Professional Documents
Culture Documents
Pasien Dengan Peritonitis
Uploaded by
Cindy Prayogo0 ratings0% found this document useful (0 votes)
20 views5 pagesnb,mn
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentnb,mn
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
20 views5 pagesPasien Dengan Peritonitis
Uploaded by
Cindy Prayogonb,mn
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
Pasien dengan peritonitis, rentan mengalam shock septic.
Shock septic merupakan shock
maldistributif. Patogenesisnya meliputi interaksi kompleks antara vasodilatasi pembuluh
darah patologis, disfungsi myocardial, dan gangguan distribusi aliran darah karena respon
inflamasi terhadap infeksi. Serangkaian abnormalitas tersebut menyebabkan kelainan
patofisiologis yang menyebabkan hipotensi, hipoperfusi, dan disfungsi organ.
Terapi penanganan hemodinamik mencakup: resusitasi cairan, terapi vasopressor, terapi
inotropic.
Resusitasi cairan
Peradangan yang menyeluruh pada membran peritoneum menyebabkan perpindahan
cairan ekstraseluler ke dalam kavum peritoneum dan ruang intersisial.
6
Pengembalian volume dalam jumlah yang cukup besar melalui intravaskular sangat
diperlukan untuk menjaga produksi urin tetap baik dan status hemodinamik tubuh. Jika
terdapat anemia dan terdapat penurunan dari hematokrit dapat diberikan transfusi PRC
(Packed Red Cells) atau WB (Whole Blood). Larutan kristaloid dan koloid harus
diberikan untuk mengganti cairan yang hilang.
7
Secara teori, cairan koloid lebih efektif untuk mengatasi kehilangan cairan intravaskuler,
tapi cairan ini lebih mahal. Sedangkan cairan kristaloid lebih murah, mudah didapat tetapi
membutuhkan jumlah yang lebih besar karena kemudian akan dikeluarkan lewat ginjal.
8
Suplemen kalium sebaiknya tidak diberikan hingga perfusi dari jaringan dan ginjal telah
adekuat dan urin telah diproduksi.
7
Berdasarkan Surviving Sepsis Campaign guidelines, selama 6 jam pertama
resusitasi, goal yang harus dicapai adalah:
Central Venous Pressure 8-12 mmHg
Mean arterial pressure (MAP) >65 mm Hg
Urine output >0.5 mL/kg/hr
Central venous (superior vena cava) or mixed venous oxygen saturation >70%
or >65%, respectively
Rekomendasi dari Surviving Sepsis Campaign, dilakukan pemberian cairan
kristaloid > = 1000 mL of crystalloids atau koloid 300-500 mL selama 30 menit.
Ketika pemberian cairan gagal memperbaiki keadaan hipoperfusi pasien, terapi
vasopressor segera diberikan.
Terapi vasopressor
Obat-obatan vasopressor menjaga tekanan darah yang adekuat dan menjaga tekanan
perfusi untuk memaksimalkan aliran darah ke organ-organ tubuh. Baik
norepinephrine dan dopamine merupakan agen vasopressor untuk menangani
hipotensi pada shock septik. Norepinephrine dan dopamine dapat Both
norepinephrine and dopamine can increase blood pressure in shock states, although
norepinephrine seems to be more powerful. Dopamine may be useful in patients with
compromised cardiac function and cardiac reserve [12], but norepinephrine is more
effective than dopamine in reversing hypotension in patients with septic shock.
Dopamine has also potentially detrimental effects on the release of pituitary
hormones and especially prolactin, although the clinical relevance of these effects is
still unclear and can have unintended effects such as tachyarrhythmias.
Dopamine has different effects based on the doses [13].
A dose of less than 5 g/kg/min results in vasodilation of renal, mesenteric, and
coronary districts. At a dose of 5-10 g/kg/min, beta-1-adrenergic effects increase
cardiac contractility and heart rate. At doses about 10 g/kg/min, alpha-adrenergic
effects lead to arterial vasoconstriction and increase blood pressure. Its major side
effects are tachycardia and arrhythmogenesis.
The use of renal-dose dopamine in sepsis is a controversial issue. In the past, low-
dose dopamine was routinely used because of the possible renal protective effects.
Dopamine at a dose of 2-3 g/kg/min was known to stimulate diuresis by increasing
renal blood flow.
A multicentre, randomised, double-blind, placebo-controlled study about low-dose
dopamine in patients with at least two criteria for the systemic inflammatory
response syndrome and clinical evidence of early renal dysfunction (oliguria or
increase in serum creatinine concentration), was published on 2000 [14]. Patients
admitted were randomly assigned a continuous intravenous infusion of low-dose
dopamine (2 g/kg/min) or placebo administered through a central venous catheter.
Administration of low-dose dopamine by continuous intravenous infusion to
critically ill patients at risk of renal failure did not confer clinically significant
protection from renal dysfunction.
A meta-analysis of literature from 1966 to 2000 for studies addressing the use of
dopamine in the prevention and/or treatment of renal dysfunction was published on
2001 [15]. The Authors concluded that the use of low-dose dopamine for the
treatment or prevention of acute renal failure was not justified on the basis of
available evidence.
Norepinephrine is a potent alpha-adrenergic agonist with
Terapi inotropic
Patients with severe sepsis and septic shock may present ineffective perfusion. Poor tissues
perfusion may cause a global tissue hypoxia, often associated to an elevated serum lactate
level. A serum lactate value greater than 4 mmol/L (36 mg/dL) is correlated with poorer
outcomes, even if hypotension is not yet present. Fluid resuscitation should be started as
early as possible.
Vasopressor drugs maintain adequate blood pressure and preserve perfusion pressure for
optimizing flow in various organs.
Both norepinephrine and dopamine are the first-line vasopressor agents to correct
hypotension in septic shock. Both norepinephrine and dopamine can increase blood
pressure in shock states, although norepinephrine seems to be more powerful. Dopamine
may be useful in patients with compromised cardiac function and cardiac reserve [12], but
norepinephrine is more effective than dopamine in reversing hypotension in patients with
septic shock. Dopamine has also potentially detrimental effects on the release of pituitary
hormones and especially prolactin, although the clinical relevance of these effects is still
unclear and can have unintended effects such as tachyarrhythmias.
Dopamine has different effects based on the doses [13].
A dose of less than 5 g/kg/min results in vasodilation of renal, mesenteric, and coronary
districts. At a dose of 5-10 g/kg/min, beta-1-adrenergic effects increase cardiac
contractility and heart rate. At doses about 10 g/kg/min, alpha-adrenergic effects lead to
arterial vasoconstriction and increase blood pressure. Its major side effects are tachycardia
and arrhythmogenesis.
The use of renal-dose dopamine in sepsis is a controversial issue. In the past, low-dose
dopamine was routinely used because of the possible renal protective effects. Dopamine at a
dose of 2-3 g/kg/min was known to stimulate diuresis by increasing renal blood flow.
A multicentre, randomised, double-blind, placebo-controlled study about low-dose
dopamine in patients with at least two criteria for the systemic inflammatory response
syndrome and clinical evidence of early renal dysfunction (oliguria or increase in serum
creatinine concentration), was published on 2000 [14]. Patients admitted were randomly
assigned a continuous intravenous infusion of low-dose dopamine (2 g/kg/min) or placebo
administered through a central venous catheter. Administration of low-dose dopamine by
continuous intravenous infusion to critically ill patients at risk of renal failure did not confer
clinically significant protection from renal dysfunction.
A meta-analysis of literature from 1966 to 2000 for studies addressing the use of dopamine
in the prevention and/or treatment of renal dysfunction was published on 2001 [15]. The
Authors concluded that the use of low-dose dopamine for the treatment or prevention of
acute renal failure was not justified on the basis of available evidence.
Norepinephrine is a potent alpha-adrenergic agonist with
You might also like
- Case NefroDocument5 pagesCase NefroCindy PrayogoNo ratings yet
- Jurnal ReadingDocument4 pagesJurnal ReadingCindy PrayogoNo ratings yet
- AU VU 6 Januari 2021Document6 pagesAU VU 6 Januari 2021Cindy PrayogoNo ratings yet
- Laporan KasusDocument24 pagesLaporan KasusCindy PrayogoNo ratings yet
- Case ReportDocument8 pagesCase ReportCindy PrayogoNo ratings yet
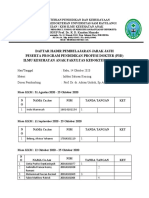
- Daftar Hadir Pembelajaran Jarak Jauh Peserta Program Pendidikan Profesi Dokter (P3D) Ilmu Kesehatan Anak Fakultas Kedokteran UnsratDocument13 pagesDaftar Hadir Pembelajaran Jarak Jauh Peserta Program Pendidikan Profesi Dokter (P3D) Ilmu Kesehatan Anak Fakultas Kedokteran UnsratCindy PrayogoNo ratings yet
- Refereat OktDocument6 pagesRefereat OktCindy PrayogoNo ratings yet
- Daftar hadir pembelajaran jarak jauh P3D Ilmu Kesehatan Anak UNSRATDocument9 pagesDaftar hadir pembelajaran jarak jauh P3D Ilmu Kesehatan Anak UNSRATCindy PrayogoNo ratings yet
- Absen Divisi Nefrologi - RabuDocument4 pagesAbsen Divisi Nefrologi - RabuCindy PrayogoNo ratings yet
- AU VU 6 Januari 2021Document6 pagesAU VU 6 Januari 2021Cindy PrayogoNo ratings yet
- Daftar Hadir Pembelajaran Jarak Jauh Peserta Program Pendidikan Profesi Dokter (P3D) Ilmu Kesehatan Anak Fakultas Kedokteran UnsratDocument13 pagesDaftar Hadir Pembelajaran Jarak Jauh Peserta Program Pendidikan Profesi Dokter (P3D) Ilmu Kesehatan Anak Fakultas Kedokteran UnsratCindy PrayogoNo ratings yet
- Daftar Hadir Pembelajaran Jarak Jauh Peserta Program Pendidikan Profesi Dokter (P3D) Ilmu Kesehatan Anak Fakultas Kedokteran UnsratDocument13 pagesDaftar Hadir Pembelajaran Jarak Jauh Peserta Program Pendidikan Profesi Dokter (P3D) Ilmu Kesehatan Anak Fakultas Kedokteran UnsratCindy PrayogoNo ratings yet
- Absen Divisi Nefrologi - RabuDocument4 pagesAbsen Divisi Nefrologi - RabuCindy PrayogoNo ratings yet
- Ablatio RetinaDocument14 pagesAblatio RetinaCindy PrayogoNo ratings yet
- Dendam Si SolihinDocument8 pagesDendam Si SolihinCindy PrayogoNo ratings yet
- Konjungtivitis FliktenDocument24 pagesKonjungtivitis FliktencatharinamNo ratings yet
- Defense MechanismDocument40 pagesDefense MechanismCindy PrayogoNo ratings yet
- Absen Divisi Nefrologi - RabuDocument4 pagesAbsen Divisi Nefrologi - RabuCindy PrayogoNo ratings yet
- Preskas CindyDocument17 pagesPreskas CindyCindy PrayogoNo ratings yet
- Presentasi Kasus NeuroDocument24 pagesPresentasi Kasus NeuroCindy PrayogoNo ratings yet
- Preskas Ablasi RetinaDocument5 pagesPreskas Ablasi RetinaCindy PrayogoNo ratings yet
- Solusio-Plasenta Nofilia - 07120090066Document21 pagesSolusio-Plasenta Nofilia - 07120090066Cindy PrayogoNo ratings yet
- Referat PsikoterapiDocument49 pagesReferat PsikoterapiCindy Prayogo100% (1)
- Presentasi Kasus NeuroDocument24 pagesPresentasi Kasus NeuroCindy PrayogoNo ratings yet
- Referat PreeklampsiaDocument24 pagesReferat PreeklampsiaCindy PrayogoNo ratings yet
- Preskas CindyDocument17 pagesPreskas CindyCindy PrayogoNo ratings yet
- Ujian CindyDocument28 pagesUjian CindyCindy PrayogoNo ratings yet
- Psikoterapi DasarDocument7 pagesPsikoterapi DasarAmrul HamdiNo ratings yet
- DCXDocument1 pageDCXCindy PrayogoNo ratings yet
- Cover Referat PSIKOTERAPIDocument1 pageCover Referat PSIKOTERAPICindy PrayogoNo ratings yet