Professional Documents
Culture Documents
Autoimmune Hepatitis
Uploaded by
Fazmial UjirCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Autoimmune Hepatitis
Uploaded by
Fazmial UjirCopyright:
Available Formats
ARTIKEL FLU BURUNG
Background
During 2004, a highly pathogenic avian influenza A (H5N1) virus caused poultry disease in eight Asian
countries and infected at least 44 persons, killing 32; most of these persons had had close contact with
poultry. No evidence of efficient person-to-person transmission has yet been reported. We
investigated possible person-to-person transmission in a family cluster of the disease in Thailand.
Full Text of Background...
Methods
For each of the three involved patients, we reviewed the circumstances and timing of exposures to
poultry and to other ill persons. Field teams isolated and treated the surviving patient, instituted
active surveillance for disease and prophylaxis among exposed contacts, and culled the remaining
poultry surrounding the affected village. Specimens from family members were tested by viral culture,
microneutralization serologic analysis, immunohistochemical assay, reverse-transcriptase
polymerase-chain-reaction (RT-PCR) analysis, and genetic sequencing.
Full Text of Methods...
Results
The index patient became ill three to four days after her last exposure to dying household chickens.
Her mother came from a distant city to care for her in the hospital, had no recognized exposure to
poultry, and died from pneumonia after providing 16 to 18 hours of unprotected nursing care. The
aunt also provided unprotected nursing care; she had fever five days after the mother first had fever,
followed by pneumonia seven days later. Autopsy tissue from the mother and nasopharyngeal and
throat swabs from the aunt were positive for influenza A (H5N1) by RT-PCR. No additional chains of
transmission were identified, and sequencing of the viral genes identified no change in the receptor-
binding site of hemagglutinin or other key features of the virus. The sequences of all eight viral gene
segments clustered closely with other H5N1 sequences from recent avian isolates in Thailand.
Full Text of Results...
Conclusions
Disease in the mother and aunt probably resulted from person-to-person transmission of this lethal
avian influenzavirus during unprotected exposure to the critically ill index patient.
KASUS FLU BURUNG
Probable Person-to-Person Transmission of Avian Influenza A (H5N1)
Kumnuan Ungchusak, M.D., M.P.H., Prasert Auewarakul, M.D., Scott F. Dowell, M.D., M.P.H.,
Rungrueng Kitphati, M.D., Wattana Auwanit, Ph.D., Pilaipan Puthavathana, Ph.D., Mongkol
Uiprasertkul, M.D., Kobporn Boonnak, M.Sc., Chakrarat Pittayawonganon, M.D., Nancy J. Cox, Ph.D.,
Sherif R. Zaki, M.D., Ph.D., Pranee Thawatsupha, M.S., Malinee Chittaganpitch, B.Sc., Rotjana
Khontong, M.D., James M. Simmerman, R.N., M.S., and Supamit Chunsutthiwat, M.D., M.P.H.
N Engl J Med 2005; 352:333-340January 27, 2005
AbstractArticleReferencesCiting Articles (281
.
During the first months of 2004, outbreaks of highly pathogenic avian influenza caused by influenza A
(H5N1) virus were recognized in eight Asian countries.1,2 The poultry outbreaks receded and then
reappeared in July in five countries, with human cases recognized in Vietnam and Thailand.3 As of
November 11, 2004, there had been 44 documented human infections and 32 deaths (mortality, 73
percent), sparking fears that this lethal pathogen might cause a pandemic.
Since the first avian influenza outbreak, in 1997,4 there has been concern that the influenza A (H5N1)
virus might either mutate and adapt to allow efficient transmission during the infection of mammals
or reassort its gene segments with human influenzaviruses during the coinfection of a single host,
resulting in a new virus that would be both highly lethal and transmissible from person to person.
Such events are believed to have preceded the influenza pandemics of 1918, 1957, and 1968.5 Several
lines of evidence indicate that the currently circulating influenza A (H5N1) viruses have in fact evolved
to more virulent forms since 1997, with a higher mortality among human cases,1,4 different antigenic
properties,6 a different internal gene constellation,7 and an expanded host range.8,9
In most of the human cases to date, the patients had well-documented exposure to sick or dying
poultry,10-12 but there have been several episodes of possible person-to-person spread. Two health
care workers who cared for patients in Hong Kong in 1997 were later found to have antibodies to
hemagglutinin H5, and one recalled having had a respiratory illness after exposure to one of the
patients.13 Two family clusters in Vietnam in 2004 were considered to be compatible with bird-to-
human spread, although limited person-to-person spread could not be ruled out.12
We report the results of an investigation into a family cluster of influenza A (H5N1) virus infections.
This cluster was unusual in that one of the infected family members lived in a distant city but provided
direct, in-hospital care for the index patient, highlighting the possibility of person-to-person
transmission.
Methods
Patients
The index patient was an 11-year-old girl who lived with her aunt and who presented to a clinic with
fever, cough, and a sore throat on September 2, 2004. She was admitted to the hospital on September
7 with a temperature of 38.5C and moderate dyspnea. Initial testing identified lymphopenia and
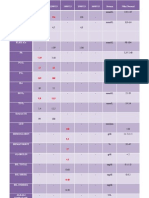
thrombocytopenia (Table 1Table 1Clinical and Epidemiologic Features of the Family Cluster of Avian
Influenza (H5N1).) and a left-lower-lobe infiltrate on chest radiography (Figure 1AFigure 1Chest
Radiographs from the Three Patients with Avian Influenza A (H5N1).). Because of progressive
respiratory distress, hypoxemia, and shock, she was transferred to the provincial hospital the next day
with a diagnosis of viral pneumonitis or the dengue shock syndrome. A serum sample was negative
for antibodies to dengue virus. Despite mechanical ventilation, administration of broad-spectrum
antibiotics, and fluid resuscitation, the patient died three hours after admission to the provincial
hospital.
The index patient's mother was a 26-year-old woman who lived in another province. She provided
bedside care for her daughter in the hospital for 16 to 18 hours on September 7 and 8. She began to
have fever and headache three days later and spent a night in her daughter's village before returning
to her home. On September 17, she was admitted to a hospital in her own province with fever and
severe dyspnea. She had lymphopenia and thrombocytopenia (Table 1) and bilateral interstitial
infiltrates on chest radiography (Figure 1B). Pneumonia and progressive respiratory failure were
diagnosed, and she died on September 20.
The index patient's aunt was a 32-year-old woman who lived with her niece. She provided bedside
care for her niece for 12 or 13 hours on September 7 and noted the onset of fever, myalgia, and chills
on September 16. An upper respiratory infection was diagnosed at a clinic on September 19, but she
had progressive difficulty breathing and was admitted to the district hospital on September 23 with a
temperature of 39.7C, lymphopenia (Table 1), and left-lower-lobe consolidation (Figure 1C). On the
day of admission, an investigating team suspected avian influenza, obtained respiratory specimens for
testing, initiated treatment with oseltamivir, and instituted full isolation precautions. Despite
moderate dyspnea and hypoxemia, her condition gradually improved, and she was discharged on
October 7.
Epidemiologic Investigations
Under the nationwide surveillance system established in Thailand in early 2004, patients who were
hospitalized with pneumonia or influenza and who had been exposed to ill poultry were reported to
the Thai Ministry of Public Health. Because the mother had no exposure to poultry and the index
patient's exposure was not initially reported, this cluster was recognized only coincidentally, during
the investigation of another pneumonia-related death at the hospital where the mother had died.
Public health staff interviewed all family members on multiple occasions, especially those with
possible exposure to sick or dying poultry, and developed and cross-checked several written timelines
of events. Medical records were reviewed for the time of onset and progression of the illnesses.
All household members, other family contacts, exposed neighbors, and exposed health care workers
were placed under active surveillance for fever and respiratory symptoms for 14 days. All remaining
poultry were culled.
Laboratory Investigations
By the time this family cluster was recognized, the index patient had died and her body had been
cremated, and the mother had died and her body had been embalmed; therefore, appropriate
specimens for influenza A (H5N1) testing were not easily obtained. Serum from the index patient and
the aunt was tested for antibodies to H5. With the permission of the family, an autopsy was
performed on the mother. Nasopharyngeal and oropharyngeal swabs were obtained from the aunt
and other household members.
Specimens were submitted for testing at the Thai National Institute of Health and the virology
laboratory at Siriraj Hospital, Mahidol University, in Bangkok, and at the Centers for Disease Control
and Prevention (CDC), in Atlanta. Specimens in transport medium were tested by conventional
reverse-transcriptase polymerase-chain-reaction
(RT-PCR) analysis and real-time RT-PCR and by cell culture and hen's-egg inoculation for viral isolation,
including two or three blind passages, as previously described.14-16 Antibody testing was performed
at Siriraj Hospital and at the CDC by means of microneutralization and enzyme-linked immunosorbent
assays, with confirmation by Western blotting.17
Fragments of the hemagglutinin gene containing sequences encoding the receptor-binding site and
fragments of other genes were amplified by RT-PCR from RNA samples extracted from embalmed lung
tissue from the mother and from the aunt's nasopharyngeal swab. RT-PCR was performed with the
use of random hexamers as primers for DNA synthesis and specific primers for RT-PCR, and the
products were sequenced directly. The nucleotide sequences were analyzed with Phylogeny Inference
Package software and the use of a maximal-parsimony algorithm.
Formalin-fixed, paraffin-embedded lung-tissue blocks from the mother were examined by routine
staining with hematoxylin and eosin and were tested with a monoclonal antibody specific for
influenza A nucleoprotein by means of a colorimetric immunohistochemical assay.18
Results
Epidemiologic Findings
Interviews of the aunt, the other surviving family members, and neighbors permitted reconstruction
of the timing of relevant exposures and the onset of illness in the index patient and her mother and
aunt (Figure 2Figure 2Timeline of Pertinent Exposures and Dates of Illness in the Three Patients.). The
last of the free-ranging household chickens died on August 29 or 30, after progressive illness and
death among the flock during the preceding weeks. The index patient was not known to have had
direct contact with the sick or dying birds, but she played and slept in the area under the elevated
house, where the chickens were also often present. The aunt buried the last five chickens on August
29 or 30, using plastic bags on her hands for protection. None of the three patients or other members
of the household had any recognized exposure to poultry from the time these chickens were buried
through the end of September.
From the time the index patient became ill until the arrival of her mother at the hospital, the aunt
provided much of her care, including bedside care for 12 or 13 hours on September 7. The girl's
mother lived in a Bangkok suburb with her husband, but they drove to the province (a four-hour trip)
on learning of her daughter's hospitalization. They stopped at the household for less than 10 minutes
to pick up a document and arrived at the hospital at about midnight. The mother then provided
bedside care for the next 16 to 18 hours, and nurses later reported that she sat on the bed, hugged
and kissed her daughter, and wiped secretions from her mouth.
After the girl's death, the mother and aunt went to the grandparents' village, 40 km from their home
village, for the three-night funeral. Poultry in this village had died from avian influenza six months
earlier, and all the remaining poultry in the village and surrounding area had been culled. Therefore,
there was no exposure to live or dead poultry, including raw chicken or eggs, during the course of the
funeral.
After noting fever on September 11, the mother returned to the aunt's village, as did the aunt. The
mother spent one night there and returned to Bangkok the following morning. The mother worked in
a garment factory and lived in a nearby apartment. There were no chickens at the apartment or at the
factory. Her husband and others could recall no exposure to live or dead poultry in the two weeks
preceding her illness. The aunt had had no known exposure to poultry since August 30, when she had
buried the last of the dead chickens. Her husband and the immediate neighbors disinfected the house
after her niece died by cleaning and spraying with a chlorine bleach solution, and they culled and
buried the remaining neighborhood chickens.
Laboratory Data
RT-PCR analysis of an oropharyngeal swab from the aunt indicated that it contained influenza A
nucleoprotein and that the sequence was most closely related to an influenza A (H5N1) virus isolated
from a chicken in Thailand in early 2004. A nasopharyngeal swab from the aunt was also weakly
positive for the influenza A nucleoprotein gene. None of the available specimens yielded
influenzaviruses on tissue culture or egg inoculation.
Serum obtained from the index patient on day 6 of her illness and from the aunt on day 8 of her
illness were negative for antibodies to H5 on micro-neutralization analysis, but a convalescent-phase
specimen obtained from the aunt on day 21 was positive.
Specimens of lung tissue obtained from the mother after her body had been embalmed were positive
for influenza A (H5N1) by RT-PCR in the Siriraj Hospital laboratory and at the CDC. Pathological
findings included diffuse alveolar damage and interstitial pneumonia in the lung; cholestasis,
congestion, and hemophagocytic activity in the liver; and congestion and depletion of lymphoid cells
in the spleen. Immunohistochemical analysis of paraffin-embedded specimens of lung tissue from the
mother revealed influenza-specific staining of multiple epithelial cells, which were sloughed within
the airways (Figure 3Figure 3Specimen of Lung Tissue from the Index Patient's Mother.).
Sequencing of RT-PCR products from the mother and the aunt revealed that all the viral genes were
avian and were closely related to other H5N1 sequences in Thailand (Figure 4Figure 4Phylogenetic
Trees of Partial Sequences of the Hemagglutinin Gene, Showing the Genetic Relatedness of the
Influenza A (H5N1) Virus Associated with Person-to-Person Transmission in the Family Cluster to
Other Recently Isolated Influenza A (H5N1) Viruses.). The receptor-binding site of the encoded
hemagglutinin was similar to those of other H5 hemagglutinins (amino acid positions 91, 130 through
134, 149, 151, 179, 186, 190, 191, and 220 through 225), including amino acid positions 222 and 224
(226 and 228 in the H3 numbering system). These amino acids are important determinants of the
receptor-binding preference (i.e., 2,3-linked vs. 2,6-linked sialic acid)19; the receptor-binding pattern
identified was avian-specific. The virus contained a 20-amino-acid deletion at the stalk of
neuraminidase and the amantadine-resistance mutation in matrix M2, similar to previously described
genotype Z viruses.20 Sequences of the virus from the aunt were more limited because of the small
sample available, but a sequence of 709 bases (nucleotides 480 to 1189) of the hemagglutinin gene
was the same in the viruses from the mother and aunt, except for one synonymous substitution at
nucleotide 936.
Discussion
We believe that the most likely explanation for the family clustering of these three cases of avian
influenza is that the virus was transmitted directly from the infected index patient to her mother and
to her aunt. Person-to-person spread of avian influenza A (H5N1) strains has been the focus of intense
concern. Ongoing surveillance for such an event across Asia has so far yielded no evidence of efficient
person-to-person spread. In this context, it is reassuring that no further transmission of the virus has
been detected and that the available characterization of the virus from this cluster showed no
adaptive change in the receptor-binding site from the avian 2,3-linked pattern toward the 2,6-linked
pattern of the human sialic acid receptor. Furthermore, phylogenetic analysis of all the genomic
segments showed that the H5N1 virus from this family cluster belongs to the prevalent genotype Z
and that there was no reassortment with human influenzaviruses. These findings confirmed that the
virus was not a new variant that has gained the ability to transmit itself from person to person more
efficiently.
Other explanations for this cluster are possible, although we believe they are less likely. The diagnosis
in the index patient could not be confirmed virologically, but the clinical features pneumonia with
lymphopenia and thrombocytopenia and rapid progression to the acute respiratory distress syndrome
and death and the exposure to sick and dying poultry correspond to all the cardinal features of
previously reported cases in humans.11,12 Antibodies to H5 were not detected but would not yet be
expected in serum collected six days after the onset of illness.21 The confirmation that the clinically
similar illnesses that followed in her mother and aunt were caused by influenza A (H5N1) provides
strong support that this pathogen also caused the disease in the girl.
It was fortuitous for the investigation that the mother lived in a distant city, where she had no
exposure to poultry, and traveled to the affected province only to care for her daughter. She had
prolonged, direct, unprotected exposure to her critically ill daughter and had not had known exposure
to poultry or poultry products. Her 10-minute visit to the affected household on September 7 and her
return to that household on September 12, after the onset of her fever, are unlikely sources of her
exposure.
The illness in the aunt also probably resulted from transmission from the index patient. Her last
recognized exposure to poultry was 17 days before the onset of her illness a period that is longer
than the accepted incubation period, which ranges from 2 to 10 days.10-12 She was exposed to the
index patient from the onset of the girl's illness through the first day of her hospitalization. We think
the bedside exposure to the index patient best explains the time and source of infection. It is also
possible that the aunt was infected by the mother (her sister), rather than by the index patient, but
this exposure would have had to have occurred during the first one or two days of the mother's
illness, when she had only mild symptoms.
Direct transmission of avian influenza from person to person has probably occurred before. In
addition to one of the Hong Kong health care workers, who had mild symptoms, and the Vietnamese
family clusters discussed above, there were three probable secondary infections among family
members of poultry workers in an outbreak of conjunctivitis caused by avian influenza A virus
(H7N7).22 Recent experimental infection of cats lends further biologic plausibility to the transmission
of H5N1 among mammals.23 The current family cluster is unique in that the secondary infections
resulted in severe disease and death and in that the epidemiologic circumstances and laboratory
findings made it possible to rule out transmission from poultry. The infection of close contacts with no
further chains of transmission suggests that the virus has not adapted to efficient human spread, but
this should not be a rationale for complacency.
Since the emergence of avian influenza H5N1 virus in 1997, the virus has gone through many
reassortment events, resulting in the emergence of several genotypes. The sequences of the
hemagglutinin and neuraminidase genes in the currently circulating genotype Z viruses differ
significantly from those of the 1997 viruses.20 This finding suggests that the virus may become more
efficient in infecting humans, either by acquiring genetic material from a human influenzavirus
through reassortment or by adapting its receptor-binding site. It has been shown that a single amino
acid substitution at position 226 or 228 of the hemagglutinin gene could change the receptor-binding
preference from avian-specific 2,3-linked sialic acid to human-specific 2,6-linked sialic acid, which is
believed to be a major determinant of the host range of epidemic and epizootic influenza A viruses.19
Although this family cluster was recognized late and partly by chance, the investigation of the cluster
was immediate, specimens were obtained and shared with the World Health Organization network,
the patients were isolated and treated, the contacts were given antiviral prophylaxis, exposed persons
were put under active surveillance, and poultry in the surrounding area were culled. If influenza A
(H5N1) remains endemic for months to years in the eight countries that contain more than 30 percent
of the world's human population, it is likely that such clusters will appear again, and it will be
necessary to investigate each one rapidly and thoroughly to determine whether a critical change in
the virus has occurred.
The 1918 influenza pandemic, also hypothesized to have originated from an animal influenzavirus
adapted to human transmission,24 killed more people in a single year than the epidemic of black
death (now believed to have been bubonic plague, caused by Yersinia pestis) in the Middle Ages killed
in a century. One author has attributed the 1918 death toll in part to the disregard for public health
on the part of a government intently focused on World War I.25 The person-to-person transmission of
one of the most lethal human pathogens in the modern world should serve as a reminder of the
urgent need to prepare for a future influenza pandemic.
Supported by a research grant from the National Center for Genetic Engineering and Biotechnology
for the viral study at Mahidol University.
We are indebted to Dr. Kamchai Rangsimunpaiboon (Kamphang Phet Provincial Hospital) and Dr.
Taweesak Kanutawong (Khanuvoralukburi Hospital) for care provided to the patients; to Dr. Krit
Nurak and the staff of the Thai Field Epidemiology Training Program; to Dr. Wirat Puthimathee,
Hatairat Suntornsuk, Lalida Jamjumras, and Nongnuan Poolkesorn (Kamphang Phet Provincial Health
Office), for assistance with our field investigation and with the follow-up of contacts; to the dedicated
laboratory staff of the Thai National Health Institute and of the CDC, including Drs. Alexander Klimov,
Ruben Donis, Jacqueline Katz, Iain Stephenson, Michael Shaw, Stephen Lindstrom, Rick Bright,
Catherine Smith, Amanda Balish, Jeannette Guarner, Wun-Ju Shieh, and Chris Paddock; to the
governor and staff of the Kampang Phet Livestock Development for poultry culling; to the staff of the
World Health Organization in Thailand and in Geneva for timely technical support; to Drs. Jaran
Tinwutthipongse, Tawat Suntarajarn, Kitti Kittiampon, and Paijitr Warachit for policy support; to Dr.
Suchai Charoenrattanakul, Deputy Minister of Health, for his encouragement of the sharing of this
investigation with the academic community; and to H.E. Sudarat Keyuraphan for her strong political
commitment to the control of avian influenza.
Source Information
From the Bureau of Epidemiology (K.U., C.P.), the Departments of Medical Sciences (R. Kitphati, W.A.,
P.T., M.C.) and Disease Control (S.C.), and the Kamphang Phet Hospital (R. Khontong), Thai Ministry of
Public Health, Nonthaburi, Thailand; the Faculty of Medicine, Siriraj Hospital, Mahidol University,
Bangkok, Thailand (P.A., P.P., M.U., K.B.); the International Emerging Infections Program, Thai
Ministry of Public Health and U.S. Centers for Disease Control and Prevention, Nonthaburi, Thailand
(S.F.D., J.M.S.); and the Centers for Disease Control and Prevention, Atlanta (N.J.C., S.R.Z.).
Address reprint requests to Dr. Ungchusak at the Bureau of Epidemiology, Department of Disease
Control, Ministry of Public Health, Tivanon Rd., Nonthaburi 11000, Thailand, or at
kum@health.moph.go.th.
KASUS DIARE
Case 19-2011 A 4-Year-Old Haitian Boy with Vomiting and Diarrhea
Jason B. Harris, M.D., M.P.H., Louise C. Ivers, M.D., and Mary Jane Ferraro, Ph.D., M.P.H.
N Engl J Med 2011; 364:2452-2461June 23, 2011
ArticleReferencesCiting Articles (1)
Presentation of Case
Dr. Ana A. Weil (Medicine): A 4-year-old Haitian boy was admitted to a hospital in Haiti affiliated with
this hospital because of vomiting and diarrhea of 10 hours' duration.
The patient had been well until approximately midnight the night before admission, when vomiting
and diarrhea developed. After approximately 6 hours of symptoms, his parents brought him to the
hospital by motorcycle taxi, traveling for 4 hours. On arrival, 10 hours after the onset of symptoms,
episodes of vomiting and diarrhea were too numerous to count.
The patient's parents said that he had not urinated for hours. He had reportedly previously been
healthy. He lived in a small village in Haiti with his parents and sibling. His 8-year-old brother had had
mild diarrhea the previous day.
On examination, the patient seemed irritable and was rapidly drinking offered liquids. The pulse was
low volume, at a rate of 150 beats per minute; the respirations were shallow, without retractions, at a
rate of 45 breaths per minute; and the skin was not hot to the touch. The blood pressure and
temperature were not obtained because of lack of equipment. The weight was estimated at 15 kg.
The eyes were sunken, skin recoil was less than 1 second but not instantaneous, capillary refill was 2
seconds, and the skin and mucous membranes were dry. The lungs were clear, and there was mild
abdominal tenderness. During the examination, the patient passed a clear, watery stool. He was
admitted to the hospital, where he shared a cot with a pediatric patient who had similar symptoms,
including diarrhea.
A reduced-osmolarity oral rehydration solution (ORS) consisting of glucose, sodium chloride,
potassium chloride, and trisodium citrate dihydrate (with 75 mmol of glucose per liter, 75 mmol of
sodium per liter, 20 mmol of potassium per liter, 65 mmol of chloride per liter, and 10 mmol of citrate
per liter), with a total osmolarity of 245 mmol per liter, was administered. During the next hour, two
episodes of vomiting and numerous episodes of diarrhea occurred.
On reexamination 1 hour after the initiation of treatment, the patient had ingested less than 200 ml.
He was combative and pushed away the ORS. The pulse was weak, and the hands and feet were cool
and clammy. Simultaneous attempts at insertion of intravenous catheters in the antecubital region
and the hand were unsuccessful; the patient became increasingly obtunded.
On the third attempt at intravenous access, a catheter was inserted into the saphenous vein of the
foot. A bolus (500 ml) of isotonic crystalloid solution containing sodium chloride, sodium lactate,
potassium chloride, and calcium chloride was administered, with manual pressure applied to the bag.
The patient remained lethargic. Dextrose (30 ml of a 20% solution) was administered rapidly into the
intravenous catheter, without improvement in mental status. A second intravenous catheter was
placed in the right antecubital region. Another bolus (500 ml) of crystalloid solution was infused
during a 30-minute period, with improvement in the level of consciousness, followed by a second liter
of the solution during the next 2 hours.
Approximately 4 hours after presentation, episodes of diarrhea were occurring too often to count, the
frequency of vomiting had decreased, and no urine output had occurred. On examination, the patient
was eagerly drinking ORS, and his mental status was markedly improved. The eyes remained sunken,
and skin turgor was slightly decreased from normal. Azithromycin (300 mg) was administered orally.
His family was encouraged to have the patient consume 200 ml of ORS per stool produced. During the
next 4 hours, he had at least six episodes of diarrhea and drank approximately 400 ml of ORS; 1 liter
of the crystalloid solution was administered intravenously. Eight hours after presentation, the total
intravenous intake was 3 liters, or approximately 200 ml per estimated kilogram of body weight. He
had urinated twice. On examination, there were no signs of dehydration, the pulse was 100 beats per
minute, and the respiratory rate was 30 breaths per minute, without rales or cough. During the
remainder of the first day, an additional liter of intravenous solution was administered (a total of 4
liters during 24 hours, or approximately 267 ml per kilogram). Overnight, the frequency of diarrhea
decreased, with an estimated 10 stools and no vomiting. Oral intake included less than 200 ml of ORS
and some broth.
On the morning of the second day, the patient's parents reported that he had cramping in his legs. On
examination, signs of dehydration were present, including sunken eyes and slightly decreased skin
turgor, with mild abdominal distention and tenderness. A bolus (500 ml) of crystalloid was
administered intravenously over a period of 4 hours, and an educator was assigned to assist his
parents in understanding the importance of ORS intake. During the next 4 hours, he consumed
approximately 800 ml of ORS without vomiting. Signs of dehydration resolved, and abdominal
distention decreased. Infusions of intravenous fluid were decreased to minimal flow. His parents were
instructed again to match stool output by administering approximately 200 ml of ORS per stool, and
his diet was increased to include meals of chicken broth and mashed bananas.
During the second night, three episodes of diarrhea occurred, and another episode between 8 a.m.
and 2 p.m. On the third morning, the patient successfully consumed meals of solid food and ORS. He
was discharged after 2.5 days, with instructions to the parents about oral hydration, point-of-use
water sterilization, and hand sanitation with soap. One week after discharge, a diagnostic test result
was received.
Differential Diagnosis
Dr. Jason B. Harris: I participated in the care of this child who presented with acute watery diarrhea
during the second week of a cholera epidemic in Haiti, which began in October 2010 and is ongoing.
The patient was admitted to a cholera treatment center that was established the previous week and
was providing care for more than 100 patients daily who had diarrhea and, in many cases, other
concomitant illnesses. No laboratory facilities were available. Like the vast majority of patients with
diarrhea in developing countries, no specific laboratory diagnosis was made in this case.
The patient presented with a common problem. Children in developing countries have a median of
three episodes of diarrhea annually,1 and diarrheal illness is the second leading cause of death among
children, resulting in 1.6 million to 2.1 million deaths annually.2 Before the recent cholera epidemic,
an average of 1 of every 93 children born in Haiti died from diarrheal illness before reaching their fifth
birthday.3 For this child, the focus is on empirical management of the acute watery diarrhea, not on
extensive clinical or laboratory investigations. Algorithms, such as those developed by the World
Health Organization (WHO),4 are helpful in managing diarrheal illness in children in resource-limited
communities.
Differential Diagnosis of Diarrheal Illness
The first step in the care of this patient is to classify the type of diarrheal illness (Table 1Table
1Classification and Common Causes of Childhood Diarrhea in Developing Countries.). Diarrhea lasting
for more than 14 days is classified as persistent diarrhea. Persistent diarrhea is caused by a distinct set
of organisms and is associated with malnutrition and chronic enteropathy. Persistent diarrhea should
raise suspicion for underlying infection with the human immunodeficiency virus (HIV); in HIV-infected
persons, unexplained persistent diarrhea is a defining illness of the acquired immunodeficiency
syndrome.5
Since our patient had acute diarrhea, the next step is to classify the diarrhea as invasive (bloody) or
noninvasive (watery). Invasive diarrhea is defined by grossly bloody or melanotic stools. Most
patients with invasive diarrhea have fever and mucus in the stool. Shigella species are the
predominant cause of invasive diarrheal illness in children in developing countries,6,7 and empirical
management of the illness should include antibiotics aimed at treating and preventing complications
of shigellosis.
This child passed watery stools without blood and did not have a tactile fever. The most common
causes of acute watery diarrhea are rotavirus in infants and enterotoxigenic Escherichia coli in
children.6 There is increasing recognition of the role of caliciviruses in causing gastroenteritis in
children and also in adults. Many acute systemic illnesses (e.g., measles, dengue fever, and malaria)
may also present with diarrhea.
Cholera
In this case, cholera was suspected because the patient presented during a known epidemic. It is
important to distinguish cholera from the other causes of noninvasive diarrhea. A rapid and simple
laboratory test for Vibrio cholerae is dark-field microscopy, which, when positive, reveals
characteristically darting bacteria. However, in resource-limited communities, the diagnosis of cholera
is most often based on clinical suspicion that takes into account the local epidemiology of diarrheal
illness. Although mild illness caused by V. cholerae is clinically indistinguishable from other causes of
diarrhea, severe cholera is associated with greater losses of fluid and electrolytes than is seen with
other causes of noninvasive diarrhea. Furthermore, patients with cholera benefit from the early
administration of appropriate antibiotics. Finally, cholera can cause large epidemics.
A classic finding in cholera is rice water stool (Figure 1DFigure 1Pathogenesis of Cholera.), which
may contain more than 1 billion (109) organisms per milliliter. Patients with severe cholera may shed
more than 10 trillion (1013) organisms per day.8 Although many V. cholerae serogroups have been
identified in the environment, only serogroups O1 and O139 have caused epidemic cholera. V.
cholerae O1, biotype El Tor, is the cause of the current global pandemic of cholera, which began in
1961. Emerging strains, termed hybrid or variant V. cholerae O1 El Tor, are the causes of more
recent epidemics, including the current epidemic in Haiti.9 These variant strains appear to combine
the enhanced ability of the El Tor biotype to persist in the environment with the greater virulence
associated with the previously circulating classical biotype.
This case illustrates the manifestations of severe cholera, or cholera gravis. Epidemic strains of V.
cholerae produce cholera toxin a toxin resulting from the ribosylation of adenosine diphosphate
which causes chloride secretion and the loss of sodium and water into the lumen of the small
intestine (Figure 1C). Stool losses in cholera are typically isotonic, and the mean sodium concentration
in the stool of children with cholera is double that seen in the diarrhea of children without cholera
(Table 2Table 2Chemical Composition of Diarrheal Stool and Therapeutic Solutions.).
Dehydration and Rehydration
In cases of rapid fluid losses, the large intestine's capacity for reabsorption is overwhelmed and death
may occur within hours. The WHO has provided guidelines for using the physical examination to
estimate dehydration in children; laboratory tests provide little additional useful information.4 This
patient had deeply sunken eyes, markedly decreased skin turgor, a weak pulse, and mental-status
changes, suggesting a 10% loss of fluid per kilogram of body weight within 12 hours after the onset of
symptoms. This is typical of severe cholera. During the first weeks of the cholera epidemic in Haiti,
deaths occurred in the community a median of 12 hours after the onset of symptoms.11 Children with
severe cholera typically present with 5 to 10% dehydration but have additional stool losses that may
exceed 20% of their body weight during the first 48 hours after admission.12 Rehydration is the
cornerstone of care for patients with cholera, but nutritional interventions, the appropriate use of
antibiotics, and recognition of common complications and coexisting conditions are also important.
Rehydration requires the rapid replacement of the initial deficit and ongoing losses with isotonic
fluids. Therapeutic fluids for patients with cholera are shown in Table 2. In the United States and
other developed countries, a typical approach to a child with dehydration is to use hypotonic
solutions to replace estimated fluid and electrolyte deficits slowly over a 24-hour period. In resource-
limited locations such as Haiti, children with diarrheal illness often present later, with more severe
dehydration, and require more rapid rehydration with isotonic solutions, particularly patients with
cholera. With optimal fluid management, the mortality associated with severe cholera is less than
0.2%.10 However, case fatality rates are usually higher in epidemic cholera,13 especially during the
early stages, when there are obstacles to providing appropriate clinical care.14 This case illustrates
some of the barriers to providing optimal rehydration therapy. Ideally, oral rehydration therapy is
initiated at the onset of illness, in the home or in the community.4 This requires the local availability,
knowledge, and acceptance of oral rehydration therapy. In this case, had ORS been used at the onset
of illness, instead of 10 hours after the onset of symptoms, it is unlikely that life-threatening shock
would have occurred during the patient's hospitalization.
For patients with severe dehydration, intravenous fluids are required immediately. Lactated Ringer's
solution is the best and most widely available commercial intravenous fluid for cholera. Ideally, the
entire fluid deficit should be replaced within 3 to 4 hours after the initiation of therapy in both
children and adults.4,15 This patient required more than 300 ml per kilogram of isotonic intravenous
and oral fluids to restore euvolemia during the first 28 hours of therapy, which is indicative of a rate
of purging that is consistent with severe cholera.
Providing adequate volumes of isotonic fluids to patients with such massive ongoing losses is also a
challenge, especially for health care workers who are unfamiliar with the fluid requirements of
patients with severe cholera. Cholera cots were assembled at this cholera treatment center and
generally are useful for recording stool output (Figure 2Figure 2Cholera Cot.). Because of space
constraints, this patient shared a cholera cot and bucket with other patients; therefore, a reliable
record of the patient's stool output was not made. However, ongoing losses can be estimated at 10 to
20 ml per kilogram per stool, and the volume of these losses can be added to the amount of fluids
needed during the initial rehydration period. In this case, euvolemia was initially restored after 8
hours and approximately 200 ml per estimated weight in kilograms; however, had such rapid ongoing
losses been factored in, the fluid could have been restored more rapidly, ideally within a 3-to-4-hour
window.
Recurrent dehydration, leg cramps, and abdominal distention developed in this patient approximately
12 hours after the initial correction of his fluid deficit. Hypokalemia was the most likely cause of the
leg cramps and abdominal distention. Hypokalemia is an important cause of death in patients with
diarrheal illness who die after initial rehydration therapy.16 In this case, the hypokalemia and the
recurrent dehydration might have been prevented if oral rehydration therapy had been used to
replace ongoing diarrheal losses. Oral rehydration therapy provides more potassium than intravenous
lactated Ringer's solution and is preferred over intravenous therapy whenever possible. Similarly, the
resumption of normal feeding should also begin as soon as possible, to prevent the sequelae of
malnutrition and such complications as hypokalemia and hypoglycemia.
Antibiotic Therapy
This patient received azithromycin early during his hospitalization, which is an appropriate treatment
for the V. cholerae strain that is circulating in Haiti. Antibiotics can lead to reductions of more than
50% in stool volume and in the duration of diarrhea, from more than 4 days to 2 days. Antibiotics also
reduce the shedding of viable V. cholerae from more than 6 days to slightly more than 1 day. This
treatment can be useful on a patient-by-patient basis and also facilitates more rapid discharge from
cholera treatment centers, thus conserving resources for other patients.17
After rehydration and antibiotic therapy, the next tier of care is to provide nutritional support and to
recognize common complications and coexisting conditions seen in patients with cholera. Zinc
supplementation (10 mg per day for infants less than 6 months of age and 20 mg per day for 10 days
for children 6 months to 5 years of age) should be provided to reduce the severity and duration of
childhood diarrheal illness in countries, such as Haiti, where zinc deficiency is common.4,18 Zinc has
the added benefit of reducing the incidence of subsequent episodes of diarrhea for several months. In
developing countries, children with diarrhea, such as this patient, are also at high risk for vitamin A
deficiency and should receive supplementation with vitamin A. Patients with clinical signs of vitamin A
deficiency should receive a three-dose series of treatment (50,000 IU for infants <6 months of age,
100,000 IU for infants 6 to 12 months of age, and 200,000 IU for children >12 months of age). In this
case, neither zinc nor vitamin A was available. In endemic areas, coexisting conditions, such as
pneumonia and sepsis, are a leading cause of death in patients with cholera.19 Therefore,
reevaluation for clinical signs of pneumonia and sepsis after rehydration is important. In this case no
such conditions were identified on sequential examinations after rehydration.
Dr. Jason B. Harris's Diagnosis
Life-threatening diarrheal illness due to Vibrio cholerae.
Pathological Discussion
Dr. Mary Jane Ferraro: The specimen that we received in the laboratory was from a different child in
Haiti who had a similar illness at the same time as this child's illness. The isolate that we obtained was
identified in our laboratory as V. cholerae. Susceptibility testing was performed and showed that the
isolate was susceptible to tetracycline and azithromycin and was resistant to sulfa drugs and nalidixic
acid. This isolate is undoubtedly the same one that had infected our patient, and this result confirms
the diagnosis of cholera. Dr. Harris, can you tell us about the additional molecular characterization
that was performed on this isolate?
Dr. Harris: At the onset of the epidemic, the initial isolates were rapidly identified as V. cholerae O1,
serotype Ogawa, by the National Public Health Laboratory in Haiti. The Centers for Disease Control
and Prevention (CDC) subsequently reported that these were hybrid strains of V. cholerae O1, biotype
El Tor.9 These are strains that produce the more virulent toxin that is associated with the previously
circulating classical biotype of cholera. To determine the phylogeny of the organism, the isolate that
Dr. Ferraro described underwent complete genome sequencing. Analysis of variable regions in the
organism's genome placed the isolate in the context of other known isolates in V. cholerae and
showed that this was a seventh pandemic strain of V. cholerae O1 El Tor and that it was most closely
related to isolates obtained in Bangladesh in the past decade.20 These phylogenetic comparisons
were based on a single nucleotide variation in selected genes and in the content of selected
hypervariable regions in both V. cholerae chromosomes. The isolate was distantly related to strains
that had circulated in South America in the early 1990s and strains that are known to cause sporadic
V. cholerae in the U.S. Gulf Coast.
The Haitian Cholera Outbreak
Dr. Eric S. Rosenberg (Pathology): Dr. Louise Ivers is with us by telephone from Port-au-Prince, Haiti.
Dr. Ivers, would you give us an update on the status of the epidemic there and the responses to the
crisis?
Dr. Louise C. Ivers: This patient presented during the second week of the cholera epidemic in Haiti,
which began in October 2010. We know now that the first cases came from the center of the country,
but the cases that alerted authorities to the epidemic occurred in the large coastal town of Saint-
Marc, 2 hours north of the capital city of Port-au-Prince. At the time of this conference, 4 months
later, the epidemic continued to evolve. As of April 8, 2011, more than 248,657 cases of cholera had
been treated and 4524 patients had died. There continue to be mini-peaks of cases reported,
particularly in areas with poor road access and in rural isolated communities that traditionally have
limited access to any health services. The number of new cases has decreased substantially since the
early phase of the epidemic and now remains relatively stable. Thus, the epidemic has not ended yet,
and as the rainy season approaches, the number of cases may increase.
Sanitation and Clean Water
In Haiti, access to clean water is lacking for the majority of the population, as it most likely was for
this patient's family. Almost a decade ago, Haiti ranked the worst of 147 countries in terms of water
resources, and little has happened since then to substantially improve services and infrastructure.
Few households have access to a formal latrine. Housing and shelter, which were inadequate in rural
Haiti before the earthquake of 2010, became even less sufficient when persons who were displaced
by the earthquake moved to stay with family and friends in already overcrowded and often poorly
constructed housing in the countryside. Many rural homes in Haiti are subject to flooding during the
rainy season, even during moderate rainfall, and most have dirt floors, which increase the challenges
of sanitation and hygiene.
Response to the Outbreak
The outbreak of cholera, the likes of which had never been seen by the current population of Haiti,
caused huge pressure on what was already a weak public health infrastructure. Initially, the causes
and methods of transmission of cholera were poorly understood by those at risk, and clean water and
soap were not widely available in the areas affected; these two issues in the context of poor access to
services led to high initial mortality rates. This patient exemplifies this problem: he did not have
access to oral rehydration early enough to prevent severe complications. The learning curve for
institutions and providers with no cholera experience was steep. In view of these challenges, the
response to the outbreak was relatively fast. Cholera treatment centers were erected, and efforts
were made to establish temporary solutions to the problem of the lack of potable water and to
introduce hygiene measures. There has been a strong response from the government of Haiti and
national and international partners, and there are now more than 400 cholera treatment facilities,
such as the one that this patient entered and that saved his life.
As the months have passed, the training of service providers, access to services for patients, water-
treatment education and supplies, and education in the community have all increased, contributing to
increased survival and a reduction in the number of new cases of cholera. Institutional mortality
nationwide, originally as high as 7 or 8%, has fallen to less than 2%. This patient's family was given
instructions in water purification and hand hygiene at the time of the patient's discharge. They were
also given supplies so they could put their education into practice. However, challenges remain. Rural
isolated communities have poor access to health services in general; poor living conditions, lack of
sanitation, and lack of access to clean water persist as a result of dire poverty.
Dr. Rosenberg: What is the likelihood that cholera will be eradicated from Haiti?
Dr. Edward T. Ryan (Infectious Diseases): We have learned from previous cholera outbreaks that once
this organism gets a foothold in the water supply in impoverished areas, it is almost impossible to
eradicate.
Anatomical Diagnosis
Vibrio cholerae O1 (toxigenic), serotype Ogawa (testing performed at the CDC).
This case was presented at the Medicine Grand Rounds, February 17, 2011.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank Dr. Lawrence Ronan for helpful input.
Source Information
From the Departments of Infectious Diseases (J.B.H.) and Pathology and Microbiology (M.J.F.),
Massachusetts General Hospital; the Department of Medicine, Brigham and Women's Hospital (L.C.I.);
and the Departments of Pediatrics (J.B.H.), Medicine (L.C.I.), and Pathology (M.J.F.), Harvard Medical
School all in Boston.
Dengue
Cameron P. Simmons, Ph.D., Jeremy J. Farrar, M.D., Ph.D., Nguyen van Vinh Chau, M.D., Ph.D., and
Bridget Wills, M.D., D.M.
N Engl J Med 2012; 366:1423-1432April 12, 2012
ArticleReferencesCiting Articles (10) Letters
Dengue is a self-limited, systemic viral infection transmitted between humans by mosquitoes. The
rapidly expanding global footprint of dengue is a public health challenge with an economic burden
that is currently unmet by licensed vaccines, specific therapeutic agents, or efficient vector-control
strategies. This review highlights our current understanding of dengue, including its clinical
manifestations, pathogenesis, tests that are used to diagnose it, and its management and prevention.
Determinants of the Current Dengue Pandemic
The global burden of dengue is large; an estimated 50 million infections per year occur across
approximately 100 countries, with potential for further spread (Figure 1Figure 1Global Dengue Risk.).1
Central to the emergence of dengue as a public health problem has been the dispersal of efficient
mosquito vectors across much of the tropical and subtropical world. The primary vector, the urban-
adapted Aedes aegypti mosquito, has become widely distributed across tropical and subtropical
latitudes. It emerged from Africa during the slave trade in the 15th through 19th centuries, spread
into Asia through commercial exchanges in the 18th and 19th centuries, and has spread globally with
the advent of increased travel and trade in the past 50 years.2 In addition, the geographic range of a
secondary vector, A. albopictus, has dramatically expanded in recent years.3 Globalization of trade, in
particular the trade of tires from used vehicles, is thought to explain the dispersal of eggs and
immature forms of these arboviral vectors into new territories.4 Endemicity has also been facilitated
by rapid urbanization in Asia and Latin America, resulting in increased population density with an
abundance of vector-breeding sites within crowded urban communities and the areas surrounding
them. Dengue infections in Africa remain largely unquantified, but recent outbreaks suggest that
substantial parts of the continent may be at risk for increasing dengue transmission. More
surveillance is required to assess the true burden of disease (see the Supplementary Appendix,
available with the full text of this article at NEJM.org).
Vector control, through chemical or biologic targeting of mosquitoes and removal of their breeding
sites, is the mainstay of dengue prevention, but this approach has failed to stop disease transmission
in almost all countries where dengue is endemic. Antigenic diversity of the dengue virus is important,
since the lack of long-term cross-immunity among the four virus types allows for multiple sequential
infections.
Thus, the spread of dengue illustrates how global trade (and the transport of the mosquito vectors),
increasing travel within and between countries (and the movement of viremic people), urban
crowding (which is conducive to multiple infections from an infected mosquito), and ineffective
vector-control strategies have supported a pandemic in the modern era. With the increasingly global
spread of dengue, practicing physicians in temperate North America, Europe, Australia, and Japan are
more likely than ever to see returning travelers with dengue infection. The diagnosis should be
considered in any patient presenting with fever that has developed within 14 days after even a brief
trip to the tropics or subtropics, including those regions where dengue has not traditionally been
considered an endemic disease.5,6
Virologic Features
Dengue is caused by one of four single-stranded, positive-sense RNA viruses (dengue virus type 1
through dengue virus type 4), also referred to as serotypes) of the genus flavivirus (family
Flaviviridae). Infectious virus and the virus-encoded NS1 are present in blood during the acute phase,
and high-level early viremia and NS1 antigenemia have been associated with more severe clinical
presentations.7-9 The detection of NS1 is also the basis for commercial diagnostic assays.10
Dengue viruses exist in two environments: the urban or endemic setting, where humans and
mosquitoes are the only known hosts, and forested areas, where transmission of mosquito-borne
viruses occurs between nonhuman primates and, rarely, from these primates to humans.11 Within
each dengue virus serotype, multiple genotypes comprise phylogenetically related sequences. Subtle
antigenic differences exist between genotypes of the same serotype,12,13 but these may not be
clinically relevant, since human infection with one serotype is believed to confer long-lived serotype-
specific immunity, but only short-lived cross-immunity between serotypes.
The dynamics of dengue viruses within urban and endemic populations are complex, involving the
birth and death of viral lineages.14,16 Although dengue has emerged in multiple new territories over
the past 40 years, the viruses themselves are paradoxically local in their evolutionary histories,
suggesting that the global dispersal of dengue virus has occurred in relatively infrequent jumps,
most likely by the movement of viremic humans to new geographic settings with a suitable vector and
a susceptible population.
Immunopathogenesis
Insights into the pathogenesis of severe dengue are hampered by the lack of an animal model that
accurately recreates the transient capillary permeability syndrome accompanied by a decreasing viral
burden that is seen in patients (Figure 2Figure 2Immunopathogenesis of Severe Dengue in Secondary
Infections.). Epidemiologic studies have identified young age, female sex, high body-mass index, virus
strain, and genetic variants of the human major-histocompatibility-complex class Irelated sequence
B and phospholipase C epsilon 1 genes as risk factors for severe dengue.18-21 Secondary infection, in
the form of two sequential infections by different serotypes, is also an epidemiologic risk factor for
severe disease.17,22,23 Mechanistically, increased risk in secondary infection is thought to be linked
to antibody-dependent enhancement of virus infection in Fc receptorbearing cells and the
generation of a large infected cell mass in vivo.24 A consequence of a large virus-infected cell mass is
a physiological environment in tissues that promotes capillary permeability; however, this hypothesis
is based on temporal associations between immunologic markers and clinical events, without
evidence of a direct, mechanistic link to causation (Figure 2).
Pathophysiology of Endothelial Dysfunction
There is no evidence that the virus infects endothelial cells, and only minor nonspecific changes have
been detected in histopathological studies of the microvasculature.25,26 Although no specific
pathway has been identified linking known immunopathogenic events with definitive effects on
microvascular permeability, thromboregulatory mechanisms, or both, preliminary data suggest that
transient disruption in the function of the endothelial glycocalyx layer occurs.27,28 This layer
functions as a molecular sieve, selectively restricting molecules within plasma according to their size,
charge, and shape. Hypoalbuminemia and proteinuria are observed during dengue infection; proteins
up to and including the size of albumin are preferentially lost; this is consistent with a small but crucial
change in the filtration characteristics of the glycocalyx.29 Both the virus itself and dengue NS1 are
known to adhere to heparan sulfate, a key structural element of the glycocalyx, and increased urinary
heparan sulfate excretion has been detected in children with severe infection.30,31
Differential Diagnosis and Disease Classification
Although most dengue virus infections are asymptomatic, a wide variety of clinical manifestations
may occur, ranging from mild febrile illness to severe and fatal disease.1 The differential diagnosis is
broad and varies as the disease evolves. During the febrile phase, it includes other arboviral infections
as well as measles, rubella, enterovirus infections, adenovirus infections, and influenza. Other
diseases that should be considered as part of the differential diagnosis, depending on the clinical
picture and local disease prevalence, include typhoid, malaria, leptospirosis, viral hepatitis, rickettsial
diseases, and bacterial sepsis.
Patients were previously classified as having either dengue fever or dengue hemorrhagic fever, with
the latter classified as grade 1, 2, 3, or 4. Over a number of years, there was increasing concern
regarding the complexity and usefulness of this classification system. In particular, there was concern
regarding the requirement that all four specific criteria (fever lasting 2 to 7 days, tendency to
hemorrhage evidenced by a positive tourniquet test or spontaneous bleeding, a platelet count of less
than 100109 per liter, and evidence of a plasma leak based on changes in the hematocrit and pleural
effusions) be met to support a diagnosis of dengue hemorrhagic fever such that some patients with
clinically severe disease were categorized inappropriately.32-34 With the recent revision of the World
Health Organization (WHO) dengue classification scheme, patients are now classified as having either
dengue or severe dengue.1,33,35 Patients who recover without major complications are classified as
having dengue, whereas those who have any of the following conditions are designated as having
severe dengue: plasma leakage resulting in shock, accumulation of serosal fluid sufficient to cause
respiratory distress, or both; severe bleeding; and severe organ impairment. It is hoped that this
system will prove more effective for triage and clinical management and will improve the quality of
surveillance and epidemiologic data collected globally. Continued efforts through prospective
multicenter studies are warranted to define the most appropriate classification scheme.
Clinical Manifestations
After an incubation period of 3 to 7 days, symptoms start suddenly and follow three phases an
initial febrile phase, a critical phase around the time of defervescence, and a spontaneous recovery
phase.
Febrile Phase
The initial phase is typically characterized by high temperature (38.5C) accompanied by headache,
vomiting, myalgia, and joint pain, sometimes with a transient macular rash. Children have high fever
but are generally less symptomatic than adults during this phase of the illness. Mild hemorrhagic
manifestations such as petechiae (Figure 3AFigure 3Hemorrhagic Manifestations of Dengue Infection.)
and bruising, particularly at venipuncture sites (Figure 3B), and a palpable liver are commonly noted.
Laboratory findings include mild-to-moderate thrombocytopenia and leukopenia, often with a
moderate elevation of hepatic aminotransferase levels. This phase lasts for 3 to 7 days, after which
most patients recover without complications.
Critical Phase
In a small proportion of patients, typically in children and young adults, a systemic vascular leak
syndrome becomes apparent around the time of defervescence, evidenced by increasing
hemoconcentration, hypoproteinemia, pleural effusions, and ascites. Initially, physiological
compensatory mechanisms are up-regulated in an attempt to maintain adequate circulation to critical
organs, resulting in narrowing of the pulse pressure when loss of plasma volume becomes critical. If
the pulse pressure narrows to 20 mm Hg or less, accompanied by signs of peripheral vascular collapse,
dengue shock syndrome is diagnosed and urgent, although careful, resuscitation is required. Systolic
pressure may remain normal or even elevated at this time, and the patient may appear deceptively
well, but once hypotension develops, systolic pressure decreases rapidly and irreversible shock and
death may follow despite aggressive attempts at resuscitation. During the transition from the febrile
to the critical phase, between days 4 and 7 of the illness, it is crucial for the clinician to be aware of
warning signs that clinically significant vascular leakage may be developing in the patient. These signs
of impending deterioration include persistent vomiting, increasingly severe abdominal pain, tender
hepatomegaly, a high or increasing hematocrit level that is concurrent with a rapid decrease in the
platelet count, serosal effusions, mucosal bleeding, and lethargy or restlessness.
Hemorrhagic manifestations are most common during this critical period. In children, clinically
significant bleeding occurs only rarely, usually in association with profound and prolonged shock.
However, major skin bleeding, mucosal bleeding (gastrointestinal or vaginal), or both may occur in
adults with no obvious precipitating factors and only minor plasma leakage (Figure 3C).36 Moderate-
to-severe thrombocytopenia is common, with nadir platelet counts below 20109 per liter often
observed during the critical phase, followed by rapid improvement during the recovery phase. A
transient increase in the activated partial-thromboplastin time and a decrease in fibrinogen levels are
also frequently noted. However, the coagulation profile is not typical of disseminated intravascular
coagulation, and the underlying mechanisms remain unclear.37-39 Infrequently, other severe
manifestations, including liver failure, myocarditis, and encephalopathy, occur, often with minimal
associated plasma leakage.
Recovery Phase
The altered vascular permeability is short-lived, reverting spontaneously to a normal level after
approximately 48 to 72 hours, and is concurrent with rapid improvement in the patient's symptoms. A
second rash may appear during the recovery phase, ranging from a mild maculopapular rash to a
severe, itchy lesion suggesting leukocytoclastic vasculitis that resolves with desquamation over a
period of 1 to 2 weeks (Figure 3D). Adults may have profound fatigue for several weeks after recovery.
Diagnostic Tests
Laboratory diagnosis of dengue is established directly by detection of viral components in serum or
indirectly by serologic means. The sensitivity of each approach is influenced by the duration of the
patient's illness (Figure 4Figure 4Laboratory Diagnostic Options in a Patient with Suspected Dengue
Infection.).10 During the febrile phase, detection of viral nucleic acid in serum by means of reverse-
transcriptasepolymerase-chain-reaction (RT-PCR) assay or detection of the virus-expressed soluble
nonstructural protein 1 (NS1) by means of enzyme-linked immunosorbent assay (ELISA) or the lateral-
flow rapid test (not currently available in the United States) is sufficient for a confirmatory diagnosis.
For primary infections in persons who have not been infected previously (which is typical in the case
of most travelers), the diagnostic sensitivity of NS1 detection in the febrile phase can exceed 90%, and
antigenemia may persist for several days after the resolution of fever. 40-42 The sensitivity of NS1
detection in the febrile phase is lower in secondary infections (60 to 80%), reflecting an anamnestic
serologic response due to a previous dengue virus or related flavivirus infection.43
Serologic diagnosis of dengue relies on the detection of high levels of serum IgM that bind dengue
virus antigens in an ELISA or a lateral-flow rapid test; IgM can be detected as early as 4 days after the
onset of fever. IgM seroconversion between paired samples is considered a confirmatory finding,
whereas detection of IgM in a single specimen obtained from a patient with a clinical syndrome that is
consistent with dengue is widely used to establish a presumptive diagnosis. Commercially available
IgM tests with acceptable performance characteristics have recently been identified.44 Serologic
diagnosis of dengue can be confounded if the patient has very recently been infected or vaccinated
with an antigenically related flavivirus (e.g., a virus associated with yellow fever or Japanese
encephalitis). In addition, patients with secondary infections mount rapid anamnestic antibody
responses in which dengue virusreactive IgG may predominate over IgM. In clinical settings where
methods of molecular detection (e.g., RT-PCR) are not available, investigation for elevated levels of
dengue virusreactive IgM or soluble NS1 in serum is a pragmatic diagnostic approach in a patient in
whom dengue is suspected.43,45
Management
Currently, no effective antiviral agents to treat dengue infection are available, and treatment remains
supportive, with particular emphasis on careful fluid management. 1 Patients who have no
complications and are able to tolerate oral fluids may remain at home with instructions to return to
the hospital immediately if bleeding or warning signs suggestive of vascular leakage develop.
However, our practice is to evaluate these patients daily in a medical clinic with a complete blood
count to monitor hematocrit and platelet values.
Development of any warning sign indicates the need for hospitalization and close observation, with
judicious use of parenteral fluids in patients with inadequate oral intake or a rapidly increasing
hematocrit. If the condition progresses to the dengue shock syndrome, prompt fluid resuscitation to
restore plasma volume is imperative, followed by ongoing fluid therapy to support the circulation at a
level just sufficient to maintain critical organ perfusion. Isotonic crystalloid solutions should be used,
and isotonic colloid solutions should be reserved for patients presenting with profound shock or those
who do not have a response to initial crystalloid therapy.46 To limit the risk of the development of
fluid overload, parenteral fluid therapy should be kept to the minimum required to maintain
cardiovascular stability until permeability reverts to a normal level.
Blood transfusion can be lifesaving for patients with severe bleeding that compromises cardiovascular
function, but it should be undertaken with care because of the risk of fluid overload. Platelet
concentrates, fresh-frozen plasma, and cryoprecipitate may also be needed depending on the
coagulation profile. However, at present, there is no evidence that prophylactic platelet transfusions
are of any value in patients who do not have clinically significant bleeding, even when
thrombocytopenia is profound.47,48 The use of prophylactic platelet transfusions is increasing in
countries where dengue is endemic, but given the associated clinical risks and the financial costs,
controlled trials need to be performed before this becomes established as the standard of care. In
patients with severe dengue infection, adjuvant therapy, including vasopressor and inotropic
therapies, renal-replacement therapy, and further treatment of organ impairment, may be necessary.
The establishment of a therapeutic pipeline and the design of randomized, controlled trials of drugs
targeting the virus or the immune response are recent developments. Recent trials have assessed
chloroquine,49 oral prednisolone (A Randomized, Placebo-Controlled, Partially Blinded [Drug versus
Placebo] Trial of Early Corticosteroid Therapy in Vietnamese Children and Young Adults with
suspected Dengue Infection; Current Controlled Trials number, ISRCTN39575233), and balapiravir (A
Randomized, Double-Blind, Placebo-Controlled Study to Evaluate the Safety and Efficacy of the
Dengue Virus Polymerase Inhibitor [Balapiravir] in Male Patients with Confirmed Dengue Virus
Infection; ClinicalTrials.gov number, NCT01096576), and further trials of statins and other antiviral
drugs are planned. Currently, there is no evidence in favor of the use of any specific therapeutic agent
for dengue.
Effects on Health Care Systems
Dengue imposes major demands on health care systems. Although severe dengue occurs in only a
small proportion of dengue infections, early identification of high-risk patients is difficult and patients
with uncomplicated infections are frequently hospitalized for observation. Rapid and effective triage
by experienced personnel at the primary health care level, efficient and affordable transportation
systems to facilitate daily clinical assessment, and public education campaigns to increase awareness
of the disease all help to reduce unnecessary admissions. Among hospitalized patients, meticulous
attention to detail is necessary to limit iatrogenic complications, including fluid overload. Ideally,
patients with severe dengue infection should be treated in dedicated high-dependency units where
frequent clinical observations by experienced staff with immediate access to repeated hematocrit
measurements can ensure that fluid therapy is carefully titrated as needed. In such circumstances,
mortality of less than 1% is achievable among patients with shock, and the need for ventilatory
support and intensive care is minimized. Improvements in the early diagnosis and risk prediction of
severe disease are urgently needed, especially in areas with a high case burden, where appropriate
allocation of limited resources is crucial to the outcome. Ongoing research aims to refine the WHO
2009 classification scheme, particularly with regard to warning signs for the development of severe
disease.
New Approaches to Targeting the Vector
New vector-control approaches include the release of genetically modified male mosquitoes that
sterilize the wild-type female population, thereby reducing egg output and the population size of the
next generation that would be available for potential transmission of the dengue virus.50 An
alternative strategy involves embryonic introduction of strains of the obligate intracellular bacterium
wolbachia into A. aegypti. Strikingly, wolbachia-infected A. aegypti are partially resistant to dengue
virus infection51,52 and can invade natural A. aegypti populations,51,53 suggesting the possibility of
induction of widespread biologic resistance to dengue viruses in A. aegypti populations.
Vaccines
The leading dengue vaccine candidate, ChimeriVax (Sanofi Pasteur), is a tetravalent formulation of
attenuated yellow fever 17D vaccine strains expressing the dengue virus prM and E proteins.54 It has
been difficult to develop a vaccine for dengue that is safe and elicits balanced neutralizing antibody
responses to all four serotypes. However, in the past 5 years, remarkable progress has been made,
and multicenter phase 23 clinical trials that are designed to determine the efficacy of this three-dose
vaccine are under way. Data on immunologic correlates of immunity are lacking. Long-term follow-up
of vaccinees will be essential to understand whether waning vaccine-elicited immunity predisposes
recipients to more severe outcomes on subsequent natural infection. Other candidates in early phases
of clinical development include vaccines containing live attenuated dengue viruses and recombinant
subunit vaccines.55
Future Directions
The field of dengue research has been invigorated over the past decade, fueled by the growing
recognition of the burden of disease coupled with the prospect of a dengue vaccine. However, no
vaccine can be an immediate global panacea, and efforts to improve treatment through application of
existing best practices in triage and fluid management, along with efforts to develop new antiviral or
other therapeutic drugs, must continue. Similarly, innovative approaches to preventing transmission
of the virus, such as through modification of mosquito populations, should be fostered. An improved
understanding of the current epidemiology of the disease and the potential for its future spread
would also assist policymakers in allocating resources to combat this global public health challenge.
Dr. Simmons reports that his institution receives consulting fees on his behalf from Unither Virology
and Tibotec and grant support on his behalf from HoffmannLa Roche. No other potential conflict of
interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
Source Information
From the Oxford University Clinical Research Unit and Wellcome Trust Major Overseas Programme
(C.P.S., J.J.F., B.W.), Hospital for Tropical Diseases (N.V.C.), Ho Chi Minh City, Vietnam; and the Centre
for Tropical Medicine, University of Oxford, Churchill Hospital, Oxford, United Kingdom (C.P.S., J.J.F.,
B.W.).
Address reprint requests to Dr. Farrar at the Hospital for Tropical Diseases, Oxford University Clinical
Research Unit, 190 Ben Ham Tu, Quan 5, Ho Chi Minh City, Vietnam, or at jfarrar@oucru.org.
Autoimmune Hepatitis
Edward L. Krawitt, M.D.
N Engl J Med 2006; 354:54-66January 5, 2006
Autoimmune hepatitis is a generally progressive, chronic hepatitis of unknown cause that occurs in
children and adults of all ages. Occasionally, it has a fluctuating course, with periods of increased or
decreased activity. The diagnosis is based on histologic abnormalities, characteristic clinical and
biochemical findings, and abnormal levels of serum globulins, including autoantibodies. Since the first
descriptions of this disorder more than 50 years ago,1 many labels have been applied, but autoimmune
hepatitis has been accepted as the most appropriate and least redundant term.2,3 Variant,
overlapping, or mixed forms of autoimmune hepatitis that share features with other putative
autoimmune liver diseases, primary biliary cirrhosis, and primary sclerosing cholangitis occur as well.
The distinctions among these disorders at present are necessarily descriptive.
It remains important to distinguish autoimmune hepatitis from other forms of chronic hepatitis, because
a high percentage of cases respond to antiinflammatory or immunosuppressive therapy, or both.
Although appropriate management can prolong survival, improve the quality of life, and avoid the need
for liver transplantation, considerable therapeutic challenges remain in the treatment of this disorder.4
Pathogenesis
A conceptual framework for the pathogenesis of autoimmune hepatitis postulates an environmental
agent that triggers a cascade of T-cellmediated events directed at liver antigens in a host genetically
predisposed to this disease, leading to a progressive necroinflammatory and fibrotic process in the liver.
Potential Triggers
The environmental agents assumed to induce autoimmune hepatitis have not been delineated but
include viruses. The finding of molecular mimicry by cross-reactivity between epitopes of viruses and
certain liver antigens adds credence to a hypothesis of virally triggered disease. Because the trigger or
triggers of autoimmune hepatitis may be part of a so-called hit-and-run phenomenon, in which
induction occurs many years before overt autoimmune disease, identifying an infectious agent may
prove impossible. There has been evidence implicating measles virus, hepatitis viruses, cytomegalovirus,
and EpsteinBarr virus as initiators of the disease; the most convincing evidence is related to hepatitis
viruses.5-7
Certain drugs, including oxyphenisatin, methyldopa, nitrofurantoin, diclofenac, interferon, pemoline,
minocycline, and atorvastatin, can induce hepatocellular injury that mimics autoimmune hepatitis.8-12
It has also been suggested that herbal agents such as black cohosh and dai-saiko-to might trigger
autoimmune hepatitis. Whether drugs and herbs unmask or induce autoimmune hepatitis or simply
cause a drug-induced hepatitis with accompanying autoimmune features is unclear. Minocycline10,11
and atorvastatin, which induce other autoimmune syndromes, have been implicated most recently as
potential triggering agents of this disease.
Genetic Susceptibility
Most knowledge concerning the genetics of autoimmune hepatitis comes from studies of the HLA genes
that reside in the major histocompatibility complex (MHC), located on the short arm of chromosome 6.
The MHC is a genetic system with extensive polymorphism. Although multiple genes are probably
involved, HLA genes appear to play the dominant role in a predisposition to autoimmune hepatitis.13,14
Type 1 autoimmune hepatitis, characterized by circulating antinuclear antibodies (ANA), smooth-muscle
antibodies, antiactin antibodies, atypical perinuclear antineutrophilic cytoplasmic antibodies (pANCA),
and autoantibodies against soluble liver antigen and liverpancreas antigen (SLA/LP), is associated with
the HLA-DR3 serotype (found in linkage disequilibrium with HLA-B8 and HLA-A1), particularly among
white patients. There is an association with HLA-DR4 among patients who are HLA-DR3negative. HLA-
DR3associated disease is more common in the early-onset, severe form of autoimmune hepatitis,
which often occurs in girls and young women. In comparison, the association with HLA-DR4 is more
common in adults and may be associated with an increased incidence of extrahepatic manifestations,
milder disease, and a better response to corticosteroid therapy. In Japan, where HLA-DR3 is rare, the
most common associated HLA locus is HLA-DR4.
The results of serotyping studies have been confirmed with the use of genotyping for HLA-DRB, DQA,
and DQB with polymerase-chain-reaction techniques. A high frequency of the HLA-
DRB1*0301DRB3*0101DQAl*0501DQB1*0201 haplotype (the first two elements correspond to the
serologic determinants DR3 and DR52) and the HLA-DRB1*0401 allele have been observed in association
with autoimmune hepatitis. In South American populations, an increased frequency of the HLA-
DRB1*1301 allele was reported,15,16 whereas in Japan, autoimmune hepatitis has been associated with
the DRB1*0405DQB1*0401 haplotype.17 In children, type 1 autoimmune hepatitis is commonly
associated with the HLA-DRB1*03 and HLA-DRB1*13 alleles.
Type 2 autoimmune hepatitis, a rare disorder characterized by antibodies against liverkidney
microsome 1 (LKM-1) and liver cytosol 1 (ALC-1), has been associated with the HLA-DRB1 and HLA-DQB1
alleles.18 HLA-DR2 appears to be protective in white northern Europeans, and a study of white
Argentineans suggested that the HLA-DRB1*1302 allele is protective.14,15
Susceptibility to autoimmune hepatitis has been reported to be associated with tumor necrosis factor
(TNF) genes, the loci of which are in the class III region of the MHC, although this finding has been
disputed.19,20 A polymorphism at position 308 of the TNF- gene has been associated with
susceptibility to type 1 autoimmune hepatitis in both European and North American patients, but it may
simply represent linkage disequilibrium with HLA-DRB1*0301. There were no significant differences in
the response to therapy between those with and those without the 308 polymorphism.19 Furthermore,
this association was not present in Japanese or Brazilian patients with autoimmune hepatitis.17,20
Similar associations of susceptibility with polymorphisms of cytotoxic T-lymphocyte antigen 4 observed
in northern European patients were not seen in Brazilian patients.21,22 Potential associations with loci
in other chromosomes are under investigation.23,24
Mechanisms of Aberrant Autoreactivity
Knowledge concerning autoantigens responsible for initiating the cascades of events in autoimmune
hepatitis is still rudimentary. A leading candidate for many years has been the asialoglycoprotein
receptor, a liver-specific membrane protein with high levels of expression in periportal hepatocytes.
Information based on the identification of SLA/LP autoantibodies and the cloning and characterization of
the SLA/LP antigen, which shares some amino acid sequences with the asialoglycoprotein receptor,
suggests that this 50-kD cytosolic protein may represent a relevant antigen in at least some patients
with type 1 autoimmune hepatitis.25,26
Evidence of an autoimmune process in the type 2 form of the disease is more compelling. The presence
of immunodominant B-cell epitopes of cytochrome P-450 2D6 (CYP2D6) and evidence of cross-reactivity
with homologues of different viruses suggest that relevant antigens exist within CYP2D6.27
The identification of CD4+ regulatory T cells has reinvoked the concept that failure of or escape from
normal suppression of reactivity against the self has an essential role in the development of
autoimmune disease. The hypothesis that this escape phenomenon occurs in autoimmune hepatitis has
remained attractive and is based on early studies of immune regulation.28-31 Recent experimental
evidence suggests that immunoregulatory dysfunction characterized by decreased numbers of
CD4+CD25+ regulatory T cells and decreased levels of scurfin, the protein product of the FOXP3 gene
that is a member of the forkhead family of transcription factors, may occur in autoimmune hepatitis.32
Such observations suggest that a decrease in the number of regulatory T cells and their ability to expand
may lead to autoimmune liver disease.
Clinical Characteristics
Autoimmune hepatitis is more common among women than men, but it occurs globally in children and
adults of both sexes in diverse ethnic groups.16-18,33-41 Since chronic viral hepatitis appears to be very
common, the prevalence of autoimmune hepatitis may be higher than reported because of concomitant
chronic hepatitis C or B or both.38
Presentation
The presentation of autoimmune hepatitis is heterogeneous, and the clinical course may be
characterized by periods of decreased or increased activity; thus, clinical manifestations are variable.
The spectrum of presentation ranges from no symptoms to debilitating symptoms and even fulminant
hepatic failure.
Patients may present with nonspecific symptoms of varying severity, such as fatigue, lethargy, malaise,
anorexia, nausea, abdominal pain, and itching. Arthralgia involving small joints is common. Physical
examination may reveal no abnormalities, but it may also reveal hepatomegaly, splenomegaly, jaundice,
and signs and symptoms of chronic liver disease.
Patients with severe or fulminant symptoms accompanied by profound jaundice and a prolonged
prothrombin time may have aminotransferase levels in the thousands.42 Many patients with an acute
presentation have histologic evidence of chronic disease on liver biopsy, indicating that they probably
have had subclinical disease for a long time. Long periods of subclinical disease may also occur after
presentation.
Autoimmune hepatitis may first become evident during pregnancy or in the early postpartum period.
Furthermore, postpartum exacerbations may occur in patients whose condition improved during
pregnancy.43-45
One clue to diagnosing autoimmune hepatitis is the presence of other diseases with autoimmune
features, commonly thyroiditis, ulcerative colitis, type 1 diabetes, rheumatoid arthritis, and celiac
disease.46,47 Occasionally, circulating antiendomysial antibodies, antigluten antibodies, and antitissue
transglutaminase antibodies may be found in patients with autoimmune hepatitis; this finding generally
reflects the coexistence of celiac sprue and autoimmune hepatitis.
Laboratory Abnormalities
In general, aminotransferase elevations are more striking than abnormalities in bilirubin and alkaline
phosphatase levels in patients with autoimmune hepatitis. Some cases, however, are characterized by
cholestasis, with high levels of conjugated bilirubin and alkaline phosphatase. In such circumstances,
extrahepatic obstruction and cholestatic forms of viral hepatitis, drug-induced disease, primary biliary
cirrhosis, primary sclerosing cholangitis, and variant syndromes must be considered.
One characteristic laboratory feature of autoimmune hepatitis, although not invariant, is a generalized
elevation of serum globulins, in particular, gamma globulin and IgG, which are generally 1.2 to 3.0 times
normal. The characteristic circulating autoantibodies seen in autoimmune hepatitis include ANA,
smooth-muscle antibody, antiactin antibody, SLA/LP autoantibodies, pANCA, antiLKM-1, and antiLC-1.
Antimitochondrial antibodies are sometimes present in patients with autoimmune hepatitis. It should be
noted, however, that autoantibodies are found in various liver diseases, and their presence, by itself, is
not diagnostic of autoimmune hepatitis. There is little evidence that autoantibodies play a part in its
pathogenesis.
Classification and Autoantibodies
Classification of autoimmune hepatitis on the basis of autoantibody patterns has been helpful to
clinicians (Table 1Table 1Classification of Autoimmune Hepatitis.). Although the distinction was initially
based on circulating antibodies alone, other differences have become apparent. The main serologic
markers of type 1 autoimmune hepatitis are ANA and smooth-muscle antibody. Titers of at least 1:80
are generally accepted as positive,3 but results vary, depending on the assays used; lower titers may
signify a positive response in children. Antiactin antibodies are more specific for type 1 autoimmune
hepatitis.48 AntiLKM-1 and antiLC-1 characterize type 2 disease.18,33,34
The identification of other circulating autoantibodies, in particular SLA/LP autoantibodies25,26,49 and
atypical pANCA,50-52 are sometimes helpful in diagnosing type 1 disease. SLA/LP autoantibodies are the
most specific autoantibody identified in type 1 autoimmune hepatitis but is found in only 10 to 30
percent of cases. Atypical pANCA is frequently present, and on rare occasions, it occurs as an isolated
autoantibody.52
AntiLKM-1 and antiLC-1 can occur alone or together in type 2 autoimmune hepatitis.18,33,34,53 Anti
LKM-1, which is directed at CYP2D6, can occur in chronic hepatitis C, though the antibody response to
immunodominant epitopes differs.27 AntiLC-1 generally occurs in conjunction with antiLKM-1, but it
may be the sole autoantibody.34 It recognizes formiminotransferase cyclodeaminase, a liver-specific 58-
kD metabolic enzyme.54
Complications
The complications of autoimmune hepatitis are the same as in any progressive liver disease. Primary
hepatocellular carcinoma is a known consequence of autoimmune hepatitis; in some patients, chronic
hepatitis progresses to cirrhosis and, ultimately, to carcinoma. However, carcinoma occurs in association
with autoimmune hepatitis less frequently than does chronic viral hepatitis.
Histologic Appearance
The histologic appearance of autoimmune hepatitis is the same as that of chronic hepatitis, and
although certain changes are characteristic, no findings are specific for autoimmune hepatitis.55 The
histologic differential diagnosis of chronic hepatitis is provided in Table 2Table 2Histologic Differential
Diagnosis of Chronic Hepatitis.. Advances in virologic studies and refinements in cholangiographic
methods have made it easier to rule out other clinical entities.
Autoimmune hepatitis is generally characterized by a mononuclear-cell infiltrate invading the limiting
plate that is, the sharply demarcated hepatocyte boundary that surrounds the portal triad and
permeates the surrounding parenchyma (periportal infiltrate, also called piecemeal necrosis or interface
hepatitis that progresses to lobular hepatitis). There may be an abundance of plasma cells, a finding that
in the past led to the use of the term plasma-cell hepatitis. Eosinophils are frequently present. The
portal lesion generally spares the biliary tree. Fibrosis is present in all but the mildest forms of
autoimmune hepatitis. In advanced disease, the fibrosis is extensive, and with the distortion of the
hepatic lobule and the appearance of regenerative nodules, it results in cirrhosis.55 Occasionally,
centrizonal lesions occur.42,57
The findings in patients with acute-onset autoimmune hepatitis differ somewhat from those with an
insidious presentation. Patients presenting with fulminant hepatic failure tend to have interface and
lobular hepatitis, lobular disarray, and hepatocyte, central, and submassive necrosis. However, they
have less fibrosis than patients who present with a more chronic course.42 Steatosis occurs in a minority
of patients,55 although nonalcoholic fatty liver disease may occur in conjunction with autoimmune
hepatitis. The various histologic appearances are depicted in Figure 1Figure 1Photomicrographs of Liver-
Biopsy Specimens from Four Patients with Autoimmune Hepatitis..
In patients who have a spontaneous or pharmacologically induced remission, the histologic findings may
revert to normal or inflammation may be confined to portal areas. In this setting, cirrhosis may become
inactive and fibrosis may diminish or disappear.55,59-61
Diagnosis
In the presence of a compatible histologic picture, the diagnosis of autoimmune hepatitis is based on
characteristic clinical and biochemical findings, circulating autoantibodies, and abnormal levels of serum
globulins. Circulating antibodies are absent in about 10 percent of patients. A scoring system proposed
and subsequently revised by the International Autoimmune Hepatitis Group3 to standardize the
diagnosis for clinical trials and population studies has had limited value and may be inaccurate when
applied to individual patients, especially children. Attempts are under way to devise a less complicated
and more accurate system.62
Variant Syndromes
Although we have long known that the clinical, histologic, and serologic profiles of so-called overlap,
mixed, or variant syndromes differ from the classic features of autoimmune hepatitis, primary biliary
cirrhosis, and primary sclerosing cholangitis, no consensus regarding categorization has been reached.
Terms such as overlap syndrome, antimitochondrial-antibodynegative primary biliary cirrhosis,
the hepatic form of primary biliary cirrhosis, autoimmune cholangitis, autoimmune
cholangiopathy, chronic autoimmune cholestasis, immunocholangitis, immune cholangiopathy,
and combined hepatitic/cholestatic syndrome have all been used to describe patients with features of
both autoimmune hepatitis and primary biliary cirrhosis. The presentation of putative coincidental
diseases, consecutive diseases, and evolution from one disease to another have highlighted the
complexity of this issue.56,58,63-66
One approach is to consider the variant syndromes of autoimmune hepatitis and primary biliary cirrhosis
as part of a continuum that extends from classic autoimmune hepatitis to classic primary biliary
cirrhosis. Examination of a biopsy specimen with histologic features of autoimmune hepatitis but
serologic findings characteristic of primary biliary cirrhosis, such as an isolated antimitochondrial
antibody directed toward enzymes in the 2-oxo acid dehydrogenase family, would be indicative of the
overlap syndrome,58 or antimitochondrial-antibodypositive autoimmune hepatitis (Table 3Table
3Characteristics of Autoimmune HepatitisPrimary Biliary Cirrhosis Variant Syndromes.). The clinical
course and response to therapy in this syndrome appear to be identical to those in classic autoimmune
hepatitis.
There is disagreement as to whether the variant most commonly called autoimmune cholangitis56,58
merely represents antimitochondrial-antibodynegative primary biliary cirrhosis (Table 3).
Immunoblotting and enzyme-linked immunosorbent assays for antimitochondrial antibodies and
primary biliary cirrhosisspecific antinuclear antibodies (anti-Sp100 and anti-gp210) have yielded
different autoantibody profiles for the two conditions, underscoring the heterogeneity of these
syndromes.66
Identifying and classifying autoimmune hepatitisprimary sclerosing cholangitis overlap syndromes is
also difficult, particularly in children.53,67-72 Autoimmune sclerosing cholangitis is the term applied
to this disease in affected children and could arguably be applied to that in adults as well. Although
primary sclerosing cholangitis can evolve to autoimmune hepatitis, autoimmune hepatitis more
commonly evolves to autoimmune sclerosing cholangitis.72 Autoimmune sclerosing cholangitis cannot
be diagnosed in the absence of cholangiographic abnormalities. Patients suspected of having
autoimmune hepatitis who also have histologic bile-duct abnormalities, cholestatic laboratory changes
(e.g., elevations of alkaline phosphatase, -glutamyltransferase, or both), pruritus, inflammatory bowel
disease, or loss of response to antiinflammatory or immunosuppressive therapy may have autoimmune
sclerosing cholangitis.
Treatment
In the 1970s, evidence that mercaptopurine and azathioprine were effective in treating autoimmune
diseases, together with controlled studies of corticosteroids, led to the opinion that autoimmune
hepatitis is a treatable disease. Antiinflammatory or immunosuppressive therapy has been a mainstay in
the treatment of both type 1 and type 2 disease. Depending on the definition of a response, therapy is
reported to be successful in 65 to 80 percent of cases, which indicates that a substantial percentage of
patients require therapy beyond standard treatment. Current response rates appear better than those
in early trials, presumably because earlier trials involved more patients with severe disease and
antedated the present ability to test for chronic viral hepatitis B and C. Ten-year survival rates (with the
end point being death or transplantation) among treated patients are now considered to exceed 90
percent; but the 20-year survival rate may be less than 80 percent among patients without cirrhosis and
less than 40 percent among those with cirrhosis at presentation.73 Once the disease is in remission,
maintenance therapy with azathioprine alone is successful in approximately 80 percent of patients.74
Response to treatment is helpful in establishing the diagnosis of autoimmune hepatitis, but the
response rate to standard therapy is not 100 percent. Thus, a lack of response cannot rule out this
diagnosis. Moreover, not all patients receive treatment, and the prescribed doses of prednisone and
azathioprine or mercaptopurine vary. In addition, other diseases, including some variant syndromes,
may respond to corticosteroids.
Progress in the medical management of autoimmune hepatitis has been slow. Considerable challenges
still exist in the areas of initial and maintenance regimens, management of relapse, management of a
lack of response to therapy, drug toxicity and intolerance, noncompliance, and treatment during
pregnancy. Although guidelines for the treatment of autoimmune hepatitis have been published by the
American Association for the Study of Liver Diseases, these are meant to be flexible.75 The
heterogeneity of autoimmune hepatitis underscores the need for individualized therapy in adults and
children.4,75,76
Standard Treatment
Initial treatment with prednisone (or prednisolone) alone or in combination with azathioprine should be
instituted in nearly all patients in whom the histologic findings include interface hepatitis, with or
without fibrosis or cirrhosis. The magnitude of aminotransferase and gamma globulin elevations does
not necessarily correlate with the histologic extent of injury and provides little help with respect to the
initiation of treatment. In patients with only portal inflammation, the decision to treat is often
determined on the basis of the levels of aminotransferase, gamma globulin, or both; the symptoms; or
the combination of levels and symptoms. Asymptomatic patients and those with portal inflammation
without fibrosis may be followed without treatment, but their clinical status, including the findings on
liver biopsy, should be monitored carefully for evidence of progression of disease, since the activity of
autoimmune hepatitis sometimes fluctuates. Initial treatment consists of combination therapy in order
to avoid or mitigate the side effects of corticosteroid treatment. An alternative approach is to wait until
remission is achieved before corticosteroid-sparing treatment with azathioprine or mercaptopurine is
initiated (Table 4Table 4Drugs Used in the Treatment of Autoimmune Hepatitis in Adults and Children.).
Adverse effects or intolerance of azathioprine, mercaptopurine, or both is an issue of particular
concern.79,80 Azathioprine is a prodrug of mercaptopurine. The methylation of mercaptopurine and 6-
thioguanosine 5'-monophosphate is catalyzed by thiopurine methyltransferase, which is encoded by
highly polymorphic genes. Patients who are homozygous for a mutation of thiopurine methyltransferase
associated with low enzyme activity are at high risk for severe complications, including death. Patients
who are heterozygous for a mutation of thiopurine methyltransferase probably are at intermediate risk.
Given these findings, some investigators have suggested performing thiopurine methyltransferase
genotyping before prescribing azathioprine or mercaptopurine. However, some patients who cannot
tolerate azathioprine appear to be able to tolerate mercaptopurine without side effects, indicating that
azathioprine-induced toxicity is not simply due to a deficiency of thiopurine methyltransferase.81
Despite the availability of reliable methods for genoptying thiopurine methyltransferase and
determining levels of mercaptopurine metabolites, their use in the clinical management of autoimmune
hepatitis is not established.79,80
In general, a patient's progress is followed by monitoring levels of serum aminotransferases and
circulating globulins (total or gamma globulin, or both, with or without IgG). The histologic response
typically lags behind the biochemical response, and a clinical remission does not necessarily mean that
there is histologic evidence of resolution. Reasonable intervals for repeated liver biopsy appear to be
one year after levels of aspartate aminotransferase and alanine aminotransferase have become normal
or approximately two years after presentation.
Although some patients remain in remission after drug treatment is withdrawn, most require long-term
maintenance therapy. In general, patients with milder disease have a better response. Adults and
children with cirrhosis at the time of the initial biopsy, particularly children with type 2 disease, rarely
stay in remission when treatment is withdrawn. Thus, lifelong maintenance therapy is generally
indicated in such cases. The wisdom of the administration of azathioprine alone or as a corticosteroid-
sparing agent should be approached by weighing the side effects of long-term corticosteroid use against
those of long-term azathioprine use; patients treated with azathioprine alone frequently have
arthralgia.74
In the presence of severe side effects from the use of corticosteroids, partial control of the autoimmune
hepatitis in patients who have multiple relapses may be preferable and can be achieved with doses of
prednisone lower than conventional doses.82 Some patients remain in remission for months or years
before the disease flares. These patients may not need antiinflammatory therapy for long periods, but
their condition should still be monitored every three to six months, so that therapy can be reinstated if
the disease becomes active.
Other Therapy
Decisions regarding the use of other medications must be based on meager data obtained from case
reports and series of small numbers of patients. Cyclosporine appeared effective in a group of adult
patients who were corticosteroid-resistant.83 A regimen of cyclosporine for six months followed by the
administration of prednisone and azathioprine was reported as successful in inducing remission in
children.78 Limited data are available concerning the use of tacrolimus,84 methotrexate,85,86
cyclophosphamide,87 ursodiol,88 budesonide,77 and mycophenolate mofetil89 (Table 4).
Treatment of Variant Syndromes
No trials have been performed that could provide a basis for the treatment of variant syndromes. The
treatment for antimitochondrial-antibodypositive autoimmune hepatitis is identical to that outlined for
classic autoimmune hepatitis. Reports concerning the effectiveness of corticosteroid therapy in other
autoimmune hepatitisprimary biliary cirrhosis variant syndromes have been conflicting. Although
ursodiol, the mainstay of treatment for primary biliary cirrhosis,90 may reduce levels of liver enzymes, it
is not known whether the drug mitigates the necroinflammatory process or retards the progression of
disease in these variant syndromes.63,65 A therapeutic trial of corticosteroids with or without ursodiol,
especially in patients with few cholestatic features, no or minimal bile-duct changes on biopsy, or both,
may be required before a long-term regimen can be devised.
Limited success has been achieved with variant forms of autoimmune hepatitisprimary sclerosing
cholangitis in adults with use of a regimen combining corticosteroids, azathioprine, and ursodiol.69
Present therapeutic options include immunosuppression, ursodiol, or both, but data regarding efficacy
are conflicting.67-69
Liver Transplantation
Liver transplantation is required in patients who are refractory to or intolerant of immunosuppressive
therapy and in whom end-stage liver disease develops. The survival rate among patients and grafts 5
years after liver transplantation is approximately 80 to 90 percent, the 10-year survival rate is
approximately 75 percent, and the recurrence rate has been reported to be as high as 42 percent.91-95
Histologic evidence of recurrence may precede clinical and biochemical evidence of recurrence.95
Recurrence may be related to the immunosuppressive regimen used after transplantation.
Autoimmune hepatitis has been reported after liver transplantation for other diseases in adults and
children,96-100 although the use of the term in this setting has been questioned. It has been suggested
that alternative nomenclature such as post-transplant immune hepatitis or graft dysfunction
mimicking autoimmune hepatitis may be more appropriate.97 This entity, however, appears to
respond well to corticosteroid treatment, thus avoiding graft rejection and the need for another
transplantation and improving long-term survival.99
Summary
Autoimmune hepatitis is a generally progressive, chronic disease with occasionally fluctuating activity
that occurs worldwide in children and adults. Although the cause of autoimmune hepatitis is unknown,
aberrant autoreactivity is thought to have a role in its pathogenesis. The diagnosis is based on histologic
changes, characteristic clinical and biochemical findings, circulating autoantibodies, and abnormal levels
of serum globulins. Variant forms of autoimmune hepatitis share features with other putative
autoimmune liver diseases, primary biliary cirrhosis, and primary sclerosing cholangitis. Despite its
clinical heterogeneity, autoimmune hepatitis generally responds to antiinflammatory or
immunosuppressive treatment, or both. Lifetime maintenance therapy may be required, especially for
patients with type 2 autoimmune hepatitis and those who have cirrhosis at presentation. Liver
transplantation has been successful in patients who have no response to medical management.
Dr. Krawitt reports having received lecture fees from Axcan Scandipharm. No other potential conflict of
interest relevant to this article was reported.
I am indebted to Dr. Ian Mackay for the education and inspiration provided by his writings and
discussions, to my colleagues Drs. Paul Mayer and Alex John, to Dr. Abdel Elhosseiny for his advice and
expertise preparing the histologic images, and to Ms. Margo Mertz for editorial assistance.
Source Information
From the Department of Medicine, University of Vermont, Burlington; and the Department of Medicine,
Dartmouth College, Hanover, N.H.
Address reprint requests to Dr. Krawitt at the University of Vermont, Given C-246, Burlington, VT 05405-
0068, or at edward.krawitt@uvm.edu.
Pyruvate Kinase Deficiency and Malaria
Kodjo Ayi, Ph.D., Gundula Min-Oo, Ph.D., Lena Serghides, Ph.D., Maryanne Crockett, M.D., Melanie
Kirby-Allen, M.D., Ian Quirt, M.D., Philippe Gros, Ph.D., and Kevin C. Kain, M.D.
N Engl J Med 2008; 358:1805-1810April 24, 2008
AbstractArticleReferencesCiting Articles (29)
.
Malaria is an important parasitic disease in humans, causing an estimated 500 million clinical cases and
more than 1 million deaths annually.1 Disease control has been hampered by drug resistance in
plasmodium parasites and by the lack of an effective vaccine.2,3 A better understanding of the
pathogenesis of malaria, including the identification of innate or adaptive host defense mechanisms
against the blood-stage parasite, may provide new targets for intervention in this disease. Such
mechanisms may be manifested as genetic determinants of susceptibility in areas of endemic disease
and during epidemics and as variations according to strain in mouse models of experimental
infections.4-7
Genetic studies of susceptibility to malaria in a mouse model for the erythroid stage of the disease, with
the use of infection with P. chabaudi, have localized a number of major loci affecting the extent of
parasite replication at the peak of infection. Recombinant congenic mouse strains AcB55 and AcB61 are
very resistant to infection with P. chabaudi; resistance in these strains segregates as a recessive
monogenic trait caused by a mutation (Ile90Asn) in the gene for pyruvate kinase (Pklr).8,9 The purpose
of this study was to determine whether pyruvate kinase deficiency protects humans against malaria and
to elucidate the molecular basis of a putative protective effect.
Pyruvate kinase catalyzes the rate-limiting step of glycolysis, converting phosphoenolpyruvate to
pyruvate with the generation of one molecule of ATP. In the absence of mitochondria (which are lacking
in mature erythrocytes), the enzyme is critical to energy production. Pyruvate kinase deficiency is the
most frequent abnormality of the glycolytic pathway and, together with a deficiency in glucose-6-
phosphate dehydrogenase (G6PD), is the most common cause of nonspherocytic hemolytic anemia.
Pyruvate kinase deficiency is inherited as an autosomal recessive trait and is caused by loss-of-function
mutations in PKLR. The prevalence of homozygous pyruvate kinase deficiency is estimated at 1 case per
20,000 persons; more than 158 mutations have been described.10,11
Methods
Subjects
From January 2006 to June 2007, subjects attending hematology clinics at the Toronto General Hospital
and the Hospital for Sick Children who were identified as having pyruvate kinase deficiency on the basis
of the clinical presentation and the results of an enzyme assay were eligible for enrollment in this study.
Their asymptomatic relatives were also eligible for enrollment. The study was approved by the
institutional review board at each center, and all subjects provided written informed consent.
We ruled out the presence of other hemolytic disorders by hemoglobin electrophoresis and assessment
of the G6PD level. Subjects with homozygous pyruvate kinase deficiency included a 39-year-old man of
Italian ancestry (Subject 1) and two women: 39-year-old Subject 2, also of Italian ancestry, and 19-year-
old Subject 3, of French ancestry. All subjects had nonspherocytic anemia. Subject 3 was transfusion-
dependent, and Subjects 1 and 2 had undergone splenectomy. A blood sample was drawn from Subject
3 before she underwent transfusion. The majority of humans with pyruvate kinase deficiency are
compound heterozygotes with respect to the mutation of PKLR.10,12 The subjects in this study had not
been previously genotyped to determine the genetic basis of their enzyme deficiency.
Identification of PKLR Mutation
Genomic DNA was isolated from the buffy coat of blood samples from subjects with pyruvate kinase
deficiency (case subjects) and persons without pyruvate kinase deficiency (control subjects) with the use
of proteinase K, phenolchloroform extraction, and isopropanol precipitation. DNA (60 ng)
specifically, the 12 coding exons of PKLR, including intronexon junctions was used as a template for
amplication by polymerase chain reaction (PCR), with 22 to 25 cycles at annealing temperatures ranging
from 56 to 58C. PCR products were purified and sequenced with the use of cycle sequencing with
fluorescent nucleotides. Traces were analyzed with the use of BioEdit
(www.mbio.ncsu.edu/BioEdit/bioedit.html), and all mutations were confirmed by sequence analysis.
Parasite Culture
P. falciparum clones ITG and 3D7 (mycoplasma-free) were maintained in continuous culture.13 To assess
parasite invasion and maturation, schizonts from synchronized cultures14 were mixed with erythrocytes
from case subjects and control subjects, as described previously.15 In all samples, invasion of
erythrocytes was assessed at 24 hours, 72 hours, and 120 hours, and maturation was assessed at 48
hours, 96 hours, and 144 hours.
Phagocytosis Assay
Human monocytes were isolated and purified from the peripheral blood of healthy donors, as described
previously.16 Thioglycollate-elicited macrophages were harvested from the peritoneal fluid of C57BL/6
mice.17 A total of 1.5105 cells per well were plated on glass coverslips in 24-well plates and incubated
for 5 days. All washed erythrocytes, including those infected with P. falciparum and those uninfected,
underwent opsonization with 50% fresh autologous serum for 30 minutes at 37C. Erythrocytes were
then washed twice, resuspended at 10% hematocrit, and incubated with macrophages adhered to glass
coverslips at a target-to-effector ratio of approximately 40:1. Phagocytosis assays were performed and
assessed as described previously.18 All experiments were performed in duplicate and repeated at least
three times.
Erythrocyte Membrane Analysis
Bound hemichromes, IgG, and C3c fragments were measured as described previously.15,18 For ring-
stage infected erythrocytes, the values were normalized to 100% parasitemia with the use of the
following formula: I=(TotNn)(1n), as described previously,15 in which I indicates the amount of
bound IgG and C3c in 100% rings; Tot, the amount of bound IgG and C3c in the whole culture; N, the
amount of bound IgG and C3c in erythrocytes without parasites; and n, the fraction of erythrocytes
without parasites. For mature-stage infected erythrocytes, the percentage of parasitemia was 5 to 10%.
Statistical Analysis
We performed comparisons with the use of either Student's t-test (two-tailed) or the MannWhitney
test.
Results
PKLR Mutations
The characteristics of the three subjects with homozygous pyruvate kinase deficiency who presented
with nonspherocytic hemolytic anemia are shown in Table 1Table 1Characteristics of Case Subjects with
PKLR Mutations.. To confirm the diagnosis, we derived genomic DNA from the subjects with pyruvate
kinase deficiency and from their asymptomatic relatives and sequenced all exons and intronexon
junctions of PKLR. We identified a homozygous G-to-A mutation at position 1269 at the 3 end of exon 9
in two related case subjects (Subjects 1 and 2), which has been previously described as a loss-of-function
mutation. It is predicted to cause missplicing of PKLR, resulting in a shortened half-life of the messenger
RNA transcript.10,11 Subject 3 was found to be homozygous for a single-base deletion at nucleotide
position 823 in exon 7 of PKLR, leading to a frameshift and premature termination of the open-reading
frame. The highly deleterious nature of this latter mutation may be responsible for the severe pyruvate
kinase deficiency in Subject 3, who was transfusion-dependent. We also identified asymptomatic
relatives of Subjects 1 and 2 who were heterozygous for the G-to-A mutation at position 1269 (Table 1).
These relatives are designated as Subjects 4 and 5.
Erythrocytes from each of the subjects with a homozygous mutation (Subjects 1, 2, and 3) were infected
in vitro (within 24 hours after collection) with two different P. falciparum isolates, 3D7 and ITG; 3D7 is
sensitive to chloroquine, and ITG is resistant to chloroquine. We initially examined whether P.
falciparum parasites invaded and matured as efficiently in erythrocytes from case subjects as in those
from control (AA) subjects. The results of multiple invasion and maturation assays with erythrocytes
from each subject with a homozygous mutation in PKLR showed a reduction in the invasion of
erythrocytes by P. falciparum parasites during three consecutive growth cycles, as compared with the
invasion of erythrocytes from control subjects (P=0.01, P<0.001, and P<0.001 for the first, second, and
third cycles, respectively) (Figure 1A and 1BFigure 1 Plasmodium falciparum Invasion of Erythrocytes
from Case Subjects and Control Subjects.). Invasion assays that used erythrocytes from subjects carrying
heterozygous mutations in PKLR (Subjects 4 and 5) did not reveal a significant defect in invasion (Figure
1C). For both homozygotes and heterozygotes, no significant differences were observed in intracellular
maturation (from the ring stage to the trophozoite stage) between erythrocytes from case subjects and
those from control subjects (Figure 1A and 1C). These results showed a reduced level of invasion of P.
falciparum in erythrocytes from subjects with homozygous mutations. They also indicated that potential
biochemical differences in the intracellular milieu, including the accumulation of glycolytic metabolic
intermediates, did not cause a difference in parasite growth in erythrocytes between homozygotes and
heterozygotes.
To further test the hypothesis that reduced invasion observed in erythrocytes from subjects with
homozygous mutations is due to reduced fitness of the parasite, including altered development of
merozoites, we examined erythrocyte invasion by merozoites derived from erythrocytes from case
subjects. We observed that merozoites from such erythrocytes had normal levels of invasion and
replication in erythrocytes from control subjects. (For details, see the Methods section and Table 1 of
the Supplementary Appendix, available with the full text of this article at www.nejm.org.) Therefore, the
observed reduction in parasite levels during in vitro cultivation in erythrocytes from case subjects
appeared to be caused by an invasion defect attributable to a property of the erythrocytes.
We examined phagocytic uptake of P. falciparum (ring-stage and mature-stage)infected erythrocytes
from case subjects and control subjects by macrophages derived from human and mouse monocytes
(Figure 2A and 2BFigure 2Phagocytosis of Erythrocytes from Case Subjects and Control Subjects.).
Phagocytosis of ring-stageinfected erythrocytes from case subjects with homozygous mutations
(Subjects 1, 2, and 3) was markedly higher than phagocytosis of parasitemia-matched infected
erythrocytes from control subjects (P<0.001). We also observed significantly enhanced clearance by
macrophages of ring-stageinfected erythrocytes derived from asymptomatic relatives who were
heterozygous for the PKLR mutation (P=0.003) (Figure 2C).
To investigate the mechanistic basis of this difference, we measured the level of deposition of opsonins
and hemichrome associated with the erythrocyte membrane.15 We correlated the enhanced phagocytic
uptake of early-stageinfected erythrocytes from Subjects 1, 2, and 3 with increased levels of
membrane-bound hemichromes (P<0.001), autologous IgG (P<0.001), and complement C3c fragments
(P<0.001), as compared with ring-stageinfected erythrocytes from subjects with wild-type PKLR (Figure
1 of the Supplementary Appendix). In contrast, macrophage uptake of mature-stageinfected
erythrocytes from case subjects did not differ significantly from that of mature-stageinfected wild-type
erythrocytes. At the mature stage of parasite development, erythrocytes from both case subjects and
control subjects displayed marked membrane damage, as evidenced by similar levels of membrane
deposition of complement C3c and IgG and by high and similar phagocytic uptake.
To determine whether macrophage uptake of ring-stageinfected erythrocytes from case subjects was
mediated by IgG or complement, we carried out phagocytosis assays with complement-inactivated
serum and in the presence of Fc-receptor blockade. We found that uptake was predominantly mediated
by complement, since inactivation of complement (in autologous serum) caused a significant decrease in
uptake, whereas Fc-receptor blockade had no significant effect (Figure 1 of the Supplementary
Appendix). As compared with erythrocytes from control subjects, uninfected erythrocytes from case
subjects also had enhanced phagocytic uptake associated with increased deposition of hemichrome,
IgG, and complement C3c, although at markedly lower levels than those in infected erythrocytes from
case subjects. Together, these results showed that erythrocytes from case subjects that were infected
with P. falciparum underwent more extensive phagocytosis than did infected erythrocytes from control
subjects, a process that occurs through a C3c-mediated pathway.
We examined single-nucleotide polymorphisms (SNPs) in PKLR in populations of varying ancestry
(www.HapMap.org), including the Yoruba of Nigeria, where malaria is endemic. We did not observe
differences in the prevalence of these SNPs in the various HapMap populations, although our analysis
was inconclusive because of the relative paucity of informative PKLR SNPs in the HapMap database.
Discussion
We have shown that pyruvate kinase deficiency has a protective effect against replication of the malarial
parasite in human erythrocytes. We have described a dual mechanism for protection against P.
falciparum in pyruvate kinase deficiency that included an invasion defect of erythrocytes from case
subjects (observed in those with a homozygous mutation) and preferential macrophage clearance of
ring-stageinfected erythrocytes from case subjects (observed in both homozygotes and heterozygotes).
The pleiotropic effect of pyruvate kinase deficiency on parasite invasion (reduced) and phagocytosis of
ring-stageinfected erythrocytes (enhanced) may provide protection against clinical malaria either by
causing an overall reduction in the parasite burden or by reducing the number of erythrocytes infected
with parasites in the trophozoite and schizont stages that are available to bind within microvascular
beds of vital organs.19
In light of the poor overall health status and relative rarity of patients with pyruvate kinase deficiency
who have homozygous mutations at PKLR (severe anemia with dependence on transfusion), it is unlikely
that full-fledged pyruvate kinase deficiency is relevant to protection against malaria in the field.
However, heterozygosity for partial or complete loss-of-function alleles or even compound
heterozygosity for mild alleles with appropriate erythropoietic compensation may have little negative
effect on overall fitness (including transmission of mutant alleles), while providing a modest but
significant protective effect against malaria. Although speculative, this situation would be similar to that
proposed for hemoglobinopathies (sickle cell and both -thalassemia and -thalassemia) and G6PD
deficiency, in which similar mechanisms of protection that are associated with increased clearance of
ring-stageinfected erythrocytes have been reported previously.6,15 Such a mechanism would be
manifested as an increase in retention or prevalence of mutant PKLR alleles in regions where malaria is
endemic, a hypothesis that can now be formally tested.
Supported by a Team Grant in Malaria (to Drs. Gros and Kain) from the Canadian Institute of Health
Research (CIHR), an operating grant (MT-37121, to Dr. Kain) from the CIHR, and a grant from Genome
Canada through the Ontario Genomics Institute and the CIHR Canada Research Chair (both to Dr. Kain).
No potential conflict of interest relevant to this article was reported.
This article (10.1056/NEJMoa072464) was published at www.nejm.org on April 16, 2008.
Source Information
From the McLaughlinRotman Centre for Global Health (K.A., L.S., M.C., K.C.K.) and the Department of
Medicine (I.Q., K.C.K.), University Health NetworkToronto General Hospital; Hematological Unit,
Hospital for Sick Children (M.K.-A.); and the McLaughlin Centre for Molecular Medicine, University of
Toronto (K.C.K.) all in Toronto; and the Department of Biochemistry and Centre for the Study of Host
Resistance, McGill University, Montreal (G.M.-O., P.G.).
Address reprint requests to Dr. Gros at the Department of Biochemistry, McGill University, 3655
Promenade Sir William Osler, Rm. 907, Montreal, QC H3G 1Y6, Canada, or at philippe.gros@mcgill.ca.
KASUS MALARIA
Presentation of Case
Dr. Deepa Kumaraiah (Medicine): A 70-year-old woman was admitted to this hospital because of
intermittent fevers of 11 weeks' duration and new-onset back and leg pain.
The patient had reportedly been in her usual health, with diabetes and hypertension, until 11 weeks
earlier when subjective fevers and chills developed shortly after she received pneumococcal and
tetanusdiphtheriapertussis vaccinations; episodic diarrhea began after a course of antibiotics.
Examination of the stool revealed Campylobacter jejuni. No treatment was given; diarrhea and fevers
reportedly resolved. Two weeks before presentation, she began to have low back pain that radiated to
her left thigh. She reported no associated trauma or injury. The pain gradually increased, without
improvement after acetaminophen, and she had difficulty walking. Her family called emergency medical
services personnel. On their arrival, she reported pain at 10 on a scale of 0 to 10, with 10 indicating the
most severe pain. The blood pressure was 140/90 mm Hg, the pulse 76 beats per minute, and the
respiratory rate 24 breaths per minute. She was brought to the emergency department at this hospital.
She reported no weakness, sensory loss, bowel or bladder dysfunction, fever, or chills.
The patient appeared uncomfortable. The temperature was 36.2C, and the lower thoracic spine, the
lumbar spine, and the lumbar paraspinal muscles were tender to palpation; other vital signs and the
remainder of the examination were normal. An electrocardiogram was normal. Radiographs of the
thoracic and lumbosacral spine revealed mild degenerative changes without evidence of fracture,
compression deformity, or subluxation. She was admitted for observation. Ibuprofen, narcotic analgesia,
and diazepam were administered, and physical therapy consultation was obtained. The patient reported
a decrease in the level of pain to 4 out of 10, and she was able to ambulate without assistance.
Oxycodone, ibuprofen, and a muscle relaxant were prescribed, and she was discharged home, with
instructions to follow up with her physician.
During the next 6 days, the pain in the low back increased to 10 of 10 and radiated to both knees.
Approximately 3 days before admission, the temperature rose to 39.4 to 40.6C each afternoon,
associated with chills, sweats, abdominal pain, and decreased appetite. The patient's family took her to
a health center associated with this hospital, where she reported that the fevers were similar to those
she had had in the past in association with malaria. On examination, the temperature was 39.2C, the
blood pressure 184/68 mm Hg, the pulse 102 beats per minute, the respiratory rate 20 breaths per
minute, and the oxygen saturation 99% while she was breathing ambient air. She appeared
uncomfortable lying in bed. There was discomfort in the right lower quadrant, without rebound
tenderness. Urinalysis revealed 50 to 100 white cells per high-power field with few bacteria and
squamous epithelial cells and was otherwise normal. An electrocardiogram was normal. She was
transferred to the emergency department at this hospital.
On arrival, additional history was obtained. The patient reported that her fevers had never completely
resolved since the onset 11 weeks before and were associated with weight loss of 4.5 kg and dysuria
during the previous 2 to 3 months. She had had type 2 (noninsulin-dependent) diabetes mellitus for
more than 10 years, hypertension, hypercholesterolemia, gastroesophageal reflux disease, headaches,
chronic peripheral edema, vitamin D deficiency, osteoarthritis, and exposure to hepatitis B virus. She
had had Helicobacter pylori infection 4 months earlier, which was treated with amoxicillin,
clarithromycin, and omeprazole, and she had had malaria in the past. On initial immigration to this
country 13 years earlier, a tuberculin skin test was positive; she was asymptomatic and reportedly did
not take isoniazid because of her age. Medications included atenolol, lisinopril, metformin, simvastatin,
diazepam, ibuprofen, oxycodone, aspirin, ergocalciferol, and calcium. She had no known allergies. The
patient had been born in East Africa; when she was in her early 50s, she moved to a refugee camp for 5
years and then immigrated to the United States. Approximately 4 years before admission, she moved to
the Middle East, where she consumed unpasteurized camel's milk; she had returned to New England 5
months before admission and lived with relatives. She did not speak English; her relatives interpreted
for her. She did not smoke, drink alcohol, or use illicit drugs. She had no known exposures to ticks, pets,
or sick contacts. Her children were well.
On examination, the temperature was 36.8C and the blood pressure 150/63 mm Hg; other vital signs
were normal. There was tenderness over the lower paraspinal muscles on the right side with palpation,
tenderness at the costovertebral angle bilaterally, and no tenderness in the midline along the length of
the spine. Deep-tendon reflexes and the remainder of the examination, including straight-leg raising,
were normal. Levels of platelets and red-cell indexes were normal, as were serum levels of calcium,
phosphorus, magnesium, total and direct bilirubin, total protein, globulin, lipase, and alkaline
phosphatase and tests of renal function; other results are shown in Table 1Table 1Laboratory Data..
Chest radiographs revealed elevation of the right hemidiaphragm, which was new in comparison with
studies performed 6 days earlier. Morphine and ceftriaxone were administered. The patient was
admitted to this hospital, and respiratory precautions were instituted.
On the first day, the temperature rose to 40.0C and a grade 2/6 systolic murmur was heard at the right
upper sternal border; the examination was otherwise unchanged. Computed tomography (CT) of the
abdomen and pelvis showed degenerative changes of the spine, most prominent at the L5S1 level, and
scattered subcutaneous calcifications in the region of the buttocks but was otherwise normal. T2-
weighted images from a magnetic resonance imaging (MRI) scan of the spine revealed hyperintense
signal and enhancement involving the end plates adjacent to the L5S1 disk space, with fluid in the disk
space, enhancement in the paravertebral soft tissues with probable extension into the ventral epidural
space at this level, and severe right foraminal stenosis with compression of the exiting right L5 nerve
roots. There were also milder degenerative changes at other levels of the lumbar spine. Urine culture
grew few colonies of mixed bacteria, and the administration of antimicrobial agents was stopped.
Examination of thick and thin smears of peripheral blood showed no organisms, and screening tests for
respiratory viruses and antibodies to the human immunodeficiency virus were negative.
On the third day, the temperature rose to 38.2C. Induration at the site of a tuberculin skin test
measured 10 mm in diameter at 48 hours. Three induced-sputum specimens showed no acid-fast bacilli.
CT of the chest revealed multiple noncalcified pulmonary nodules (4 mm in diameter), as well as
calcified subcarinal lymph nodes, features consistent with previous granulomatous infection. A
transthoracic echocardiogram showed no evidence of valvular vegetations. Results of serum protein
electrophoresis and testing for rheumatoid factor were normal; tests for antibodies to hepatitis C virus
were negative, and no Bence Jones proteins were detected in the urine. An interferon-release assay
(IGRA), a test to detect the release of interferon- in response to Mycobacterium tuberculosis antigen,
was negative.
On the fifth day, a diagnostic result was received.
Differential Diagnosis
Dr. Mark S. Drapkin: Thirty-nine years ago, when I was in training at this institution, a fellow senior
resident admonished, Never fall in love with a diagnosis. I fear that as I thought about this case, I fell in
love with a diagnosis. Even as I've reread the case history many times, I confess that I cannot get that
diagnosis out of my mind. But, as we shall see, I am no longer so sure, which is probably a good thing.
Dr. Kamath, may we see the imaging studies?
Dr. Ravi S. Kamath: Radiographs of the thoracic and lumbar spine obtained during the patient's initial
visit to the emergency department showed multilevel degenerative changes, most pronounced at the
L5S1 level, including disk-space narrowing, end-plate sclerosis, and large marginal osteophytes;
however, no cortical erosion is seen along the adjacent end plates (Figure 1AFigure 1Imaging Studies.).
A chest radiograph was unremarkable. After the patient was admitted to this hospital, a CT scan of the
abdomen and pelvis showed no evidence of infection. Evaluation of the spine showed disk-space
narrowing and end-plate degenerative changes at the L5S1 level. Thickening of the anterior epidural
space was noted at that level, a finding that can be seen with conventional degenerative disk disease
(Figure 1B).
The patient then underwent MRI of the lumbar spine with the administration of gadolinium; this
revealed hypointensity on T1-weighted images, hyperintensity on T2-weighted images, and
enhancement within the vertebral bodies adjacent to the L5S1 disk space (Figure 1C, 1D, and 1E). Also,
fluid was noted in the disk space. The anterior epidural space appears thickened at that level, with
hyperintensity on T2-weighted images and enhancement in the epidural space adjacent to the L5 and S1
vertebral bodies. Mild soft-tissue edema and enhancement were also seen anterior to the L5 and S1
vertebral bodies. As noted on the previous radiographs and CT scans, the patient had large
circumferential osteophytes arising from the end plates adjacent to the L5S1 disk space. Of note, the
patient did have other MRI findings that could have contributed to back pain with radicular symptoms,
including a large diskosteophyte complex and facet arthropathy at the L5S1 level that caused bilateral
foraminal narrowing, especially on the right side, with resulting impingement of the L5 nerve roots
(Figure 1F).
The MRI was ordered specifically to address the question of whether the patient might have an infection
in the spine, and on this point there was some disagreement among radiologists involved in the care of
this patient. End-plate changes such as those seen in this patient are common in degenerative disk
disease, and inflammatory changes in the adjacent epidural space and paraspinal soft tissues can also be
seen. The patient did not have the obvious cortical destruction that is typically seen with bacterial
osteomyelitis or diskitis (disk-space infection). Some radiologists thought that infection was unlikely.
Others noted that the fluid in the disk space and the extent of paraspinal inflammation suggested
infection. The findings are equivocal, but I think it would be reasonable to consider infection, particularly
a more indolent or atypical one, as a possibility.
Dr. Drapkin: Could the patient have had a noninfectious illness? Although fever may occur with tumors,
a neoplasm is unlikely to spread between vertebrae and to the disk space and surrounding soft tissue, as
occurred in this patient. A few reports have shown that gout can mimic epidural infection,1-4 but that
process would be more localized. Vasculitis can cause elevated temperatures and levels of inflammatory
markers but not the anatomical abnormalities present in this case. Sarcoidosis can affect lymphatic
tissue and can be present in bone, but I believe the manifestation would be different from the
manifestation of this patient's illness. I cannot see a relationship between the current illness and the
recent immunizations.
Pyogenic Infections
It is likely that the patient has either pyogenic or granulomatous infection. If pyogenic infection (due to,
for example, the most common pathogen, Staphylococcus aureus) had spread as widely as the infection
spread in this case, I would have expected more flagrant clinical signs of systemic inflammatory
response and of local impingement on the spinal cord or nerves than occurred in this patient after an
11-week period. I think pyogenic infection is very unlikely.
This patient has a history of C. jejuni enteritis. There are a few case reports of osteomyelitis due to
campylobacter,5-7 but that organism is common in the intestine and only rarely results in bacteremia or
in secondary hematogenously seeded infection.
Granulomatous Infections
The diagnosis that first appealed to me in this case was tuberculosis. The patient had ample opportunity
to acquire the infection in Africa. She had spent 5 years in a refugee camp, undoubtedly living under
crowded conditions and perhaps with limited access to medical care, conditions associated with a high
risk of the acquisition of tuberculosis.
What about the results of the tuberculin skin test and the IGRA? According to one study, in patients with
active tuberculosis, the sensitivity of an IGRA is approximately 83%, and the sensitivity of a tuberculin
skin test is approximately 89%. 8 In another study, the tuberculin skin test was positive in 95% of
patients, the IGRA in 89%, and either one or the other test in 99%.9 The negative predictive value of an
IGRA has been shown to be 79%.10 This suggests that in patients with active tuberculosis, both an IGRA
and a tuberculin skin test usually, but not always, are positive. Previous immunization with bacille
CalmetteGurin can result in the positive tuberculin skin test and negative IGRA seen in this patient,
but she also had evidence of granulomatous disease on chest imaging, so I think we are compelled to
view the tuberculin skin test as a true positive and the IGRA as a false negative. The sterile pyuria could
be due to concurrent genitourinary tuberculosis. Therefore, tuberculosis remains a very plausible
diagnosis, although there is some diagnostic uncertainty.
A word should be said about the assumption that one can be too old for treatment of latent
tuberculosis. Although adverse reactions to isoniazid occur more frequently as age increases, age alone
is not considered a contraindication to treatment.11
Now we come to the entity that is trying to displace tuberculosis as my preferred diagnosis. The more I
think about this case and pay close attention to time intervals, the more I am drawn to another
organism. First of all, we have the camel's milk. If one does a Google search for camel's milk, 195 of
the first 200 hits extol the nutritional and other putative benefits of that food product. The remaining 5
refer to the potential harm associated with the drinking of unpasteurized camel's milk. When one
searches PubMed using the same search terms, however, one encounters brucellosis in the second
citation. Could our patient have acquired brucellosis from drinking unpasteurized camel's milk?
Brucellosis
Brucellosis is common over a wide region, from Iran to Somalia to Tunisia.12 Serologic surveys have
shown that 2 to 15% of camels in this geographic area have antibodies against brucella. 13-16 A recent
report describes brucellosis in two persons returning home to Singapore after drinking unpasteurized
camel's milk during the Hajj pilgrimage.17 In animals in the Middle East, Brucella melitensis (serovar 2 or
3) predominates; in humans, serovar 3 is the cause of most cases.12
How does brucellosis fit with this patient's illness? Fever is the primary symptom of brucellosis, often
with chills; osteoarticular disease is the most common complication when focal infection is diagnosed.
Our patient had both fever and osteoarticular disease. One third of patients with brucellosis have
hepatic or splenic enlargement, and 10% have genitourinary involvement, which may explain our
patient's pyuria.18 Brucellosis often involves the spine19; in children, the sacroiliac joint is most
frequently involved; in older patients, such as this one, spinal infection is most frequent, and 60% of
cases are lumbar, most often at the L4 or L5 level. Radiographic changes may not become apparent until
2 to 8 weeks after symptoms begin, with anterior and superior erosions of the vertebral bodies being
common. Perilesional bone formation at the anterior vertebral end plates can produce a so-called
parrot-beak appearance. Marked destruction of vertebral bodies, usually in the thoracic or
thoracolumbar area, is more common in tuberculosis, whereas disk destruction is seen more often in
brucellosis. I compared the findings in this case with those reported in cases of brucella infection,
tuberculous infection, and pyogenic vertebral infection and found that this patient's signs and symptoms
seem to line up more with brucellosis than with tuberculosis (Table 2Table 2Clinical Signs and Symptoms
of Brucellosis, Tuberculosis, and Pyogenic Infection Involving the Spine.).20
Paravertebral abscesses are less common in brucellosis than in tuberculosis, but they can occur.18 It has
been suggested that the constellation of back pain, elevations in the erythrocyte sedimentation rate and
the level of serum C-reactive protein, a history of previous tuberculosis, and involvement of posterior
spinal elements on imaging is pathognomonic of tuberculosis. 21 On MRI, a well-defined abnormal
paraspinal signal and a thin, smooth abscess wall suggest tuberculous infection.22 In truth, I find it quite
difficult to distinguish among tuberculosis, brucellosis, and pyogenic infection purely on the basis of
imaging.
Could the patient also have endocarditis? She had an outflow murmur, possibly originating at the aortic
valve. This may have been due to increased flow related to fever but also could connote structural
valvular disease. The duration of fever could have indicated prolonged bacteremia. Vegetations were
not revealed on transthoracic echocardiography. However, the sensitivity of transthoracic
echocardiography in detecting infective endocarditis is approximately 60% or 70%, so a normal result
does not rule out infective endocarditis.23 Less than 2% of patients with brucellosis have
endocarditis.18 A transesophageal echocardiogram may help with the diagnosis.23
The incubation period for brucellosis ranges from 1 to 2 weeks for acute disease to months for late
disease. 18 This patient's symptoms started about 2 months after her return from the Middle East.
Diagnosis of brucellosis can prove difficult. In automated blood-culture systems, growth often can be
detected after 3 to 5 days of incubation.18 Laboratory personnel should be alerted to the need to hold
the cultures longer than the customary 5 days and also to take precautions to avoid infection
themselves.24,25 If cultures are negative, a presumptive diagnosis can be made serologically, although
seropositivity can derive from previous infection and not necessarily indicate active infection, especially
in people who have resided in endemic regions. 18
The diagnostic test is most likely a blood culture that yielded growth of brucella. It is possible that a
serologic test for brucella antibodies was reported as positive, but that would not have been definitive.
If I am wrong about brucella, I suspect that tuberculosis is the next most likely diagnosis.
If the patient had been shown to have brucellosis, I would have prescribed initial treatment with
doxycycline and streptomycin, perhaps followed by prolonged oral therapy with doxycycline and
rifampin. If endocarditis had been shown, I would have sought cardiothoracic surgical consultation.
In summary, I initially chose tuberculous spondylitis as the most likely diagnosis; the prominent
paraspinous inflammation points in that direction. However, on reflection, I am willing to abandon that
diagnosis in favor of a much less common one brucellosis because it seems to be the best fit on the
basis of the information we are given.
Dr. Eric S. Rosenberg (Pathology): Dr. Calderwood, would you tell us your clinical impression?
Dr. Michael S. Calderwood (Infectious Diseases): We saw this patient on the night of admission. Because
of language difficulties, there was confusion about what countries the patient had recently visited, so
malaria was a consideration. However, a rapid test for malaria was negative.
We focused our thinking on the pyuria in the absence of pyelonephritis on abdominal imaging, the
history of untreated latent tuberculosis, and the consumption of unpasteurized camel's milk.
Tuberculosis was initially high on our list. However, as we considered the patient's consumption of
unpasteurized milk, prolonged fever, and sacroiliac pain, brucellosis became our leading diagnosis.
Because of her new heart murmur, we were also concerned about endocarditis.
Clinical Diagnosis
Brucellosis, most likely involving the spine.
Dr. Mark S. Drapkin's Diagnoses
Spondylitis, associated paraspinous and disk-space infection, and possibly endocarditis, all due to
Brucella melitensis.
Pathological Discussion
Dr. Ji Yeon Kim: The diagnostic result came from three sets of blood-culture bottles for aerobic and
anaerobic bacterial culture. Blood was obtained on hospital day 1 while the patient was in the
emergency department. After 5 days in the automated blood-culture system, all three aerobic bottles
turned positive. Gram's staining showed small, gram-negative coccoid rods, which are characteristic of
B. melitensis (Figure 2AFigure 2Microbiologic Studies.). After 48 hours of incubation, cultures of the
isolate on horse-blood agar and chocolate agar plates showed pinpoint, smooth, translucent,
nonhemolytic colonies (Figure 2B); the organisms were strongly positive for catalase, oxidase, and
urease, findings consistent with brucella species. The isolate was sent to the Massachusetts Department
of Public Health State Laboratory Institute and the Centers for Disease Control and Prevention (CDC),
where extensive biochemical analysis and detection of DNA by real-time polymerase chain reaction
further identified the organism as B. melitensis.
Paired serum samples were also sent to the CDC for brucella microagglutination, which revealed high
total antibody titers indicative of presumptive brucellosis. The temporality of the infection is difficult to
determine because of the delayed presentation.
In summary, the laboratory findings, along with the patient's history of drinking unpasteurized camel
milk and her clinical symptoms, are consistent with the diagnosis of B. melitensis bacteremia and
probable diskitis or osteomyelitis due to brucella.
Dr. Rosenberg: Dr. Calderwood, how did you manage this patient's care?
Dr. Calderwood: There are a number of treatment regimens for brucellosis. We targeted the treatment
to brucella involving the spine. There was ongoing debate as to whether this patient also had
endocarditis and what that would mean for surgical intervention. The patient had a normal
transthoracic echocardiogram and declined a transesophageal echocardiogram. Our initial treatment
regimen included streptomycin (for 2 weeks) and concurrent rifampin and doxycycline.26,27
The question of how long to treat was also discussed. We decided to treat for a total of 6 months. After
2 weeks of streptomycin, the patient had improved dramatically. Therefore, we discontinued
streptomycin after 15 days and continued doxycycline and rifampin for the duration.
When we first saw the patient she was unable to move in bed, let alone get out of bed, and after 2
weeks of treatment, she was mobile. After 1 month of therapy, she no longer had fevers or night
sweats, the anorexia had improved, she was gaining weight, and she was much more mobile. After 5
months of therapy, she did not require any assistive devices and had only minor pain.
Anatomical Diagnosis
Brucella melitensis bacteremia.
This case was presented at Medicine Case Conference.
Dr. Drapkin reports holding stock in Abbott, Merck, MedcoHealth, Forest Laboratories, and Hospira. No
other potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank Dr. John A. Branda for providing representative photographs of brucella species; and the
Massachusetts Department of Public Health State Laboratory Institute and the Centers for Disease
Control and Prevention for definitively identifying B. melitensis and for performing serologic studies for
brucella.
Source Information
From the Infectious Diseases Service, NewtonWellesley Hospital, Newton, MA (M.S.D.); and the
Departments of Radiology (R.S.K.) and Pathology (J.Y.K.), Massachusetts General Hospital; the
Department of Medicine, Tufts University School of Medicine (M.S.D.); and the Departments of
Radiology (R.S.K.) and Pathology (J.Y.K.), Harvard Medical School all in Boston.
You might also like
- Hadist BukhariDocument1 pageHadist BukhariFazmial UjirNo ratings yet
- Hasil Lab HyperkalemiaDocument1 pageHasil Lab HyperkalemiaFazmial UjirNo ratings yet
- Autoimmune HepatitisDocument69 pagesAutoimmune HepatitisFazmial UjirNo ratings yet
- Central Vena KanulasiDocument20 pagesCentral Vena KanulasiFazmial UjirNo ratings yet
- Compartment SyndromeDocument29 pagesCompartment SyndromeFazmial UjirNo ratings yet
- Myasthenia Gravis: Disusun Oleh: Fazmial Rakhmawati 1102009110Document1 pageMyasthenia Gravis: Disusun Oleh: Fazmial Rakhmawati 1102009110Fazmial UjirNo ratings yet
- 45 83 1 SMDocument9 pages45 83 1 SMmrizkidm2301No ratings yet
- Module 7 Compartment Syndrome. Diagnosis and TreatmentDocument6 pagesModule 7 Compartment Syndrome. Diagnosis and TreatmentFazmial UjirNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document1 pageP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Fazmial UjirNo ratings yet
- Dr. Jusi Susilowati, SP - PD Dr. Ariadi Humardhani, SP - PD Dr. Nugroho Budhi Santoso, SP - PDDocument3 pagesDr. Jusi Susilowati, SP - PD Dr. Ariadi Humardhani, SP - PD Dr. Nugroho Budhi Santoso, SP - PDFazmial UjirNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document1 pageP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Fazmial UjirNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)