Professional Documents
Culture Documents
595 2012 Article 387
Uploaded by
ReZa Frisca0 ratings0% found this document useful (0 votes)
16 views5 pagesKISTA KOLEDOKUS
Original Title
595_2012_Article_387
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentKISTA KOLEDOKUS
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
16 views5 pages595 2012 Article 387
Uploaded by
ReZa FriscaKISTA KOLEDOKUS
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
CASE REPORT
Intrahepatic cholangiocarcinoma arising 28 years after excision
of a type IV-A congenital choledochal cyst: report of a case
Takafumi Kumamoto
Kuniya Tanaka
Kazuhisa Takeda
Kazunori Nojiri
Ryutaro Mori
Kouichi Taniguchi
Ryusei Matsuyama
Michio Ueda
Mitsutaka Sugita
Yasushi Ichikawa
Youji Nagashima
Itaru Endo
Received: 7 October 2011 / Accepted: 5 July 2012 / Published online: 23 October 2012
The Author(s) 2012. This article is published with open access at Springerlink.com
Abstract This report presents a rare case of intrahepatic
cholangiocarcinoma (IHCC) arising 28 years after excision
of a type IV-A congenital choledochal cyst. The patient
underwent excision of a congenital choledochal cyst
(Todanis type IV-A) at 12 years of age, with Roux-en-Y
hepaticojejunostomy reconstruction. She received a pan-
creaticoduodenectomy (PD) using the modied Child
method for an infection of a residual congenital chole-
dochal cyst in the pancreatic head at the age of 18. She was
referred to this department with a liver tumor 22 years
later. Left hemihepatectomy with left-side caudate lobec-
tomy was performed and the tumor was pathologically
diagnosed to be IHCC. The cause of the current carcino-
genesis was presumed to be reux of pancreatic juice into
the residual intrahepatic bile duct during surgery. This case
suggests that a careful long-term follow-up is important for
patients with congenital choledochal cysts, even if a sep-
aration-operation was performed at a young age, and
especially after PD.
Keywords Choledochal cyst Hepatectomy
Intrahepatic cholangiocarcinoma
Introduction
Intrahepatic cholangiocarcinoma (IHCC) is the second
most common primary liver cancer, and the incidence is
increasing [1]. There is a signicant association between
the presence of congenital choledochal cysts and the
development of hepatobiliary malignancies, including
IHCC. [27] The cause of carcinogenesis in these cases is
presumed to be the reux of pancreatic juice into the bile
duct and the accumulation of mixed bile in the biliary
system caused by an anomalous junction of the pancreati-
cobiliary duct.
The recommended standard surgical treatment is the
excision of the dilated extrahepatic bile duct, with a
hepaticoenterostomy to stop the reux of pancreatic juice.
This is called a separation-operation. However, some
patients develop biliary cancer long after a separation-
operation. The development of intrahepatic cholangiocar-
cinoma after pancreaticoduodenectomy has not previously
been reported in patients with congenital biliary dilation,
however, this report presents a case of intrahepatic chol-
angiocarcinoma arising 28 years after the initial separa-
tion-operation for a Todanis type IV-A congenital
choledochal cyst, and 22 years after pancreaticoduoden-
ectomy for infection of a residual congenital choledochal
cyst in the pancreatic head.
Case report
A 40-year-old female was referred to this department for
further examination of a liver tumor. She had undergone
excision of a congenital choledochal cyst (Todanis type
IV-A) at 12 years of age, with Roux-en-Y hepaticojejun-
ostomy reconstruction (Fig. 1a). She underwent a
T. Kumamoto (&) K. Tanaka K. Takeda K. Nojiri
R. Mori K. Taniguchi R. Matsuyama M. Ueda M. Sugita
Y. Ichikawa Y. Nagashima I. Endo
Department of Gastroenterological Surgery, Yokohama City
University Graduate School of Medicine, Yokohama, Japan
e-mail: t.kumamoto@k5.dion.ne.jp
T. Kumamoto K. Tanaka K. Takeda K. Nojiri R. Mori
K. Taniguchi R. Matsuyama M. Ueda M. Sugita
Y. Ichikawa Y. Nagashima I. Endo
Department of Molecular Pathology, Yokohama City University
Graduate School of Medicine, 39 Fukuura Kanazawa-ku,
Yokohama 236-0004, Japan
1 3
Surg Today (2014) 44:354358
DOI 10.1007/s00595-012-0387-2
pancreaticoduodenectomy (PD) at the age of 18, using the
modied Child method to treat an infection of a residual
congenital choledochal cyst in the pancreatic head
(Fig. 1b). The patient had been well with no symptoms
since her last operation, so she had not undergone regular
follow-up during the 18 years since her second operation.
She was diagnosed with a chronic hepatitis C virus
(HCV) infection during a medical checkup at the age of 37,
and was referred to our hospital for treatment. She had
received interferon and ribavirin therapy and nally
obtained a sustained viral response, after which she
underwent regular follow-up. Follow-up-dynamic abdom-
inal computed tomography (CT) revealed a low-density
tumor o the left medial section (Fig. 2a) at the age of 40.
Serum carcinoembryonic antigen (CEA) and DUPAN-2
levels were elevated to 6.3 ng/ml and 360 U/ml, respec-
tively. Positron emission tomography-CT (PET-CT)
revealed the maximum standardized uptake value (SUV-
max) of the liver tumor to be 9.3, with no signs of lymph
node metastasis, intraperitoneal dissemination, or hepatic
metastasis. 3D-drip infusion cholangiography-CT (3D-
DIC-CT) revealed dilation of the right and left hepatic
ducts of up to 20 mm and tumor invasion of the B2 ? 3
bile duct; the hepaticojejunostomy was not affected by the
tumor (Fig. 2b). The tumor was diagnosed to be IHCC.
She underwent a left hemihepatectomy with left-sided
caudate lobectomy, preserving the hepaticojejunostomy
that had been established in the previous operation. Intra-
operative frozen sections of the cut end of the left hepatic
duct and lymph node of the hilar lesion revealed no
metastasis. Amylase levels in the bile juice of the left
hepatic duct were 7621 U/L, and bile juice culture detected
the presence of Enterococcus faecalis.
The cut surface of the tumor was 32 mm in diameter,
hard and whitish; the margin was somewhat lobulated and
the tumor had invaded the bile duct of the lateral segment
(Fig. 3a). The tumor contained atypical cells with nuclei
with enriched chromatin and showed morphological vari-
ety. The atypical cells had a poorly glandular arrangement
(Fig. 3b).
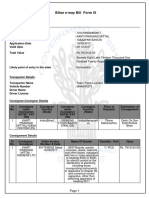
Fig. 1 Schematic illustration of the reconstruction. a Excision of the
extrahepatic dilated bile duct with Roux-en-Y hepaticojejunostomy
reconstruction separated the bile from the pancreatic juice ow.
Arrow with the broken line shows the ow of the pancreatic juice.
b Pancreaticoduodenectomy (PD) using a modied Child method was
performed for infection of residual congenital choledochal cyst in
pancreatic head. Arrow with the broken line shows the ow of
pancreatic juice that could enter the intrahepatic bile duct. c Pancre-
aticogastrostomy after PD. Arrow with the broken line shows the ow
of pancreatic juice, which is less likely to move backward to the bile
duct
Fig. 2 Enhanced abdominal computed tomography and three dimen-
sional-drip infusion cholangiography-computed tomography. a
Arrows show a low-density tumor, 32 mm in diameter, in the lateral
section of the liver. Arrow heads shows a dilated intrahepatic bile
duct. b 3D-DIC-CT revealed dilation of the right and left hepatic
ducts to 20 mm, and tumor invasion of the B2 ? 3 bile duct but not
the hepaticojejunostomy
Surg Today (2014) 44:354358 355
1 3
The patient received postoperative adjuvant systemic
chemotherapy with gemcitabine. There was no recurrence
10 months after surgery.
Discussion
The development of biliary cancer is a major complication
in patients with congenital choledochal cysts, with an
incidence of hepatobiliary malignancies associated with
congenital choledochal cysts ranging from 2.5 to 28 %
[27]. Although the mechanism of carcinogenesis has not
been fully elucidated, it is reported that the carcinogenetic
process is caused by repeated damage and restoration of the
biliary epithelium by a mutual countercurrent of pancreatic
and bile juice. The regenerated epithelium gradually pro-
duces a variant accompanied by cellular atypical changes,
as well as mutations of the K-ras and p53 genes [8]. These
processes may lead to mucosal metaplasia and biliary tract
malignancy.
Excision of the entire extrahepatic bile duct and hepat-
icoenterostomy are recommended to prevent the develop-
ment of biliary carcinoma, because it separates bile from
pancreatic juice ow. However, some patients develop
intrahepatic cholangiocarcinoma long after the separation-
operation. Kobayashi et al. [8]. reported biliary tract cancer
before and after separation-operations for patients with
congenital biliary dilation, and concluded that the relative
risk in the post-surgery group was still higher than in the
general population, although it was decreased by approxi-
mately 50 % after the separation-operation. This suggests
that the epithelium of the remnant bile duct wall may have
already progressed to a precancerous stage by the time of
surgery, and that genetic changes may have taken place or
continued during the postoperative period. Furthermore, all
patients in this previous study that developed bile duct
carcinoma after surgery had a Todanis type IV-A dilation,
characterized by narrowing of the peripheral bile duct and a
dilated pathologic bile duct. [9] A complete resection of a
dilated pathologic intrahepatic bile duct is not a straight-
forward procedure, and thus the risk of developing cancer
remains high. This was also true in the current case, in
which the patient was diagnosed with Todanis type IV-A
dilation and the residual dilated intrahepatic duct was
detected by 3D-DIC-CT.
Patients who undergo biliary-enteric anastomosis are
thought to be at risk for developing IHCC after surgery for
benign disease, as the reux of activated pancreatic juice
and bacterial contamination can cause chronic inamma-
tion and carcinogenic processes. Tocchi et al. [10] reported
that the incidence of cholangiocarcinomas after choledo-
choduodenostomy or hepaticojejunostomy for benign dis-
ease is 7.6 and 1.9 %, respectively, and this signicant
difference occurs because the activated pancreatic juice can
more easily ow back to the biliary tract in a choledo-
choduodenostomy. Therefore, the reux of activated pan-
creatic juice might be the strongest carcinogenic factor.
Re-exposure to pancreatic juice may have been one of
the causes of cancer in the current case. The residual
dilated intrahepatic bile duct appeared to have been stim-
ulated by a mutual countercurrent of pancreatic and bile
juice and by intestinal bacteria, because E. faecalis was
detected in a culture of the bile juice and amylase levels
were 7621 U/L in the bile juice of the left hepatic duct.
Therefore, pancreaticogastrostomy is recommended for
patients with congenital choledochal cysts after PD,
because it is more difcult for pancreatic juice to ow
backward to the bile duct during this procedure (Fig. 1 c).
Re-anastomosis of the hepaticojejunostomy using another
Roux-en-Y to prevent pancreatic juice from owing
Fig. 3 Gross ndings of the excised specimen and histopathological
ndings. a Arrow shows the tumor and the arrow head shows the
dilated intrahepatic bileduct.The cut surface of the tumor was 32 mm
in diameter, hard and whitish; the margin wassomewhat lobulated and
the tumor had invaded the B2 ? 3 bile duct. b The tumor
wascomposed of solid cell nests with occasional glandular spaces.
Tumor nuclei werevesicular with coarse chromatin, small nuclei and
eosinophilic cytoplasm
356 Surg Today (2014) 44:354358
1 3
backward to residual dilated right hepatic duct during
resection of the IHCC was planned in the current case,
because the patient was relatively young. However, the
adhesion of the hepatic hilum and jejunum was strong and
there was a risk of damage to the right hepatic artery.
Therefore, only a left hemihepatectomy with left-sided cau-
date lobectomy was performed, preserving the hepaticojej-
unostomythat hadbeenestablishedinthe previous operation.
Infection with hepatitis B virus or HCV is suggested to
be involved in the pathogenesis of IHCC. A large cohort
study revealed that HCV infection conferred a more than
two fold elevated risk of developing IHCC, [11] while
Yamamoto et al. [12] reported that nodular IHCC appears
to be related to hepatitis viral infection and could be
detected at an early stage by following up cases of chronic
hepatitis and cirrhosis. The current patient had not under-
gone regular follow-up for 18 years after her second
operation. However, she underwent periodic medical
check-ups after being diagnosed with chronic HCV infec-
tion that allowed IHCC to be detected early and a poten-
tially curative operation to be performed.
An extensive literature search revealed ten reports
describing IHCC arising after surgery for a congenital
choledochal cyst (Table 1). The 11 patients, including the
current case, included ve males, ve females and one case
of unknown gender, ranging in age from 16 to 66 years.
The mean period between the primary operation and the
development of cancer was 15.3 years (234 years) and the
type of dilation was Todanis type IV-A in eight patients
and type I in one patient. The IHCC was resected suc-
cessfully in only four of these patients, three had an
unresectable advanced tumor and one had a resectable
tumor that was inoperable due to poor liver function. A
periodic medical check-up is important for detecting the
tumor at an early stage; since cholangiocarcinoma is not
characterized by distinct clinical symptoms until its
advanced late stages.
This report presented a case of intrahepatic cholangio-
carcinoma arising 28 years after the initial operation of
excision of a Todanis type IV-A congenital chole-
dochal cyst with reconstruction by Roux-en-Y hepati-
cojejunostomy. The patient had multiple possible risk
factors for developing IHCC, including remaining IV-A
congenital biliary dilation, subsequent modied Child PD
that induced re-exposure of pancreatic juice, and chronic
HCV infection. Careful long-term follow-up is therefore
recommended for high risk patients even after separation-
operation.
Conict of Interest The authors have no conict of interest.
Open Access This article is distributed under the terms of the
Creative Commons Attribution License which permits any use, dis-
tribution, and reproduction in any medium, provided the original
author(s) and the source are credited.
References
1. Yamamoto M, Ariizumi S. Surgical outcomes of intrahepatic
cholangiocarcinoma. Surg Today. 2011;41:896902.
2. Nagorney DM, McIlrath DC, Adson MA. Choledochal cysts in
adults: clinical management. Surgery. 1984;96:65663.
3. Kagawa Y, Kashihara S, Kuramoto S, Maetani S. Carcinoma
arising in a congenitally dilated biliary tract: report of a case and
review of the literature. Gastroenterology. 1978;74:128694.
4. Todani T, Tabuchi K, Watanabe Y, Kobayashi Y, Kobayashi T.
Carcinoma arising in the wall of congenital bile duct cysts.
Cancer. 1979;44:113441.
5. Yamaguchi M. Congenital choledochal cysts: analysis of 1,433
patients in the Japanese literature. Am J Surg. 1980;140:6537.
6. Deaiel DJ, Rossi RL, Munson JL, Braasch JW, Silverman ML.
Management of bile duct cysts in adults. Arch Surg. 1986;121:
4105.
7. Todani T, Watanabe Y, Urushihara N, Morotomi Y, Maeba T.
Choledochal cyst, pancreatobiliary malunion, and cancer.
J Hepatobiliary Pancreat Surg. 1994;1:24751.
8. Kasuya K, Nagawaka Y, Matsudo T, Ozawa T, Tsuchida A. p53
gene mutation and p53 protein overexpression in a patient with
Table 1 Published cases
of intrahepatic
cholangiocarcinoma
arising several years after
surgery for a congenital
choledochal cyst
Case Sex Age (years) Todani tumor
type
Years after
surgery
Site of
carcinoma
Resectability First author
1 F 58 IV-A 7 Lt Unresected Gallagher [13]
2 F 38 IV-A 17 Unresected Chandhuri [14]
3 M 33 20 Rt Unresected Cohen [15]
4 IV-A 2 Rt Resected Scudamore [16]
5 M 29 IV-A 3 Bil Unresected Joseph [17]
6 F 18 IV-A 2.4 Lt Unresected Kobayashi [9]
7 F 52 I 10 A Resected Goto [18]
8 M 46 IV-A 26 M Unresected Suzuki [19]
9 M 44 IV-A 34 Lt Resected Shimamura [20]
10 M 66 20 Rt Unresected Matsuura [21]
11 F 40 IV-A 28 M Resected Present case
Surg Today (2014) 44:354358 357
1 3
simultaneous double cancer of the gallbladder and bile duct
associated with pancreaticobiliary maljunction. J Hepatobiliary
Pancreat Surg. 2009;16:37681.
9. Kobayashi S, Asano T, Yamasaki M, Kenmochi T, Nakagohri T.
Risk of bile duct carcinogenesis after excision of extrahepatic bile
ducts in pancreaticobiliary maljunction. Surgery. 1999;126:93944.
10. Tocchi A, Mazzoni G, Liotta G, Lepre L, Gassini D. Late
development of bile duct cancer in patients who had biliary-
enteric drainage for benign disease: a follow-up study of more
than 1,000 patients. Ann Surg. 2001;234:2104.
11. El-Serag HB, Engels EA, Landgern O, Chiao E, Henderson L,
Amaratunge HC, et al. Risk of hepatobiliary and pancreatic
cancers after hepatitis C virus infection: a population-based study
of U.S. veterans. Hepatology. 2009;49:11623.
12. Yamamoto M, Takasaki K, Nakano M, Saito A. A minute nodular
intrahepatic cholangiocarcinoma. Cancer. 1998;82:21459.
13. Gallagher PJ, Millis RR, Mitchinson MJ. Congenital dilatation of
the intrahepatic bile ducts with cholangiocarcinoma. J Clin
Pathol. 1972;25:8048.
14. Chaudhuri PK, Chaudhuri B, Schuler JJ, Nyhus LM. Carcinoma
associated with congenital cystic dilation of bile ducts. Arch
Surg. 1982;117:134951.
15. Cohen GP, ODonnell C. Malignant change within surgically
drained choledochal cysts. Australas Radiol. 1992;36:21921.
16. Scudamore CH, Hemming AW, Teare JP, Fache JS, Erb SR. Sur-
gical management of choledochal cysts. Am J Surg. 1994;167:
497500.
17. Joseph VT. Surgical techniques and long-term results in the
treatment of choledochal cyst. J Pediatr Surg. 1990;25:7827.
18. Goto N, Yasuda I, Uematsu T, Kanemura N, Takai S. Intrahepatic
cholangiocarcinoma arising 10 years after the excision of congenital
extrahepatic biliary dilation. J Gastroenterol. 2001;36:85662.
19. Suzuki S, Amano K, Harada N, Tanaka S, Hayashi T, Suzuki M,
et al. A case of intrahepatic cholangiocarcinoma arising 26 years
after excision of congenital biliary dilation (in Japanese with
English abstract). Jpn J Gastroenterol Surg. 1988;207:1427.
20. Shimamura K, Kurosaki I, Sato D, Takana K, Yokoyama N, Sato
Y, et al. Intrahepatic cholangiocarcinoma arising 34 years after
excision of a type IV-A congenital choledochal cyst: report of a
case. Surg Today. 2009;39:24751.
21. Matsuura H, Inui K, Wakabayashi T, Okushima K, Miyoshi H,
Nakamura Y, et al. A cholangiocarcinoma detected while treating
intrahepatic stones 20 years after operative biliary diversion for
congenital dilatation of the bile duct. JJBA. 2009;23:2016.
358 Surg Today (2014) 44:354358
1 3
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- HivDocument53 pagesHivReZa FriscaNo ratings yet
- SrableDocument39 pagesSrableYatza Sanches SanchesNo ratings yet
- EndokrinDocument5 pagesEndokrinReZa FriscaNo ratings yet
- Setting Gprs-Mms All Operator Di Handphone Data Account: Account Name APN User Name Password Authentic TypeDocument4 pagesSetting Gprs-Mms All Operator Di Handphone Data Account: Account Name APN User Name Password Authentic TypeReZa FriscaNo ratings yet
- Hydatid Cyst Within A Choledochal CystDocument4 pagesHydatid Cyst Within A Choledochal CystReZa FriscaNo ratings yet
- Recomend Ac I OnesDocument14 pagesRecomend Ac I OnesReZa FriscaNo ratings yet
- Choledochal Cysts - A Review of LiteratureDocument14 pagesCholedochal Cysts - A Review of LiteratureReZa FriscaNo ratings yet
- 821032Document5 pages821032ReZa FriscaNo ratings yet
- Choledochal Cysts - A Review of LiteratureDocument14 pagesCholedochal Cysts - A Review of LiteratureReZa FriscaNo ratings yet
- Jkss 85 225Document5 pagesJkss 85 225ReZa FriscaNo ratings yet
- Analysis of Risk FactorsDocument6 pagesAnalysis of Risk FactorsReZa FriscaNo ratings yet
- ALERGYDocument6 pagesALERGYReZa FriscaNo ratings yet
- Analysis of Risk FactorsDocument6 pagesAnalysis of Risk FactorsReZa FriscaNo ratings yet
- ALERGYDocument6 pagesALERGYReZa FriscaNo ratings yet
- NODocument5 pagesNOReZa FriscaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Single Door Feeder Pillar 200A MCCBDocument1 pageSingle Door Feeder Pillar 200A MCCBMiqdad AliNo ratings yet
- Raspberry Pi 3 and BeagleBone Black For Engineers - UpSkill Learning 124Document124 pagesRaspberry Pi 3 and BeagleBone Black For Engineers - UpSkill Learning 124Dragan IvanovNo ratings yet
- Manual 35S EnglishDocument41 pagesManual 35S EnglishgugiNo ratings yet
- Full Download Short Term Financial Management 3rd Edition Maness Test BankDocument35 pagesFull Download Short Term Financial Management 3rd Edition Maness Test Bankcimanfavoriw100% (31)
- Antoine Constants PDFDocument3 pagesAntoine Constants PDFsofiaNo ratings yet
- (Eng) Zx890lch 5a Ks En316Document13 pages(Eng) Zx890lch 5a Ks En316MC TAK LEENo ratings yet
- Chennai To Vishakhapatnam El6Vvd: Indigo 6E-6835Document3 pagesChennai To Vishakhapatnam El6Vvd: Indigo 6E-6835VENKATESH POONDRUNo ratings yet
- Ecotopia Remixed II-FormattedDocument54 pagesEcotopia Remixed II-FormattedthisisdarrenNo ratings yet
- Class 12 Maths Project On Prime NumbersDocument13 pagesClass 12 Maths Project On Prime Numbersanon_3835245630% (1)
- Moses ManualDocument455 pagesMoses ManualDadypeesNo ratings yet
- Active Faults in MalaysiaDocument52 pagesActive Faults in MalaysiaHazim HaNo ratings yet
- Smoldering Combustion: Guillermo ReinDocument20 pagesSmoldering Combustion: Guillermo ReinAhmed HussainNo ratings yet
- #Dr. Lora Ecg PDFDocument53 pages#Dr. Lora Ecg PDFمحمد زينNo ratings yet
- Banachek UnlimitedDocument34 pagesBanachek UnlimitedserenaNo ratings yet
- Earth Sciences Notes Csir-Ugc Net JRFDocument57 pagesEarth Sciences Notes Csir-Ugc Net JRFmanas773No ratings yet
- Stanley B. Alpern - Amazons of Black Sparta - The Women Warriors of Dahomey-New York University Press (2011)Document308 pagesStanley B. Alpern - Amazons of Black Sparta - The Women Warriors of Dahomey-New York University Press (2011)georgemultiplusNo ratings yet
- 3161 GIS Data ModelsDocument13 pages3161 GIS Data Modelsapi-3788255No ratings yet
- L GH Catalog PullingDocument60 pagesL GH Catalog PullingLuis LuperdiNo ratings yet
- Product Stock Exchange Learn BookDocument1 pageProduct Stock Exchange Learn BookSujit MauryaNo ratings yet
- The Unofficial Aterlife GuideDocument33 pagesThe Unofficial Aterlife GuideIsrael Teixeira de AndradeNo ratings yet
- Texto CuritibaDocument1 pageTexto CuritibaMargarida GuimaraesNo ratings yet
- Engineering Structures: C.X. Dong, A.K.H. Kwan, J.C.M. HoDocument14 pagesEngineering Structures: C.X. Dong, A.K.H. Kwan, J.C.M. HoElieser SinagaNo ratings yet
- ZhentarimDocument4 pagesZhentarimLeonartNo ratings yet
- Maths All FormulasDocument5 pagesMaths All FormulasVishnuNo ratings yet
- Sample Dilapidation ReportDocument8 pagesSample Dilapidation ReportczarusNo ratings yet
- LJ-V7080 DatasheetDocument2 pagesLJ-V7080 DatasheetOrhan DenizliNo ratings yet
- Angewandte: ChemieDocument13 pagesAngewandte: ChemiemilicaNo ratings yet
- Project Title Discipline Project Stage Client Attendance CirculationDocument4 pagesProject Title Discipline Project Stage Client Attendance CirculationgregNo ratings yet
- Chapter 04 Product and ServDocument43 pagesChapter 04 Product and ServAlireza AlborziNo ratings yet
- Pre RmoDocument4 pagesPre RmoSangeeta Mishra100% (1)