Professional Documents
Culture Documents
Understanding Auditory Processing Disorders in Children
Uploaded by
Zhen JinxCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Understanding Auditory Processing Disorders in Children
Uploaded by
Zhen JinxCopyright:
Available Formats
Understanding Auditory Processing Disorders in
Children
by Teri James Bellis, PhD, CCC-A
In recent years, there has been a dramatic upsurge in professional and public awareness of
Auditory Processing Disorders (APD), also referred to as Central Auditory Processing Disorders
(CAPD). Unfortunately, this increase in awareness has resulted in a plethora of misconceptions and
misinformation, as well as confusion regarding just what is (and isn't) an APD, how APD is
diagnosed, and methods of managing and treating the disorder. The term auditory processing
often is used loosely by individuals in many different settings to mean many different things, and
the label APD has been applied (often incorrectly) to a wide variety of difficulties and disorders. As
a result, there are some who question the existence of APD as a distinct diagnostic entity and
others who assume that the term APD is applicable to any child or adult who has difficulty listening
or understanding spoken language. The purpose of this article is to clarify some of these key
issues so that readers are better able to navigate the jungle of information available on the subject
in professional and popular literature today.
Terminology and Definitions
In its very broadest sense, APD refers to how the central nervous system (CNS) uses auditory
information. However, the CNS is vast and also is responsible for functions such as memory,
attention, and language, among others. To avoid confusing APD with other disorders that can
affect a person's ability to attend, understand, and remember, it is important to emphasize that
APD is an auditory deficit that is not the result of other higher-order cognitive, language, or related
disorder.
There are many disorders that can affect a person's ability to understand auditory information. For
example, individuals with Attention Deficit/Hyperactivity Disorder (ADHD) may well be poor
listeners and have difficulty understanding or remembering verbal information; however, their
actual neural processing of auditory input in the CNS is intact. Instead, it is the attention deficit
that is impeding their ability to access or use the auditory information that is coming in. Similarly,
children with autism may have great difficulty with spoken language comprehension. However, it is
the higher-order, global deficit known as autism that is the cause of their difficulties, not a specific
auditory dysfunction. Finally, although the terms language processing and auditory processing
sometimes are used interchangeably, it is critical to understand that they are not the same thing
at all.
For many children and adults with these disorders and others - including mental retardation and
sensory integration dysfunction - the listening and comprehension difficulties we often see are due
to the higher-order, more global or all-encompassing disorder and not to any specific deficit in the
neural processing of auditory stimuli per se. As such, it is not correct to apply the label APD to
these individuals, even if many of their behaviors appear very similar to those associated with
APD. In some cases, however, APD may co-exist with ADHD or other disorders. In those cases,
only careful and accurate diagnosis can assist in disentangling the relative effects of each.
Diagnosing APD
Children with APD may exhibit a variety of listening and related complaints. For example, they
may have difficulty understanding speech in noisy environments, following directions, and
discriminating (or telling the difference between) similar-sounding speech sounds. Sometimes they
may behave as if a hearing loss is present, often asking for repetition or clarification. In school,
children with APD may have difficulty with spelling, reading, and understanding information
presented verbally in the classroom. Often their performance in classes that don't rely heavily on
listening is much better, and they typically are able to complete a task independently once they
know what is expected of them. However, it is critical to understand that these same types of
symptoms may be apparent in children who do not exhibit APD. Therefore, we should always keep
in mind that not all language and learning problems are due to APD, and all cases of APD do not
lead to language and learning problems. APD cannot be diagnosed from a symptoms checklist. No
matter how many symptoms of APD a child may have, only careful and accurate diagnostics can
determine the underlying cause.
A multidisciplinary team approach is critical to fully assess and understand the cluster of problems
exhibited by children with APD. Thus, a teacher or educational diagnostician may shed light on
academic difficulties; a psychologist may evaluate cognitive functioning in a variety of different
areas; a speech-language pathologist may investigate written and oral language, speech, and
related capabilities; and so forth. Some of these professionals may actually use test tools that
incorporate the terms "auditory processing" or "auditory perception" in their evaluation, and may
even suggest that a child exhibits an "auditory processing disorder." Yet it is important to know
that, however valuable the information from the multidisciplinary team is in understanding the
child's overall areas of strength and weakness, none of the test tools used by these professionals
are diagnostic tools for APD, and the actual diagnosis of APD must be made by an audiologist.
To diagnose APD, the audiologist will administer a series of tests in a sound-treated room. These
tests require listeners to attend to a variety of signals and to respond to them via repetition,
pushing a button, or in some other way. Other tests that measure the auditory system's
physiologic responses to sound may also be administered. Most of the tests of APD require that a
child be at least 7 or 8 years of age because the variability in brain function is so marked in
younger children that test interpretation may not be possible.
Once a diagnosis of APD is made, the nature of the disorder is determined. There are many types
of auditory processing deficits and, because each child is an individual, APD may manifest itself in
a variety of ways. Therefore, it is necessary to determine the type of auditory deficit a given child
exhibits so that individualized management and treatment activities may be recommended that
address his or her specific areas of difficulty.
Treating APD
It is important to understand that there is not one, sure-fire, cure-all method of treating APD.
Notwithstanding anecdotal reports of "miracle cures" available in popular literature or on the
internet, treatment of APD must be highly individualized and deficit-specific. No matter how
successful a particular therapy approach may have been for another child, it does not mean that it
will be effective for your child. Therefore, the key to appropriate treatment is accurate and careful
diagnosis by an audiologist.
Treatment of APD generally focuses on three primary areas: changing the learning or
communication environment, recruiting higher-order skills to help compensate for the disorder,
and remediation of the auditory deficit itself. The primary purpose of environmental modifications
is to improve access to auditorily presented information. Suggestions may include use of electronic
devices that assist listening, teacher-oriented suggestions to improve delivery of information, and
other methods of altering the learning environment so that the child with APD can focus his or her
attention on the message.
Compensatory strategies usually consist of suggestions for assisting listeners in strengthening
central resources (language, problem-solving, memory, attention, other cognitive skills) so that
they can be used to help overcome the auditory disorder. In addition, many compensatory
strategy approaches teach children with APD to take responsibility for their own listening success
or failure and to be an active participant in daily listening activities through a variety of active
listening and problem-solving techniques.
Finally, direct treatment of APD seeks to remediate the disorder, itself. There exist a wide variety
of treatment activities to address specific auditory deficits. Some may be computer- assisted,
others may include one-on-one training with a therapist. Sometimes home-based programs are
appropriate whereas others may require children to attend therapy sessions in school or at a local
clinic. Once again, it should be emphasized that there is no one treatment approach that is
appropriate for all children with APD. The type, frequency, and intensity of therapy, like all aspects
of APD intervention, should be highly individualized and programmed for the specific type of
auditory disorder that is present.
The degree to which an individual child's auditory deficits will improve with therapy cannot be
determined in advance. Whereas some children with APD experience complete amelioration of
their difficulties or seem to "grow out of" their disorders, others may exhibit some residual degree
of deficit forever. However, with appropriate intervention, all children with APD can learn to
become active participants in their own listening, learning, and communication success rather than
hapless (and helpless) victims of an insidious impairment. Thus, when the journey is navigated
carefully, accurately, and appropriately, there can be light at the end of the tunnel for the millions
of children afflicted with APD.
Key Points:
APD is an auditory disorder that is not the result of higher-order, more global deficit such as
autism, mental retardation, attention deficits, or similar impairments.
Not all learning, language, and communication deficits are due to APD.
No matter how many symptoms of APD a child has, only careful and accurate diagnosis can
determine if APD is, indeed, present.
Although a multidisciplinary team approach is important in fully understanding the cluster of
problems associated with APD, the diagnosis of APD can only be made by an audiologist.
Treatment of APD is highly individualized. There is no one treatment approach that is
appropriate for all children with APD.
How We Hear
Parts of the Ear: Outer Ear | Middle Ear | Inner Ear
Hearing is one of the five senses. It is a complex
process of picking up sound and attaching meaning
to it. The ability to hear is critical to understanding
the world around us.
The human ear is a fully developed part of our bodies
at birth and responds to sounds that are very faint as
well as sounds that are very loud. Even before birth,
infants respond to sound.
So, how do we hear?
The ear can be divided into three parts leading up to the brain the outer ear, middle ear and
the inner ear.
The outer ear consists of the ear canal and eardrum. Sound travels down the ear canal,
striking the eardrum and causing it to move or vibrate.
The middle ear is a space behind the eardrum that contains three small bones called
ossicles. This chain of tiny bones is connected to the eardrum at one end and to an
opening to the inner ear at the other end. Vibrations from the eardrum cause the
ossicles to vibrate which, in turn, creates movement of the fluid in the inner ear.
Movement of the fluid in the inner ear, or cochlea, causes changes in tiny structures
called hair cells. This movement of the hair cells sends electric signals from the inner
ear up the auditory nerve (also known as the hearing nerve) to the brain.
The brain then interprets these electrical signals as sound
Degree of Hearing Loss
Degree of hearing loss refers to the severity of the loss. The table below shows one of the more
commonly used classification systems. The numbers are representative of the patient's hearing
loss range in decibels (dB HL).
Degree of hearing loss Hearing loss range (dB HL)
Normal 10 to 15
Slight 16 to 25
Mild 26 to 40
Moderate 41 to 55
Moderately severe 56 to 70
Severe 71 to 90
Profound 91+
Source: Clark, J. G. (1981). Uses and abuses of hearing loss classification. Asha, 23, 493500.
Hearing loss can be categorized by which part of the auditory system is damaged. There are three
basic types of hearing loss:
conductive hearing loss,
Conductive hearing loss occurs when sound is not conducted efficiently through the outer ear canal
to the eardrum and the tiny bones (ossicles) of the middle ear. Conductive hearing loss usually
involves a reduction in sound level or the ability to hear faint sounds. This type of hearing loss can
often be corrected medically or surgically.
Some possible causes of conductive hearing loss:
Fluid in the middle ear from colds
Ear infection (otitis media)
Allergies (serous otitis media)
Poor eustachian tube function
Perforated eardrum
Benign tumors
Impacted earwax (cerumen)
Infection in the ear canal (external otitis)
Presence of a foreign body
Absence or malformation of the outer ear, ear canal, or middle ear
sensorineural hearing loss,
Sensorineural hearing loss (SNHL) occurs when there is damage to the inner ear (cochlea), or to
the nerve pathways from the inner ear to the brain. Most of the time, SNHL cannot be medically or
surgically corrected. This is the most common type of permanent hearing loss.
SNHL reduces the ability to hear faint sounds. Even when speech is loud enough to hear, it may
still be unclear or sound muffled.
Some possible causes of SNHL:
Illnesses
Drugs that are toxic to hearing
Hearing loss that runs in the family (genetic or hereditary)
Aging
Head trauma
Malformation of the inner ear
Exposure to loud noise
and mixed hearing loss.
Sometimes a conductive hearing loss occurs in combination with a sensorineural hearing loss
(SNHL). In other words, there may be damage in the outer or middle ear and in the inner ear
(cochlea) or auditory nerve. When this occurs, the hearing loss is referred to as a mixed hearing
loss.
Classroom Acoustics
A student's ability to hear and understand what is being said in the classroom is vital for learning.
Unfortunately, this ability can be reduced in a noisy classroom. Poor classroom acoustics occur
when the background noise and/or the amount of reverberation in the classroom are so high that
they interfere with learning and teaching. We know that when classroom acoustics are poor then it
can affect
speech understanding
reading and spelling ability
behavior in the classroom
attention
concentration
academic achievement
What is background noise and reverberation?
Background noise is any unwanted sound that interferes with what you want to hear. Background
noise in a classroom can come from many sources such as traffic, lawnmowers, children on the
playground or in the hallway, heating or air conditioning units, audiovisual equipment, or other
students.
Reverberation refers to the phenomenon of sound continuing to be present in a room because of
sound reflecting off of surfaces such as desks or chairs. When sound lingers in a room there is
more interference with speech. In a classroom it is important to have a short reverberation time.
Who is affected by poor classroom acoustics?
All children are affected by poor classroom acoustics, but it can be a particular problem for children
with the following problems:
hearing loss, including children with a hearing loss in one ear (unilateral hearing loss)
temporary hearing loss in one or both ears (ear infection or build up of middle ear fluid)
learning disabilities
auditory processing disorders
speakers of another language
speech and language delay
attention problems
Poor classroom acoustics can also affect the teacher. It is estimated that teachers use their voices
for approximately 60% of their workday. The strain on the voice gets worse when the teacher has
to talk louder to overcome poor classroom acoustics. Studies have shown that teachers are 32
times more likely to have voice problems compared to similar occupations.
Creating an environment where good communication can take place should be a goal for any
classroom or learning space. Communication breaks down when the classroom acoustics are poor.
Reducing noise and reverberation in any space used for learning, such as community buildings,
home-based classrooms, and classrooms in places of worship, is important.
To learn about improving the acoustics in your classroom see Tips for Creating a Good Listening
Environment.
Tips for Creating a Good Listening Environment in the
Classroom
If your classroom is too noisy here are some simple tips to help make the environment quieter:
Place some rugs or carpet in the room if there none.
Hang window treatments such as curtains or blinds.
Hang soft materials such as felt or corkboard on the walls.
Place tables at an angle around the room to interfere with the pathways of sound.
Hang soft materials such as flags or student artwork around the room and from the ceiling.
Turn off noisy equipment when it is not in use.
Try to keep windows and doors closed when possible.
Replace noisy light fixtures.
Avoid open classrooms where many classes are taught in a large space.
Talk to the students about noise and demonstrate how it can be difficult to hear when many
children are talking at the same time.
Avoid dividing the class into groups where one group is listening to audiovisual equipment such
as the TV and the other group is listening to the teacher.
Remind visitors to the classroom that they should not be talking when the teacher is talking.
Place latex-free soft tips on the bottoms of chairs and tables. Do not use tennis balls to
dampen the sound! Tennis balls are made of latex which can cause allergic reactions in some
individuals. Also, mold can grow inside of the open tennis balls, which also poses a health risk.
Sports balls and materials free of latex are available from a variety of sources
ACUTE AND INTERMEDIATE PHASE NURSING IN TBI:
SENSORY-PERCEPTUAL, COMMUNICATION, AND
COGNITION DEFICITS
Sensory-Perceptual Deficits
1. Problems/Causes include deficits as a result of the injury in
vision, communication, and/or perception of self, body
image, illness, spatial relationships, agnosia, and apraxia
2. Nursing Diagnoses include:
o Perception of illness deficits, such as denial of
hemiplegia or other motor or sensory deficits and
anosognosia, the inability to recognize the denial or
unawareness of a deficit
o Body image disturbance, the patient's concept of the
sum of his/her body parts in relationship to the whole,
including unilateral neglect, the ignoring of the
hemiplegic side
o Sensory/perceptual alterations, such as:
Hemianopia (loss of vision in half of the
visual field) and defects in localizing objects
in space, estimating size, judging distances,
remembering arrangement of objects, finding
one's way to or back from places, telling time,
and right-hand discrimination
Agnosia, the inability to recognize familiar
objects with the senses
o Self-care deficit, such as apraxia, the inability to carry
out a learned, voluntary act in the absence of paralysis
3. Assessments include:
o Fails to use, shows a lack of concern for, lacks
awareness of or denies the part of the body involved
in hemiplegia or other motor or sensory deficits
o Draws an object and omits the side of the object that
corresponds to the affected side of the body
o Has difficulty walking through a doorway, exhibits
impaired recall of objects in a familiar environment,
has difficulty reading and computation, and is unable
to identify left or right
o Unable to identify common objects by sight or with
the eyes closed or to respond appropriately to
common sounds
o Exhibits clumsiness or an inability to carry out ADLs
correctly or to complete a task involving a sequence
of components
4. Nursing Interventions include:
o Accepting the patient's perception of, stimulating the
affected side or body part, teaching the patient to
position and care for the affected side or body part,
and positioning the affected side or part in the
patient's visual field
o Encouraging the patient to handle and use the affected
side or body part and teaching visual scanning and
other compensatory measures
o Providing verbal cues and instructions to the affected
side or body part
o Having the patient use other, intact senses to identify
stimuli or objects, teaching relearning via the drill
method, protecting the patient from injury, and
interpreting the patient's behavior for the family
o Encouraging participation in ADLs, correcting
mistakes or misuse of equipment, and reteaching
forgotten skills
Communication Deficits
1. Problems and Nursing Diagnoses - Aphasia in 1 of 3 forms:
o Nonfluent aphasia, the inability to express thoughts
verbally or in writing, can vary from mild to severe
o Fluent aphasia, the ability to hear, but not fully
comprehend speech, resulting in speech by the patient
that contains many errors and may be lengthy
o Global aphasia, a combination of expressive and
receptive aphasia in which little of the communication
system is left intact
2. Assessments
o Needs to search for words, chooses incorrect words
o Can communicate only by pointing, pantomime, etc.
3. Nursing Interventions include:
o Stimulating conversation, giving patient time to
search for words, disregarding incorrect words, and
generally supporting the patient's efforts to speak
o Accepting alternate forms of communication and
showing the patient pictures to permit communication
o Standing close so patient is aware of lip movements
o Speaking slowly and distinctly in a normal speaking
voice, using vocabulary or gestures the patient can
understand
o Anticipating the patient's needs
Cognitive Deficits
1. Problems/Nursing Diagnoses include:
o Shortened attention span and concentration, due to
diminished alertness, effort, and selection of stimuli
received
o Impaired judgment, due to decreased comprehension
and an inability to determine the consequences of
actions
o Impaired memory, both verbal and visual memory
o Initiation and sequencing problems
2. Assessments
o Inability to focus long enough to permit
understanding and appropriate response, and easily
distracted by external environmental factors
o Inability to take action in a safe and appropriate
manner
o Inability to retain information for 1 minute - 1 hour
(short-term memory) or for 1 hour or longer (long-
term memory)
o Inability to start a task and complete it from start to
finish
3. Nursing Interventions
o Attention: Reduce/minimize distractions, simply tasks
and procedures, allow ample time for task completion,
refocus attention as needed, avoid fatigue, provide
frequent verbal, visual, or tactile cues, and encourage
simple leisure activities
o Judgment: Allow patient to make simple decisions,
involve patient in other decision making processes,
and provide patient choices, ample time, and frequent
feedback
o Memory: Encourage use of memory aids, provide
clocks, calendars, radios and TVs, structure daily
exercises, post schedule/routine in a highly visible
place, and repeat and record new information as
needed for later review
o Initiate/sequence: Post daily schedule in a highly
visible place, break tasks into smaller steps, provide
cues for each step, allow patient to complete each
step, and provide supervision and support
Based on information in Hickey JV. The Clinical Practice of Neurological and Neurosurgical Nursing, 4th ed., Philadelphia: Lippincott, 1997 and in
Chin PA, et al. Rehabilitation Nursing Practice, N.Y.: McGraw-Hill, 1998, except for information where other papers are cited.
You might also like
- Waj3103 IslDocument5 pagesWaj3103 IslZhen JinxNo ratings yet
- Super ReportDocument8 pagesSuper ReportSameer GhuryeNo ratings yet
- Isl Week 11Document3 pagesIsl Week 11Zhen JinxNo ratings yet
- Isl 5Document4 pagesIsl 5Zhen JinxNo ratings yet
- Self Learning6Document4 pagesSelf Learning6Zhen JinxNo ratings yet
- Isl Week 9Document3 pagesIsl Week 9Zhen JinxNo ratings yet
- Isl 10 and 12Document5 pagesIsl 10 and 12Zhen JinxNo ratings yet
- ResourcesDocument13 pagesResourcesNajmi TajudinNo ratings yet
- Learning 2Document7 pagesLearning 2Zhen JinxNo ratings yet
- Real-Life Problem Using Theory of SetsDocument3 pagesReal-Life Problem Using Theory of SetsZhen JinxNo ratings yet
- How To Write A News Cast ScriptsDocument2 pagesHow To Write A News Cast ScriptsZhen JinxNo ratings yet
- Re FferenceDocument1 pageRe FferenceZhen JinxNo ratings yet
- WatDocument1 pageWatZhen JinxNo ratings yet
- HosannaDocument1 pageHosannaZhen JinxNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Bronfenbrenner S Ecological TheoryDocument24 pagesBronfenbrenner S Ecological TheoryJulie Anne BunaoNo ratings yet
- Edexcel GCSE Mathematics (Linear) – 1MA0 ALGEBRA: EXPAND & FACTORISEDocument8 pagesEdexcel GCSE Mathematics (Linear) – 1MA0 ALGEBRA: EXPAND & FACTORISETakayuki MimaNo ratings yet
- (AC-S05) Week 05 - Pre-Task - Quiz - Weekly Quiz - INGLES IV (11287)Document5 pages(AC-S05) Week 05 - Pre-Task - Quiz - Weekly Quiz - INGLES IV (11287)Enith AlzamoraNo ratings yet
- JDVP-TVL Program Billing StatementDocument2 pagesJDVP-TVL Program Billing StatementジナNo ratings yet
- NN Post Excursion Jacob Ballas 2014 t2Document3 pagesNN Post Excursion Jacob Ballas 2014 t2api-342873214No ratings yet
- Jesse Robredo Memorial BookDocument141 pagesJesse Robredo Memorial Bookannoying_scribd100% (1)
- Lesson Plan For Teaching WritingDocument7 pagesLesson Plan For Teaching WritingSaharudin YamatoNo ratings yet
- ReferencesDocument6 pagesReferencesPaula Jane LemoncitoNo ratings yet
- Context CLuesDocument17 pagesContext CLuesjes0009100% (1)
- Toning Revelation BookDocument35 pagesToning Revelation Bookmaicumotz100% (2)
- Cuban Visions 2011 ScribdDocument62 pagesCuban Visions 2011 ScribdCubanVisions100% (2)
- History of Nursing ProfessionDocument161 pagesHistory of Nursing ProfessionRashmi C SNo ratings yet
- VDC Final Project - Group3Document18 pagesVDC Final Project - Group3Aarav BalachandranNo ratings yet
- 2019-2020 Schola Application PDFDocument2 pages2019-2020 Schola Application PDFJane Limsan PaglinawanNo ratings yet
- Effective For The 2009-2010 School Year: School Uniform and Appearance PolicyDocument7 pagesEffective For The 2009-2010 School Year: School Uniform and Appearance Policyapi-250489050No ratings yet
- BS Artificial Intelligence Graduatoria Web Non-EU 2023-2024 Rettifica 14-06-2023 - PdfaDocument14 pagesBS Artificial Intelligence Graduatoria Web Non-EU 2023-2024 Rettifica 14-06-2023 - PdfayashbinladenNo ratings yet
- My Educational PhilosophyDocument6 pagesMy Educational PhilosophyRiza Grace Bedoy100% (1)
- 2022 IISMA Awards for Indonesian Students to Study AbroadDocument22 pages2022 IISMA Awards for Indonesian Students to Study AbroadRafli RidwanNo ratings yet
- Doing PhilosophyDocument71 pagesDoing Philosophyrheamay libo-onNo ratings yet
- Ventures3e SB Transitions3e U01Document15 pagesVentures3e SB Transitions3e U01محمد ٦No ratings yet
- Didactic Reduction: Literature Art Ancient Greek EducationDocument3 pagesDidactic Reduction: Literature Art Ancient Greek EducationEka PrastiyantoNo ratings yet
- SF Parish School 1st Grading Period ResultsDocument5 pagesSF Parish School 1st Grading Period ResultsShela may AntrajendaNo ratings yet
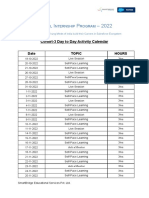
- Virtual Internship Program Activity CalendarDocument2 pagesVirtual Internship Program Activity Calendaranagha joshiNo ratings yet
- Unit Test - The Southwest Region: - /15 PointsDocument10 pagesUnit Test - The Southwest Region: - /15 Pointsapi-480186406No ratings yet
- Penulisan Rujukan Mengikut Format Apa Contoh PDFDocument16 pagesPenulisan Rujukan Mengikut Format Apa Contoh PDFzatty kimNo ratings yet
- Hoc Volume1Document46 pagesHoc Volume1nordurljosNo ratings yet
- Pembugaran EnglishDocument3 pagesPembugaran EnglishgomyraiNo ratings yet
- College Code College Name BranchDocument32 pagesCollege Code College Name BranchRaju DBANo ratings yet
- Heritage Tourism in IndiaDocument13 pagesHeritage Tourism in Indiavinay narneNo ratings yet
- Declaration: Engineering in Mechanical Engineering Under VISVESVARAYA TECHNOLOGICAL UNIVERSITY, BelgaumDocument4 pagesDeclaration: Engineering in Mechanical Engineering Under VISVESVARAYA TECHNOLOGICAL UNIVERSITY, BelgaumChandan KNo ratings yet