Professional Documents
Culture Documents
Silicone Granuloma of The Facial Tissues
Uploaded by
entgo8282Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Silicone Granuloma of The Facial Tissues
Uploaded by
entgo8282Copyright:
Available Formats
Vol. 94 No.
1 July 2002
ORAL AND MAXILLOFACIAL PATHOLOGY Editor: Alan R. Gould
Silicone granuloma of the facial tissues: A report of seven cases
Giuseppe Ficarra, MD,
a
Adalberto Mosqueda-Taylor, DDS,
b
and Roman Carlos, DDS,
c
Florence, Italy; Mexico City, Mexico; and Guatemala City, Guatemala
AZIENDA OSPEDALIERA CAREGGI AND UNIVERSITY OF FLORENCE; DEPARTAMENTO DE ATENCION A LA
SALUD, UNIVERSIDAD AUTONOMA METROPOLITANA XOCHIMILCO; AND HOSPITAL HERRERA, LLERANDI/
AMEDESGUA
The liquid form of silicone, called dimethicone (dimethylpolysiloxane), has been used extensively in some
countries during the past 4 decades for soft tissue augmentation. Although considered biologically inert, this material
has been reported as potentially inducing, after tissue injection, a granulomatous inammatory response of variable
severity. Interestingly, a remarkable paucity of reports exists about the development of complications after injections of
liquid silicone into the facial tissues, especially considering its high frequency of use. The purpose of this article is to
describe the clinical and microscopic features of 7 cases of silicone-induced granulomas that developed after injection
of the facial tissues for cosmetic purposes and to discuss the differential diagnosis and management of this condition.
(Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:65-73)
Silicone (polydimethylsiloxane) is a term applied to
certain polymeric organosilicon compounds that may
be in liquid, gel, or solid forms (Table I).
1
The liquid
form, called dimethicone (dimethylpolysiloxane), has
been used extensively in some countries during the past
4 decades for soft tissue augmentation.
1-3
Although
initial studies supported the belief that this material was
biologically inert, subsequent reports have shown that
silicone may induce a granulomatous inammatory re-
sponse of variable severity.
1,4,5
Interestingly, a remark-
able paucity of reports exists about the development of
complications after injections of liquid silicone into the
facial tissues, especially considering its high frequency
of use.
6-14
Development of systemic manifestations,
such as scleroderma, has been reported in patients who
have received silicone implants. However, these cases
remain highly controversial and are still a subject of
debate and litigation.
6,15
The purpose of this article is to
describe the clinical and microscopic features of 7 cases
of silicone-induced granulomas that developed after
injection of the facial tissues for cosmetic purposes and
to discuss the differential diagnosis and management of
this condition.
CASE REPORTS
In Table II, the main clinical characteristics of the 7
patients with silicone granuloma of the facial tissues are
summarized.
Case 1 was presented in part by Dr Giuseppe Ficarra at the Clinico-
Pathological Conference of the 10th Meeting of the International
Association of Oral Pathologists, La Antigua, Guatemala, Sep 17-21,
2000.
a
Adjunct Professor and Director, Section of Oral Pathology and
Medicine, Azienda Ospedaliera Careggi and University of Florence,
Italy.
b
Professor, Department of Oral Pathology and Medicine. Departa-
mento de Atencion a la Salud, Universidad Autonoma Metropolitana
Xochimilco, Mexico City, Mexico.
c
Associate, Department of Pathology. Hospital Herrera, Llerandi/
Amedesgua, Guatemala City, Guatemala.
Received for publication Dec 11, 2001; returned for revision Jan 11,
2002; accepted for publication Feb 15, 2002.
Copyright 2002 by Mosby, Inc.
1079-2104/2002/$35.00 0 7/14/124459
doi:10.1067/moe.2002.124459
Table I. Types of silicone and common applications
Type Applications
Gel Breast implants
Liquid Breast injection (no longer used)
Soft tissue injection (used in some countries
for cosmetic purposes)
Therapeutic embolization
Cardiopulmonary surgery as antifoam agent
Elastomer Breast implants
Heart valves prostheses
Finger joint prostheses
Hemodialysis equipment (tubes)
Modied from Travis WD, Balogh K, and Abraham JL, 1985.
6
o
o
o
ORAL SURGERY
ORAL MEDICINE
ORAL PATHOLOGY
65
Case 1
A 56-year-old Italian woman was seen at our clinic with
redness and swelling of the orofacial soft tissues accompanied
by pain and burning sensation. At the time of the rst visit,
the medical history was negative for relevant systemic dis-
eases and the patient did not declare anything remarkable in
relation to the facial problem. She indicated that the facial
swellings had a 3-year duration and uctuated in size. Clinical
examination showed diffuse swelling of the lower contour of
the face with involvement of the soft tissues overlying the
mandible and both lips (Fig 1). The swelling was accompa-
ined by signs of cellulitis, including redness and warmth, of
the involved areas. On palpation, multiple ill-dened subcu-
taneous masses were appreciated along the inferior border of
the mandible, both extraorally and intraorally. Intraoral ex-
amination revealed a normal appearance of the mucosal sur-
Fig 1. Case 1. Multiple tumefactions are visible on lower contour of face and lips.
Table II. Summary of cases of silicone granuloma of facial tissues
Case
Age/gender/
nationality
Reason for
silicone
injection Anatomic sites Treatment Follow-up result
1 56/female/
Italian
Cosmesis Both lips and soft tissues
of lower contour of face
Anti-
inammatory
drugs; systemic
corticosteroid
3 years; persistent disease
2 34/male/
Italian
Cosmesis Upper lip Excisional biopsy 2 years; resolution
3 50/female/
Mexican
Cosmesis Lower lip and right mental
region
Local injections
of
corticosteroids
2 years; stable disease
4 39/female/
Mexican
Traumatic
deformity of
facial tissues
Lower lip with extension
to labial commissures
Excisional biopsy 3 years; stable disease
5 38/female/
Mexican
Cosmesis Lower lip Excisional biopsy 2 years; resolution
6 52/female/
Guatemalan
Cosmesis Upper lip Excisional biopsy Lost to follow-up
7 77/female/
Guatemalan
Cosmesis Upper lip Excisional biopsy Lost to follow-up
66 Ficarra, Mosqueda-Taylor, and Carlos ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
July 2002
face and presence of ssured tongue. On the basis of the
clinical ndings, a working diagnosis of Melkersson-
Rosenthal syndrome was made. A biopsy specimen was ob-
tained from 1 of the subcutaneous masses in the mandibular
vestibule. Light microscopic examination revealed skeletal
muscle with surrounding connective tissue inltrated by his-
tiocytes and numerous cystic spaces (Fig 2). The cystic spaces
varied somewhat in size and did not appear to contain residual
droplets of silicone (Fig 3). Varying degrees of brosis were
present among the cystic spaces. Special stains, including
periodic acid-Schiff (PAS), oil red O, and alcian blue, were
negative. A nal diagnosis of silicone granuloma was made.
The patient admitted that she had received liquid silicone
injections into the facial soft tissues for cosmetic purposes 10
Fig 2. Case 1. At low magnication, multiple cystic spaces are evident among connective tissue and skeletal muscle bers
(hematoxylin-eosin stain; original magnication, 4).
Fig 3. Case 1. Numerous round to ovoid empty cavities of varying sizes are visible. Fibrosis, histiocytes, and lymphocytes are
present between cavities (hematoxylin-eosin stain; original magnication, 10).
Ficarra, Mosqueda-Taylor, and Carlos 67 ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
Volume 94, Number 1
years previously. The patient then was treated with antiin-
ammatory drugs and systemic corticosteroid (prednisone 60
mg/day), and a partial resolution of symptoms and tumefac-
tion was obtained. After 3 years of follow-up, the patient still
showed persistent disease.
Case 2
A 34-year-old transvestite Italian man had received liquid
silicone injections into the lips 7 years previously for cos-
metic purposes. A recurrent subcutaneous mass subsequently
developed within the right upper lip, accompanied by local
signs of inammation (Fig 4). An excisional biopsy was done
that showed the presence of silicone granuloma, and the
histopathologic aspects were similar to those described in
case 1 (Fig 5). After 2 years of follow-up, no signs of
recurrence were observed.
Case 3
A 50-year-old Mexican woman was seen with an asymp-
tomatic diffuse enlargement of the lower lip that affected the
entire vermilion border, adjacent skin, and the labial mucosa,
extending to the right mental region (Fig 6). On palpation, the
lesion had a homogeneous rubbery consistency. The patient
stated that she had received 2 liquid silicone injections of
unknown medical grade in the lower lip 5 years earlier for
cosmetic purposes, and she indicated that the lesion had been
slowly enlarging during the last 4 years. A biopsy specimen
was obtained, and microscopic examination revealed numer-
ous empty small cystic spaces of varying sizes, surrounded by
histiocytes, which diffusely inltrated the supercial lamina
propria down to underlying adipose tissue and striated mus-
cle. The cystic spaces varied in size and did not stain with
special stains, including PAS, oil red O, and alcian blue.
Foreign body multinucleated giant cells were infrequently
found. The patient was treated with 3 injections of 1 mL of
triamcinolone (10 mg/mL) each, 1 every 10 days, after which
minimal reduction of the lesion was observed. She refused
surgical treatment and is currently asymptomatic, with no
change in size of the lesion over the last 2 years.
Case 4
A 39-year-old Mexican woman was seen with a history of
a slowly growing, well-dened lower lip swelling of rubbery
consistency that extended from the midline to 1 cm beyond
the labial commissure and affected both skin and mucosal
surfaces. With a presumptive diagnosis of a labial salivary
gland adenoma, the lesion was excised. Histopathologic ex-
amination revealed a diffuse granulomatous inltrate with
numerous multinucleated foreign body giant cells, many of
which surrounded vacuoles of varying sizes containing small
fragments of translucent refractile foreign material. These
particles were nonbirefringent when viewed with polarized
light and did not stain with special stains, such as PAS, alcian
blue, and oil red O. The lesion extended from the supercial
lamina propria deep into the underlying skeletal muscle and
was clearly demarcated from the adjacent brous tissue. The
reaction extended beyond the lower surgical margin. The
patient admitted she received 1 liquid silicone injection in the
affected area 7 years previously during a surgical procedure
for correction of a previous surgical scar caused by a motor
vehicle accident. After 3 years of follow-up, the patient still
has persistent disease.
Fig 4. Case 2. Swelling of upper right lip.
68 Ficarra, Mosqueda-Taylor, and Carlos ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
July 2002
Case 5
A 38-year-old Mexican woman underwent injection of liquid
silicone for lower lip augmentation 7 years previously. The
patient did well for 5 years until she started to notice a gradual
size increase of 2 localized areas of the lip mucosa, resulting in
nodules, each approximately 2 cm in diameter. Two years after
the lesions were rst noticed, the patient consulted a maxillo-
facial surgeon, who performed excisional biopsy of both nod-
ules. Histopathologic examination revealed extensive areas
of brohistiocytic inammation that surrounded numerous
individual and empty cystic spaces of varying sizes, giving
the appearance of Swiss cheese, extending from the inter-
face with the overlying atrophic squamous epithelium to
the supercial bundles of underlying skeletal muscle. Post-
operative follow-up was uneventful, and 2 years later, the
patient remains well without disgurement.
Fig 5. Case 2. Histopathologic aspect is similar to that depicted in Fig 3 (hematoxylin-eosin stain; original magnication, 10).
Fig 6. Case 3. Diffuse enlargement of lower lip with involvement of entire vermilion border, adjacent skin, and labial mucosa,
extending to right mental region.
Ficarra, Mosqueda-Taylor, and Carlos 69 ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
Volume 94, Number 1
Case 6
A 52-year-old Guatemalan woman sought medical advice
because of a swelling involving her upper lip of approximately
1 month duration. The lesion was rm, mobile, diffuse, and
slightly tender on palpation. The clinical diagnosis was salivary
gland adenoma or nerve sheath tumor. Excisional biopsy was
difcult because of the poorly dened limits of the lesion, and
for this reason, it was taken in several pieces. Microscopic
examination revealed the same histopathologic aspects as the
previous cases. Special stains, including PAS, oil red O, and
alcian blue, were all negative. On a subsequent visit, the patient
admitted to receiving injection of an unknown substance for
cosmetic purposes 1 year before consultation. She commented
that the substance was injected by a cosmetologist, not a physi-
cian. Wound healing was uneventful, and the patient was lost to
follow-up 1 month after consultation.
Case 7
A 77-year-old woman from Guatemala City was referred
by her dentist who noted several submucosal nodules involv-
ing the buccal mucosa bilaterally and the upper lip. The
lesions appeared well circumscribed, relatively mobile, and
nontender on palpation. Medical history was remarkable for
severe, incapacitating, and deforming rheumatoid arthritis,
diagnosed 15 years previously. On further questioning, the
patient admitted that approximately 5 years before consulta-
tion a cosmetologist recommended injections of a special
substance as a new harmless method to correct wrinkles.
According to the patient, the substance was manufactured by
an unknown South American pharmaceutical company and
was injected by a physician. The name of the doctor was
provided, but it did not appear in the les of the Guatemalan
College of Physicians. Therefore, it was likely that this person
was not a real doctor, and if so, he was illegally practicing in
Guatemala. A biopsy was planned with the clinical diagnoses
of orofacial granulomatosis versus silicone granuloma. Mi-
croscopic examination revealed ndings identical to the cases
previously described. The patient was lost to follow-up 2
months after consultation.
DISCUSSION
Silicones are biomaterials ranging from liquid to
solid products and are used widely in medicine. Sili-
cone elastomers (solid forms) are found in implanted
prosthetic devices, contact lenses, and intravenous uid
tubing, and silicone liquid (dimethylpolysiloxane) is
used mainly for soft tissue augmentation.
1,2
When rst introduced in medical practice, silicone
was considered a safe biomaterial because it did not
seem to elicit any pathologic reaction in human tissues.
It was used for a variety of cosmetic purposes, such as
breast, facial, and penis augmentation,
6,16-18
or for med-
ical conditions, such as hemifacial atrophy, Weber-
Christian disease, and traumatic deformities of the fa-
cial tissues.
7,9
However, despite its purported inert
behavior, silicone was soon realized to produce granu-
lomas in human and animal tissues. In 1964, Winer et
al
19
used the term siliconoma to report the granulo-
matous reactions in soft tissues of patients who had
received liquid silicone injections. Animal experiments
also showed the production of granulomas in subcuta-
neous sites after liquid injections and in viscera when
administered with intraperitoneal or vascular injec-
tion.
20
Since 1964, the Federal Drug Administration
(FDA), with jurisdiction solely in the United States, has
limited the clinical use of silicone to a few treatment
protocols and a few experienced investigators. Since
then, a great reduction in the incidence and severity of
such reactions has been observed with use of medical-
grade or FDA-investigational formulations of silicone,
which produce predictable and self-limited inamma-
tory and broplastic responses. The designation of
medical-grade silicone refers to particle purity, sterile
preparation, and constant viscosity. This silicone is
clear, colorless, odorless, and unaffected by storage. It
also is characterized by high water repellency, low
surface tension, low volatility, heat stability, and the
ability to remain in liquid form indenitely.
1,2
Despite
these renements, reports have been seen of severe
chronic inammatory reaction to medical-grade sili-
cone used by FDA-approved investigators, and thus,
this practice has generally been abandoned.
7,21
On the
other hand, in spite of the limited use of silicone in the
United States, the clinical use of non-FDA-approved
liquid silicones and other substances for facial tissue
augmentation in Europe, Asia, and Latin America con-
tinues.
6,11,22,23
The pathogenesis of silicone granuloma is not well
dened. Several investigations have shown that re-
peated exposure to silicone gel may induce an antigen-
specic lymphocyte-mediated response. However, the
results of these studies, which have been mainly con-
ducted to analyze the effects of spillage of silicone
gel-lled mammary implants, remain highly controver-
sial.
24
Tissue reaction to silicone varies in relation to
the form that has been used. Particles of silicone elas-
tomer characteristically produce a foreign body giant
cell reaction that is particularly evident in lymph nodes.
In contrast, when silicone gel or liquid is introduced
into soft tissues, the strong foreign body giant cell
reaction seen with silicone elastomer is typically ab-
sent. Silicone gel and liquid in tissues usually produce
round to oval empty cystic spaces. These spaces may be
small and uniform or large with variation in size and
shape, depending on the amount of silicone injected
into the tissue. Silicone also has the ability of migration
to distant sites. For example, silicone can migrate from
breast gel implants through soft tissues to a variety of
sites, including the upper arm, the chest, the shoulder,
and the axillary lymph nodes. Lymph node involve-
ment also has been observed in patients with elastomer
70 Ficarra, Mosqueda-Taylor, and Carlos ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
July 2002
nger joint implants. Hematogenous dissemination of
particles to viscera represents an additional pattern of
silicone migration. This is seen in patients undergoing
hemodialysis and cardiopulmonary bypass, in patients
with cardiac valve prostheses, and also in patients with
soft tissue injection.
6
Hematogenous spread of silicone
has been reported in almost every organ, including the
liver, kidneys, lungs, brain, pancreas, and bone mar-
row.
6,25
Silicone injections in facial tissues have been used
extensively for a wide variety of medical and cosmetic
purposes over the last 4 decades. The occurrence of un-
desirable reactions is well known and ranges from mild
local inammatory reactions to severe facial deformities
from inltrative granulomatous reactions.
6-14
Some inves-
tigators consider that these adverse effects have been
caused by the presence of impurities in preparations used
in the past, when adulterants were added to the silicone in
a misguided attempt to increase the dermal reaction and to
x the silicone within a brous capsule.
1,26
We present 7 examples of this unusual reaction in
patients who underwent injection of liquid silicone in
the facial tissues 1 to 10 years before development of
facial deformity. All cases occurred in patients from
countries where the exact nature of the silicone injected
is unknown. Because silicone-related complications
tend to appear several years after injection, they will
possibly be observed in future years in those countries
where there is lack of strict control in the use of
nonFDA-approved silicone or other modelating
agents. At least 9 reports about granulomatous inam-
mation after silicone injection of facial tissues exist.
6-14
The time interval between silicone inltration and onset
of symptoms ranged from 5 months to 15 years, which
is similar to that observed in these cases.
The severity of the adverse reaction after inltration
of silicone is highly variable, ranging from local ery-
thema, ecchymosis, hyperpigmentation, and texture
problems (ie, uneven contour) to excessive tissue ele-
vation, pain, chronic ulceration, and migratory subcu-
taneous masses.
1,6,8,10
Although mild inammatory and
brous reactions are observed in most cases, Raszewski
et al
10
described, 19 years after injection of silicone for
nasal bridge augmentation, a locally aggressive bro-
blastic reaction with inltration beyond the subcutane-
ous tissues of the face, including the left orbit and the
frontal and temporal bones. This complication led to
resection of the left upper face and enucleation of the
left eye. On the other hand, it is important to realize that
silicone can migrate to locations distant from the orig-
inal site of application and to lymph nodes, creating a
pattern of clinical presentation, which may be confused
with a malignant neoplasm or other granulomatous
diseases if the clinician or pathologist is unaware of the
patients previous exposure to silicone.
6
Fortunately, silicone granulomas are easily identied
in most cases with light microscopy.
27
Silicone pro-
duces a range of histologic reactions in tissues, depend-
ing on the form of silicone used and the location of the
lesion. The tissue reaction to silicone gel and liquid is
different from that produced in response to silicone
elastomer because the exhuberant foreign body giant
cell reaction seen with the latter is typically absent in
the former. On the other hand, silicone liquid within the
tissue usually shows presence of round to oval cystic
spaces, which tend to appear empty on light micro-
scopic examination. These may be relatively small and
uniform or large and irregular, depending on the
amount of material introduced into the tissues. Sur-
rounding brosis may be induced by migration of sili-
cone particles along tissue planes, such as that occur-
ring after ruptured breast implants
25
or through the
production of silica from silicone by macrophages.
10,28
Silicone has been shown to also enter the blood-
stream from soft tissue injection sites and with direct
intravascular injection. Several fatalities have occurred
shortly after soft tissue injections of large amounts of
liquid silicone, some of which was probably injected
directly into the bloodstream.
6,13
From a clinical point of view, the differential diag-
nosis of silicone granuloma includes a variety of con-
ditions that are listed in Table III. Labial cases seen as
well-dened nodules suggest a differential diagnosis of
salivary gland cyst and tumor, soft tissue cyst (dermoid
cyst), and tumor.
29,30
Cases seen as persistent or recur-
rent solid facial swelling or multiple nodules resemble
a number of disorders. Recurrent facial erysipelas may
Table III. Differential diagnosis of silicone granuloma
Well-dened single nodule
Salivary gland cysts and tumors
Soft tissue cysts (dermoid cyst) or tumors
Persistent or recurrent solid facial swelling or multiple nodules
Infections: recurrent facial erysipelas, tuberculosis, lepromatous leprosy, South American blastomycosis, trichinosis
Inammatory disease: allergic contact dermatitis, facial edema with eosinophilia, cheilitis glandularis apostematosa, Aschers syndrome
Orofacial granulomatosis: Crohns disease, Melkersson-Rosenthal syndrome, sarcoidosis
Foreign body granulomas: parafnoma, talc granuloma, silica, silicone, bovine collagen, etc
Ficarra, Mosqueda-Taylor, and Carlos 71 ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
Volume 94, Number 1
result in persistent lymphedematous swelling of the
affected part. Typically, patients with erysipelas report
repeated bouts of swelling with pain, fever, and ery-
thema. Other infectious diseases that may give similar
features are tuberculosis (lupus vulgaris), lepromatous
leprosy, South American blastomycosis, and trichino-
sis.
29
Among inammatory diseases sharing this pattern
of clinical presentation are allergic contact dermatitis,
facial edema with eosinophilia, cheilitis glandularis
apostematosa, and Aschers syndrome. Facial edema
with eosinophilia, a rare disorder rst described in
1985,
31
is characterized by diffuse nonpitting edema of
the face associated with marked peripheral-blood eo-
sinophilia. The edema is episodic initially but eventu-
ally persistent. Skin biopsy reveals perivascular inl-
trates of lymphocytes admixed with small numbers of
eosinophils. Cheilites glandularis apostematosa is char-
acterized by inammation and hypertrophy of the mi-
nor salivary glands in the lower lip.
29
Aschers syn-
drome affects the upper lip, producing nodular
submucosal swelling (double lip). This rare syndrome
is also characterized by blepharochalasis, inammation
of accessory lacrimal glands, and thyromegaly.
32
Oro-
facial granulomatosis, such as Crohns disease, Melk-
ersson-Rosenthal syndrome, and sarcoidosis, also may
be confused with silicone granuloma. Crohns disease
involving the oral mucosa may result in progressive
rubbery swelling of the buccal surfaces. On histologic
examination, noncaseating granulomas are seen in the
submucosa.
33
Melkersson-Rosenthal syndrome is a
unique disorder with the triad of facial nerve palsy,
lingua plicata (ssured tongue), and solid facial swell-
ing.
34,35
The complete syndrome is, however, rarely
seen, and orofacial swelling remains the sine qua non of
the disease and precedes other features in approxi-
mately 40% of cases. Sarcoidosis may involve the lips
or facial skin, producing characteristic shiny purple-red
nodules.
29
Foreign body granulomas parafnoma and
talc granuloma and granulomatous response to silica,
silicone, and bovine collagen can be differentiated from
silicone granuloma through their histologic aspects and
use of polarized light.
36
Finally, for extensive and ag-
gressive cases, such as that reported by Raszewski et
al,
10
low-grade brosarcoma and desmoid bromatosis
should be considered in the differential diagnosis.
Treatment of soft tissue silicone granuloma is dif-
cult, and surgical excision is warranted when possi-
ble.
7,12,14
For well-circumscribed nodular lesions, sur-
gical excision represents a reasonable and effective
approach as it has been observed in some of our pa-
tients. Instead, for widespread lesions, complete eradi-
cation of the granulomatous tissue is highly improbable
and surgery may lead to scarring and stulas. Even
though corticosteroids have produced benecial effects
in the treatment of some granulomatous diseases,
19
their efcacy appears limited and their therapeutic role
is not well dened by appropriate studies. Prednisone
has mainly been used in doses ranging from 1 mg/d to
60 mg/d, with transient improvement of patient signs
and symptoms. Successful response has been reported
recently by Senet et al
12
with the use of minocycline for
the treatment of 2 cases of cutaneous silicone granulo-
mas, and these authors suggested that the benecial
effects of minocycline are related to its antiinamma-
tory or immunomodulating effects and to antigranulo-
matous properties, which have been shown in vitro.
37,38
Liquid silicone injections remain controversial, par-
ticularly in those countries where there is inadequate
investigation and control of biomaterials used for soft
tissue augmentation. In our patients and in most previ-
ously reported cases, the medical grade of the injected
silicone was unknown.
We thank Drs J. C. Lopez Noriega and C. Liceaga for
contributing cases 2 and 3.
REFERENCES
1. Clark DP, Hanke CW, Swanson NA. Dermal implants: safety of
products injected for soft tissue augmentation. J Am Acad Der-
matol 1989;21:992-8.
2. Selmanowitz VJ, Orentreich N. Medical grade uid silicone: a
monographic review. J Dermatol Surg Oncol 1977;3:597-611.
3. Brown JB. Studies of silicones and Teon as subcutaneous
prostheses. Plast Reconstr Surg 1961;28:86-92.
4. Hench LL. Biomaterials. Science 1980;208:826-31.
5. Ben-Hur N, Neumen Z. Siliconoma: another cutaneous response
to dimethylpolysiloxane. Plast Reconstr Surg 1965;36:629-34.
6. Travis WD, Balogh K, Abraham JL. Silicone granulomas: report
of three cases and review of the literature. Hum Pathol 1985;16:
19-27.
7. Achauer BM. A serious complication following medical-grade
silicone injection of the face. Plast Reconstr Surg 1983;71:251-3.
8. Mastruserio N, Pesqueira MJ, Cobb MW. Severe granulomatous
reaction and facial ulceration occurring after subcutaneous sili-
cone injection. J Am Acad Dermatol 1996;34:849-52.
9. Pearl RM, Laub DR, Kaplan DN. Complications following sili-
cone injections for augmentations of the contours of the face.
Plast Reconstr Surg 1978;61:888-91.
10. Raszewski R, Guyuron B, Lash RH, et al. A severe brotic
reaction after cosmetic liquid silicone injection. J Craniomaxil-
lofac Surg 1990;18:225-8.
11. Bigata X, Ribera M, Bielsa I, Ferrandiz C. Adverse granuloma-
tous reaction after cosmetic dermal silicone injection. Dermatol
Surg 2001;27:198-200.
12. Senet P, Bachelez H, Ollivaud L, Vignon-Pennamen D, Duber-
tret L. Minocycline for the treatment of cutaneous silicone gran-
ulomas. Br J Dermatol 1999;140:985-7.
13. Ellenbogen R, Ellenbogen R, Rubin L. Injectable uid silicone
therapy. Human morbidity and mortality. JAMA 1975;234:
308-9.
14. Rees TD, Ballantyne DL, Seidman I. Eyelid deformities caused
by injection of silicone uid. Br J Plast Surg 1971;24:125-8.
15. Sanchez-Guerrero J, Colditz GA, Karlson EW, et al. Silicone
breast implants and the risk of connective-tissue diseases and
symptoms. N Engl J Med 1995;332:1666-70.
16. Symmers W. Silicone mastitis in topless waitresses. Br Med J
1968;3:19-22.
17. Datta NS, Kern FB. Silicone granuloma of the penis. J Urol
1973;109:840-2.
72 Ficarra, Mosqueda-Taylor, and Carlos ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
July 2002
18. Bigata X, Ribera M, Bielsa I, Ferrandiz C. Adverse granuloma-
tosis reaction after cosmetic dermal silicone injection. Dermatol
Surg 2001;27:198-200.
19. Winer LH, Stenberg TH, Lehman R, et al. Tissue reactions to
injected silicone liquids. Arch Dermatol 1964;90:588-92.
20. Ben-Hur N, Ballantyne DL, Rees TD, et al. Local and systemic
effects of dimethylpolysiloxane uid in mice. Plast Reconstr
Surg 1967;39:423-7.
21. Vinnick CA. The hazards of silicone injections. JAMA 1976;
236:959-62.
22. Chastre J, Basset F, Viau F, et al. Acute pneumonitis after
subcutaneous injections of silicone in transsexual men. N Engl
J Med 1983;309:856-60.
23. Arenas R, Milla L, Castillo JM. Paniculitis granulomatosa por
guayacol en aceite de sesamo. Estudio de tres casos. Dermatol
Rev Mex 1988;32:148-54.
24. Narini PP, Semple JL, Hay JB. Repeated exposure to silicone gel
can induce delayed hypersensitivity. Plast Reconstr Surg 1995;
96:371-80.
25. Capozzi A, DuBou R, Pennisi VR. Distant migration of silicone
gel from a ruptured breast implant. Plast Reconstr Surg 1989;62:
302-3.
26. McDowell F. Complications with silicones: what grade of sili-
cone? How do we know it was silicone? Plast Reconstr Surg
1978;61:892-4.
27. Requena C, Izquierdo MJ, Navarro M, Martinez A, et al. Adverse
reactions to injectable aesthetic microimplants. Am J Dermato-
pathol 2001;23:197-202.
28. Schmidt JA, Oliver CN, Lepe-Zuniga JL, Green I, Gery I. Silica-
stimulated monocytes release broblast proliferation factors
identical to interleukin 1. J Clin Invest 1984;73:1462-72.
29. Neville BW, Damm DD, Allen CM, Bouquout JE, editors. Oral
and maxillofacial pathology. Philadelphia: WB Saunders Com-
pany; 1995. p. 142-80; 322-61.
30. Ficarra G, editor. Manuale di patologia e medicina orale, 2nd ed.
Milan: McGraw-Hill; 2001. p. 83-9; 151-76.
31. Songsiridej V, Peters MS, Dor PJ, Ackerman SJ, Gleich GJ,
Busse WW. Facial edema and eosinophilia: evidence for eosin-
ophil degranulation. Ann Intern Med 1985;103:503-6.
32. Barnett ML, Bosshardt LL, Morgan AF. Double lip and double
lip with blepharochalasis (Aschers syndrome). Oral Surg Oral
Med Oral Pathol 1972;34:727-33.
33. Ficarra G, Cicchi P, Amorosi A, Piluso S. Oral Crohns disease
and pyostomatitis vegetants: an unusual association. Oral Surg
Oral Med Oral Pathol 1993;75:220-4.
34. Rubino I, Ficarra G. Sindrome di Melkersson-Rosenthal. Descri-
zione di due casi. Minerva Stomatol 1994;43:595-9.
35. Rogers RS. Melkersson-Rosenthal syndrome and orofacial gran-
ulomatosis. Dermatol Clin 1996;14:371-9.
36. Shapiro PE. Noninfectious granulomas. In: Elder D, Elenitsas R,
Jaworsky C, Johnson B Jr, editors. Levers histopathology of the
skin. 8th ed. Philadelphia: Lippincott-Raven; 1997. p. 317-40.
37. Webster GF, Toso SM, Hegemann L. Inhibition of a model of in
vitro granuloma formation by tetracyclines and ciprooxacin.
Involvement of protein kinase C. Arch Dermatol 1994;130:748-
52.
38. Tilley BC, Alarcon GS, Heyse SP, et al. Minocycline in rheu-
matoid arthritis. A 48-week, double blind, placebo-controlled
trial. Ann Intern Med 1995;122:81-9.
Reprint requests:
Dr Giuseppe Ficarra
Section of Oral Pathology and Medicine
Department of Odontology and Stomatology
Viale Morgagni 85
50134 Florence Italy
gicarr@tin.it
CALL FOR REVIEW ARTICLES
The January 1993 issue of Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology,
and Endodontics contained an Editorial by the Journals Editor in Chief, Larry J. Peterson, that
called for a Review Article to appear in each issue.
These Review Articles should be designed to review the current status of matters that are
important to the practitioner. These articles should contain current developments, changing
trends, as well as reafrmation of current techniques and policies.
Please consider submitting your article to appear as a Review Article. Information for
authors appears in each issue of Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology,
and Endodontics.
We look forward to hearing from you.
Ficarra, Mosqueda-Taylor, and Carlos 73 ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
Volume 94, Number 1
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Copeland Erotica.Document12 pagesCopeland Erotica.Craig Monger25% (4)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Breast Men Film ReflectionDocument1 pageBreast Men Film ReflectionCharlene ElioNo ratings yet
- The Maxilla-Premaxilla Approach To Extensive Nasal Septum SurgeryDocument13 pagesThe Maxilla-Premaxilla Approach To Extensive Nasal Septum Surgeryentgo8282100% (1)
- Breast Implant Illness Scientific Evidence of Its ExistenceDocument16 pagesBreast Implant Illness Scientific Evidence of Its ExistenceDiego Fernando Mosquera AgudeloNo ratings yet
- 98 PAGE Sample Office Policy and ProceduresDocument98 pages98 PAGE Sample Office Policy and ProceduresDenise MathreNo ratings yet
- Breast AugmentationDocument2 pagesBreast AugmentationAlexandre Campos Moraes AmatoNo ratings yet
- Debate - Cosmetic SurgeryDocument13 pagesDebate - Cosmetic Surgeryrgk2060No ratings yet
- MCQ Breast Surgery Bordeaux 2010Document9 pagesMCQ Breast Surgery Bordeaux 2010Ismail Evren100% (1)
- 1997 - Laura Nader - Controlling ProcessesDocument28 pages1997 - Laura Nader - Controlling ProcessesValentin TappeserNo ratings yet
- Silicone Granuloma of The Face Treated With MinocyclineDocument4 pagesSilicone Granuloma of The Face Treated With Minocyclineentgo8282No ratings yet
- Case Presentation SiliconomaDocument24 pagesCase Presentation Siliconomaentgo8282No ratings yet
- Simultaneous Presentation of Silicone and Silica GranulomaDocument4 pagesSimultaneous Presentation of Silicone and Silica Granulomaentgo8282No ratings yet
- Cutaneous Silicone Granuloma Mimicking Breast Cancer After Ruptured Breast ImplantDocument4 pagesCutaneous Silicone Granuloma Mimicking Breast Cancer After Ruptured Breast Implantentgo8282No ratings yet
- Neck Lymphadenitis Due To Silicone Granuloma After MammaryDocument6 pagesNeck Lymphadenitis Due To Silicone Granuloma After Mammaryentgo8282No ratings yet
- Complications After Facial Contour Augmentation With Injectable Silicone. Diagnosis and Treatment. Report of A Severe CaseDocument6 pagesComplications After Facial Contour Augmentation With Injectable Silicone. Diagnosis and Treatment. Report of A Severe Caseentgo8282No ratings yet
- H 2 02 (1) (1) .FeedbackDocument8 pagesH 2 02 (1) (1) .Feedbackentgo8282No ratings yet
- Silicone Lymphadenopathy - An Unexpected CauseDocument4 pagesSilicone Lymphadenopathy - An Unexpected Causeentgo8282No ratings yet
- Silicone Migration To The Contralateral Axillary Lymph Nodes and Breast After Highly Cohesive Silicone Gel Implant FailureDocument3 pagesSilicone Migration To The Contralateral Axillary Lymph Nodes and Breast After Highly Cohesive Silicone Gel Implant Failureentgo8282No ratings yet
- Posterior TympanotomyDocument6 pagesPosterior Tympanotomyentgo8282No ratings yet
- Granulomatous Reaction To Silicone InjectionDocument4 pagesGranulomatous Reaction To Silicone Injectionentgo8282No ratings yet
- - 에 기침하면서 어지럼증 발생하여 앞으로 서러지고 glabella 부위 수상 택시 타고 내리다가 안면부수상Document14 pages- 에 기침하면서 어지럼증 발생하여 앞으로 서러지고 glabella 부위 수상 택시 타고 내리다가 안면부수상entgo8282No ratings yet
- Locoregional Silicone Spread After High Cohesive Gel Silicone Implant RuptureDocument2 pagesLocoregional Silicone Spread After High Cohesive Gel Silicone Implant Ruptureentgo8282No ratings yet
- Fitting and Modifying Hearing InstrumentsDocument32 pagesFitting and Modifying Hearing Instrumentsentgo8282No ratings yet
- 2010KoreanGuideline pediatricOM forSMEDDocument109 pages2010KoreanGuideline pediatricOM forSMEDentgo8282No ratings yet
- Treatment PhilosophyDocument1 pageTreatment Philosophyentgo8282No ratings yet
- 5 (1) (1) .Compression of DilonDocument63 pages5 (1) (1) .Compression of Dilonentgo8282No ratings yet
- Acute supraglottitis의 치료Document4 pagesAcute supraglottitis의 치료entgo8282No ratings yet
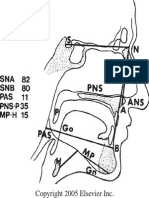
- Standard Cephalometric TracingDocument1 pageStandard Cephalometric Tracingentgo8282No ratings yet
- Please Answer The Following Questions Based On This ScaleDocument1 pagePlease Answer The Following Questions Based On This Scaleentgo8282No ratings yet
- Basics of Sleep Staging CMPDocument25 pagesBasics of Sleep Staging CMPentgo8282No ratings yet
- Thyroid Isthmusectomy - A Critical AppraisalDocument4 pagesThyroid Isthmusectomy - A Critical Appraisalentgo8282No ratings yet
- Orocraniofacial Features Clinical ScaleDocument1 pageOrocraniofacial Features Clinical Scaleentgo8282No ratings yet
- BPPV-마산, 창원 신경과Document38 pagesBPPV-마산, 창원 신경과entgo8282No ratings yet
- BPPV in The ElderlyDocument5 pagesBPPV in The Elderlyentgo8282No ratings yet
- BPPV and Long-Term Follow-UpDocument4 pagesBPPV and Long-Term Follow-Upentgo8282No ratings yet
- Case Presentation김봉태Document12 pagesCase Presentation김봉태entgo8282No ratings yet
- Case Presentation-Bilateral Peritonsillar AbscessDocument29 pagesCase Presentation-Bilateral Peritonsillar Abscessentgo8282No ratings yet
- Catalogo Eurosilicone EnglishDocument32 pagesCatalogo Eurosilicone EnglishKaterina De FernandezNo ratings yet
- HUM 251 Breast ImplantsDocument3 pagesHUM 251 Breast ImplantsAssignment ExpertsNo ratings yet
- Cosmetic Surgery PpsDocument27 pagesCosmetic Surgery Ppsyamos2No ratings yet
- SiliconaDocument3 pagesSiliconaLucilaNo ratings yet
- Newsletter ISAPS May-August11 PDFDocument21 pagesNewsletter ISAPS May-August11 PDFhuyenthanh1807No ratings yet
- Functional Biocompatibility Testing of Silicone Breast Implants and A NovelDocument7 pagesFunctional Biocompatibility Testing of Silicone Breast Implants and A NovelIim MafahirNo ratings yet
- Breast Reconstruction After Mastectomy For Breast Tumor: About 24 CasesDocument6 pagesBreast Reconstruction After Mastectomy For Breast Tumor: About 24 CasesIJAR JOURNALNo ratings yet
- Eurosilicone Product Catalogue 2012 PDFDocument27 pagesEurosilicone Product Catalogue 2012 PDFLiliana AyalaNo ratings yet
- Linguine Sign PDFDocument2 pagesLinguine Sign PDFserubimNo ratings yet
- Surgical Cure of Clarithromycin Resistant Mycoba - 2020 - Journal of Clinical TuDocument5 pagesSurgical Cure of Clarithromycin Resistant Mycoba - 2020 - Journal of Clinical TuKarina ChristantoNo ratings yet
- 1er Février 2012. Commission Européenne PIP "Stress Test".Document15 pages1er Février 2012. Commission Européenne PIP "Stress Test".LeMonde.frNo ratings yet
- Law of Tort AssignmentDocument11 pagesLaw of Tort AssignmentChabala ChibeloNo ratings yet
- Breast UltrasoundDocument57 pagesBreast UltrasoundYoungFanjiensNo ratings yet
- CasesDocument17 pagesCasesManzoor AhmedNo ratings yet
- Product Ref GuideDocument20 pagesProduct Ref GuideAnonymous 6rAHpKA3PxNo ratings yet
- AB202011 Ch09 StudentWorkbookDocument7 pagesAB202011 Ch09 StudentWorkbookcasti13425% (4)
- Journal Pone 0118161Document10 pagesJournal Pone 0118161David PesireronNo ratings yet
- Arn Report List 20200505Document305 pagesArn Report List 20200505zoheir salmaniNo ratings yet
- Aesthetic Fellowship ReviewDocument2 pagesAesthetic Fellowship ReviewnikitagustiNo ratings yet
- Human Cloning Is The Creation of A Genetically Identical Copy of A HumanDocument1 pageHuman Cloning Is The Creation of A Genetically Identical Copy of A HumanJomark ValerioNo ratings yet
- Literature Review Plastic SurgeryDocument5 pagesLiterature Review Plastic Surgeryf0typiwydeb3100% (2)
- Breast MRIDocument12 pagesBreast MRIZintan HospitalNo ratings yet