontitis who were positive for what has become to be
165
Cytokine gene polymorphism and immunoregulation
Table 2. Summary of principal ndings of studies that investigated associations between the periodontitis associated genotype (PAG) and chronic periodontitis
(including implant studies)
Author, Year Genotype reported Subjects Study design Principal findings
Kornman et al. (108) PAG: Allele 2 of the
IL1A 889 SNP and Allele 2
of the IL1B 3953
SNP
49 patients with mild/no periodontitis,
42 with moderate periodontitis and 43
with severe periodontitis. All 35 years
Cross-sectional In non-smokers, a statistically
significant association between
severity of periodontitis and PAG
was identified. In smokers, severity
of disease was not correlated with
genotype.
Gore et al. (66) PAG: Allele 2 of the
IL1A 889 SNP and Allele 2
of the IL1B 3953
SNP
32 periodontitis patients and 32
periodontally healthy age-matched and
gender-matched controls
Cross-sectional No statistically significant association
between PAG and severity of periodontitis.
However, frequency of allele 2 of IL1B
3953 SNP alone was significantly
increased in severe periodontitis patients
compared to mild periodontitis patients,
but not compared to healthy patients.
Ehmke et al. (50) PAG: Allele 2 of the
IL1A 889 SNP and Allele 2
of the IL1B 3953
SNP
33 periodontal maintenance patients
monitored for 2 years
Longitudinal No differences in the survival rates of
sites or teeth not exhibiting attachment
loss 2 mm compared to baseline were
found between PAG-positive and
PAG-negative patients.
Galbraith et al. (62) IL-1b (3953)
20 patients with gingivitis and 20
patients with chronic periodontitis and
45 referent population subjects of
unknown periodontal status
Cross-sectional The frequency of allele 2 of the IL1B
3953 SNP was significantly increased in
patients with advanced periodontitis. There
was a significant correlation between IL1B
3953 genotype and IL-1b production by
oral and peripheral blood PMNs.
McGuire & Nunn (127) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3953
SNP
42 periodontal maintenance patients
monitored for 14 years
Longitudinal Both smoking and presence of PAG were
significantly associated with tooth loss. Both
smoking and PAG-positive status increased
the risk of tooth loss.
Wilson & Nunn (193) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3954 SNP
27 patients with 33 implants that had
been lost or had 50% bone loss
compared to 38 patients with no bone
or implant loss.
Cross-sectional There was no evidence to associate increased
risk of implant loss with PAG status. Smoking
increased the risk for implant failure 2.5 times,
however.
Armitage et al. (8) PAG: Allele 2 of the
IL1A 4845 SNP and Allele
2 of the IL1B 3953
SNP
Convenience sample of 300 Chinese
volunteers
Cross-sectional Only 2.3% of subjects were PAG-positive. Too
few of the subjects were PAG-positive to
establish any relationship with susceptibility
to chronic periodontitis.
1
6
6
T
a
y
l
o
r
e
t
a
l
.
Cutler et al. (33) PAG: Allele 2 of the
IL1A 4845 SNP and Allele
2 of the IL1B 3953
SNP
52 subjects with localised mild-moderate
chronic periodontitis
Cross-sectional No clinical differences were evident between
PAG-positive and PAG-negative patients.
De Sanctis &
Zucchelli (38)
PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3954 SNP
40 periodontitis patients undergoing
periodontal guided tissue regeneration
(GTR) surgery
Cross-sectional No statistically significant differences identified
between PAG-positive and PAG-negative patients
in baseline plaque or bleeding scores, probing
depth, attachment level or gingival recession.
Lang et al. (118) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3954 SNP
323 periodontal maintenance patients
monitored over 4 recall appointments
Longitudinal No effect of PAG on changes in bleeding on
probing (BOP) in the whole population because
of an overriding effect of smoking. PAG-positive
never-smokers (n 139) had a significantly
elevated chance of an increase in % BOP during
the recall period.
Mark et al. (121) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3953
SNP
10 PAG-positive and 10 PAG-negative
patients with mildmoderate chronic
periodontitis
Cross-sectional No significant differences in probing depths or
attachment levels between PAG-positive and
PAG-negative patients. Furthermore, there were
no significant differences in IL-1b production
by peripheral blood monocytes between
the two groups.
McDevitt et al. (125) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3954 SNP
46 controls (no disease or mild
periodontitis); 44 cases (moderate-severe
periodontitis). All 35 years
Cross-sectional Non-smokers or former light smokers
(<5 pack-years) who were PAG-positive were
more likely to have moderatesevere
periodontitis compared to PAG-negatives.
Cattabriga et al. (21) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3954 SNP
60 non-smoking periodontal maintenance
patients
Longitudinal PAG was not associated with increased tooth
loss after 10 years in 60 non-smoking, well
maintained, periodontitis patients.
Cullinan et al. (32) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3954 SNP
Convenience sample of 295 subjects
monitored for 5 years
Longitudinal A significant relationship between PAG and
increased mean probing depth in non-smokers
>50 years old was identified. PAG-positive
smokers, and PAG-positive patients with
P. gingivalis in their plaque had an increased
number of probing depths 3.5 mm.
Papapanou et al. (142) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3953
SNP
132 periodontitis patients and 73
periodontally healthy age- and gender-
matched controls
Cross-sectional PAG was positively correlated with severity of
attachment loss in periodontitis patients. PAG
was identified in 45.2% of cases and 41.7% of
controls (P > 0.05). There was no relationship
between genotype and subgingival microbial
profiles.
1
6
7
C
y
t
o
k
i
n
e
g
e
n
e
p
o
l
y
m
o
r
p
h
i
s
m
a
n
d
i
m
m
u
n
o
r
e
g
u
l
a
t
i
o
n
Table 2. continued
Author, Year Genotype reported Subjects Study design Principal findings
Laine et al. (114) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3954 SNP
53 non smoking and 52 smoking patients
with severe periodontitis
Cross-sectional No association between PAG and disease in
either smokers or non-smokers. PAG was
significantly associated with disease in
non-smokers without P. gingivalis or A.
actinomycetemcomitans
Thomson et al. (180) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3953
SNP
861 26-year-old subjects with periodontitis Cross-sectional After controlling for gender, smoking status
and plaque levels, PAG-positive subjects had
12 times the odds of having at least one tooth
with a 5 mm probing depth.
Caffesse et al. (16) PAG: Allele 2 of the
IL1A 4845 SNP and Allele 2
of the IL1B 3954 SNP
22 patients with previous gingival recession
treated by connective tissue grafts
Cross-sectional No association was identified between PAG and
response to mucogingival surgery. There were no
differences in mean gingival inflammation, probing
depth and attachment level scores between
PAG-positive and PAG-negative patients.
Meisel et al. (129) PAG: Allele 2 of the
IL1A 889 SNP and Allele 2
of the IL1B 3954 SNP
154 Caucasian chronic periodontitis patients Cross-sectional No significant differences in allele frequencies
were noted between subjects with mild/moderate
versus severe periodontitis. However, the extent
of attachment loss (defined as % of sites > 4 mm)
was significantly associated with PAG in smokers.
These authors concluded that PAG shows an
interaction with smoking, and non-smokers
are not at increased risk, even if they are
PAG-positive.
Rogers et al. (150) PAG: Allele 2 of the
IL1A 889 SNP and Allele 2
of the IL1B 3953
SNP
119 patients with a variety of diagnoses
including aggressive periodontitis, chronic
periodontitis, failed and successful implants,
and 60 periodontally healthy controls
Cross-sectional The composite genotype (i.e. PAG) showed no
association with the incidence of periodontitis
or the severity of disease. The IL-1b (3953)
SNP alone was associated with chronic
periodontitis. There was no association
between failure of implants and either PAG,
or IL1A or IL1B genotype individually.
Due to nomenclature change, the polymorphism at ILIB 3953 is now referred to as ILIB 3954 (69). At present, allele 2 of the ILIA 4845 SNP is assessed as opposed to the ILIA 889 SNP because they are concordant and it is
technically easier to analyze the ILIA 4845 SNP (107).
1
6
8
T
a
y
l
o
r
e
t
a
l
.
Table 3. Summary of principal ndings of studies that investigated associations between the periodontitis associated genotype (PAG) and aggressive periodontitis
Author, Year Genotype reported Subjects Study design Principal findings
Diehl et al. (42) IL1A 889 SNP,
IL1B 3953
SNP
141 aggressive periodontitis
patients and 144 controls
Cross-sectional Allele 1 (as opposed to allele 2) of the IL1B 3953 SNP
was associated with increased risk for aggressive
periodontitis. This study used the transmission disequilibrium
test (TDT), a statistically powerful method used in genetic
epidemiology that avoids problems of mismatching of cases
and controls, and that can be used to study populations
comprising different racial or ethnic groups.
Parkhill et al. (143) IL1B 3953
SNP 70 aggressive periodontitis
patients and 72 periodontally
healthy controls
Cross-sectional The frequency of allele 1 of the IL1B 3953
SNP was found
to be significantly increased in aggressive periodontitis
patients. Upon stratification for smoking status, a significant
difference was found in the IL-1b genotype distribution
between aggressive periodontitis smokers compared to control
smokers, but not between aggressive periodontitis
non-smokers and control non-smokers.
Walker et al. (188) IL1A 889 SNP and
IL1B 3953
SNP
37 African Americans with
localized aggressive periodontitis
and 104 periodontally healthy
controls
Cross-sectional IL1B 3953 SNP allele 1 was found in > 99% of the control
population, and in 100% of the aggressive periodontitis
population. Given the high prevalence of this genotype in
the control group, the authors concluded that studies of
this SNP would provide little diagnostic or predictive
information for localized aggressive periodontitis.
Hodge et al. (87) IL1A 889 SNP and
IL1B 3953
SNP
56 patients with generalized
aggressive periodontitis and 56
periodontally healthy controls
Cross-sectional There were no significant differences between patients and
controls for any of the genotype or allele frequencies
investigated. Smoking status, when included as a covariate,
did not influence the results.
Tai et al. (173) PAG: Allele 2 of the
IL1A 4845 SNP and
Allele 2 of the
IL1B 3954 SNP
47 patients with generalized
aggressive periodontitis and 97
periodontally healthy controls
Cross-sectional No significant differences in the frequencies of these alleles
between patients and controls in this Japanese cohort.
Due to nomenclature change, the polymorphism at IL1B 3953 is now referred to as IL1B 3954 (69). Presently, allele 2 of the IL1A 4845 SNP is assessed as opposed to the IL1A 889 SNP because they are concordant and it is
technically easier to analyse the IL1A 4845 SNP (107).
1
6
9
C
y
t
o
k
i
n
e
g
e
n
e
p
o
l
y
m
o
r
p
h
i
s
m
a
n
d
i
m
m
u
n
o
r
e
g
u
l
a
t
i
o
n
known as the periodontitis associated genotype (PAG)
had an approximately seven times greater chance of
having severe periodontitis than those who were
PAG-negative (108). PAG is a composite IL-1 geno-
type formed by the combination of two rare alleles at
separate SNPs in this cluster (55, 108). The rst of
these is at position 889 in the IL1A promoter, where
the least common allele (allele 2) results from a C to T
transition. The second is at position 3954 of the
IL1B gene, where the least common allele (allele 2)
also results from a C to T transition. The IL1B 3954
SNP was formerly referred to as 3953 but was chan-
ged after an alteration in numbering convention (69).
Analysis of the IL1A 889 SNP has been superseded
by analysis of the IL1A 4845 SNP (a G to T transi-
tion) which is technically more straightforward and,
as these two SNPs are in complete linkage disequili-
brium with one another, analysis of the IL1A 4845
SNP provides the same genetic information (107).
Signicantly, there is preliminary evidence from
population studies that a haplotype containing the
PAG (i.e. allele 2 of both these loci) may be part of a
common IL-1 haplotype (29, 110).
Most studies, like the original Kornman study, have
been cross-sectional studies of the PAG in patients
with what is now classied as chronic periodontitis
(7). Thus in two studies from the same research
group, PAG was correlated with severity of period-
ontitis in non-smokers with chronic periodontitis but
not in smokers or former smokers with chronic peri-
odontitis (108, 125). Smoking is a major risk factor for
periodontitis (101), and recent large-scale epide-
miologic studies have estimated that smoking may
be responsible for more than 50% of cases of period-
ontitis in Western populations (181). Smoking is
clearly, therefore, a factor that confounds risk assess-
ment in relation to genotyping of individuals in
cross-sectional studies, and must be accounted for
in study designs. The fact that the PAG was shown to
be a signicant risk factor only when smokers were
excluded underscores the importance of smoking as
a environmental risk factor for periodontitis (108,
125). However, Laine et al. (114) in reported that
PAG was not signicantly associated in either
smokers with severe chronic periodontitis (n 52)
or non-smokers with severe chronic periodontitis
(n 53).
Other studies have generated conicting results
regarding the importance of the PAG. It must be
stated, however, that most studies have suffered from
small study populations and cross-sectional designs
and, furthermore, have utilized varying criteria for
diagnosing the presence of periodontitis. Papapanou
et al. (142) conrmed that PAG correlates with sever-
ity of periodontitis (as measured by attachment loss)
in a study of 132 patients with chronic periodontitis.
However, three studies of smaller numbers of
patients (52, 30 and 32 respectively) did not nd
any evidence of association between PAG and sever-
ity of periodontitis (33, 38, 66). Although some stu-
dies distinguished between patients with smoking
experience and those without (108, 114, 125), other
investigations have not stratied their data with
respect to smoking (38, 66, 142). Meisel et al. (129)
in a cross-sectional study of 154 chronic periodonti-
tis patients determined that PAG was associated with
increased severity of disease only in smokers but not
in non-smokers, supporting the notion that there is
an interaction between these two risk factors.
Others have investigated possible associations of
PAG with various aspects of periodontal disease pro-
gression, relating PAG to changes in parameters of
periodontal disease in individual patients. The objec-
tive of periodontal therapy is, ultimately, to preserve
a functional, aesthetic, pain-free dentition. There-
fore, the most useful study of the impact of genotype
on periodontal status would be of longitudinal design
in which tooth loss is carefully monitored. McGuire
et al. (127) found that PAG was signicantly asso-
ciated with extent of tooth loss after 14 years in 42
patients with chronic periodontitis and had an addi-
tive effect with smoking. However, the data were not
clear with regard to how many teeth were lost per
patient, and how many teeth were lost in the smok-
ing and non-smoking groups. Twenty-six of the 42
patients in this study were PAG-negative even though
all had a clinical diagnosis of chronic periodontitis.
Furthermore, other studies have failed to identify
increased tooth loss in PAG-positive patients (21,
50), suggesting that PAG status is not a good predic-
tor of the likelihood of tooth loss in periodontitis
patients.
With regard to associations of PAG status and other
periodontal clinical parameters, Lang et al. found
that PAG was not associated with changes in bleed-
ing on probing in 323 chronic periodontitis patients,
including smokers (118). However, there was a sig-
nicant association in a subgroup of this cohort who
had never smoked, with more gingival bleeding in
those who were PAG-positive. Other studies have
failed to identify any correlation between genetic
status and bleeding on pressure (as reviewed by
Greenstein & Hart (69)). Bleeding on pressure is
known to be a very poor indicator of periodontal
disease activity (although absence of it is a highly
specic predictor of periodontal health, with a low
170
Taylor et al.
incidence of false positive results) (24) and is clearly
affected by factors other than a potential effect of
genotype, such as oral hygiene and compliance with
periodontal supportive therapy programs.
In the largest study of periodontal disease progres-
sion published to date, Cullinan et al. (32) studied
295 patients over a period of 5 years and revealed a
relationship between the PAG and increased period-
ontal probing depth in non-smokers older than 50
years of age. Furthermore, PAG-positive smokers and
PAG-positive patients with plaque containing Por-
phyromonas gingivalis also had increased pocket
depths (32). However, several other studies have
failed to provide any evidence for a contribution of
PAG to periodontal disease progression and/or
response to treatment. Cattabriga et al. (21) found
that PAG was not related to tooth loss after 10 years
in 60 non-smoking patients with chronic periodon-
titis. Ehmke et al. (50) found that parameters of peri-
odontal disease progression were independent of
PAG in 33 chronic periodontitis patients over 2 years,
although there was no stratication of the patients
with respect to smoking habit. DeSanctis et al. (38)
reported no relationship between PAG and response
to guided tissue regeneration therapy in 40 patients at
1 year post-treatment, but did identify more attach-
ment loss between 1 and 4 years post-treatment in
PAG-positive patients than in PAG-negative patients.
Periodontal disease parameters and response to
mucogingival surgery were not related to PAG in a
group of 22 patients (16).
Studies of the role of PAG in periodontal disease
have been extended to the investigation of the
levels and diversity of species of periodontal bacteria
in patients with different IL-1 genotypes. Thus
Socransky et al. (170) reported quantitative rather
than qualitative differences in the periodontal micro-
ora in patients with the PAG in a study of 108
chronic periodontitis patients. In particular, species
associated with measures of periodontal inamma-
tion were elevated in PAG-positive patients (170).
However, in a study of 132 periodontitis patients,
no correlation between possession of PAG and char-
acteristics of the subgingival microora was noted
(142).
Other workers have investigated the association of
other combinations of IL-1 genotypes with period-
ontal disease. Kornman et al. (108) did not nd any
signicant association between individual IL-1 gen-
otypes (IL1A 889, IL1A 511, IL1B 3954 SNPs and
IL1RN VNTR) and disease severity in 134 chronic
periodontitis patients. In contrast, three other stu-
dies have reported a signicant association between
allele 2 of the IL1B 3954 SNP and chronic period-
ontitis, albeit in much smaller cohorts of patients (62,
66, 150).
An important factor when considering the role of
the IL-1 genotype in periodontal pathogenesis is
whether or not PAG status impacts on clinical deci-
sion making or treatment protocols (69, 70). At the
present time, there is not enough evidence to suggest
that patients who are PAG-positive should be man-
aged differently from those who are PAG-negative.
There are certainly no longitudinal clinical studies
that have attempted to evaluate the therapeutic ben-
et of different periodontal treatment protocols that
have been employed depending on IL-1 genotype.
As noted earlier, a pathogenic microora is neces-
sary for initiation of periodontitis. It is quite concei-
vable, therefore, that the majority of PAG-positive
patients will not develop periodontitis if the bacterial
pathogens do not overwhelm the host response. One
potential benet of genotyping dental patients is that
it may allow dentists to identify those patients who
might be at increased risk for disease in the future,
and to suggest appropriate preventive strategies.
However, there is insufcient evidence that PAG-
positive patients are at greater risk for disease than
PAG-negative patients at the present time, and
implementation of aggressive maintenance strate-
gies could result in unnecessary treatment, with the
potential for iatrogenic periodontal breakdown
occurring, for example, as a result of excessive instru-
mentation of shallow pockets (120) or overzealous
toothbrushing by patients (153).
A reasonable conclusion might be that there are
genetic associations between polymorphisms in the
IL-1 cluster and periodontal disease but that unam-
biguous results are not yet apparent because of the
heterogeneity of the disease and/or the variable
design of the reported studies. Similarly, there have
been no consistent ndings with respect to the inter-
action of PAG and smoking in periodontal disease.
Furthermore, associations between particular genes
and periodontal disease have only been demon-
strated in certain populations (typically white Cau-
casians), and generally not in other racial or ethnic
groups (8, 42, 188). These ndings may reect differ-
ences in the prevalence of these genotypes in the
different racial groups. It is clear, therefore, that
genetic tests based upon these specic genes may
not apply to all patients (69). The utility of testing for
PAG on a population basis is likely to be governed by
the effectiveness of periodontal treatment, patient
compliance with maintenance care, the presence of
known risk factors (such as smoking) and the cost of
171
Cytokine gene polymorphism and immunoregulation
undertaking the test (83). The value of genetic testing
in identifying at risk patients and preventing severe
disease is reduced as compliance with maintenance
protocols increases. In a review of studies analyzing
PAG and periodontal disease, Greenstein and Hart
(69) concluded that `the ability of the genetic sus-
ceptibility test to forecast which patients will develop
increased bleeding on probing, periodontitis, or loss
of teeth or dental implants is ambiguous'. Further
prospective clinical trials were advocated and existing
data were not considered sufcient to alter patient
management practices at that time (69). Cullinan
et al. (32) conclude that in their patient population
`IL-1 genotype is a contributory but non-essential
risk factor for periodontal disease progression';
this is a reasonable conclusion of the state of our
knowledge at this time.
In contrast to genetic associations in chronic per-
iodontitis, studies of aggressive periodontitis indicate
that PAG is not associated with this disorder (42, 87).
Furthermore, there is evidence that allele 1 (rather
than allele 2) of the IL1B 3954 SNP is associated
with risk of aggressive periodontitis (42, 143). Similar
studies were attempted in aggressive periodontitis in
a wholly African American population but the authors
concluded that because of the high frequency of
allele 1 of the IL1B 3954, SNP studies of this poly-
morphism were not useful in this population (188).
Also, studies of aggressive periodontitis in a Japanese
population failed to nd any association between
aggressive periodontitis and genotype with respect
to the IL1B 3954, IL1B 511 or the IL1A 4853 SNPs
although there was a signicant association with
IL1RN intron 2 VNTR genotype (173). However, there
was no similar association with IL1RN intron 2 VNTR
genotype in studies of a UK population (143).
There is little evidence that cytokine
genes outside the IL-1 cluster are
associated with periodontal disease
To date there have only been a limited number of
studies of the association of polymorphisms in other
cytokine gene loci and periodontal disuse. The TNFA
308 SNP was not found to be associated with disease
severity in a study of 134 patients with chronic per-
iodontitis (108). Furthermore, Galbraith et al. (62)
studied 32 patients with chronic periodontitis but
found no signicant associations with three separate
SNPs (including the 308 SNP) in the promoter
region of the TNFA gene. No signicant disease asso-
ciations were found in a study of four TNFA promoter
SNPs (including two of the SNPs studied by Galbraith
et al.) in 90 chronic periodontitis patients (30). Simi-
larly, there was no association between alleles of a
TNFA microsatelllite polymorphism and aggressive
periodontitis in study of 91 patients (103). An investi-
gation of microsatellite repeat polymorphisms in the
promoter region of IL10 did not reveal any association
with aggressive periodontitis in two separate studies
(82, 103). There was nosignicant associationbetween
TNFA genotype or IL10 genotype and aggressive
periodontitis in a Japanese population (52, 196). There
is, however, some preliminary evidence that genotype
with respect to the IL2 330 SNP might be associated
with severity in aggressive periodontitis (155).
Study design is a critical factor in
genetic association studies
There are good arguments supporting the use of
case-controlled association studies in the investiga-
tion of the genetic basis for common complex dis-
eases such as periodontitis. Linkage analysis may be
less sensitive in detecting weak genetic effects and
requires consistent segregation across generations in
families, which is not always apparent (116, 148). In
addition, in linkage analysis, though there are several
members in each family, each family has only a sin-
gle index and therefore represents a single data point.
Power calculations reveal that linkage analysis
requires much larger sample numbers than associa-
tion studies (148). In contrast, association studies, if
large enough, can be powered to be sensitive enough
to detect genes with very modest effects and may be
a powerful adjunct to linkage studies, especially
when a region of the chromosome has been identi-
ed by linkage (17, 116).
However, studies of the PAG as a candidate geno-
type in periodontitis are just one example of genetic
association studies that are not consistently repro-
duced (191). Furthermore, the ndings of many asso-
ciation studies have not been supported by evidence
from linkage analysis and this has raised serious con-
cerns about the design of studies for complex dis-
eases (17, 191).
The weaknesses of case controlled studies are well-
documented. Sample selection and study design are
two of the most critical elements but sample size is
paramount and is the major reason for the lack of
reproducibility of case-control association studies
(17). There is a tendency to analyze and publish data
based on small patient groups; studies based on
small samples run an elevated risk of both false-posi-
tive associations (type 1 statistical errors) and of
172
Taylor et al.
false-negative associations (type 2 statistical errors).
The key to understanding the sample size require-
ments of a study lies with calculation of the statistical
power (149, 177). The sample size determines the
strength of the genetic association that can be con-
dently detected. Smaller samples are required to
detect associations with odds ratios of 4 or 5. Histori-
cally, we have considered an odds ratio of greater than
3 to be signicant but current evidence from com-
plex diseases (with large heritable components) indi-
cates that the predicted odds ratios for many genes
may be 1.5 or less (17). To identify associations with
such small effects condently, very large numbers of
patients will need to be studied. Such numbers may
only be available through multicenter collaboration
or use of prospectively collected cohorts such as the
Biobank UK initiative (194). It is likely, therefore that
many of the published studies of genetic associations
and periodontal disease have been underpowered.
Meta analysis of genetic association studies compar-
ing smaller studies with larger-scale well-controlled
designs have further underlined the importance of
sample size (5, 99).
Stratication within populations can lead to spuri-
ous disease associations in case-control studies (17,
116). To avoid this problem, controls need to be
closely matched with the disease population. This is
difcult in many diseases, including chronic period-
ontitis, where the age of disease onset varies. Chronic
periodontitis is a disease that exhibits continuous
variability and therefore association studies have
compared genotype with severity within patient
populations rather than use the traditional case-
control model. However, most genetic association
studies of chronic periodontitis have been cross-
sectional studies and have not allowed for the long-
itudinal uctuation of disease severity which often
occurs in individual patients. Furthermore, it is
extremely difcult to design longitudinal periodontal
studies that adequately allow for known systemic risk
factors for periodontal disease, such as smoking and
stress (152) or, indeed, local risk factors. Coupled
with this is the problem, in longitudinal studies, of
accurately identifying over time whether disease
progression is occurring. The rate of progression
of chronic periodontitis is typically slow, with the
majority of periodontal sites remaining stable for
prolonged periods of time (168). A statistical model
which considers disease progression parameters in
the context of multiple risk factors has been devel-
oped and applied to studies of PAG and periodontal
disease (32, 57). These type of models need to be
elaborated and applied more widely.
Problems of sample selection could be overcome
by redesigning association studies and moving away
from the case-control model. Prospective cohort
studies (e.g. Biobank UK) or alternative types of asso-
ciation studies based upon the transmission disequi-
librium test (TDT) may overcome some of the above
problems (17). A detailed discussion of alternative
models for studies of IL-1 polymorphism and human
disease has been presented elsewhere (65).
In conclusion, studies reported to date have suf-
fered from a variety of problems including lack of
statistical power and small sample populations, vari-
able criteria used to diagnose periodontitis, cross-
sectional designs, and difculties in identifying a
control group due to the continuous variability of
chronic periodontitis and the different age of onset
of disease between individuals. By contrast, aggres-
sive periodontitis may offer some advantages for
study since there are fewer problems with diagnosis,
variable phenotype and age of onset. Furthermore,
there is a more clearly dened genetic element to this
disease (75, 86). However, aggressive periodontitis is
much less prevalent than chronic periodontitis. To
generate sufciently large study populations, colla-
borations between centers are essential in order to
undertake sufciently powered studies. Notwith-
standing this requirement, genetic associations
dened in studies of aggressive periodontitis would
be valuable in that they would inform studies of the
more common but variable chronic periodontitis.
Studies of the effect of genetic
polymorphism on cytokine expression
in vitro and in vivo have not yielded
consistent results
The suggestion that cytokine gene polymorphisms
inuence periodontal disease pathogenesis would
be strengthened by reproducible evidence from
experimental systems at the molecular and cellular
level. Disappointingly, few studies have reported
experiments directly analyzing the relationship
between ILI genotypes which constitute PAG and
cytokine expression. Studies of samples from 33
healthy donors showed that monocyte IL-1b produc-
tion after lipopolysaccharide/phytohemagglutinin
stimulation is related to the IL1B 3954 SNP (144).
This report is often quoted in support of a biological
effect for the IL1B 3954 SNP and the PAG. More
recent studies, however, have not directly repro-
duced these ndings. For example, Santtila et al.
(154) found that the IL1B 3954 and ILB 511 SNPs
have no inuence on mononuclear cell IL-1b
173
Cytokine gene polymorphism and immunoregulation
production in samples from 50 healthy donors. In a
study of 30 healthy individuals representing 10 sam-
ples with each genotype, Dominici et al. (47)
reported that the IL1B 3954 SNP had no effect on
lipopolysaccharide-induced IL-1b secretion. Simi-
larly, the IL1B 3954 SNP did not inuence consti-
tutive or induced IL-1b secretion in peripheral blood
mononuclear cells in vitro or plasma levels in vivo
in a study of 55 healthy volunteers (187). Data from
two similar studies indicated that there was no sta-
tistically signicant increase in IL-1b production by
peripheral blood and oral polymorphonuclear cells
from chronic periodontitis patients and healthy con-
trols, and IL-1b production was not related to IL1B
3954 genotype (62, 66).
There is evidence that the TT genotype (i.e. two
copies of allele 2) of the SNP at position 889 of IL1A
inuences IL-1b levels in whole blood (90). Dominici
et al. employed transient transfection assays using
reporter gene constructs containing allele-specic
sequences and reported that the same TT genotype
of the IL1A 889 SNP signicantly increased the tran-
scriptional activity of IL1A over the AA genotype (46).
However, the effect on IL-1a mRNA levels and
plasma IL-1a was small and inconsistent over time.
Interestingly, the presence of the T allele at position
889 of IL1A creates a consensus site for the transcrip-
tion factor Skn1 (46). There is a paucity of studies
that have addressed the issue of the inuence of PAG
on IL-1 production in vitro. In a systematic study of
monocyte responses to a panel of relevant stimula-
tors, no relationship between PAG and IL-1b produc-
tion was found (121). Also, there are few studies of
cytokine gene polymorphism and in vivo IL-1 levels
in periodontal disease. The relationship between
specic IL-1 genotypes and the level of IL-1b in the
gingival crevicular uid and periodontal tissues in 22
patients has been studied (55). IL-1b levels in shallow
periodontal pockets were higher in patients with the
PAG compared to patients without PAG (both before
and after treatment), indicating that there may be
some local phenotypic differences in chronic period-
ontitis associated with IL-1 genotype (55). Indeed,
this assumption forms the basis for clinical studies
in which associations between PAG and periodontal
status have been identied. Carriage of allele 2 of the
IL1A889 SNP (part of the PAG) was associated with
signicantly increased levels of GCF IL-1a in 46
patients with chronic periodontitis (165). Interest-
ingly, differences in IL-1a in patients stratied
according to IL1A genotype were higher in non-smo-
kers than in `heavy' smokers, emphasizing the pos-
sible role of exogenous factors in cytokine gene
production (165). In summary, the evidence for a
direct biological effect of the IL-1 SNPs that form
the PAG remains variable and incomplete. It is pos-
sible that observed genetic associations are the result
of linkage disequilibrium with functional poly-
morphisms elsewhere on chromosome 2. In this
regard there is evidence that other SNPs in the
IL1A locus inuence IL-1 regulation. For example,
the ILIB 31 SNP forms part of a TATA box sequence
and electrophoretic mobility shift assays have
demonstrated that the T allele of this polymorphism
increases DNAprotein interactions at this site in
vitro (51). Also, the IL1B 31 SNP is located close to
the site of binding of two protein factors important in
regulation of IL1B transcription (106, 199). There was
almost complete linkage disequilibrium between the
IL1B 31 SNP and the IL1RN intron 2 VNTR and it
was suggested IL1B31T/IL1RN
2 may constitute a
proinammatory haplotype (51). However, the IL1A
31 SNP does not inuence IL-1b production in vi-
tro or in vivo (187). There is some evidence that the
VNTR polymorphism in intron 2 of IL1RN has an
effect on IL-1 production. Danis et al. (35) reported
that the IL1RN
2 allele was associated with high pro-
duction of IL-1Ra and low IL-1a in granulocyte
macrophage colony-stimulating factor stimulated
monocytes. However, in the same study no genetic
inuences on IL-1b production were demonstrated.
This is in contrast to a study of peripheral blood
mononuclear cells stimulated with phorbol ester
and the calcium ionophore A23187 that demon-
strated that the IL1RN
2 allele was associated with
high production of IL-1b (154). Recently, a very care-
ful study by Vamvakopoulos et al. (187) has provided
evidence that the genotype with respect to the VNTR
polymorphism in intron 2 of the IL1RN has a direct
effect on both IL-1Ra and IL-1b secretion. The levels
of plasma IL-1Ra and IL-1b correlated, suggesting
coordinate regulation of these cytokines. Further-
more, in vitro and in vivo analyses indicated that
the IL1RN
1 allele was associated with high IL-1b
and low IL-1Ra levels. Conversely, the IL1RN
2 allele
was associated with low IL-1b and high IL-1Ra levels
(187). Hurme et al. (91) also found that the IL1RN
2
allele was associated with high IL-1Ra levels. Signi-
cantly, the inuence of IL1RN genotype was inde-
pendent of other IL-1 gene polymorphisms and was
not inuenced by exogenous modiers of IL-1b
such as dexamethasone (187). Furthermore, there
are three sequences in the repeat region of the IL1RN
intron 2 VNTR which potentially correspond to bind-
ing sites for known regulatory proteins and therefore
variable number of repeats might have functional
174
Taylor et al.
signicance (174). However, Clay et al. (27) demon-
strated that the IL1RN
2 allele did not inuence spe-
cic mRNA production in keratinocyte cell lines.
Taken together, the data suggest the IL1RN intron 2
VNTR may have a role in the regulation of the bio-
logical activity of IL-1b, although the results from the
limited number of studies performed have not been
consistent. It has been suggested that, since different
cell stimuli were employed in these studies, the data
may reect differential genetic regulation of the
various intracellular signaling pathways leading to
cytokine gene regulation and protein synthesis (187).
The number of genes in the IL-1 cluster, the exten-
sive polymorphism and the high degree of linkage
disequilibrium across this region complicates the
analysis and interpretation of functional studies of
genetic polymorphism.
In contrast to genes in the IL-1 cluster, the effect of
polymorphisin in the TNFA locus on TNF-a produc-
tion has been studied in far greater detail and serves
as a paradigm for studies of the biological inuence
of other cytokine gene polymorphisms. Both micro-
satellite polymorphisms and SNPs in the TNFA locus
seem to inuence TNF-a production but distinguish-
ing direct effects is complicated by signicant linkage
disequilibrium both within the TNFA locus and with
nearby HLA class I and II alleles (74, 192). Signi-
cantly, there are at least 10 SNPs in the putative
promoter region of the TNFA gene, although some
of the allelic variants are rare (74). The majority of
in vitro studies using reporter gene constructs and
experiments measuring cytokine secretion by cul-
tured cells indicate that the TNFA 308A allele may
increase TNFA transcription and TNF-a production,
although not all studies have conrmed these nd-
ings (74, 98, 104, 112). Neither the TNFA 238 or
TNFA 308 SNPs seem to inuence circulating levels
of TNF-a, perhaps reecting differences between
local and systemic regulation of cytokines (89, 113).
Knight et al. provided direct evidence for differences
in the interaction of the transcription factor OCT-1
between different allelic variants of the TNFA 376
SNP (105). Signicantly, no protein binding at the
TNFA 238 or TNFA 308 SNPs was found and these
polymorphisms may therefore inuence TNF-a pro-
duction by linkage disequilibrium with the functional
TNFA 376 SNP (105). Also, NF-kB binds to the site
of the TNFA 863 SNP when the C allele is present
but is inhibited in the presence of the A allele (185).
There is evidence that microsatellite repeat poly-
morphisms in the IL10 promoter inuence IL-10 pro-
duction, although the data with respect to SNPs in
the same locus are conicting (31, 56, 123, 184).
Similar inconsistencies have been reported for the
inuence of polymorphisms in other cytokine genes,
e.g. the IFNG gene (19, 145) and the IL6 gene (59, 80,
81).
Evidence for a direct relationship of cytokine gene
polymorphism, regulation of cytokine expression
and subsequent effects on immunoregulation and
disease therefore remains inconsistent and incom-
plete. Gene transcription, and the inuence of struc-
tural variants on this process, is likely to be context
dependent; thus the inuence of genetic polymorph-
ism will be different in diverse cell types at different
developmental stages and in different environments.
For example, detailed investigations using transient
transfection assays have revealed that the inuence
of the TNFA 308A allele varies between stimulus
delivered and cell type studied (112). In vitro studies
of IL-6 expression reveal complex interactions
between individual SNPs comprising common hap-
ltoypes (178). Also, IL-6 production by naive neonatal
cells was inuenced by IL6 genotype but IL-6 produc-
tion was independent of genotype in healthy adults,
indicating that IL-6 was under different immunore-
gulatory inuences in cells with previous contact
with exogenous antigens (100). These phenomena
might also explain the different conclusions derived
from studies of different individual experimental sys-
tems. Clearly, more detailed studies involving analy-
sis of the interaction of multiple polymorphic sites
and detailed scrutiny of molecular regulators of gene
transcription using more sophisticated techniques
are required (105, 186).
Summary and future prospects
The genetic element for periodontal disease, a cen-
tral pathogenic role for cytokines, as well as the prin-
ciple of individual variation in disease experience are
tenets of periodontal research. However, a role for
cytokine gene polymorphism in immunoregulation
in periodontal disease remains suggestive rather than
being rmly established. The problems (and some
potential solutions) relating to association analyses
and experimental studies of cytokine gene poly-
morphisms at the molecular genetic level are out-
lined in the preceding sections. Our response to
these challenges will be aided by the recent and
rapidly developing elds of genomics, proteomics
and bioinformatics.
Developments in genomics are providing funda-
mental structural information about the human
genome and genomic variation, e.g. dbSNP
175
Cytokine gene polymorphism and immunoregulation
(Table 1)(155, 163). Analysis of the entire genomic
complement of individual human SNPs in popula-
tion studies of genetic association remains beyond
our technical and economic resources. However, the
increasing availability of high throughput techno-
logies should make analysis of SNPs across multiple
gene loci a fairly routine matter and association
studies incorporating the analysis of several thousand
gene polymorphisms are beginning to be done
(18). Characterization of the physical relationship
between individual SNPs in the genome and devel-
opment of a genome-wide haplotype map will facil-
itate more detailed studies of genetic basis for
human disease (61). For example, genotyping studies
within individual loci have revealed that haplotypes
within particular genetic regions contain informative
SNPs and redundant SNPs; determination of the gen-
otype of informative SNPs identies the haplotype in
that gene or region of the genome and these have
been termed `haplotype tag SNPs' (htSNPs) (97).
Genotyping htSNPs promises to reduce the genotyp-
ing effort required and to aid investigations of the
role of polymorphism and linkage disequilibrium
across wide regions of the genome.
Developments in technologies able to provide
mRNA proles (transcriptomics) and protein proles
(proteomics) at the cellular level are providing
comprehensive phenotypic information with a wide
range of applications in immunologic and patho-
logic studies of human disease. Cellular immune
responses can now be mapped to changes in regu-
latory networks, rather than individual mediators, in
response to dened stimuli (161). These technologies
promise to facilitate comprehensive studies of geno-
type/phenotype relationships and will provide more
sophisticated models for analyzing complex ele-
ments of human diseases (25). There is an increasing
appreciationthat biological research relies onefcient
and imaginative information processing, especially
in the post-genomic era. Bioinformatic approaches
have evolved from demands of handling nucleic acid
and protein sequences in molecular biological
research and have now expanded to other areas such
as immunologic research, where analysis of complex
regulatory networks is critical to understanding
immune responses in health and disease (2).
There is no doubt that we now have the technolo-
gic basis to generate and analyze large volumes of
information in the pursuit of understanding complex
diseases such as periodontal disease at the molecular
genetic level. However, in order to successfully
exploit these developments there needs to be a move
away from the reductionist view, which supports a
central role for individual gene variants and loci in
genetic susceptibility to complex diseases. Periodon-
tal disease should be viewed as a polygenic disease in
which many interacting gene variants contribute to
disease susceptibility. Also, sophisticated models
need to be developed which integrate modern per-
spectives on genetic variation at the genomic level,
the dynamic nature of host immune responses and
the relationship between immune parameters and
disease activity (25, 147). These models must also
consider the multifactorial nature of periodontal dis-
ease and in particular the contribution of environ-
mental factors such as smoking. However, given the
critical role of cytokines in immune responses, the
limited information concerning the role of cytokine
polymorphisms outside the IL-1 cluster, and our
restricted understanding of cytokine regulation,
cytokine genes and immune regulation are likely to
remain an important eld of investigation in period-
ontal research.
Note
The Ensembl Human Genome Browser (http://
www.ensembl.org/Homo_sapiens/) now has a user-
friendly interface for viewing detailed and contem-
porary information concerning SNPs and other
genetic variants in the human genome, including
those in the cytokine gene loci.
References
1. Anonymous. Position paper: epidemiology of periodontal
diseases. American Academy of Periodontology. J Period-
ontol 1996: 67: 935945.
2. Aderem A, Hood L. Immunology in the post-genomic era.
Nat Immunol 2001: 2: 373375.
3. Alexander MB, Damoulis PD. The role of cytokines in the
pathogenesis of periodontal disease. Curr Opin Periodon-
tol 1994: 3953.
4. Alheim K, McDowell TL, Symons JA, Duff GW, Bartfai T. An
AP-1 site is involved in the NGF induction of IL-1a in PC12
cells. Neurochem Int 1996: 29: 487496.
5. Altshuler D, Hirschhorn JN, Klannemark M, Lindgren CM,
Vohl MC, Nemesh J, Lane CR, Schaffner SF, Bolk S, Brewer
C, Tuomi T, Gaudet D, Hudson TJ, Daly M, Groop L, Land-
er ES. The common PPARg Pro12Ala polymorphism is
associated with decreased risk of type 2 diabetes. Nat Genet
2000: 26: 7680.
6. Arend WP, Malyak M, Smith MF, Jr, Whisenand TD, Slack
JL, Sims JE, Giri JG, Dower SK. Binding of IL-1a, IL-1b, and
IL-1 receptor antagonist by soluble IL-1 receptors and
levels of soluble IL-1 receptors in synovial fluids. J Immu-
nol 1994: 153: 47664774.
176
Taylor et al.
7. Armitage GC. Development of a classification system for
periodontal diseases and conditions. Ann Periodontol
1999: 4: 16.
8. Armitage GC, Wu Y, Wang HY, Sorrell J, di Giovine FS, Duff
GW. Low prevalence of a periodontitis-associated interleu-
kin-1 composite genotype in individuals of Chinese heri-
tage. J Periodontol 2000: 71: 164171.
9. Bailly S, Fay M, Israel N, Gougerot-Pocidalo MA. The tran-
scription factor AP-1 binds to the human interleukin 1a
promoter. Eur Cytokine Netw 1996: 7: 125128.
10. Baker PJ, Roopenian DC. Genetic susceptibility to chronic
periodontal disease. Microbes Infect 2002: 4: 11571167.
11. Banchereau J, Steinman RM. Dendritic cells and the con-
trol of immunity. Nature 1998: 392: 245252.
12. Banyer JL, Hamilton NH, Ramshaw IA, Ramsay AJ. Cyto-
kines in innate and adaptive immunity. Rev Immunogenet
2000: 2: 359373.
13. Bidwell J, Keen L, Gallagher G, Kimberly R, Huizinga T,
McDermott M, Oksenberg J, McNicholl J, Pociot F, Hardt
C, D'Alfonso S. Cytokine gene polymorphism in human
disease: on-line data bases. Genes Immun 1999: 1: 319.
14. Bidwell J, Keen L, Gallagher G, Kimberly R, Huizinga T,
McDermott MF, Oksenberg J, McNicholl J, Pociot F, Hardt
C, D'Alfonso S. Cytokine gene polymorphism in human
disease: on-line databases, supplement 1. Genes Immun
2001: 2: 6170.
15. Birkedal-Hansen H. Role of cytokines and inflammatory
mediators in tissue destruction. J Periodontal Res 1993: 28:
500510.
16. Caffesse RG, De La Rosa RM, De La Rosa GM, Weltman R.
Effect of interleukin-1 gene polymorphism in a periodon-
tally healthy Hispanic population treated with mucogingi-
val surgery. J Clin Periodontol 2002: 29: 177181.
17. Cardon LR, Bell JI. Association study designs for complex
diseases. Nat Rev Genet 2001: 2: 9199.
18. Carrasquillo MM, McCallion AS, Puffenberger EG, Kashuk
CS, Nouri N, Chakravarti A. Genome-wide association
study and mouse model identify interaction between
RET and EDNRB pathways in Hirschsprung disease. Nat
Genet 2002: 32: 237244.
19. Cartwright N, Demaine A, Jahromi M, Sanders H, Kaminski
ER. A study of cytokine protein secretion, frequencies of
cytokine expressing cells and IFN-G gene polymorphisms
in normal individuals. Transplantation 1999: 68: 1546
1552.
20. Casey LC, Balk RA, Bone RC. Plasma cytokine and endo-
toxin levels correlate with survival in patients with the
sepsis syndrome. Ann Intern Med 1993: 119: 771778.
21. Cattabriga M, Rotundo R, Muzzi L, Nieri M, Verrocchi G,
Cairo F, Pini PG. Retrospective evaluation of the influence
of the interleukin-1 genotype on radiographic bone levels
in treated periodontal patients over 10 years. J Periodontol
2001: 72: 767773.
22. Chakravarti A. Population genetics making sense out of
sequence. Nat Genet 1999: 21: 5660.
23. Chakravarti A. To a future of genetic medicine. Nature
2001: 409: 822823.
24. Chapple IL. Periodontal disease diagnosis: current status
and future developments. J Dent 1997: 25: 315.
25. Cheung VG, Spielman RS. The genetics of variation in gene
expression. Nat Genet 2002: 32: 522525.
26. Choi JI, Borrello MA, Smith ES, Zauderer M. Polarization of
Porphyromonas gingivalis-specific helper T-cell subsets by
prior immunization with Fusobacterium nucleatum. Oral
Microbiol Immunol 2000: 15: 181187.
27. Clay FE, Tarlow JK, Cork MJ, Cox A, Nicklin MJ, Duff GW.
Novel interleukin-1 receptor antagonist exon polymorph-
isms and their use in allele-specific mRNA assessment.
Hum Genet 1996: 97: 7236.
28. Colotta F, Re F, Muzio M, Bertini R, Polentarutti N, Sironi
M, Giri JG, Dower SK, Sims JE, Mantovani A. Interleukin-1
type II receptor: a decoy target for IL-1 that is regulated by
IL-4. Science 1993: 261: 472475.
29. Cox A, Camp NJ, Nicklin MJ, di Giovine FS, Duff GW. An
analysis of linkage disequilibrium in the interleukin-1 gene
cluster, using a novel grouping method for multiallelic
markers. Am J Hum Genet 1998: 62: 11801188.
30. Craandijk J, van Krugten MV, Verweij CL van d V, Loos BG.
Tumor necrosis factor-a gene polymorphisms in relation
to periodontitis. J Clin Periodontol 2002: 29: 2834.
31. Crawley E, Kay R, Sillibourne J, Patel P, Hutchinson I, Woo
P. Polymorphic haplotypes of the interleukin-10 5' flanking
region determine variable interleukin-10 transcription and
are associated with particular phenotypes of juvenile rheu-
matoid arthritis. Arthritis Rheum 1999: 42: 11011108.
32. CullinanMP, WestermanB, Hamlet SM, Palmer JE, FaddyMJ,
Lang NP, Seymour GJ. A longitudinal study of interleukin-1
gene polymorphisms and periodontal disease in a general
adult population. J Clin Periodontol 2001: 28: 11371144.
33. Cutler CW, Stanford TW, Abraham C, Cederberg RA,
Boardman TJ, Ross C. Clinical benefits of oral irrigation
for periodontitis are related to reduction of pro-inflamma-
tory cytokine levels and plaque. J Clin Periodontol 2000: 27:
134143.
34. Daly AK, Day CP, Donaldson PT. Polymorphisms in im-
munoregulatory genes: towards individualized immuno-
suppressive therapy? Am J Pharmacogenomics 2002: 2:
1323.
35. Danis VA, Millington M, Hyland VJ, Grennan D. Cytokine
production by normal human monocytes: inter-subject
variation and relationship to an IL-1 receptor antagonist
(IL-1Ra) gene polymorphism. Clin Exp Immunol 1995: 99:
303310.
36. Darveau RP. Oral innate host defense responses: interac-
tions with microbial communities and their role in the
development of disease. In: Oral Bacterial Ecology: The
Molecular Basis. Wymondham, UK: Horizon Scientific
Press, 2000: 169218.
37. Darveau RP, Tanner A, Page RC. The microbial challenge in
periodontitis. Periodontol 2000 1997: 14: 1232.
38. De Sanctis M, Zucchelli G. Interleukin-1 gene polymorph-
isms and long-term stability following guided tissue regen-
eration therapy. J Periodontol 2000: 71: 606613.
39. Del Prete GF, De Carli M, Mastromauro C, Biagiotti R,
Macchia D, Falagiani P, Ricci M, Romagnani S. Purified
protein derivative of Mycobacterium tuberculosis and ex-
cretory-secretory antigen(s) of Toxocara canis expand in
vitro human T cells with stable and opposite (type 1 T
helper or type 2 T helper) profile of cytokine production.
J Clin Invest 1991: 88: 346350.
40. Delima AJ, Karatzas S, Amar S, Graves DT. Inflammation
andtissuelosscausedbyperiodontal pathogensisreducedby
interleukin-1 antagonists. J Infect Dis 2002: 186: 511516.
41. Dennison DK, Van Dyke TE. The acute inflammatory res-
ponse and the role of phagocytic cells in periodontal health
and disease. Periodontol 2000 1997: 14: 5478.
177
Cytokine gene polymorphism and immunoregulation
42. Diehl SR, Wang Y, Brooks CN, Burmeister JA, Califano JV,
Wang S, Schenkein HA. Linkage disequilibrium of inter-
leukin-1 genetic polymorphisms with early-onset period-
ontitis. J Periodontol 1999: 70: 418430.
43. Dinarello CA. The interleukin-1 family: 10 years of discov-
ery. FASEB J 1994: 8: 13141325.
44. Dinarello CA. Interleukin-1. Cytokine Growth Factor Rev
1997: 8: 253265.
45. Dinarello CA, Ikejima T, Warner SJ, Orencole SF, Lonne-
mann G, Cannon JG, Libby P. Interleukin 1 induces inter-
leukin 1. I. Induction of circulating interleukin 1 in rabbits
in vivo and in human mononuclear cells in vitro. J Immu-
nol 1987: 139: 19021910.
46. Dominici R, Cattaneo M, Malferrari G, Archi D, Mariani C,
Grimaldi LM, Biunno I. Cloning and functional analysis of
the allelic polymorphism in the transcription regulatory
region of interleukin-1a. Immunogenetics 2002: 54: 8286.
47. Dominici R, Malferrari G, Mariani C, Grimaldi L, Biunno I.
The interleukin 1b exonic (3953) polymorphism does not
alter in vitro protein secretion. Exp Mol Pathol 2002: 73:
139141.
48. Dunn E, Sims JE, Nicklin MJ, O'Neill LA. Annotating
genes with potential roles in the immune system: six
new members of the IL-1 family. Trends Immunol 2001:
22: 533536.
49. Eberl M. Don't count your interleukins before they've
hatched. Trends Immunol 2002: 23: 341342.
50. Ehmke B, Kress W, Karch H, Grimm T, Klaiber B, Flemmig
TF. Interleukin-1 haplotype and periodontal disease pro-
gression following therapy. J Clin Periodontol 1999: 26:
810813.
51. El Omar EM, Carrington M, Chow WH, McColl KE, Bream
JH, Young HA, Herrera J, Lissowska J, Yuan CC, Rothman
N, Lanyon G, Martin M, Fraumeni JF, Jr, Rabkin CS. Inter-
leukin-1 polymorphisms associated with increased risk of
gastric cancer. Nature 2000: 404: 398402.
52. Endo M, Tai H, Tab K, Kobayashi T, Yamazaki K, Yoshie H.
Analysis of single nucleotide polymorphisms in the 5
0
-
flanking region of tumor necrosis factor-a gene in Japanese
patients with early-onset periodontitis. J Periodontol 2001:
72: 15541559.
53. Endres S, Ghorbani R, Lonnemann G, van der Meer JW,
Dinarello CA. Measurement of immunoreactive interleu-
kin-1b from human mononuclear cells: optimization of
recovery, intrasubject consistency, and comparison with
interleukin-1a and tumor necrosis factor. Clin Immunol
Immunopathol 1988: 49: 424438.
54. Endres S, Cannon JG, Ghorbani R, Dempsey RA, Sisson SD,
Lonnemann G, van der Meer JW, Wolff SM, Dinarello CA.
In vitro production of IL 1b, IL 1a, TNF and IL2 in healthy
subjects: distribution, effect of cyclooxygenase inhibition
and evidence of independent gene regulation. Eur J Im-
munol 1989: 19: 23272333.
55. Engebretson SP, Lamster IB, Herrera-Abreu M, Celenti RS,
Timms JM, Chaudhary AG, di Giovine FS, Kornman KS.
The influence of interleukin gene polymorphism on ex-
pression of interleukin-1b and tumor necrosis factor-a in
periodontal tissue and gingival crevicular fluid. J Period-
ontol 1999: 70: 567573.
56. Eskdale J, Gallagher G, Verweij CL, Keijsers V, Westendorp
RG, Huizinga TW. Interleukin 10 secretion in relation to
human IL-10 locus haplotypes. Proc Natl Acad Sci USA
1998: 95: 94659470.
57. Faddy MJ, Cullinan MP, Palmer JE, Westerman B, Seymour
GJ. Antedependence modeling in a longitudinal study of
periodontal disease: the effect of age, gender, and smoking
status. J Periodontol 2000: 71: 454459.
58. Fenton MJ, Vermeulen MW, Clark BD, Webb AC, Auron PE.
Human pro-IL-1 b gene expression in monocytic cells is
regulated by two distinct pathways. J Immunol 1988: 140:
22672273.
59. Fishman D, Faulds G, Jeffery R, Mohamed-Ali V, Yudkin
JS, Humphries S, Woo P. The effect of novel poly-
morphisms in the interleukin-6 (IL-6) gene on IL-6 tran-
scription and plasma IL-6 levels, and an association with
systemic-onset juvenile chronic arthritis. J Clin Invest 1998:
102: 13691376.
60. Furutani Y. Molecular studies on interleukin-1a. Eur Cyto-
kine Netw 1994: 5: 533538.
61. Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J,
Blumenstiel B, Higgins J, DeFelice M, Lochner A, Faggart
M, Liu-Cordero SN, Rotimi C, Adeyemo A, Cooper R, Ward
R, Lander ES, Daly MJ, Altshuler D. The structure of hap-
lotype blocks in the human genome. Science 2002: 296:
22252229.
62. Galbraith GM, Hendley TM, Sanders JJ, Palesch Y, Pandey
JP. Polymorphic cytokine genotypes as markers of disease
severity in adult periodontitis. J Clin Periodontol 1999: 26:
705709.
63. Garrison SW, Nichols FC. LPS-elicited secretory responses
in monocytes: altered release of PGE2 but not IL-1b in
patients with adult periodontitis. J Periodontal Res 1989:
24: 8895.
64. Gemmell E, Marshall RI, Seymour GJ. Cytokines and
prostaglandins in immune homeostasis and tissue des-
truction in periodontal disease. Periodontol 2000 1997:
14: 112143.
65. di Giovine F, Camp NJ, Cox A, Chaudhary AG, Sorrell J,
Crane A, Duff GW. Detection and population analysis of IL-
1 and TNF gene polymorphisms. In: Balkwill F, ed. Cyto-
kine Molecular Biology. Oxford: Oxford University Press,
2000: 2146.
66. Gore EA, Sanders JJ, Pandey JP, Palesch Y, Galbraith GM.
Interleukin 1b 3953 allele 2: association with disease
status in adult periodontitis. J Clin Periodontol 1998: 25:
781785.
67. Granowitz EV, Porat R, Mier JW, Pribble JP, Stiles DM,
Bloedow DC, Catalano MA, Wolff SM, Dinarello CA.
Pharmacokinetics, safety and immunomodulatory effects
of human recombinant interleukin-1 receptor antagonist
in healthy humans. Cytokine 1992: 4: 353360.
68. Greenfeder SA, Nunes P, Kwee L, Labow M, Chizzonite RA,
Ju G. Molecular cloning and characterization of a second
subunit of the interleukin 1 receptor complex. J Biol Chem
1995: 270: 1375713765.
69. Greenstein G, Hart TC. A critical assessment of interleukin-
1 (IL-1) genotyping when used in a genetic susceptibility
test for severe chronic periodontitis. J Periodontol 2002: 73:
231247.
70. Greenstein G, Hart TC. Clinical utility of a genetic suscept-
ibility test for severe chronic periodontitis: a critical eva-
luation. J Am Dent Assoc 2002: 133: 452459.
71. Groux H, O'Garra A, Bigler M, Rouleau M, Antonenko S, de
Vries JE, Roncarolo MG. A CD4 T-cell subset inhibits
antigen-specific T-cell responses and prevents colitis. Nat-
ure 1997: 389: 737742.
178
Taylor et al.
72. Guasch JF, Bertina RM, Reitsma PH. Five novel intragenic
dimorphisms in the human interleukin-1 genes combine
to high informativity. Cytokine 1996: 8: 598602.
73. Haffajee AD, Socransky SS, Smith C, Dibart S. Microbial
risk indicators for periodontal attachment loss. J Period-
ontal Res 1991: 26: 293296.
74. Hajeer AH, Hutchinson IV. Influence of TNFa gene poly-
morphisms on TNFa production and disease. Hum Immu-
nol 2001: 62: 11911199.
75. Hart T. Genetic risk factors for early-onset periodontitis.
J Periodontol 1996: 67: 355366.
76. Hart TC, Kornman KS. Genetic factors in the pathogenesis
of periodontitis. Periodontol 2000 1997: 14: 202215.
77. Hassell TM, Harris EL. Genetic influences in caries and
periodontal diseases. Crit Rev Oral Biol Med 1995: 6:
319342.
78. Haukim N, Bidwell JL, Smith AJ, Keen LJ, Gallagher G,
Kimberly P, Huizinga T, McDermott MF, Oksenberg J,
McNicholl J, Pociot F, Hardt C, D'Alfonso S. Cytokine gene
polymorphism in human disease: on-line databases, Sup-
plement 2. Genes Immun 2002: 3: 313330.
79. Heasman PA, Collins JG, Offenbacher S. Changes in crevi-
cular fluid levels of interleukin-1b, leukotriene B4, prosta-
glandin E2, thromboxane B2 and tumour necrosis factor a
in experimental gingivitis in humans. J Periodontal Res
1993: 28: 241247.
80. Heesen M, Bloemeke B, Heussen N, Kunz D. Can the
interleukin-6 response to endotoxin be predicted? Studies
of the influence of a promoter polymorphism of the inter-
leukin-6 gene, gender, the density of the endotoxin recep-
tor CD14, and inflammatory cytokines. Crit Care Med 2002:
30: 664669.
81. Heesen M, Obertacke U, Schade FU, Bloemeke B, Ma-
jetschak M. The interleukin-6 G (174)C polymorphism
and the ex vivo interleukin-6 response to endotoxin in
severely injured blunt trauma patients. Eur Cytokine Netw
2002: 13: 7277.
82. Hennig BJ, Parkhill JM, Chapple IL, Heasman PA, Taylor JJ.
Dinucleotide repeat polymorphism in the interleukin-10
gene promoter (IL-10.G) and genetic susceptibility to
early-onset periodontal disease. Genes Immun 2000: 1:
402404.
83. Higashi MK, Veenstra DL, del Aguila K Hujoel P. The cost-
effectiveness of interleukin-1 genetic testing for periodon-
tal disease. J Periodontol 2002: 73: 14741484.
84. Hill AV. Immunogenetics. Defence by diversity. Nature
1999: 398: 668669.
85. Hill AV. The genomics and genetics of human infectious
disease susceptibility. Annu Rev Genomics Hum Genet
2001: 2: 373400.
86. Hodge P, Michalowicz B. Genetic predisposition to period-
ontitis in children and young adults. Periodontol 2000
2001: 26: 113134.
87. Hodge PJ, Riggio MP, Kinane DF. Failure to detect an
association with IL1 genotypes in European Caucasians
with generalised early onset periodontitis. J Clin Period-
ontol 2001: 28: 430436.
88. Honig J, Rordorf-Adam C, Siegmund C, Wiedemann W,
Erard F. Increased interleukin-1b (IL-1b) concentration
in gingival tissue from periodontitis patients. J Periodontal
Res 1989: 24: 362367.
89. Huizinga TW, Westendorp RG, Bollen EL, Keijsers V,
Brinkman BM, Langermans JA, Breedveld FC, Verweij CL,
van de GL, Dams L, Crusius JB, Garcia-Gonzalez A, van
Oosten BW, Polman CH, Pena AS. TNF-a promoter poly-
morphisms, production and susceptibility to multiple
sclerosis in different groups of patients. J Neuroimmunol
1997: 72: 149153.
90. Hulkkonen J, Laippala P, Hurme M. A rare allele combina-
tion of the interleukin-1 gene complex is associated with
high interleukin-1b plasma levels in healthy individuals.
Eur Cytokine Netw 2000: 11: 251255.
91. Hurme M, Santtila S. IL-1 receptor antagonist (IL-1Ra)
plasma levels are co-ordinately regulated by both IL-1Ra
and IL-1b genes. Eur J Immunol 1998: 28: 25982602.
92. Irwin CR, Myrillas TT. The role of IL-6 in the pathogenesis
of periodontal disease. Oral Dis 1998: 4: 4347.
93. Ishihara Y, Zhang JB, Fakher M, Best AM, Schenkein HA,
Barbour SE, Tew JG. Non-redundant roles for interleukin-
1a and interleukin-1b in regulating human IgG2. J Period-
ontol 2001: 72: 13321339.
94. Jacob CO, Fronek Z, Lewis GD, Koo M, Hansen JA, McDe-
vitt HO. Heritable major histocompatibility complex class
II-associated differences in production of tumor necrosis
factor a: relevance to genetic predisposition to systemic
lupus erythematosus. Proc Natl Acad Sci USA 1990: 87:
12331237.
95. Jarrous N, Kaempfer R. Induction of human interleukin-1
gene expression by retinoic acid and its regulation at pro-
cessing of precursor transcripts. J Biol Chem 1994: 269:
2314123149.
96. Jeffreys AJ, Wilson V, Thein SL, Weatherall DJ, Ponder BA.
DNA ``fingerprints'' and segregation analysis of multiple
markers in human pedigrees. Am J Hum Genet 1986: 39:
1124.
97. Johnson GC, Esposito L, Barratt BJ, Smith AN, Heward J,
Di Genova G, Ueda H, Cordell HJ, Eaves IA, Dudbridge
F, Twells RC, Payne F, Hughes W, Nutland S, Stevens H,
Carr P, Tuomilehto-Wolf E, Tuomilehto J, Gough SC,
Clayton DG, Todd JA. Haplotype tagging for the identi-
fication of common disease genes. Nat Genet 2001: 29:
233237.
98. de Jong BA, Westendorp RG, Bakker AM, Huizinga TW.
Polymorphisms in or near tumour necrosis factor (TNF)-
gene do not determine levels of endotoxin-induced TNF
production. Genes Immun 2002: 3: 2529.
99. Keavney B, McKenzie C, Parish S, Palmer A, Clark S,
Youngman L, Delepine M, Lathrop M, Peto R, Collins R.
Large-scale test of hypothesised associations between the
angiotensin-convertingenzyme insertion/deletion poly-
morphism and myocardial infarction in about 5000 cases
and 6000 controls. International Studies of Infarct Survival
(ISIS) Collaborators. Lancet 2000: 355: 434442.
100. Kilpinen S, Hulkkonen J, Wang XY, Hurme M. The promo-
ter polymorphism of the interleukin-6 gene regulates in-
terleukin-6 production in neonates but not in adults. Eur
Cytokine Netw 2001: 12: 6268.
101. Kinane DF, Chestnutt IG. Smoking and periodontal dis-
ease. Crit Rev Oral Biol Med 2000: 11: 356365.
102. Kinane DF, Lappin DF. Clinical, pathological and immuno-
logical aspects of periodontal disease. Acta Odontol Scand
2001: 59: 154160.
103. Kinane DF, Hodge P, Ellis R, Gallagher G. Analysis of ge-
netic polymorphisms at the interleukin-10 and tumour
necrosis factor loci in early-onset periodontitis. J Period-
ontal Res 1999: 34: 379386.
179
Cytokine gene polymorphism and immunoregulation
104. Knight JC, Kwiatkowski D. Inherited variability of tumor
necrosis factor production and susceptibility to infectious
disease. Proc Assoc Am Physicians 1999: 111: 290298.
105. Knight JC, Udalova I, Hill AV, Greenwood BM, Peshu N,
Marsh K, Kwiatkowski D. A polymorphism that affects
OCT- 1 binding to the TNF promoter region is associated
with severe malaria. Nat Genet 1999: 22: 145150.
106. Kominato Y, Galson D, Waterman WR, Webb AC, Auron
PE. Monocyte expression of the human prointerleukin 1b
gene (IL1b) is dependent on promoter sequences which
bind the hematopoietic transcription factor Spi1/PU.1.
Mol Cell Biol 1995: 15: 5968.
107. Kornman KS, di Giovine FS. Genetic variations in cytokine
expression: a risk factor for severity of adult periodontitis.
Ann Periodontol 1998: 3: 327338.
108. Kornman KS, Crane A, Wang HY, di Giovine FS, Newman
MG, Pirk FW, Wilson TG, Jr, Higginbottom FL, Duff GW.
The interleukin-1 genotype as a severity factor in adult
periodontal disease. J Clin Periodontol 1997: 24: 7277.
109. Kornman KS, Page RC, Tonetti MS. The host response to
the microbial challenge in periodontitis: assembling the
players. Periodontol 2000 1997: 14: 3353.
110. Kornman KS, Pankow J, Offenbacher S, Beck J, di Giovine
F, Duff GW. Interleukin-1 genotypes and the association
between periodontitis and cardiovascular disease. J Period-
ontal Res 1999: 34: 353357.
111. Kracht M, Saklatvala J. Transcriptional and post-transcrip-
tional control of gene expression in inflammation. Cyto-
kine 2002: 20: 91106.
112. Kroeger KM, Steer JH, Joyce DA, Abraham LJ. Effects of
stimulus and cell type on the expression of the 308 tu-
mour necrosis factor promoter polymorphism. Cytokine
2000: 12: 110119.
113. Kubota T, McNamara DM, Wang JJ, Trost M, McTiernan
CF, Mann DL, Feldman AM. Effects of tumor necrosis
factor gene polymorphisms on patients with congestive
heart failure. VEST Investigators for TNF Genotype
Analysis. Vesnarinone Survival Trial. Circulation 1998: 97:
24992501.
114. Laine ML, Farre MA, Gonzalez G, van Dijk LJ, Ham AJ,
Winkel EG, Crusius JB, Vandenbroucke JP, van Winkelhoff
AJ, Pena AS. Polymorphisms of the interleukin-1gene family,
oral microbial pathogens, and smoking in adult period-
ontitis. J Dent Res 2001: 80: 16951699.
115. Lander ES. Array of hope. Nat Genet 1999: 21: 34.
116. Lander ES, Schork NJ. Genetic dissection of complex traits.
Science 1994: 265: 20372048.
117. Landi L, Amar S, Polins AS, Van Dyke TE. Host mechan-
isms in the pathogenesis of periodontal disease. Curr Opin
Periodontol 1997: 4: 310.
118. Lang NP, Tonetti MS, Suter J, Sorrell J, Duff GW, Kornman
KS. Effect of interleukin-1 gene polymorphisms on gingival
inflammation assessed by bleeding on probing in a period-
ontal maintenance population. J Periodontal Res 2000: 35:
102107.
119. Liew FY. T (H)1 and T (H)2 cells: a historical perspective.
Nat Rev Immunol 2002: 2: 5560.
120. Lindhe J, Socransky SS, Nyman S, Haffajee A, Westfelt E.
``Critical probing depths'' in periodontal therapy. J Clin
Periodontol 1982: 9: 323336.
121. Mark LL, Haffajee AD, Socransky SS, Kent RL, Jr, Guerrero
D, Kornman K, Newman M, Stashenko P. Effect of the
interleukin-1 genotype on monocyte IL-1b expression in
subjects with adult periodontitis. J Periodontal Res 2000:
35: 172177.
122. Masada MP, Persson R, Kenney JS, Lee SW, Page RC, Alli-
son AC. Measurement of interleukin-1a and -1b in gingival
crevicular fluid: implications for the pathogenesis of per-
iodontal disease. J Periodontal Res 1990: 25: 156163.
123. Maurer M, Kruse N, Giess R, Toyka KV, Rieckmann P.
Genetic variation at position 1082 of the interleukin 10
(IL10) promotor and the outcome of multiple sclerosis.
J Neuroimmunol 2000: 104: 98100.
124. McDevitt HO. Discovering the role of the major histocom-
patibility complex in the immune response. Annu Rev Im-
munol 2000: 18: 117.
125. McDevitt MJ, Wang HY, Knobelman C, Newman MG, di
Giovine FS, Timms J, Duff GW, Kornman KS. Interleukin-1
genetic association with periodontitis in clinical practice.
J Periodontol 2000: 71: 156163.
126. McFarlane CG, Reynolds JJ, Meikle MC. The release of
interleukin-1 b, tumor necrosis factor-a and interferon-g by
cultured peripheral blood mononuclear cells from patients
with periodontitis. J Periodontal Res 1990: 25: 207214.
127. McGuire MK, Nunn ME. Prognosis versus actual outcome.
IV. The effectiveness of clinical parameters and IL-1 geno-
type in accurately predicting prognoses and tooth survival.
J Periodontol 1999: 70: 4956.
128. McGuirk P, Mills KH. Pathogen-specific regulatory T cells
provoke a shift in the Th1/Th2 paradigm in immunity to
infectious diseases. Trends Immunol 2002: 23: 450455.
129. Meisel P, Siegemund A, Dombrowa S, Sawaf H, Fanghaenel
J, Kocher T. Smoking and polymorphisms of the interleu-
kin-1 gene cluster (IL-1a, IL-1b, and IL-1RN) in patients
with periodontal disease. J Periodontol 2002: 73: 2732.
130. Michalowicz BS. Genetic and heritable risk factors in per-
iodontal disease. J Periodontol 1994: 65: 479488.
131. Molvig J, Baek L, Christensen P, Manogue KR, Vlassara H,
Platz P, Nielsen LS, Svejgaard A, Nerup J. Endotoxin-sti-
mulated human monocyte secretion of interleukin 1, tu-
mour necrosis factor a, and prostaglandin E2 shows stable
interindividual differences. Scand J Immunol 1988: 27:
705716.
132. Monks BG, Martell BA, Buras JA, Fenton MJ. An upstream
protein interacts with a distinct protein that binds to the
cap site of the human interleukin 1b gene. Mol Immunol
1994: 31: 139151.
133. Mori N, Prager D. Transactivation of the interleukin-1a
promoter by human T-cell leukemia virus type I and
type II Tax proteins. Blood 1996: 87: 34103417.
134. Nicklin MJ, Weith A, Duff GW. A physical map of the region
encompassing the human interleukin-1a, interleukin-1b,
and interleukin-1 receptor antagonist genes. Genomics
1994: 19: 382384.
135. Nicklin MJ, Barton JL, Nguyen M, FitzGerald MG, Duff
GW, Kornman K. A sequence-based map of the nine genes
of the human interleukin-1 cluster. Genomics 2002: 79:
718725.
136. O'Neill LA, Dinarello CA. The IL-1 receptor/toll-like recep-
tor superfamily: crucial receptors for inflammation and
host defense. Immunol Today 2000: 21: 206209.
137. Offenbacher S. Periodontal diseases: pathogenesis. Ann
Periodontol 1996: 1: 821878.
138. Offenbacher S, Heasman PA, Collins JG. Modulation of
host PGE2 secretion as a determinant of periodontal
disease expression. J Periodontol 1993: 64: 432444.
180
Taylor et al.
139. Okada H, Murakami S. Cytokine expression in periodontal
health and disease. Crit Rev Oral Biol Med 1998: 9: 248266.
140. Page RC, Schroeder HE. Pathogenesis of inflammatory
periodontal disease. A summary of current work. Lab
Invest 1976: 34: 235249.
141. Page RC, Offenbacher S, Schroeder HE, Seymour GJ, Korn-
man KS. Advances in the pathogenesis of periodontitis:
summary of developments, clinical implications and fu-
ture directions. Periodontol 2000 1997: 14: 216248.
142. Papapanou PN, Neiderud AM, Sandros J, Dahlen G. Inter-
leukin-1 gene polymorphism and periodontal status. A
case-control study. J Clin Periodontol 2001: 28: 389396.
143. Parkhill JM, Hennig BJ, Chapple IL, Heasman PA, Taylor JJ.
Association of interleukin-1 gene polymorphisms with
early-onset periodontitis. J Clin Periodontol 2000: 27:
682689.
144. Pociot F, Molvig J, Wogensen L, Worsaae H, Nerup J. A
TaqI polymorphism in the human interleukin-1b (IL-1b)
gene correlates with IL-1b secretion in vitro. Eur J Clin
Invest 1992: 22: 396402.
145. Pravica V, Asderakis A, Perrey C, Hajeer A, Sinnott PJ,
Hutchinson IV. In vitro production of IFN-g correlates with
CA repeat polymorphism in the human IFN-g gene. Eur J
Immunogenet 1999: 26: 13.
146. Preiss DS, Meyle J. Interleukin-1b concentration of gingival
crevicular fluid. J Periodontol 1994: 65: 423428.
147. Ricciardi-Castagnoli P, Granucci F. Opinion: interpretation
of the complexity of innate immune responses by func-
tional genomics. Nat Rev Immunol 2002: 2: 881889.
148. Risch NJ. Searching for genetic determinants in the new
millennium. Nature 2000: 405: 847856.
149. Risch N, Teng J. The relative power of family-based and
case-control designs for linkage disequilibrium studies of
complex human diseases I. DNA pooling. Genome Res
1998: 8: 12731288.
150. Rogers MA, Figliomeni L, Baluchova K, Tan AE, Davies G,
Henry PJ, Price P. Do interleukin-1 polymorphisms predict
the development of periodontitis or the success of dental
implants? J Periodontal Res 2002: 37: 3741.
151. Sachidanandam R, Weissman D, Schmidt SC, Kakol JM,
Stein LD, Marth G, Sherry S, Mullikin JC, Mortimore BJ,
Willey DL, Hunt SE, Cole CG, Coggill PC, Rice CM, Ning Z,
Rogers J, Bentley DR, Kwok PY, Mardis ER, Yeh RT, Schultz
B, Cook L, Davenport R, Dante M, Fulton L, Hillier L,
Waterston RH, McPherson JD, Gilman B, Schaffner S,
Van Etten WJ, Reich D, Higgins J, Daly MJ, Blumenstiel
B, Baldwin J, Stange-Thomann N, Zody MC, Linton L,
Lander ES, Altshuler D. A map of human genome sequence
variation containing 1.42 million single nucleotide poly-
morphisms. Nature 2001: 409: 928933.
152. Salvi GE, Lawrence HP, Offenbacher S, Beck JD. Influence
of risk factors on the pathogenesis of periodontitis. Period-
ontol 2000 1997: 14: 173201.
153. Sangnes G. Traumatization of teeth and gingiva related to
habitual tooth cleaning procedures. J Clin Periodontol
1976: 3: 94103.
154. Santtila S, Savinainen K, Hurme M. Presence of the IL-1RA
allele 2 (IL1RN
2) is associated with enhanced IL-1b pro-
duction in vitro. Scand J Immunol 1998: 47: 195198.
155. Scarel-Caminaga RM, Trevilatto PC, Souza AP, Brito RB,
Line SR. Investigation of an IL-2 polymorphism in patients
with different levels of chronic periodontitis. J Clin Period-
ontol 2002: 29: 587591.
156. Schenkein HA. Finding genetic risk factors for periodontal
diseases: is the climb worth the view? Periodontol 2000
2002: 30: 7990.
157. Schindler R, Clark BD, Dinarello CA. Dissociation between
interleukin-1b mRNA and protein synthesis in human peri-
pheral blood mononuclear cells. J Biol Chem 1990: 265:
1023210237.
158. Schindler R, Ghezzi P, Dinarello CA. IL-1 induces IL-1. IV.
IFN-g suppresses IL-1 but not lipopolysaccharide-induced
transcription of IL-1. J Immunol 1990: 144: 22162222.
159. Seymour GJ. Importance of the host response in the
periodontium. J Clin Periodontol 1991: 18: 421426.
160. Seymour GJ, Gemmell E. Cytokines in periodontal disease:
where to from here? Acta Odontol Scand 2001: 59: 167173.
161. Shaffer AL, Rosenwald A, Hurt EM, Giltnane JM, Lam LT,
Pickeral OK, Staudt LM. Signatures of the immune res-
ponse. Immunity 2001: 15: 375385.
162. Shapira L, Soskolne WA, Sela MN, Offenbacher S, Barak V.
The secretion of PGE2, IL-1b, IL-6, and TNF a by adherent
mononuclear cells from early onset periodontitis patients.
J Periodontol 1994: 65: 139146.
163. Sherry ST, Ward MH, Kholodov M, Baker J, Phan L,
Smigielski EM, Sirotkin K. dbSNP: the NCBI database of
genetic variation. Nucl Acids Res 2001: 29: 308311.
164. Shirakawa F, Saito K, Bonagura CA, Galson DL, Fenton MJ,
Webb AC, Auron PE. The human prointerleukin 1b gene
requires DNA sequences both proximal and distal to the
transcription start site for tissue-specific induction. Mol
Cell Biol 1993: 13: 13321344.
165. Shirodaria S, Smith J, McKay IJ, Kennett CN, Hughes FJ.
Polymorphisms in the IL-1A gene are correlated with levels
of interleukin-1a protein in gingival crevicular fluid of
teeth with severe periodontal disease. J Dent Res 2000:
79: 18641869.
166. Sims JE, Giri JG, Dower SK. The two interleukin-1 receptors
play different roles in IL-1 actions. Clin Immunol Immu-
nopathol 1994: 72: 914.
167. Sims JE, Nicklin MJ, Bazan JF, Barton JL, Busfield SJ, Ford
JE, Kastelein RA, Kumar S, Lin H, Mulero JJ, Pan J, Pan Y,
Smith DE, Young PR. A new nomenclature for IL-1-family
genes. Trends Immunol 2001: 22: 536537.
168. Socransky SS, Haffajee AD, Goodson JM, Lindhe J. New
concepts of destructive periodontal disease. J Clin Period-
ontol 1984: 11: 2132.
169. Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL Jr.
Microbial complexes in subgingival plaque. J Clin Period-
ontol 1998: 25: 134144.
170. Socransky SS, Haffajee AD, Smith C, Duff GW. Micro-
biological parameters associated with IL-1 gene poly-
morphisms in periodontitis patients. J Clin Periodontol
2000: 27: 810818.
171. Stashenko P, Fujiyoshi P, Obernesser MS, Prostak L,
Haffajee AD, Socransky SS. Levels of interleukin 1 b in
tissue from sites of active periodontal disease. J Clin Peri-
odontol 1991: 18: 548554.
172. Stashenko P, Jandinski JJ, Fujiyoshi P, Rynar J, Socransky
SS. Tissue levels of bone resorptive cytokines in period-
ontal disease. J Periodontol 1991: 62: 504509.
173. Tai H, Endo M, Shimada Y, Gou E, Orima K, Kobayashi
T, Yamazaki K, Yoshie H. Association of interleukin-1
receptor antagonist gene polymorphisms with early onset
periodontitis in Japanese. J Clin Periodontol 2002: 29:
882888.
181
Cytokine gene polymorphism and immunoregulation
174. Tarlow JK, Blakemore AI, Lennard A, Solari R, Hughes HN,
Steinkasserer A, Duff GW. Polymorphism in human IL-1
receptor antagonist gene intron 2 is caused by variable
numbers of an 86-bp tandem repeat. Hum Genet 1993:
91: 403404.
175. Tatakis DN. Interleukin-1 and bone metabolism: a review.
J Periodontol 1993: 64: 416431.
176. Taylor SL, Renshaw BR, Garka KE, Smith DE, Sims JE.
Genomic organization of the interleukin-1 locus. Genomics
2002: 79: 726733.
177. Teng J, Risch N. The relative power of family-based and
case-control designs for linkage disequilibrium studies of
complex human diseases. II. Individual genotyping. Gen-
ome Res 1999: 9: 234241.
178. Terry CF, Loukaci V, Green FR. Cooperative influence of
genetic polymorphisms on interleukin 6 transcriptional
regulation. J Biol Chem 2000: 275: 1813818144.
179. Tewari A, Buhles WC Jr, Starnes HF Jr, . Preliminary report:
effects of interleukin-1 on platelet counts. Lancet 1990:
336: 712714.
180. Thomson WM, Edwards SJ, Dobson LE, Tompkins GF,
Poulton R, Knight DA, Braithwaite AW. IL-1 genotype
and adult periodontitis among young New Zealanders.
J Dent Res 2001: 80: 17001703.
181. Tomar SL, Asma S. Smoking-attributable periodontitis in
the United States: findings from NHANES III. National
Health and Nutrition Examination Survey. J Periodontol
2000: 71: 743751.
182. Tonetti MS, Imboden MA, Lang NP. Neutrophil migration
into the gingival sulcus is associated with transepithelial
gradients of interleukin-8 and ICAM1. J Periodontol 1998:
69: 11391147.
183. Tsukada J, Saito K, Waterman WR, Webb AC, Auron PE.
Transcription factors NF-IL6 and CREB recognize a com-
mon essential site in the human prointerleukin 1 b gene.
Mol Cell Biol 1994: 14: 72857297.
184. Turner DM, Williams DM, Sankaran D, Lazarus M, Sinnott
PJ, Hutchinson IV. An investigation of polymorphism in
the interleukin-10 gene promoter. Eur J Immunogenet
1997: 24: 18.
185. Udalova IA, Kwiatkowski D. Interaction of AP1 with a
cluster of NF-kB binding elements in the human TNF
promoter region. Biochem Biophys Res Commun 2001:
289: 2533.
186. Udalova IA, Mott R, Field D, Kwiatkowski D. Quantitative
prediction of NF-kB DNAprotein interactions. Proc Natl
Acad Sci USA 2002: 99: 81678172.
187. Vamvakopoulos J, Green C, Metcalfe S. Genetic control of
IL-1b bioactivity through differential regulation of the IL-1
receptor antagonist. Eur J Immunol 2002: 32: 29882996.
188. Walker SJ, Van Dyke TE, Rich S, Kornman KS, di Giovine FS,
Hart TC. Genetic polymorphisms of the IL-1a and IL-1b
genes in African-American LJP patients and an African-
American control population. J Periodontol 2000: 723728.
189. Wang DG, Fan JB, Siao CJ, Berno A, Young P, Sapolsky R,
Ghandour G, Perkins N, Winchester E, Spencer J, Kruglyak
L, Stein L, Hsie L, Topaloglou T, Hubbell E, Robinson E,
Mittmann M, Morris MS, Shen N, Kilburn D, Rioux J, Nus-
baum C, Rozen S, Hudson TJ, Lander ES. Large-scale iden-
tification, mapping, and genotyping of single-nucleotide
polymorphisms in the human genome. Science 1998: 280:
10771082.
190. Weber JL. Human DNA polymorphisms and methods of
analysis. Curr Opin Biotechnol 1990: 1: 166171.
191. Weiss KM, Terwilliger JD. How many diseases does it take
to map a gene with SNPs? Nat Genet 2000: 26: 151157.
192. Wilson AG, de Vries N, Pociot F, di Giovine FS, van der
Putte LB, Duff GW. An allelic polymorphism within the
human tumor necrosis factor a promoter region is strongly
associated with HLA A1, B8, and DR3 alleles. J Exp Med
1993: 177: 557560.
193. Wilson TG, Nunn M. The relationship between the inter-
leukin-1 periodontal genotype and implant loss. Initial
data. J Periodontol 1999: 70: 724729.
194. Wright AF, Carothers AD, Campbell H. Gene-environment
interactions the BioBank UK study. Pharmacogenomics J
2002: 2: 7582.
195. Xie Y, Chen C, Stevenson MA, Auron PE, Calderwood SK.
Heat shock factor 1 represses transcription of the IL-1b
gene through physical interaction with the nuclear factor
of interleukin 6. J Biol Chem 2002: 277: 1180211810.
196. Yamazaki K, Tab K, Nakajima T, Ohsawa Y, Ueki K, Itoh H,
Yoshie H. Interleukin-10 gene promoter polymorphism in
Japanese patients with adult and early-onset periodontitis.
J Clin Periodontol 2001: 28: 828832.
197. Yang Z, Wara-Aswapati N, Chen C, Tsukada J, Auron PE.
NF-IL6 (C/EBPb) vigorously activates IL1b gene expression
via a Spi-1 (PU.1) protein-protein tether. J Biol Chem 2000:
275: 2127221277.
198. Zadeh HH, Nichols FC, Miyasaki KT. The role of the cell-
mediated immune response to Actinobacillus actinomyce-
temcomitans and Porphyromonas gingivalis in periodonti-
tis. Periodontol 2000 1999: 20: 239288.
199. Zaldivar F, Nugent DJ, Imfeld K, Berman MA. Identifica-
tion of a novel regulatory element in the human interleu-
kin 1a (IL-1a) gene promoter. Cytokine 2002: 20: 130135.
200. Zhang Y, Rom WN. Regulation of the interleukin-1b (IL-1b)
gene by mycobacterial components and lipopolysacchar-
ide is mediated by two nuclear factor-IL6 motifs. Mol Cell
Biol 1993: 13: 38313837.
182
Taylor et al.
You might also like
- Cytokines and Prostaglandins in Immune Homeostasis and Tissue Destruction in Periodontal DiseaseDocument32 pagesCytokines and Prostaglandins in Immune Homeostasis and Tissue Destruction in Periodontal DiseaseDiana GomezNo ratings yet
- The Cytokine Network Involved in The Host Immune Response To PeriodontitisDocument13 pagesThe Cytokine Network Involved in The Host Immune Response To PeriodontitisGeorgi GugicevNo ratings yet
- Inflmsi JosDocument27 pagesInflmsi Jospramita wahyu dyastiNo ratings yet
- Cytokine Networks Regulating Inflammation and Immune Defense in The Oral CavityDocument10 pagesCytokine Networks Regulating Inflammation and Immune Defense in The Oral CavityReiska KumalaNo ratings yet
- Journal Kiki - VeldaDocument18 pagesJournal Kiki - VeldaYvonne DoyleNo ratings yet
- Implications Pathogenesis: GingivalDocument30 pagesImplications Pathogenesis: GingivalI Gede MahardikaNo ratings yet
- (7P) Host-Microbial Interactions in Periodontal DiseasesDocument6 pages(7P) Host-Microbial Interactions in Periodontal DiseasesNegrus StefanNo ratings yet
- Immunological Differences and Similarities Between Chronic Periodontitis and Aggressive PeriodontitisDocument13 pagesImmunological Differences and Similarities Between Chronic Periodontitis and Aggressive PeriodontitisSiti Harwati DesrimelinaNo ratings yet
- Nihms371504 PDFDocument37 pagesNihms371504 PDFYuniarNo ratings yet
- Stüber F, 2004Document6 pagesStüber F, 2004Hendry SusantoNo ratings yet
- Periodontology 2000 - 2017 - Hajishengallis - Revisiting The Page Schroeder Model The Good The Bad and The Unknowns inDocument36 pagesPeriodontology 2000 - 2017 - Hajishengallis - Revisiting The Page Schroeder Model The Good The Bad and The Unknowns inrmartins76No ratings yet
- Etiopatogênses Artigo ORIGINALDocument33 pagesEtiopatogênses Artigo ORIGINALLego is LefeNo ratings yet
- Hajishengallis 2020 - Current Understanding of Periodontal Disease PathogenesisDocument38 pagesHajishengallis 2020 - Current Understanding of Periodontal Disease PathogenesisLuiz Guilherme FiorinNo ratings yet
- Preshaw 2018 Periodontology - 2000Document19 pagesPreshaw 2018 Periodontology - 2000Dr. DeeptiNo ratings yet
- Genetic Factors Pathogenesis Periodontitis: Thomas Hart KornmanDocument14 pagesGenetic Factors Pathogenesis Periodontitis: Thomas Hart KornmanPiyusha SharmaNo ratings yet
- Streptococcus PyogenesDocument11 pagesStreptococcus PyogenesverajovvanaNo ratings yet
- Title ManuscriptsDocument19 pagesTitle ManuscriptsSam Bradley DavidsonNo ratings yet
- Fimmu 06 00555Document20 pagesFimmu 06 00555www.henry1020No ratings yet
- The Causes and Consequences of Variation in Human Cytokine Production in Health PDFDocument9 pagesThe Causes and Consequences of Variation in Human Cytokine Production in Health PDFLluis GomezNo ratings yet
- Dyke Et Al-2013-Journal of Clinical PeriodontologyDocument7 pagesDyke Et Al-2013-Journal of Clinical PeriodontologyElena IancuNo ratings yet
- Review Article Porphyromonas Gingivalis Periodontal Infection and ItsDocument11 pagesReview Article Porphyromonas Gingivalis Periodontal Infection and ItsMitzi Carolina SierraNo ratings yet
- T CellsDocument12 pagesT CellsGabriela CismaruNo ratings yet
- UTI and Innate ImmuneDocument11 pagesUTI and Innate ImmuneJose HumbertoNo ratings yet
- Why Have Clinical Trials in Sepsis FailedDocument9 pagesWhy Have Clinical Trials in Sepsis FailedxiaojianNo ratings yet
- CQTLDocument28 pagesCQTLrenyuandshisenyuanNo ratings yet
- Host Modulation in Periodontics PDFDocument12 pagesHost Modulation in Periodontics PDFCindyJessica100% (1)
- GENETICSDocument9 pagesGENETICSDewy HazeNo ratings yet
- Periodontal Infectogenomics: ReviewDocument6 pagesPeriodontal Infectogenomics: ReviewNadya PurwantyNo ratings yet
- HHS Public AccessDocument52 pagesHHS Public AccessIdmNo ratings yet
- Role of Receptor Activator of Ligand and OsteoprogeterinDocument20 pagesRole of Receptor Activator of Ligand and OsteoprogeterindendydwirizkiNo ratings yet
- Pro InflammatoryDocument6 pagesPro InflammatoryfridaniyantiNo ratings yet
- Leukocyte Adhesion Deficiency I (LAD I) and PeriodontitisDocument10 pagesLeukocyte Adhesion Deficiency I (LAD I) and PeriodontitisnadhiracindyNo ratings yet
- Neuroimunomodulação 3 - Complicações para o HospedeiroDocument3 pagesNeuroimunomodulação 3 - Complicações para o HospedeiroLetícia Maraqui PrezziNo ratings yet
- Review: New Concepts in The Pathophysiology of Inflammatory Bowel DiseaseDocument11 pagesReview: New Concepts in The Pathophysiology of Inflammatory Bowel DiseaseReynalth Andrew Sinaga100% (1)
- Host Modulation in PeriodonticsDocument12 pagesHost Modulation in PeriodonticsFirma Nurdinia DewiNo ratings yet
- Prevotella SPPDocument12 pagesPrevotella SPPRobert Alejandro Rodriguez NinoNo ratings yet
- Interactions Between Parasites and Human MicrobiotDocument6 pagesInteractions Between Parasites and Human MicrobiotGregorio De Las CasasNo ratings yet
- Silva 2019 The Role of TNF As A ProinflammatoDocument7 pagesSilva 2019 The Role of TNF As A ProinflammatoWaldenei DNo ratings yet
- Articulo 5Document20 pagesArticulo 5Daniella Rodriguez ReyesNo ratings yet
- Microorganisms 11 00115Document15 pagesMicroorganisms 11 00115Mariana PalaciosNo ratings yet
- Biomedicine & Pharmacotherapy: ReviewDocument12 pagesBiomedicine & Pharmacotherapy: Reviewkorede juniorNo ratings yet
- Avanços Vacinas Contra Fungos 2007Document33 pagesAvanços Vacinas Contra Fungos 2007Bruno Nogueira BarrosNo ratings yet
- Molecular Aspects Perio Pathogenesis MeyleDocument11 pagesMolecular Aspects Perio Pathogenesis MeyleChristine LomuntadNo ratings yet
- Bacterial Invasion of Epithelial Cells and Spreading in Periodontal TissueDocument16 pagesBacterial Invasion of Epithelial Cells and Spreading in Periodontal TissueEduardo Garza GarzaNo ratings yet
- The Role of Inflammation and Genetics in Periodontal DiseaseDocument14 pagesThe Role of Inflammation and Genetics in Periodontal DiseaseNishtha KumarNo ratings yet
- Cytokine: Mohammad M.Y. Khorasani, Gholamhossein Hassanshahi, Aniela Brodzikowska, Hossein Khorramdelazad TDocument8 pagesCytokine: Mohammad M.Y. Khorasani, Gholamhossein Hassanshahi, Aniela Brodzikowska, Hossein Khorramdelazad TJade LolongNo ratings yet
- Mapping The PathogenesisDocument9 pagesMapping The PathogenesisAnonymous k8rDEsJsU1No ratings yet
- Periodontal Microbial Complexes Associated With Specific Cell and Tissue ResponsesDocument11 pagesPeriodontal Microbial Complexes Associated With Specific Cell and Tissue ResponsesHiramNo ratings yet
- Periodontology 2000Document1,832 pagesPeriodontology 2000Adrian BoerNo ratings yet
- 10 1111@prd 12331 PDFDocument21 pages10 1111@prd 12331 PDFRaghadNaifRawabdehNo ratings yet
- Pulmonary, Sleep, and Critical Care Updates: Update in Tuberculosis and Nontuberculous Mycobacterial Disease 2010Document6 pagesPulmonary, Sleep, and Critical Care Updates: Update in Tuberculosis and Nontuberculous Mycobacterial Disease 2010Joseph Sipiran ReyesNo ratings yet
- Inflammation and RegenerationDocument6 pagesInflammation and RegenerationTaufiqurrahman Abdul DjabbarNo ratings yet
- Canan 2014 JLBDocument1 pageCanan 2014 JLBNandan GokhaleNo ratings yet
- Host Modulation Therapy - An Innovative Paradigm inDocument8 pagesHost Modulation Therapy - An Innovative Paradigm inpaper kitaNo ratings yet
- Cytoquine Storm and SepsisDocument12 pagesCytoquine Storm and SepsisEduardo ChanonaNo ratings yet
- Molecular Systems Biology - 2022 - Studniberg - Molecular Profiling Reveals Features of Clinical Immunity andDocument25 pagesMolecular Systems Biology - 2022 - Studniberg - Molecular Profiling Reveals Features of Clinical Immunity andFaiz SheeNo ratings yet
- Microbioma y OtorrinoDocument19 pagesMicrobioma y Otorrinodayenu barraNo ratings yet
- Periodontal Diseases As Bacterial Infection: Bascones Martinez A Figuero Ruiz EDocument8 pagesPeriodontal Diseases As Bacterial Infection: Bascones Martinez A Figuero Ruiz EWidaRostinaNo ratings yet
- Antifertility Vaccines: Peter J. Delves, Torben Lund and Ivan M. RoittDocument7 pagesAntifertility Vaccines: Peter J. Delves, Torben Lund and Ivan M. RoittLinguumNo ratings yet
- Antigen-Presentation and The Role of Dendritic Cells in PeriodontitisDocument23 pagesAntigen-Presentation and The Role of Dendritic Cells in PeriodontitiskochikaghochiNo ratings yet
- Ijp 18 5 Grandini 7Document6 pagesIjp 18 5 Grandini 7kochikaghochiNo ratings yet
- Ijp 18 5 Mack 9Document6 pagesIjp 18 5 Mack 9kochikaghochiNo ratings yet
- Effect of Original Water Content in Acrylic Resin On Processing ShrinkageDocument2 pagesEffect of Original Water Content in Acrylic Resin On Processing ShrinkagekochikaghochiNo ratings yet
- Peri-Implant Bone Loss As A Function of Tooth-Implant DistanceDocument7 pagesPeri-Implant Bone Loss As A Function of Tooth-Implant DistancekochikaghochiNo ratings yet
- Preoperative Radiologic Planning of Implant Surgery in Compromised PatientsDocument14 pagesPreoperative Radiologic Planning of Implant Surgery in Compromised PatientskochikaghochiNo ratings yet
- Diagnosis of Periodontal Manifestations of Systemic DiseasesDocument13 pagesDiagnosis of Periodontal Manifestations of Systemic DiseaseskochikaghochiNo ratings yet
- Periodontal Diagnoses and Classi®cation of Periodontal DiseasesDocument13 pagesPeriodontal Diagnoses and Classi®cation of Periodontal DiseaseskochikaghochiNo ratings yet
- Analysis of Host Responses and Risk For Disease Progression: Sinem E. Sahingur & Robert E. CohenDocument27 pagesAnalysis of Host Responses and Risk For Disease Progression: Sinem E. Sahingur & Robert E. CohenkochikaghochiNo ratings yet
- The Structures, Properties, and Functions of BiomoleculesDocument49 pagesThe Structures, Properties, and Functions of BiomoleculesKirsten Andrea MagallanesNo ratings yet
- Session No. 2.1. Biological Molecules - Carbohydrates and LipidsDocument31 pagesSession No. 2.1. Biological Molecules - Carbohydrates and LipidsShekaina Faith Cuizon LozadaNo ratings yet
- Mechanism and Regulation of FibrinolysisDocument8 pagesMechanism and Regulation of FibrinolysisNalini RooplalNo ratings yet
- MacromoleculesDocument16 pagesMacromoleculesLou MenesesNo ratings yet
- Blotting Assignment by MPhil 5,12Document31 pagesBlotting Assignment by MPhil 5,12Amina ChNo ratings yet
- Dna Replication: Meselson & Stahl's Experiment (1958)Document4 pagesDna Replication: Meselson & Stahl's Experiment (1958)Angie LawrenceNo ratings yet
- Diabetes and Insulin Signaling Case StudyDocument3 pagesDiabetes and Insulin Signaling Case StudyJoey Ma100% (2)
- TaqMan Universal PCR ProtocolDocument60 pagesTaqMan Universal PCR Protocolkrista_jw9525No ratings yet
- Allnex-2K-Epoxy Amine Systems Calculation Tool 012022-Final-Version-locked 4.1Document6 pagesAllnex-2K-Epoxy Amine Systems Calculation Tool 012022-Final-Version-locked 4.1Shani PatelNo ratings yet
- Biochem Lec 3Document97 pagesBiochem Lec 3yashika gargNo ratings yet
- Secondary MessengerDocument50 pagesSecondary MessengerFlorlin Grace YradNo ratings yet
- Restriction EnzymesDocument9 pagesRestriction EnzymesskmfscNo ratings yet
- Ion Ampliseq Exome Rdy Library Preparation: User GuideDocument44 pagesIon Ampliseq Exome Rdy Library Preparation: User GuideSurendra RajvanshiNo ratings yet
- Sanger SequencingDocument4 pagesSanger SequencingMilka RahmanNo ratings yet
- Day 4. Warm-Up. STAAR® Blitz. Science. BiologyDocument2 pagesDay 4. Warm-Up. STAAR® Blitz. Science. BiologyRaul Ramirez RangelNo ratings yet
- Nucleic Acids WorksheetDocument4 pagesNucleic Acids WorksheetNatalie PembertonNo ratings yet
- Transcription and Translation PracticeDocument2 pagesTranscription and Translation PracticeKajal VaghasiaNo ratings yet
- F3 Assignment 3.1 - Balanced DietDocument2 pagesF3 Assignment 3.1 - Balanced DietAshleyNo ratings yet
- Protein MicroarrayDocument40 pagesProtein MicroarrayMohd Uzair Ansari100% (1)
- BiomoelculeDocument2 pagesBiomoelculeDaniel VillahermosaNo ratings yet
- RNA Transcription and TranslationDocument11 pagesRNA Transcription and TranslationMaiSakurajimaNo ratings yet
- PBIO-534 Syllabus, Fall'13 (2) ADocument4 pagesPBIO-534 Syllabus, Fall'13 (2) AMike GNo ratings yet
- Macromolecule LabDocument6 pagesMacromolecule Labapi-271196093No ratings yet
- Antigen Processing and PresentationDocument2 pagesAntigen Processing and PresentationEllya Latifah IlyasNo ratings yet
- CBSE Quick Revision Notes CBSE Class-11 Biology Chapter-09 BiomoleculesDocument8 pagesCBSE Quick Revision Notes CBSE Class-11 Biology Chapter-09 BiomoleculesHARSH PahwaNo ratings yet
- Antisense RNA Technology and Its ApplicationsDocument2 pagesAntisense RNA Technology and Its Applicationssomu1No ratings yet
- Alexander Vologodskii - The Basics of Molecular Biology-Springer (2022)Document188 pagesAlexander Vologodskii - The Basics of Molecular Biology-Springer (2022)Rey M100% (2)
- Chapter 13 SummaryDocument5 pagesChapter 13 SummaryCharlotteNo ratings yet
- Science Quarter 4-Module 1 Protein Synthesis: NameDocument6 pagesScience Quarter 4-Module 1 Protein Synthesis: NameChristian jade QuijanoNo ratings yet
- BCH210 Midterm Exam 2015Document12 pagesBCH210 Midterm Exam 2015Jefin Abraham Mathews100% (1)