Professional Documents
Culture Documents
MANUAL LYMPH DRAINAGE EFFICIENTLY REDUCES POSTOPERATIVE FACIAL SWELLING AND DISCOMFORT AFTER REMOVAL OF IMPACTED THIRD MOLARS, Szolnoky G. 2007
Uploaded by
Felipe RoncerosCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MANUAL LYMPH DRAINAGE EFFICIENTLY REDUCES POSTOPERATIVE FACIAL SWELLING AND DISCOMFORT AFTER REMOVAL OF IMPACTED THIRD MOLARS, Szolnoky G. 2007
Uploaded by
Felipe RoncerosCopyright:
Available Formats
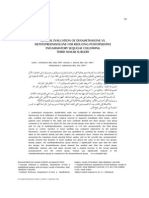
138
Lymphology 40 (2007) 138-142
MANUAL LYMPH DRAINAGE EFFICIENTLY REDUCES
POSTOPERATIVE FACIAL SWELLING AND DISCOMFORT
AFTER REMOVAL OF IMPACTED THIRD MOLARS
G. Szolnoky, K. Szendi-Horvth, L. Seres, K. Boda, L. Kemny
Departments of Dermatology and Allergology (Phlebo-Lymphology and Wound Care Unit) (GS,LK),
Dentistry and Oral Surgery (LS), and Medical Informatics (KB), University of Szeged, and Department
of Physiotherapy (KS-H), Istvan Bugyi County Hospital, Szentes, Hungary
after MLD (p=0.0295). This initial study
demonstrates that MLD may promote an
improvement of lymph circulation and work
in an adjunctive role for reduction of
postoperative swelling and pain following
removal of impacted third molars.
Keywords: wisdom tooth, operation, pain,
swelling, manual lymph drainage
Wisdom tooth removal is a commonly
undertaken procedure which is necessary
when the jaws are not large enough to
accommodate the wisdom teeth or the
wisdom teeth are lying in a poor position (1).
Removal of third molars can vary greatly in
difficulty, some being very straightforward,
others being difficult and requiring surgical
intervention. Following the procedure,
patients develop pain and swelling associated
with the surgical sites, and this is variable
from person to person without apparent
reason. The extent and difficulty of operation
are also variables (2), and there have been
some attempts to predict pain and swelling
based on preoperative conditions (3).
Postoperative edema and pain can be
alleviated via a wide variety of local and
systemic treatments. Local cooling with
ice-packs is the most common postoperative
care to minimize swelling, although no
evidence supports its usage (4). Non-steroid
anti-inflammatory drugs have been shown
ABSTRACT
The removal of wisdom teeth is often
associated with severe postoperative edema
and pain, and operation on the third molar
can cause local inflammation that impairs
lymph transport. The objective of the study
was to assess the efficacy of manual lymph
drainage (MLD) in reducing swelling following
bilateral wisdom tooth removal. Ten
consecutive patients with bilateral impacted
wisdom teeth that required surgical removal
were enrolled in the study. Each patient
was postoperatively treated with MLD (after
Vodders method) on one side of the neck
region with the untreated contralateral side
as a control. Swelling was evaluated using a
tape-measure placed in contact with the
skin. The six landmarks of measurement
included tragus-lip junction, tragus-pogonion,
mandibular angle-external corner of eye,
mandibular angle-ala nasi, mandibular angle-
lip junction, and mandibular angle-median
point of chin. Subjective assessment of MLD
was conducted with self-evaluation using a
visual analogue bar scale (VAS, range 0-100
mm). Of the 6 linear measurements, 4 lines
(2, 4, 5, 6) showed a significant reduction
of swelling on the side of MLD compared to
the untreated side. Mean score of VAS of
pretreatment condition was 35.5 20.60 mm
that decreased to 22 19.32 mm measured
139
to efficiently reduce pain and inflammation
(5-9) while application of antibiotics
(prophylaxis or treatment) provides a reliable
infection control (6). Removal of wisdom
teeth and other oral surgery procedures may
cause rapidly evolving, severe edema and
sometimes hardly bearable pain as the
consequence of post-traumatic inflammation
(3). Any kind of surgical intervention can
play a role as a dynamic factor in the
development of local lymphatic insufficiency
causing lymphatic vessels to be temporarily
unable to cope with excessive amount of
lymph. This aspect of inflammation raised
the need for a method that would enhance
lymphatic transport capacity. Manual lymph
drainage (MLD) is a gentle massage technique
that improves lymph flow, microcirculation
and tissue oxygenation, and reduces edema
and pain (10). It is applicable to any area of
the body and various forms of edema
including head and neck swelling. In this
region, encephalopathy with lymph stasis,
cervical post-traumatic lymphedema, post-
traumatic increased intracranial pressure,
and surgery-associated swelling are all
candidates for MLD (10). So far, evidence
proving its efficacy has not been published.
The aim of this study was to investigate
whether the application of MLD in the case
of third molar extraction can efficiently
diminish postoperative pain and swelling.
One of the greatest obstacles for a precise,
reliable and objective demonstration of the
characteristics of a drug or a technique is the
difficulty in volume-reduction assessment.
Although numerous methods have been tried,
some have been shown to lack sensitivity,
and others are laborious and not applicable
from the operative standard point (11-14).
A new objective method using linear
measurements has recently been published
to allow precise detection and monitoring
of changes in facial swelling (15).
PATIENTS AND METHODS
Ten consecutive patients with bilateral
impacted wisdom teeth that required surgical
removal entered the study. All third molar
teeth were partially or completely covered
by mucosa and cortical bone. All patients had
the right and left sided wisdom teeth in the
same position so the planned surgical proce-
dure was the same on both sides. Patients
signed a written informed consent approved
by the Ethical Committee of the University
of Szeged. Exclusion criteria included facial
or neck inflammatory skin diseases, carotis
sinus hyperaesthesia, hyperthyroidism, and
patients who rejected unilateral MLD as a
part of post-operative treatment. Position of
impacted teeth was visualized with X-ray
examination. Patients were not given pre-
operative antibiotic treatment. Male/female
ratio was 7/3 and the mean age was 21 years
(14-27 years). Each patient underwent
bilateral removal of the third molar teeth.
The same surgeon performed the procedures
on the left and the right side. Three patients
had both upper and lower, while 7 had only
lower wisdom tooth removal. Briefly, surgical
intervention occurred as follows (16). All
operations were performed under general
anaesthesia. Mucoperiosteal flap was
reflected from the mesial corner of the first
molar distally to the retromolar region. Bone
was removed with a water-cooled round
burr. In four patients, both lower teeth were
sectioned with fissure bur. The socket was
irrigated with sterile physiological salt
solution. A 4-0 resorbable suture was used to
close the wound. One suture was placed
interdentally between the first and second
molars, and two stitches were used to close
the distal part of incision. No penicillin or
diclofenac allergy was reported, therefore
patients received 375 mg oral amoxicillin/
clavulanic acid three times daily for 5 days
and 50 mg oral diclofenac three times daily
for three days.
Each patient was treated unilaterally in
the neck region using Vodders method as
described elsewhere (10). The side of MLD
was decided by randomization. Each patient
served as his own control, hence the untreated
140
T
A
B
L
E
M
e
a
s
u
r
e
m
e
n
t
o
f
A
n
a
t
o
m
i
c
L
a
n
d
m
a
r
k
s
o
f
t
h
e
F
a
c
e
P
r
i
o
r
t
o
O
p
e
r
a
t
i
o
n
,
P
o
s
t
o
p
e
r
a
t
i
v
e
l
y
B
e
f
o
r
e
a
n
d
a
f
t
e
r
t
h
e
F
u
l
l
C
o
u
r
s
e
o
f
M
L
D
.
R
e
s
u
l
t
s
a
r
e
D
i
s
p
l
a
y
e
d
a
s
M
e
a
n
D
a
t
a
S
D
D
a
y
1
D
i
f
f
e
r
e
n
c
e
D
a
y
0
(
P
r
i
o
r
t
o
(
S
u
r
g
i
c
a
l
D
a
y
6
(
E
n
d
o
f
P
r
e
-
P
o
s
t
-
o
r
a
l
s
u
r
g
e
r
y
)
i
n
t
e
r
v
e
n
t
i
o
n
)
p
h
y
s
i
o
t
h
e
r
a
p
y
)
T
r
e
a
t
m
e
n
t
p
L
i
n
e
1
(
c
m
)
T
r
e
a
t
e
d
9
.
3
9
0
.
5
9
1
0
1
.
0
6
9
.
5
6
0
.
7
1
0
.
4
4
0
.
7
2
n
.
s
.
(
t
r
a
g
u
s
-
l
i
p
j
u
n
c
t
i
o
n
)
U
n
t
r
e
a
t
e
d
9
.
5
3
0
.
6
6
9
.
5
9
0
.
4
8
9
.
3
3
0
.
4
6
0
.
2
6
0
.
3
7
L
i
n
e
2
(
c
m
)
T
r
e
a
t
e
d
9
.
9
2
0
.
8
0
1
0
.
8
3
1
.
1
0
1
0
.
1
7
0
.
8
7
0
.
6
6
0
.
4
1
0
.
0
4
9
(
t
r
a
g
u
s
-
p
o
g
o
n
i
o
n
)
U
n
t
r
e
a
t
e
d
9
.
6
4
1
.
1
5
1
0
.
3
8
0
.
5
3
1
0
.
0
9
0
.
4
5
0
.
2
9
0
.
5
2
L
i
n
e
3
(
c
m
)
T
r
e
a
t
e
d
8
.
1
0
.
6
0
9
.
0
1
1
.
0
1
8
.
2
1
0
.
5
7
0
.
8
0
0
.
8
5
0
.
0
5
4
(
m
a
n
d
i
b
u
l
a
r
a
n
g
l
e
-
e
y
e
U
n
t
r
e
a
t
e
d
8
.
0
2
0
.
8
6
8
.
6
9
0
.
8
3
8
.
3
1
0
.
6
4
0
.
3
8
0
.
4
9
e
x
t
e
r
n
a
l
c
o
r
n
e
r
)
L
i
n
e
4
(
c
m
)
T
r
e
a
t
e
d
1
0
.
4
3
0
.
5
9
1
1
.
2
3
0
.
9
6
1
0
.
5
8
0
.
8
9
0
.
6
5
0
.
5
6
0
.
0
4
9
(
m
a
n
d
i
b
u
l
a
r
a
n
g
l
e
-
U
n
t
r
e
a
t
e
d
1
0
.
3
7
1
.
2
5
1
0
.
7
9
1
.
2
9
1
0
.
6
4
0
.
8
9
0
.
1
5
0
.
9
2
a
l
a
n
a
s
i
)
L
i
n
e
5
(
c
m
)
T
r
e
a
t
e
d
1
0
.
7
0
0
.
6
9
1
1
.
3
3
0
.
6
4
1
0
.
5
8
0
.
9
1
0
.
4
2
0
.
3
4
0
.
0
2
9
(
m
a
n
d
i
b
u
l
a
r
a
n
g
l
e
-
l
i
p
U
n
t
r
e
a
t
e
d
1
0
.
6
8
0
.
7
3
1
1
.
1
5
0
.
9
0
1
1
.
0
6
0
.
7
6
0
.
0
9
0
.
3
6
j
u
n
c
t
i
o
n
)
L
i
n
e
6
(
c
m
)
T
r
e
a
t
e
d
1
4
.
5
0
0
.
8
0
1
5
.
3
1
0
.
9
4
1
4
.
5
7
0
.
8
1
0
.
7
4
0
.
5
0
0
.
0
1
6
(
m
a
n
d
i
b
u
l
a
r
a
n
g
l
e
U
n
t
r
e
a
t
e
d
1
4
.
6
4
1
.
8
1
1
4
.
9
6
1
.
2
6
1
4
.
8
5
1
.
2
0
0
.
1
1
0
.
5
8
m
e
d
i
a
n
p
o
i
n
t
o
f
c
h
i
n
)
141
side was appropriate for comparison. 30-min
MLD was carried out once daily in the first,
second and third postoperative day. Evalua-
tion of the therapy was scheduled to the
sixth postoperative day, when sutures were
completely removed.
Swelling was evaluated with the objective
method using a tape-measure graduated in
millimeters, placed in contact with the skin.
The six landmarks of measurement were as
follows: tragus-lip junction, tragus-pogonion,
mandibular angle-external corner of eye,
mandibular angle-ala nasi, mandibular angle-
lip junction, mandibular angle-median point
of chin. The previously described method of
measurement was accomplished prior to
operation, on the first and sixth postoperative
day. Subjective assessment of MLD based on
change in pain and general discomfort was
assessed with self-evaluation using a 100-mm-
length bar for the representation of visual
analogue scale (VAS) on the first and sixth
postoperative day. 0 reflected a painless state,
and 100 corresponded to intense, unbearable
pain (15).
Statistical Analysis
Distances at preoperative, onset stage
were not considered. The change between
postsurgical conditions was calculated at
each side. A one-tailed paired t-test was used
to examine whether the mean change at the
MLD-treated side was significantly greater
than the change at the control side.
RESULTS
The self-assessment of pain using VAS
for pretreatment condition was 35.5 20.60
mm which decreased to 22 19.32 mm
measured after the full-course of MLD
(p=0.029). This finding reflected a significantly
improved quality of life within the study
group (patients 6, 8 and 9 demonstrated no
difference before and after MLD). The Table
shows the alteration of distances between the
examined anatomic sites. Of the 6 linear
measurements, two landmarks failed to
demonstrate a significant reduction of
swelling on the side of MLD compared to
untreated, control side (line 1 and just not
significant line 3). All other lines (2, 4, 5, 6)
demonstrated a significant difference.
DISCUSSION
Previous studies have shown that the use
of corticosteroids, non-steroidal antiinflam-
matory drugs, and antibiotics after wisdom-
tooth removal may contribute to decreased
swelling and pain, and some of these methods
could exert a synergistic effect. Emerging
cases of drug-allergy and drug-associated side
effects are focusing more attention on alter-
native methods (17). In a preliminary study,
local cryotherapy after third molar extraction
seemed to lower severe consequences such as
swelling and pain. Despite the fact that ice-
packs are widely used for inflammation- and
trauma-related edema reduction, no strong
evidence supports their application.
It is well-known that operation and
traumatic injuries alter lymph circulation
causing local edema usually by inflammation
promoting a dynamic insufficiency compo-
nent of lymphedema. Mechanical causes can
also occur when transport capacity is affected
from complete or incomplete blockade of
lymph vessels. MLD patterned after Vodder
has been indicated for the head and neck
region in the case of neoplastic or cancer
treatment-related lymphedemas, and we
have also shown the beneficial effect of MLD
in the trapdoor phenomenon of facial
subcutaneous pedicle flaps (18). MLD is
thought to increase transport capacity of
lymph vessels by raising the lymphangio-
motor activity and stimulating lymph nodes
to further improve lymph transport.
The availability of a value to quantify
swelling in an objective and repeatable
fashion has long been a goal of research,
especially in dentistry or oral surgery in
order to evaluate the efficacy of a drug and
to obtain data for comparison studies. The
142
simplest methods, which entail having the
patient or physician compile VAS, are highly
influenced by the subjective nature of visual
evaluation. Although numerous methods
have been devised to provide objective
measurement of facial swelling, some are
imprecise, and others more complex, expen-
sive, and difficult to standardize (11-14).
The present study used the method of linear
measurement originally tested in facial
abscesses to more precisely quantify the
changes in facial volume (15). This method
provided a series of data points utilizing
defined landmarks.
This study using reproducible facial
measurements and a VAS pain scale has
demonstrated that a significant reduction in
facial swelling and pain can be obtained using
MLD after removal of impacted third molars.
REFERENCES
1. Conrad, S, GH Blakey, DA Shugars, et al:
Patients perception of recovery after third
molar surgery. J. Oral. Maxillofac. Surg. 57
(1999), 1288-1294.
2. Renton, T, N Smeeton, M McGurk: Factors
predictive of difficulty of of mandibular third
molar surgery. Br. Dent. J. 190 (2001), 607-610.
3. Yuasa, H, M Sugiura: Clinical postoperative
findings after removal of impacted mandibular
third molars: prediction of postoperative
facial swelling and pain based on preoperative
variables. Br. J. Oral. Maxillofac. Surg. 42
(2004), 209-214.
4. van der Westhuijzen, AJ, PJ Becker, J
Morkel, et al: A randomized observer blind
comparison of bilateral facial ice pack therapy
with no ice therapy following third molar
surgery. Int. J. Oral. Maxillofac. Surg. 34
(2005), 281-286.
5. Bamgbose, BO, JA Akinwande, WL Adeyemo,
et al: Effects of co-administered dexametha-
sone and diclofenac potassium on pain,
swelling and trismus following third molar
surgery. Head Face Med. 1 (2005), 11.
6. Graziani, F, L Corsi, M Fornai, et al: Clinical
evaluation of piroxicam-FDDF and azithro-
mycin in the prevention of complications
associated with impacted lower third molar
extraction. Pharmacol. Res. 52 (2005), 485-490.
7. Bjornsson, GA, HR Haanes, LA Skoglund:
A randomized, double-blind crossover trial
of paracetamol 1000 mg four times daily vs
ibuprofen 600 mg: Effect on swelling and
other postoperative events after third molar
surgery. Br. J. Clin. Pharmacol. 55 (2003),
405-412.
8. Amin, MM, DM Laskin: Prophylactic use of
indomethacin for prevention of postsurgical
complications after removal of impacted third
molars. Oral. Surg. Oral Med. Oral Pathol. 55
(1983), 448-451.
9. Schultze-Mosgau, S, R Schmelzeisen, JC
Frolich, et al: Use of ibuprofen and methyl-
prednisolone for the prevention of pain and
swelling after removal of impacted third
molars. J. Oral Maxillofac. Surg. 53 (1995), 2-7.
10. Fldi, M, S Kubik: Textbook of Lymphology.
Urban & Fischer 2002. pp 532-537.
11. Van Gool, AV, JJT Bosch, G Boreing: A
photographic method of assessing swelling
following third molar removal. Int. J. Oral
Surg. 4 (1975), 121-129.
12. Milles, M, PJ Desjardins, HE Pawel: The
facial plethismograph: A new instrument to
measure facial swelling volumetrically. J.
Oral Maxillofac. Surg. 43 (1985), 346-352.
13. Burke, PH: The accuracy and range of certain
stereophotographic measurement of facial
morphology. Trans. Eur. Orthod. Soc. (1972),
543-553.
14. Bjorn, H, C Lundquist, CE Hjelmstrom: A
photogrammetric method of measuring the
volume of facial swelling. J. Dent. Res. 33
(1954), 295.
15. Montebugnoli, L, D Servidio, RA Miaton,
et al: An objective method of assessing facial
swelling in patients with dental abscesses
treated with clarithromycin. Min. Stomatol.
53 (2004), 263-271.
16. Rakprasitkul, S, V Pairuchvej: Mandibular
third molar surgery with primary closure and
tube drain. Int. J. Oral. Maxillofac. Surg. 26
(1997), 187-190.
17. Laureano Filho, JR, ED de Oliveira e Silva,
CI Batista, et al: The influence of cryotherapy
on reduction of swelling, pain and trismus
after third-molar extraction: a preliminary
study. J. Am. Dent. Assoc. 136 (2005), 774-778.
18. Szolnoky, G, G Mohos, A Dobozy, L Kemeny:
Manual lymph drainage reduces trapdoor
effect in subcutaneous island pedicle flaps.
Int. J. Dermatol. 45 (2006), 1468-70.
Gyozo Szolnoky, MD, PhD
Department of Dermatology and Allergology
University of Szeged
P.O. BOX 427
H-6720 Szeged, Hungary
Tel: 36-20-326-6161
Fax: 36-62-545954
Email:
szolnoky@mail.derma.szote.u-szeged.hu
You might also like
- Flap Design and Mandibularthird Molar Surgery A Splitmouth Randomized Clinical StudyDocument5 pagesFlap Design and Mandibularthird Molar Surgery A Splitmouth Randomized Clinical StudyFatima SiddiquiNo ratings yet
- Piezosurgery Vs ConventionalDocument5 pagesPiezosurgery Vs ConventionalSaskia ParamitaNo ratings yet
- The Effect of Flap Design On Wound Healing After PDocument8 pagesThe Effect of Flap Design On Wound Healing After PGauri AroraNo ratings yet
- An Audit of Impacted Mandibular Third Molar SurgeryDocument5 pagesAn Audit of Impacted Mandibular Third Molar SurgeryChieAstutiaribNo ratings yet
- Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, And Endodontology Volume 93 Issue 1 2002 [Doi 10.1067_moe.2002.119519] Norbert Jakse; Vedat Bankaoglu; Gernot Wimmer; Antranik Eskici; -- Primary WounDocument6 pagesOral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, And Endodontology Volume 93 Issue 1 2002 [Doi 10.1067_moe.2002.119519] Norbert Jakse; Vedat Bankaoglu; Gernot Wimmer; Antranik Eskici; -- Primary WounMr-Ton DrgNo ratings yet
- Arto AtmDocument9 pagesArto AtmELIS JOHANA PATERNINA MOGUEANo ratings yet
- Oroantral Communications. A Retrospective Analysis: Josué Hernando, Lorena Gallego, Luis Junquera, Pedro VillarrealDocument5 pagesOroantral Communications. A Retrospective Analysis: Josué Hernando, Lorena Gallego, Luis Junquera, Pedro VillarrealPla ParichartNo ratings yet
- Dex For Dental Pain & SwellingDocument7 pagesDex For Dental Pain & Swellingandrew herring100% (1)
- Magnetic BBDocument7 pagesMagnetic BBVicente ContrerasNo ratings yet
- Eshghpour 2015Document7 pagesEshghpour 2015123No ratings yet
- Reliability of Two Surgical Methods For Oroantral Communication Closure A Clinical Study of 20 Patients 2161 119X.1000113Document4 pagesReliability of Two Surgical Methods For Oroantral Communication Closure A Clinical Study of 20 Patients 2161 119X.1000113AndreHidayatNo ratings yet
- Read The Following Abstract of The Journal and Answer The QuestionsDocument4 pagesRead The Following Abstract of The Journal and Answer The QuestionsNada Syafa TitaniaNo ratings yet
- Prognosis of Luxated Permanent Teeth - The Development of Pulp NecrosisDocument15 pagesPrognosis of Luxated Permanent Teeth - The Development of Pulp NecrosisFlorin IonescuNo ratings yet
- Read The Following Abstract of The Journal and Answer The QuestionsDocument3 pagesRead The Following Abstract of The Journal and Answer The QuestionsichaNo ratings yet
- Case Report: Modified and Grafted Coronectomy: A New Technique and A Case Report With Two-Year FollowupDocument7 pagesCase Report: Modified and Grafted Coronectomy: A New Technique and A Case Report With Two-Year FollowupMuhammad ArifNo ratings yet
- Atm ArtDocument6 pagesAtm ArtYessyka EscalanteNo ratings yet
- Infection of Impacted Lower ThirdDocument5 pagesInfection of Impacted Lower ThirdjoseluisNo ratings yet
- JC TopicDocument6 pagesJC Topicवाधूलं कण्णन् कुमारस्वामिNo ratings yet
- EscleroterápiaDocument5 pagesEscleroterápiaMario CastroNo ratings yet
- 1 s2.0 S0266435613004105 MainDocument5 pages1 s2.0 S0266435613004105 MainMr-Ton DrgNo ratings yet
- Conjunctival Autografting Combined With Low-Dose Mitomycin C For Prevention of Primary Pterygium RecurrenceDocument9 pagesConjunctival Autografting Combined With Low-Dose Mitomycin C For Prevention of Primary Pterygium RecurrenceNatalia LeeNo ratings yet
- Matijevi, M. 2012 PDFDocument7 pagesMatijevi, M. 2012 PDFFelipe RoncerosNo ratings yet
- Fixed Versus Removable Orthodontic Appliances To Correct Anterior Crossbite in The Mixed Dentition-A Randomized Controlled Trial PDFDocument6 pagesFixed Versus Removable Orthodontic Appliances To Correct Anterior Crossbite in The Mixed Dentition-A Randomized Controlled Trial PDFJejeNo ratings yet
- The Effect of One-Suture and Suture-Less Techniques On Post-Operative HealingDocument55 pagesThe Effect of One-Suture and Suture-Less Techniques On Post-Operative HealingMarco Antonio Miranda RodriguezNo ratings yet
- Management of Dry SocketDocument4 pagesManagement of Dry SocketFakhrul ImamNo ratings yet
- 904nm 0.6W - 12663 - 2013 - Article - 544Document7 pages904nm 0.6W - 12663 - 2013 - Article - 544Gino DammiuncrodinoNo ratings yet
- The Effect of Low-Level Laser Therapy On Orthodontically Induced Root Resorption - NG 17Document9 pagesThe Effect of Low-Level Laser Therapy On Orthodontically Induced Root Resorption - NG 17Antonio LoureiroNo ratings yet
- Coronectomy of Mandibular Third MolarsDocument2 pagesCoronectomy of Mandibular Third MolarsChalu TamuraNo ratings yet
- A Novel Proforma For Clinical and Radiographic Evaluation of Impacted Third Molars Prior To Surgical RemovalDocument9 pagesA Novel Proforma For Clinical and Radiographic Evaluation of Impacted Third Molars Prior To Surgical RemovalRNo ratings yet
- Gap ArthroplastyDocument5 pagesGap ArthroplastyMax FaxNo ratings yet
- Efficacy of Intra-Alveolar Chlorhexidine Gel in Reducing Frequency of Alveolar Osteitis in Mandibular Third Molar SurgeryDocument4 pagesEfficacy of Intra-Alveolar Chlorhexidine Gel in Reducing Frequency of Alveolar Osteitis in Mandibular Third Molar SurgeryCahyo AdyNo ratings yet
- Treatment of Condylar Fractures With An Intraoral ApproachDocument26 pagesTreatment of Condylar Fractures With An Intraoral Approachdhiraj.2367No ratings yet
- Cephx Invisalign PDFDocument9 pagesCephx Invisalign PDFVieussens JoffreyNo ratings yet
- Original ArticleDocument6 pagesOriginal ArticleWayan Sutresna YasaNo ratings yet
- OgundipeDocument6 pagesOgundipeIria GonzalezNo ratings yet
- Piezosurgery Versus Rotatory Osteotomy in Mandibular Impacted Third Molar ExtractionDocument17 pagesPiezosurgery Versus Rotatory Osteotomy in Mandibular Impacted Third Molar ExtractionHUYNH TRINHNo ratings yet
- Dexametasone Post OperativeDocument9 pagesDexametasone Post OperativeProfaceNo ratings yet
- DexametasonaDocument5 pagesDexametasonashveys_mNo ratings yet
- 8 - Clinical Outcome in Periradicular Surgery Effect of Patient - and Tooth-Related Factors - A Multicenter StudyDocument8 pages8 - Clinical Outcome in Periradicular Surgery Effect of Patient - and Tooth-Related Factors - A Multicenter StudykochikaghochiNo ratings yet
- The Surgical Removal of Mandibular Third Molars: A Study in Decision MakingDocument6 pagesThe Surgical Removal of Mandibular Third Molars: A Study in Decision MakingAmine AzzazNo ratings yet
- Quirurgico PDFDocument10 pagesQuirurgico PDFrosaNo ratings yet
- Univers Complu Madrid NBF - Cordales Alveolitis Por Extra.Document8 pagesUnivers Complu Madrid NBF - Cordales Alveolitis Por Extra.juan perezNo ratings yet
- 1 s2.0 S0720048X16300286Document6 pages1 s2.0 S0720048X16300286Yuda ArifkaNo ratings yet
- Assessment of Nerve Injuries after Tooth RemovalDocument5 pagesAssessment of Nerve Injuries after Tooth RemovaljamilatulmilaNo ratings yet
- Does Elastic Therapeutic Tape ReduceDocument10 pagesDoes Elastic Therapeutic Tape ReducegreynerNo ratings yet
- Short Nose Correction-By Man Koon SuhDocument4 pagesShort Nose Correction-By Man Koon SuhJW整形医院(JW plastic surgery)No ratings yet
- Rana M. 2011 PDFDocument7 pagesRana M. 2011 PDFFelipe RoncerosNo ratings yet
- Ultrasonography-Guided Arthrocentesis Versus ConventionalDocument10 pagesUltrasonography-Guided Arthrocentesis Versus ConventionalEduardo Garza GarzaNo ratings yet
- Holland 1984Document7 pagesHolland 1984Kyaw MoeNo ratings yet
- Jurnal 2Document6 pagesJurnal 2Dzaenap UlfahNo ratings yet
- Comparison of Microsurgical and Conventional Open Flap DebridementDocument9 pagesComparison of Microsurgical and Conventional Open Flap DebridementNoemi LukacsNo ratings yet
- The Learning Curve in Revision Cholesteatoma Surgery: Milan StankovicDocument7 pagesThe Learning Curve in Revision Cholesteatoma Surgery: Milan StankovicLia BirinkNo ratings yet
- Class NoteDocument25 pagesClass NoteHAMIDNo ratings yet
- Cju 005Document5 pagesCju 005gifar ihsanNo ratings yet
- Effectiveness of Physiotherapy and Gaalas Laser in The Management of Temporomandibular Joint DisordersDocument6 pagesEffectiveness of Physiotherapy and Gaalas Laser in The Management of Temporomandibular Joint DisordersjoserodrrNo ratings yet
- 1 s2.0 S0011853211000346 Main PDFDocument6 pages1 s2.0 S0011853211000346 Main PDFMichael XuNo ratings yet
- Elgelke Et Al Ift 2013Document7 pagesElgelke Et Al Ift 2013Deyvyd LimaNo ratings yet
- Treatment of Deep Caries LesionsDocument8 pagesTreatment of Deep Caries Lesionsrojek63No ratings yet
- Modified Gap Arthroplasty and Myrhaugs Incision As A Treatment Option in Management of Temporomandibular Joint Ankylosis A Study of 10 CasesDocument6 pagesModified Gap Arthroplasty and Myrhaugs Incision As A Treatment Option in Management of Temporomandibular Joint Ankylosis A Study of 10 CasesS EllurNo ratings yet
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Evaluación Por TC y RM de Tumores Orbitarios: Nuestra ExperienciaDocument10 pagesEvaluación Por TC y RM de Tumores Orbitarios: Nuestra ExperienciaFelipe RoncerosNo ratings yet
- Amorin Gomes A.C. 2005 PDFDocument4 pagesAmorin Gomes A.C. 2005 PDFFelipe RoncerosNo ratings yet
- Prolactina - RMDocument11 pagesProlactina - RMAlex PomaNo ratings yet
- Linfoma Cerebral Primario. Patrones ImagenológicosDocument6 pagesLinfoma Cerebral Primario. Patrones ImagenológicosFelipe RoncerosNo ratings yet
- Wahid A. 2013 PDFDocument3 pagesWahid A. 2013 PDFFelipe RoncerosNo ratings yet
- FREQUENCY OF NERVE INJURIES FOLLOWING EXTRACTION OF IMPACTED MANDIBULAR 3RD MOLARS, Ahmad T. 2013Document4 pagesFREQUENCY OF NERVE INJURIES FOLLOWING EXTRACTION OF IMPACTED MANDIBULAR 3RD MOLARS, Ahmad T. 2013Felipe RoncerosNo ratings yet
- Biopsia Radioquirúrgica de Mama en 2.060 Pacientes. Experiencia HospitalariaDocument6 pagesBiopsia Radioquirúrgica de Mama en 2.060 Pacientes. Experiencia HospitalariaFelipe RoncerosNo ratings yet
- Infarto Renal Agudo: Un Diagnóstico para Tener en CuentaDocument5 pagesInfarto Renal Agudo: Un Diagnóstico para Tener en CuentaFelipe RoncerosNo ratings yet
- Prolactina - RMDocument11 pagesProlactina - RMAlex PomaNo ratings yet
- General Technique of Third Molar Removal, Bouloux G.F. 2007Document21 pagesGeneral Technique of Third Molar Removal, Bouloux G.F. 2007Felipe Ronceros100% (1)
- Manual Lymph Drainage Efficiently Reduces Postoperative Facial Swelling and Discomfort After Removal of Impacted Third MolarsDocument5 pagesManual Lymph Drainage Efficiently Reduces Postoperative Facial Swelling and Discomfort After Removal of Impacted Third MolarsFelipe RoncerosNo ratings yet
- Oral Health Related Quality of Life Following Non Surgical (Routine) Tooth Extraction: A Pilot StudyDocument6 pagesOral Health Related Quality of Life Following Non Surgical (Routine) Tooth Extraction: A Pilot StudyFelipe RoncerosNo ratings yet
- Meshram V.S. 2013Document7 pagesMeshram V.S. 2013Felipe RoncerosNo ratings yet
- TRAIT ANXIETY, SEX, AGE AND DENTAL TREATMENT EXPERIENCE AS DETERMINANTS OF DENTAL ANXIETY AMONG CHRONIC DENTAL PATIENTS IN NIGERIA, Akhigbe K.O. 2014Document13 pagesTRAIT ANXIETY, SEX, AGE AND DENTAL TREATMENT EXPERIENCE AS DETERMINANTS OF DENTAL ANXIETY AMONG CHRONIC DENTAL PATIENTS IN NIGERIA, Akhigbe K.O. 2014Felipe RoncerosNo ratings yet
- Huang G.J. 2014Document8 pagesHuang G.J. 2014Felipe RoncerosNo ratings yet
- Queral-Godoy E. 2006 PDFDocument6 pagesQueral-Godoy E. 2006 PDFFelipe RoncerosNo ratings yet
- Sefvan Janjua O. 2013 PDFDocument5 pagesSefvan Janjua O. 2013 PDFFelipe RoncerosNo ratings yet
- Watbson R. 2011 PDFDocument8 pagesWatbson R. 2011 PDFFelipe RoncerosNo ratings yet
- Robinson P.P. 2000 PDFDocument9 pagesRobinson P.P. 2000 PDFFelipe RoncerosNo ratings yet
- Srinivas M. Susarla. 2003 PDFDocument10 pagesSrinivas M. Susarla. 2003 PDFFelipe RoncerosNo ratings yet
- Vares Y. 2014 PDFDocument8 pagesVares Y. 2014 PDFFelipe RoncerosNo ratings yet
- Renton T PDFDocument5 pagesRenton T PDFFelipe RoncerosNo ratings yet
- Rana M. 2011 PDFDocument7 pagesRana M. 2011 PDFFelipe RoncerosNo ratings yet
- Rafetto L. K. 2012 PDFDocument2 pagesRafetto L. K. 2012 PDFFelipe Ronceros100% (1)
- Bello S.A. 2011 PDFDocument8 pagesBello S.A. 2011 PDFFelipe RoncerosNo ratings yet
- White Paper On Third Molar DataDocument25 pagesWhite Paper On Third Molar DataVinay KumarNo ratings yet
- AAOMS Age Related 3rd Molar StudyDocument9 pagesAAOMS Age Related 3rd Molar StudyVikas VatsNo ratings yet
- Rehman K. 2002 PDFDocument3 pagesRehman K. 2002 PDFFelipe RoncerosNo ratings yet
- Rehman K. 2002 PDFDocument1 pageRehman K. 2002 PDFFelipe RoncerosNo ratings yet




![Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, And Endodontology Volume 93 Issue 1 2002 [Doi 10.1067_moe.2002.119519] Norbert Jakse; Vedat Bankaoglu; Gernot Wimmer; Antranik Eskici; -- Primary Woun](https://imgv2-1-f.scribdassets.com/img/document/224676744/149x198/8c2fa96a30/1400316861?v=1)