Professional Documents
Culture Documents
Frontotemporal Dementia Talk
Uploaded by
kattbattOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Frontotemporal Dementia Talk
Uploaded by
kattbattCopyright:
Available Formats
Frontotemporal
Dementia (FTD)
Monica K. Crane, MD
Associate Director
Cole Neuroscience Center, UTMCK
Clinical Assistant Professor, Dept. of Medicine
Frontotemporal dementia
(FTD) Overview
Background and clinical definition
Prevalence
Anatomy
FTD clinical subtypes
Neuropathology and genetics of
Frontotemporal lobe dementia (FTLD)
Historical cases
FTD = a clinical neurodegenerative disease
affecting frontal & temporal lobes
Personality changes
Loss of socially
acceptable behavior &
emotions
Bizarre and compulsive
behaviors
Language dysfunction
Movement disorder
FTD International Research Criteria:
1. Early disinhibition
2. Early apathy, loss of
motivation
3. Loss of emotional recognition
4. Perseverative, compulsive,
ritualistic behavior
5. Hyperorality/ dietary changes
6. FTD neuropsychological profile
Either #7 or #8 one
symptom from #1-6
7. Frontal and/or
anterior temporal
atrophy; other radiologic
findings
8. Presence of a known
mutation
B. L. Miller, C. Ikonte, M. Ponton, et al. Neurology 1997;48;937
OR
Three of the following:
Dementia That's Neither
Alzheimer's Nor Easy
FDG-PET images of metabolic activity: healthy controls,
AD, and FTD. Scale red (high FDG uptake)-yellow-
green-blue (low FDG uptake).
Normal Alzheimer's FTD
Photo Credit: Dr. J anet Miller, Dr. Suzanna Lee, MGH/ Harvard, Radiology Rounds April 2006
Dement i a Pr eval enc e
(% of eac h t ype seen i n US)
FTD syndromes~10-15%
Alzheimers Disease (AD) ~ 50-70%
Vascular dementia ~ 5-10%
Dementia with Lewy Bodies & Parkinsons
disease dementia ~10%
Boxer AL, Miller BL. Alzheimer Dis Assoc Disord. 2005;19 S1:S3-6
FTD Prevalence
FTD: Alzheimers disease (AD) ratio is 1:1 in
those aged 45-65.
Ratnavalli et al, Neurology 2002.
FTD is more common that AD below age 60.
Knopman et al, Neurology 2004.
FTD spectrum comprises near 15% or more
of the total FTD dementia cases.
Boxer AL, Miller BL. Alzheimer Dis Assoc Disord. 2005.
Picks disease FTD
Picks is an autopsy finding only
so do not use this term. The
clinical disease is FTD.
In 1892, Dr. Pick reported a case of a
71 year-old man with focal atrophy
and aphasia, & concluded that
progressive brain atrophy can lead
to symptoms of local disturbance
through local accentuation of the
diffuse process.
Dr. Arnold Pick (1851-1924)
Prof. of Psychiatry, Prague
History of Psychiatry v. 1994, 539-547. GE Berrios , DM Girling. Classic Text No 20. Cambridge.
From: LM Shaw LM, Korecka M, Clark CM, Lee VMY, Troganowski. Biomarkers of neurodeneration for diagnosis and monitoring
therapeutics Nature Reviews Drug Discovery. 2007;6:295-303.
Frontotemporal lobar degeneration (FTLD) =
Neuropathology of clinical FTD
Picks is a small subset of FTLD
Heterogeneity of FTD
subtypes:
Anatomy and Clinical
presentation
What areas of the brain are
affected in FTD?
FTD damages 3 major networks:
Dorosolateral prefrontal cortex (DLPFC)
Anterior cingulate cortex (ACC)
Orbitofrontal cortex (OFC)
Areas affected in FTD versus AD
Hagmann P, Cammoun L, Gigandet X, Meuli R, Honey CJ , et al. Entorhinal cortex 2009
Clinical Presentation:
FTD Subtypes
Frontotemporal dementia subtypes
Behavior variant (bvFTD)
Semantic dementia (SD)
Progressive nonfluent aphasia (PNFA)
Progressive Supranuclear Palsy (PSP)
Corticobasal degeneration (CBD)
FTD with motor neuron disease (FTD-MND)
ALS/CTE (Chronic Traumatic Encephalopathy)
Boxer AL, Miller BL. Clinical features of frontotemporal dementia. Alzheimer Dis Assoc
Disord. 2005;19 S1:S3-6
Behavioral variant (bvFTD)
Approximately 60% of patients with any form
of FTD have bvFTD.
Figure 1. Coronal pathology
section showing asymmetric
right-sided atrophy (R
temporal cortices with
widening of the inferior horn
of the lateral ventral).
L
R
Clinical Features of bv-FTD
Gradual onset
Impaired judgment and
planning
Apathy
Impaired insight
(anosognosia)
Loss of empathy and
emotion recognition
(alexithymia)
Disinhibition
Abnormal eating
behavior
Stereotypical or
ritualistic behavior
Personal neglect
Profanity use during letter fluency tasks can
differentiate FTD from AD. Ringman J M et al. Cogn Behav Neurol
2010;23:159-64
Clinical Features FTD AD
Age of onset Rarely >75 Increases w age
Behavior & Social
problems
Early disinhibition, +
socially inappropriate
Moderate-severe,
increases with severity
Language Isolated language
problem
Language + memory
Visuospatial deficit
Rare in mild-moderate Common
Motor signs Common Unusual
Mood Alexithymia, withdrawal,
verbal irritability, labile
Sadness, anhedonia
Psychotic features Somatic, religious,
bizarre delusions
Delusions increase with
disease severity
Appetite/
hunger/diet
Overeating, weight ;
carbohydrate craving
Weight loss, anorexia;
misses meals
Muangpaisan W. Geriat Aging. 2007; McKhann MG et al. Arch Neurol 2001; Muangpaisan W et al.
Neuro J Thai 2003
>50% of FTD subtypes misdiagnosed as
primary psychiatric disease
Figure. % of patients initially misdiagnosed prior to ND diagnosis
Woolley et al. J Clin Psychiatry. 201; 72(2): 126133.
Dougherty J D et al.
The computerized
self test (CST): an
interactive, internet
accessible cognitive
screening test for
dementia. J
Alzheimer's Dis 2010
Apr;20:185-95.
Crane MK et al.
Distinguishing
Frontotemporal
dementia from
Alzheimers disease:
A pilot study
employing the
Computer Self-Test
(CST). Dementia
Geriatr Cogn Disord
2010;30:62.
Computer Self-Test (CST)
as a diagnostic tool
CST Cognitive pattern differentiates AD from FTD
Crane, MK et al.Neurology. 2011 Suppl(March) 76;
VIDEO example of bvFTD
alexithymia
VIDEO example of a
bvFTD patient with a
palmar grasp reflex
Frontotemporal dementia subtypes
Behavior variant (bvFTD)
Semantic dementia (SD)
Progressive nonfluent aphasia (PNFA)
Progressive Supranuclear Palsy (PSP)
Corticobasal degeneration (CBD)
FTD with motor neuron disease (FTD-MND)
ALS/CTE (Chronic Traumatic Encephalopathy)
Boxer AL, Miller BL. Alzheimer Dis Assoc Disord. 2005;19 S1:S3-6
Semantic dementia (SD) or temporal variant
LEFT predominance
Language features: fluent speech
but loss of semantics (word choice)
Reading declines, numbers intact
RIGHT predominance
Severe deficits in
understanding emotions;
loss of empathy
Difficulty recognizing
faces and facial expression
Eventually R-sided
disease progresses to L
with language features,
and visa versa
SD patients develop
bvFTD behaviors
VIDEO example of
semantic deficits
VIDEO example of bvFTD
with phonetic fluency
deficits
Frontotemporal dementia subtypes
Behavior variant (bvFTD)
Semantic dementia (SD)
Progressive nonfluent aphasia
(PNFA)
Progressive Supranuclear Palsy (PSP)
Corticobasal degeneration (CBD)
FTD with motor neuron disease (FTD-MND)
ALS/CTE (Chronic Traumatic Encephalopathy)
Boxer AL, Miller BL. Alzheimer Dis Assoc Disord. 2005;19 S1:S3-6
Progressive nonfluent
aphasia (PNFA)
20% of FTD cases
Hesitant, effortful speech;
stutter or return of
childhood stutter
Anomia, agrammatism,
sound errors (gat for cat)
Eventually develop severe
movement disorder that
overlaps with PSP and
CBD
Marcel Ravel, (1875-1937)
French composer.
- in the early stages of
PNFA/FTD when
composing the orchestral
work Bolro (1928).
Progressive nonfluent aphasia (PNFA)
Fig. Coronal T1 weighted MRI of mild and moderate PNFA
Case 1: mild PNFA, atrophy of temporal lobe & pars triangularis.
Case 2: moderate PNFA, global atrophy with L-sided and
perisylvian predominance.
Case 1 Case 2
Frontotemporal dementia subtypes
Behavior variant (bvFTD)
Semantic dementia (SD)
Progressive nonfluent aphasia (PNFA)
Progressive Supranuclear Palsy (PSP)
Corticobasal degeneration (CBD)
FTD with motor neuron disease (FTD-MND)
ALS/CTE (Chronic Traumatic Encephalopathy)
Boxer AL, Miller BL. Alzheimer Dis Assoc Disord. 2005;19 S1:S3-6
Progressive supranuclear palsy (PSP)
Progressive supranuclear palsy
Deterioration of cells in the brainstem,
frontal cortex and basal ganglia
Dudley Moore 1935-2002
Progressive
supranuclear
palsy (PSP)
key features
Postural instability and falls within first year of diagnosis
Vertical supranuclear opthalmoparesis
Upward gaze paresis with abnormal saccadic eye
movements
Axial rigidity
Cognitive decline
Early stage difficult to distinguish from multiple system atrophy,
Parkinson disease, and small vessel diease.
Most patients with PNFA have PSP or CBD postmortem
PSP radiologic features
Hypometabolism on FDG-PET in basal ganglia, brainstem,
and frontal lobes
Midbrain
atrophy in
PSP
(A) Normal:
convex upper
border of the
midbrain
(B) Severe
atrophy of the
midbrain with
(C) concave
upper border of
midbrain
humming bird
sign.
C
A
B
Frontotemporal dementia subtypes
Behavior variant (bvFTD)
Semantic dementia (SD)
Progressive nonfluent aphasia (PNFA)
Progressive Supranuclear Palsy (PSP)
Corticobasal degeneration (CBD)
FTD with motor neuron disease (FTD-MND)
ALS/CTE (Chronic Traumatic Encephalopathy)
Boxer AL, Miller BL. Alzheimer Dis Assoc Disord. 2005;19 S1:S3-6
Corticobasal Degeneration (CBD) criteria
Core Features
Cortical dysfunction
Asymmetric ideomotor apraxia
Alien limb phenomenon
Visual or sensory hemineglect
Focal or asymmetric myoclonus
Non-fluent aphasia (overlap with
PNFA)
Extrapyramidal dysfunction
Asymmetric rigidity lacking
sustained levodopa response,
and focal dystonia
Supportive Features
Lateralized cognitive
dysfunction with
preserved memory
and learning
MRI with asymmetric
atrophy in parietal
and frontal cortex
FDG-PET decreased
glucose uptake in
parietal and frontal
cortex, basal ganglia
and thalamus.
Figure. CBD. Pt1: Mild, focal atrophy of corpus callosum with mild
hypometabolism in L frontoparietal cortex (arrow). Pt2: Moderate atrophy of
corpus callosum, moderate hypometabolism in L frontoparietal cortex (arrows)
Pt3: Severe, diffuse atrophy with bilateral hypometabolism accentuated in the
right frontoparietal cortex (arrows)
Frontotemporal dementia subtypes
Behavior variant (bvFTD)
Semantic dementia (SD)
Progressive nonfluent aphasia (PNFA)
Progressive Supranuclear Palsy (PSP)
Corticobasal degeneration (CBD)
FTD with motor neuron disease
(FTD-MND)
ALS/CTE (Chronic Traumatic Encephalopathy
Elevated levels of the TDP-43 protein have been found in CTE, a
also been identified in patients with CTE, a condition that often
mimics ALS and that has been associated with athletes who have
experienced multiple concussions and head injury.
FTD with motor neuron disease
(FTD-MND)
FTD-MND is a CLINICAL PHENOTYPE:
15% of FTD patients also have FTD-MND
FTD-MND co-occurs in patients with bvFTD but rare in
PNFA, CBD, PSP
Early cognitive and behavioral changes with MND symptoms:
slurring of speech, difficulty swallowing, choking
Autonomic dysfunction
limb weakness or muscle wasting
Patients live 1.4 years after diagnosis (respiratory
complications of bulbar symptoms as cause of death)
Most common MND is amyotrophic lateral sclerosis (ALS);
older ALS patients may also have behavioral or cognitive
problems similar to those seen in FTD (FTD-ALS syndrome)
Results of MRI voxel-based morphometry analyses: behavior
& language dominant FTD-MND analysis compared to control
Coon E et al. Neurology 2011;76:1886-1892
Both with frontotemporal gray matter loss. Behavioral variant
FTD-MND in frontal lobes. Language variant FTD-MND in
L lateral inferior temporal lobe and R putamen.
Neuropathology
and Genetics
FTD inheritance
Genetic (40%)
Approximately 20-50% of
FTD patients have an
affected 1
st
degree relative.
Familial FTD is suspected
when 2+ family members are
affected in 2+ generations.
Among individuals with FTD,
approximately 10% have a
single gene mutation
(autosomal dominant
inheritance).
Sporadic (60%)
50-80% of individuals
appear to be the first
person with FTD in the
family, also called
sporadic or nonfamilial
FTD (family not at risk).
Frontotemporal Lobar Degeneration (FTLD) is
the pathologic confirmation of clinical FTD
FTLDs are histopathologic
diagnosis with neuronal
loss & gliosis, spongiosis
& ballooned neurons
(image below).
Abnormal protein inclusions
in neurons & glial cells.
Tauopathies: FTLD with
tau+ inclusions
TDP-43 proteinopathies:
FTLD with tau-, alpha-
synuclein- inclusions
which contain the protein
TDP-43 + conjugated with
ubiquitin+
FUS: tau-, ubiquitin+,
TDP-43-, with fused in
sarcoma (FUS) inclusions
Seelar H, Rohrer LD, Pijnenburg YAL, Fox NC, can Swieten J C. Clinical, genetic and pathological
heterogeneity of frontotemporal dementia: A review. J Neurol Neurosurg Psychiatry 2010.
Tau immunopositive inclusions and neurofibrillary
tangles (NFTs) in tauopathy family of FTLDs
Pick inclusion bodies:
tau-positive spherical
cytoplasmic neuronal inclusions,
composed of straight filaments
NFTs and neuritic
threads (arrow) in the
gray matter of the frontal
cortex.
Perinuclear inclusions
of (asterisk) within the
frontal cortex
Reynolds M R et al. J. Neurosci. 2006;26:10636-10645
BIGGEST ADVANCE in ALS
and FTD
Chromosome 9 open reading frame 72
(C9ORF72) gene mutation most common
cause of familial ALS and FTD
Toxic buildup of RNA
Similar to other ALS genes but not SOD1
40% of familial ALS of European descent
15% of familiar ALS SOD1 mutation
Same expansion in 12% familial FTDand 3% sporadic FTD, 4%
in sporadic ALS!
Renton A, Majounie E, Waite A, J S-S, Sara Rollinson S, Gibbs J , et al. A Hexanucleotide Repeat Expansion in C9ORF72 Is the
Cause of Chromosome 9p21-Linked ALS-FTD. Neuron. 2011;72(2):257.
Dejesus-Hernandez M, Mackenzie I, Boeve B, Boxer A, Matt Baker, Rutherford N, et a Neuron. 2011;72(2):245.
Trained in mathematics, chemistry
and biology, Anne Adams, PhD
decided to leave her career in
science (1986) to care for a family
member and to take up art.
In 1994, she became fascinated
with the music of Ravel, and thus
painted Unravelling Bolro a
work that translated the famous
musical score into visual form.
Ironically, Ravel was in early PNFA
when composing Bolro. Both
Adams and Ravel died from
complications of PNFA/FTD.
Marcel Ravel
French
Composer
(1875-1937)
Anne Adams,
PhD
Chemist
(1940-2007)
FTD and creative bursts
Anne Adams, Unravelling Bolro, 1994
Each vertical figure represents a bar of music, with height corresponding to
volume. The theme repeats & builds until a change to orange/pink, representing
the key change preceding the dramatic conclusion.
Dr. Anne Adams,
Amsterdam (2004)
At the time of this painting,
Adams was nearly mute
taking 10-15 seconds to
initiate a word and was
formally diagnosed with
PNFA.
Adams then developed
a shuffling gait, R limb
apraxia and dystonia, and
stopped all verbal
communication. She died in
2007 from advanced FTD
with motor and respiratory
symptoms.
Seeley W W et al. Brain 2008;131:39-49
Questions?
Special thanks to the Cole Family Foundation for their ongoing
support of the Cole Neuroscience Center at UTMCK, and to
the Bagby family for their willingness to share and educate
others
Special recognition goes to my clinical mentor, Dr. J ohn
Dougherty, as well as to the neurologists and clinical team at
Cole Neuroscience Center.
You might also like
- Day 1: The Ultimate Guide To Decoding A Child's Sensory SystemDocument45 pagesDay 1: The Ultimate Guide To Decoding A Child's Sensory SystemLuca ServentiNo ratings yet
- Neuropsychological Tools for Dementia: Differential Diagnosis and TreatmentFrom EverandNeuropsychological Tools for Dementia: Differential Diagnosis and TreatmentRating: 3 out of 5 stars3/5 (1)
- Evaluation and Treatment of Neuropsychologically Compromised ChildrenFrom EverandEvaluation and Treatment of Neuropsychologically Compromised ChildrenNo ratings yet
- Treatment of Wernicke'S Aphasia With Jargon: A Case StudyDocument11 pagesTreatment of Wernicke'S Aphasia With Jargon: A Case StudyIvanaNo ratings yet
- Dyssemia Rating ScaleDocument8 pagesDyssemia Rating ScaleHazardous7No ratings yet
- Clinical Neurophysiology of The Vestibular System (001-057) PDFDocument57 pagesClinical Neurophysiology of The Vestibular System (001-057) PDFAriel CarterNo ratings yet
- Swallow Screening ToolDocument1 pageSwallow Screening Toolidris LajideNo ratings yet
- SOP Kids Club COVID 19 Measure For GO 2Document2 pagesSOP Kids Club COVID 19 Measure For GO 2adjcdaughtNo ratings yet
- Check Unit 555 November Immunology V3 PDFDocument25 pagesCheck Unit 555 November Immunology V3 PDFdragon66No ratings yet
- Degenerative DiseasesDocument29 pagesDegenerative DiseasesAwang WibisonoNo ratings yet
- Pseudobulbar Palsy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPseudobulbar Palsy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Language Dysfunction - Continnum - 2015Document19 pagesLanguage Dysfunction - Continnum - 2015Carolina Posada OrtizNo ratings yet
- Malingering and Neurological Basis of Crime: Presented by Ayesha, Fiza, Sahar, UsmaniaDocument87 pagesMalingering and Neurological Basis of Crime: Presented by Ayesha, Fiza, Sahar, UsmaniaMehroba malikNo ratings yet
- Occupational Therapy NICU SOAP Notes TemplateDocument1 pageOccupational Therapy NICU SOAP Notes TemplateNur Shuhada Suntong100% (1)
- (American Academy of Clinical Neuropsychology Oxford Workshop) Glenn E. Smith, Mark W. Bondi - Mild Cognitive Impairment and Dementia_ Definitions, Diagnosis, and Treatment-Oxford University Press (20 (1).pdfDocument416 pages(American Academy of Clinical Neuropsychology Oxford Workshop) Glenn E. Smith, Mark W. Bondi - Mild Cognitive Impairment and Dementia_ Definitions, Diagnosis, and Treatment-Oxford University Press (20 (1).pdfNicole CamachoNo ratings yet
- Treatment of Feeding Disorders in Children With Down SyndromeDocument13 pagesTreatment of Feeding Disorders in Children With Down SyndromeDaniela Aguirre GonzálezNo ratings yet
- ORLADocument10 pagesORLACarol CoelhoNo ratings yet
- Cognitive Assessment ToolkitDocument24 pagesCognitive Assessment ToolkitTeuku Ona AriefNo ratings yet
- Diagnostic Assessment and Management of Dysphagia in Patients With Alzheimer's DiseaseDocument9 pagesDiagnostic Assessment and Management of Dysphagia in Patients With Alzheimer's DiseaseLarissa MeloNo ratings yet
- Non-Speech Oro-Motor Exercises in Post-Stroke Dysarthria Intervention PDFDocument16 pagesNon-Speech Oro-Motor Exercises in Post-Stroke Dysarthria Intervention PDFhgood1001No ratings yet
- Finger Tapping Test AveragesDocument10 pagesFinger Tapping Test AveragesLuis ReyesNo ratings yet
- Dysphagia: Diagnosis and Treatment of Esophageal Motility DisordersFrom EverandDysphagia: Diagnosis and Treatment of Esophageal Motility DisordersMarco G. PattiNo ratings yet
- Common Classifications of AphasiaDocument1 pageCommon Classifications of AphasiaAhmad HasanNo ratings yet
- Ardila PDFDocument208 pagesArdila PDFGabyNoriegaNo ratings yet
- Neurocognitive Disorders: Ares Mari R. PadrejuanDocument33 pagesNeurocognitive Disorders: Ares Mari R. PadrejuanAres Mari PadrejuanNo ratings yet
- DyslexiaDocument19 pagesDyslexiaJubie MathewNo ratings yet
- Ccu PSG en DysphagiaDocument52 pagesCcu PSG en DysphagiaTni JolieNo ratings yet
- Cognitive 1Document3 pagesCognitive 1bobbysingersyahooNo ratings yet
- Developmental AssessmentDocument15 pagesDevelopmental AssessmentShailesh MehtaNo ratings yet
- Estimation of Premorbid Intelligence in Spanish People With The Word Accentuation Test and Its Application To The Diagnosis of DemenciaDocument14 pagesEstimation of Premorbid Intelligence in Spanish People With The Word Accentuation Test and Its Application To The Diagnosis of DemenciathebeholderNo ratings yet
- Measuring Oral Health and Quality of LifeDocument172 pagesMeasuring Oral Health and Quality of LifeCalin Dragoman100% (1)
- Global AphasiaDocument5 pagesGlobal AphasiaMuhammad Agus NurNo ratings yet
- 1326 Yorkston Kathryn PDFDocument70 pages1326 Yorkston Kathryn PDFArunprasad DurairajNo ratings yet
- From Anxiety To Meltdown: How Individuals On The Autism Spectrum Deal With Anxiety, Experience Meltdowns, Manifest Tantrums, and How You Can Intervene Effectively - PsychologyDocument4 pagesFrom Anxiety To Meltdown: How Individuals On The Autism Spectrum Deal With Anxiety, Experience Meltdowns, Manifest Tantrums, and How You Can Intervene Effectively - PsychologyfobisokaNo ratings yet
- Duffy Apraxia of SpeechDocument6 pagesDuffy Apraxia of SpeechRicardo OrdóñezNo ratings yet
- 200.201701-s MND Aware Living With MND - Aspects of CareDocument48 pages200.201701-s MND Aware Living With MND - Aspects of Careuni3467173No ratings yet
- PHYSIOTIMES Vol.7, Issue 5, March'2016Document1 pagePHYSIOTIMES Vol.7, Issue 5, March'2016PHYSIOTIMESNo ratings yet
- Living With Autism: Establishing Positive Sleep PatternsDocument4 pagesLiving With Autism: Establishing Positive Sleep PatternsanacrisnuNo ratings yet
- Frontal Lobe Syndromes: BackgroundDocument2 pagesFrontal Lobe Syndromes: BackgroundFausiah Ulva MNo ratings yet
- AphasiaDocument8 pagesAphasiaapi-308647214No ratings yet
- Vestibular Rehab in ShortDocument43 pagesVestibular Rehab in Shortshankerahul50% (2)
- Advanced Neurology Course Palermo 2017Document372 pagesAdvanced Neurology Course Palermo 2017Andrea BiniNo ratings yet
- Assessment and Treatment of Linguistic Deficits PDFDocument96 pagesAssessment and Treatment of Linguistic Deficits PDFJumraini TammasseNo ratings yet
- Ot Guidelines ParkinsonDocument145 pagesOt Guidelines ParkinsonFanny100% (1)
- Neuropsychological AssessmentDocument112 pagesNeuropsychological AssessmentCatalina BuzduganNo ratings yet
- Dysphagia in Huntington'sDocument5 pagesDysphagia in Huntington'sDani PiñaNo ratings yet
- Effective SLPDocument10 pagesEffective SLPRené Ignacio Guzmán SalgadoNo ratings yet
- Long-Term Memory Problems in Children and Adolescents: Assessment, Intervention, and Effective InstructionFrom EverandLong-Term Memory Problems in Children and Adolescents: Assessment, Intervention, and Effective InstructionNo ratings yet
- Frontal Lobe SyndromeDocument7 pagesFrontal Lobe SyndromeMu Z100% (1)
- Wisconsin Card Sorting Test Embedded Validity Indicators Developed For Adults Can Be Extended To ChildrenDocument16 pagesWisconsin Card Sorting Test Embedded Validity Indicators Developed For Adults Can Be Extended To ChildrenAnonymous 7YP3VYNo ratings yet
- Frontal Lobe SyndromeDocument15 pagesFrontal Lobe SyndromeLetitia Claudia DobraniciNo ratings yet
- Dysarthria AssessmentDocument11 pagesDysarthria AssessmentvviraaNo ratings yet
- Eating Assessment Tool EAT 10 PDFDocument70 pagesEating Assessment Tool EAT 10 PDFCarol Artigas GómezNo ratings yet
- Aphasia and Aphasic Syndromes, Neurourology Rehabilitation PDFDocument19 pagesAphasia and Aphasic Syndromes, Neurourology Rehabilitation PDFTahysse Andrea Varela SilvaNo ratings yet
- Judgment of Line OrientationDocument10 pagesJudgment of Line OrientationmcfenollarNo ratings yet
- Articulation ProblemDocument3 pagesArticulation ProblemErrorry JecksonNo ratings yet
- Manual PDFDocument84 pagesManual PDFEdsh Radgedolf RosalesNo ratings yet
- DysphagiaDocument1 pageDysphagiaShin EscaresesNo ratings yet
- Peripheral Vs Central Vestibular DisordersDocument2 pagesPeripheral Vs Central Vestibular DisordersraraNo ratings yet
- Cognitive Neuropsychology of ReadingDocument6 pagesCognitive Neuropsychology of ReadingDaniel MunarNo ratings yet
- Preventing Aspiration Pneumonia by Addressing Three Key Risk Factors - Dysphagia, Poor Oral Hygiene, and Medication UseDocument14 pagesPreventing Aspiration Pneumonia by Addressing Three Key Risk Factors - Dysphagia, Poor Oral Hygiene, and Medication UseStacey WoodsNo ratings yet
- Neurology 2016 Benjamin 324 33Document12 pagesNeurology 2016 Benjamin 324 33kattbattNo ratings yet
- The Argyll Robertson Pupil.12Document5 pagesThe Argyll Robertson Pupil.12kattbattNo ratings yet
- The Argyll Robertson Pupil.12Document5 pagesThe Argyll Robertson Pupil.12kattbattNo ratings yet
- Normality Checking 11 PsDocument4 pagesNormality Checking 11 PskattbattNo ratings yet
- The Argyll Robertson Pupil.12Document5 pagesThe Argyll Robertson Pupil.12kattbattNo ratings yet
- The Argyll Robertson Pupil.12Document5 pagesThe Argyll Robertson Pupil.12kattbattNo ratings yet
- The Argyll Robertson Pupil.12Document5 pagesThe Argyll Robertson Pupil.12kattbattNo ratings yet
- Brand ThyselfDocument68 pagesBrand ThyselfkattbattNo ratings yet
- Pract Neurol-2014-Zeman-136-44 PDFDocument9 pagesPract Neurol-2014-Zeman-136-44 PDFkattbattNo ratings yet
- The Argyll Robertson Pupil.12Document5 pagesThe Argyll Robertson Pupil.12kattbattNo ratings yet
- Brand ThyselfDocument68 pagesBrand ThyselfkattbattNo ratings yet
- Should We Get MarriedDocument10 pagesShould We Get MarriedkattbattNo ratings yet
- Atlas of Sleep MedicineDocument362 pagesAtlas of Sleep MedicinekattbattNo ratings yet
- J Neurol Neurosurg Psychiatry 2015 Garg JNNP 2014 309649Document10 pagesJ Neurol Neurosurg Psychiatry 2015 Garg JNNP 2014 309649kattbattNo ratings yet
- Bar-One Fridge Cheesecake: Chocolate BaseDocument1 pageBar-One Fridge Cheesecake: Chocolate BasekattbattNo ratings yet
- Chocolate Macaroons RecipeDocument1 pageChocolate Macaroons RecipekattbattNo ratings yet
- Evaluation of Macrocytic AnemiasDocument8 pagesEvaluation of Macrocytic Anemiasmy accountNo ratings yet
- QRP Neurology Part 2Document245 pagesQRP Neurology Part 2lakshminivas PingaliNo ratings yet
- Hernia - Surgery PrecisDocument1 pageHernia - Surgery PrecisSherif WagdyNo ratings yet
- Gastro MCQsDocument14 pagesGastro MCQsvaegmundigNo ratings yet
- Esophageal Diverticula - AMBOSSDocument1 pageEsophageal Diverticula - AMBOSSRazan Al-ZataryNo ratings yet
- JACC Volume 78, Issue 11 SeptemberDocument122 pagesJACC Volume 78, Issue 11 SeptemberFareesha KhanNo ratings yet
- Acute Myeloid LeukemiaDocument1 pageAcute Myeloid LeukemiaAlleah Salbo KepusNo ratings yet
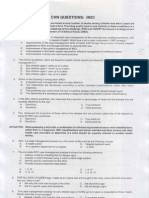
- CHN Questions ImciDocument5 pagesCHN Questions Imciredskie08100% (6)
- Nursing Case Presentation For A Patient With CABG: Subject: Medical Surgical Nursing-IIDocument10 pagesNursing Case Presentation For A Patient With CABG: Subject: Medical Surgical Nursing-IIanamika sharmaNo ratings yet
- ConjunctivitisDocument9 pagesConjunctivitisSaranya DeviNo ratings yet
- Diabetis 2Document33 pagesDiabetis 2Fercho MedNo ratings yet
- Rle Procedure StudyDocument4 pagesRle Procedure StudyMyangel LoiseNo ratings yet
- Horrific US Medical Experiments Come To LightDocument2 pagesHorrific US Medical Experiments Come To Lighthalojumper63No ratings yet
- Osce RadioDocument74 pagesOsce Radioberhanu nathanielNo ratings yet
- Digital Covid Questionnaire For Revival Approval FormatDocument2 pagesDigital Covid Questionnaire For Revival Approval Formatsouravdey3No ratings yet
- Garssen, 2004 - Physical Training and Fatigue, Fitness, and Quality of Life in Guillain-Barre Syndrome and CIDPDocument3 pagesGarssen, 2004 - Physical Training and Fatigue, Fitness, and Quality of Life in Guillain-Barre Syndrome and CIDPkarinaNo ratings yet
- Drug Study - Ello - Ampicillin - MultivitaminsDocument3 pagesDrug Study - Ello - Ampicillin - MultivitaminsCHRISTINE GRACE ELLONo ratings yet
- Basics of Soft - Tissue ExaminationDocument32 pagesBasics of Soft - Tissue ExaminationGurudutt PaiNo ratings yet
- Acetylcholine Esterase AntibodyDocument2 pagesAcetylcholine Esterase AntibodySrinivasanNo ratings yet
- Buttaravoli, Philip - Minor Emergencies - Blunt Scrotal Trauma (2007)Document3 pagesButtaravoli, Philip - Minor Emergencies - Blunt Scrotal Trauma (2007)Vivian ChanNo ratings yet
- Immunology and Immunochemistry PDFDocument8 pagesImmunology and Immunochemistry PDFboatcomNo ratings yet
- Nursing Care Plan: University of Tabuk Faculty of Applied Medical Science Department of NursingDocument3 pagesNursing Care Plan: University of Tabuk Faculty of Applied Medical Science Department of NursingZedoo AlmaroaaneNo ratings yet
- Clinical Learning Log 3 Go Solo - Docx-1Document11 pagesClinical Learning Log 3 Go Solo - Docx-1JezraleFame AntoyNo ratings yet
- 14.4 Cancer ScreeningDocument2 pages14.4 Cancer Screeningvenkat krishnanNo ratings yet
- Dr. Khairiyadi, M.Kes., Sp.A Departemen Ilmu Kesehatan Anak RSUD Ulin BanjarmasinDocument78 pagesDr. Khairiyadi, M.Kes., Sp.A Departemen Ilmu Kesehatan Anak RSUD Ulin BanjarmasinEldhaNo ratings yet
- Post Traumatic Stress DisorderDocument4 pagesPost Traumatic Stress DisorderaploureyNo ratings yet
- The Truth About Polio VaccineDocument23 pagesThe Truth About Polio Vaccinemagnumquest67% (3)
- Drug Study FINALDocument32 pagesDrug Study FINALhomeworkping1No ratings yet