Professional Documents
Culture Documents
ACLS-Study-Guide-2011 MADE EASY
Uploaded by
Frances Albaña TevesCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ACLS-Study-Guide-2011 MADE EASY
Uploaded by
Frances Albaña TevesCopyright:
Available Formats
ACLS Study Guide 2011
See www.heart.org/eccstudent. The code is found in the ACLS Provider Manual page ii.
The ACLS Provider exam is 50-mutiple choice questions. Passing score is 84%. Student may miss 8 questions. For
students taking ACLS for the first time or renewing students with a current card, exam remediation is permitted should
student miss more than 8 questions on the exam. Viewing the ACLS book ahead of time with the online resources is
very helpful. The American Heart Association link is www.heart.org/eccstudent and has an ACLS Precourse SelfAssessment, supplementary written materials and videos. The code for the online resources is on the ACLS Provider
Manual page ii. Basic Dysrhythmias knowledge is required in relation to asystole, ventricular fibrillation, tachycardias
in general and bradycardias in general. Student does not need to know the ins and outs of each and every one. For
Tachycardias student need to differentiate wide complex (ventricular tachycardia) and narrow complex
(supraventricular tachycardia or SVT).
BLS Overview CAB
Stroke
Cincinnati Pre-Hospital Stroke Scale
Facial Droop, Arm Drift,
Abnormal Speech
Push Hard and Fast-Repeat every 2 minutes
Anytime there is no pulse or unsure about a pulse do
COMPRESSIONS
Elements of good CPR
Rate-at least 100
Recoil
Compression depth at least 2 inches
Minimize interruptions (less than 10 seconds)
Avoid excessive ventilation
Switch compressors every 2 min or 5 cycles
If AED doesnt promptly analyze rhythm: compressions.
rtPA can be given within 3 hours from symptom onset.
Important to transport patient to an appropriate
hospital with CT capabilities. If CT not available divert to
the closest hospital (i.e. 15 min away) with CT
Acute Coronary Syndromes
Vital signs, 02, IV,
12 Lead for CP, epigastric pain, or rhythm change
Defibrillation
Tachycardia with a Pulse
If unstable (wide or narrow) - go straight to
synchronized cardioversion
If stable narrow complex
obtain 12 lead
vagal maneuvers
adenosine 6mg RAPID IVP, followed by 12mg
Courtesy Terry Rudd RN, MSN
Key Medical Resources Inc.
November 2011, Page 1
Waveform Capnography in ACLS (PETCO2)
Allows for accurate monitoring of CPR
Most reliable indicator for ET tube placement
Bradycardia
Need to assess stable versus unstable.
If stable, monitor, observe, and consult.
If unstable. . .
Atropine 0.5mg IV. Can repeat Q3-5 minutes.
Maximum dose=3mg (Including heart blocks)
If Atropine ineffective
Transcutaneous pacing
Dopamine infusion (2-10mcg/kg/min)
Epinephrine infusion (2-10mcg/min)
Cardiac Arrest
Shockable Rhythms:
Ventricular Fibrillation (VF)
Ventricular Tachycardia (VT) without pulse
Return of Spontaneous Circulation (ROSC)
Post Resuscitation Care
Biphasic: 120-200J Monophasic: 360J
Non-Shockable Rhythms:
PEA
Asystole
2 minute cycles of compressions, shocks (if
VF/VT), and rhythm checks.
Epi 1 mg every 3-5 minutes (preferred method IV)
NO MORE ATROPINE for Asystole and PEA
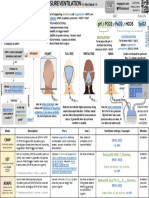
Ventilations 30:2 Ratio
Rescue breathing 1 breath every 5-6 sec
If advanced airway 8-10 ventilations/minute
Treat reversible causes (Hs and Ts)
Hypoxia or ventilation problems
Hypovolemia
Hypothermia
Hypo-/hyper-kalemia
Hydrogen ion (acidosis)
Tamponade, cardiac
Tension pneumothorax
Toxins poisons, drugs
Thrombosis coronary (AMI) pulmonary (PE)
Points to Ponder
COMPRESSIONS are very important.
Rigor mortis is an indicator of termination of efforts.
Simple airway maneuvers, such as a head-tilt, may
help.
The Medical Emergency Teams (MET) can identify and
treat pre-arrest situations.
Consider terminating efforts after deterioration to
asystole and prolonged resuscitation time.
Courtesy Terry Rudd RN, MSN
Key Medical Resources Inc.
November 2011, Page 2
You might also like
- Music Theory Worksheet 1 The StaffDocument1 pageMusic Theory Worksheet 1 The StaffFrances Albaña TevesNo ratings yet
- Ele&Arr&Com&Rev&Das&Zip&1 STDocument492 pagesEle&Arr&Com&Rev&Das&Zip&1 STeuinpersoana100% (3)
- Beyond The Basics of Respiratory Care - Anatomy, Physiology, Evaluation and Intervention PDFDocument56 pagesBeyond The Basics of Respiratory Care - Anatomy, Physiology, Evaluation and Intervention PDFMarie Petalcorin100% (1)
- A Primer of ECG (Gnv64)Document100 pagesA Primer of ECG (Gnv64)Viju K G100% (1)
- Music Theory Worksheet 2 Staff High LowDocument1 pageMusic Theory Worksheet 2 Staff High LowJosé Miguel Méndez0% (1)
- Pic PALS PDFDocument57 pagesPic PALS PDFJimcyNo ratings yet
- ACLS Algorithms Adult 2010 Revised May 31 2011Document12 pagesACLS Algorithms Adult 2010 Revised May 31 2011arturschander3614No ratings yet
- ECG Masters' Collection Volume 2Document218 pagesECG Masters' Collection Volume 2Илија Радосављевић100% (1)
- Children's Healthcare of Atlanta PICU Orientation ManualDocument18 pagesChildren's Healthcare of Atlanta PICU Orientation ManualdmallozziNo ratings yet
- DYSRHYTHMIASDocument9 pagesDYSRHYTHMIASgudobenNo ratings yet
- Pacing ManualDocument76 pagesPacing ManualMirela Sfaraiala LuculescuNo ratings yet
- Respiratory Therapist or Respiratory Care PractitionerDocument2 pagesRespiratory Therapist or Respiratory Care Practitionerapi-77419731No ratings yet
- NIPPVDocument35 pagesNIPPVAnusha VergheseNo ratings yet
- ECG Clinical TeachingDocument21 pagesECG Clinical TeachingSumi SajiNo ratings yet
- Fluid and Electrolyte Balance in ICUDocument46 pagesFluid and Electrolyte Balance in ICUtapas_kbNo ratings yet
- Cardiac ArrhythmiasDocument11 pagesCardiac ArrhythmiasChino Paolo SamsonNo ratings yet
- American Heart Association Guidelines For CPR 2015: Christopher RyalinoDocument50 pagesAmerican Heart Association Guidelines For CPR 2015: Christopher RyalinoLightNo ratings yet
- Respiratory Therapist, NICU/ICUDocument5 pagesRespiratory Therapist, NICU/ICUapi-77517256No ratings yet
- ACLS Practical Case Scenarios (1 June 2011)Document15 pagesACLS Practical Case Scenarios (1 June 2011)nersNo ratings yet
- Sinus ArrhythmiaDocument6 pagesSinus ArrhythmiaVincent Maralit MaterialNo ratings yet
- ECG quiz STEMI PEA adrenaline sodium bicarbonate CPR DNACPRDocument5 pagesECG quiz STEMI PEA adrenaline sodium bicarbonate CPR DNACPRS Vaibhav100% (2)
- Assessment Algorithm For Sedated Adult ICU Patients: No YesDocument18 pagesAssessment Algorithm For Sedated Adult ICU Patients: No YeshendraNo ratings yet
- Long QT SyndromeDocument6 pagesLong QT SyndromeJ M NoronhaNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Cardiac Arrest: Asystole, PEADocument27 pagesCardiac Arrest: Asystole, PEAMateas ZsoltNo ratings yet
- PEDIATRIC ASSESSMENT OVERVIEWDocument2 pagesPEDIATRIC ASSESSMENT OVERVIEWAghnia Nafila100% (1)
- Pediatric Respiratory EmergenciesDocument68 pagesPediatric Respiratory EmergenciesPAKINUGNo ratings yet
- Acls Provider: Advanced Cardiovascular Life SupportDocument1 pageAcls Provider: Advanced Cardiovascular Life SupportmaraínaNo ratings yet
- Intra Aortic Ballon Pump FlowsheetDocument2 pagesIntra Aortic Ballon Pump FlowsheetYudi Aryasena Radhitya PurnomoNo ratings yet
- ACLS Secondary Survey For A Patient in Respiratory Arrest: BLS Arrest Figure 1. Basic Life Support Primary SurveyDocument30 pagesACLS Secondary Survey For A Patient in Respiratory Arrest: BLS Arrest Figure 1. Basic Life Support Primary SurveyLusia NataliaNo ratings yet
- ACLS DrugsDocument4 pagesACLS DrugsEduard Espeso Chiong-Gandul Jr.No ratings yet
- ECMO Monitoring - PediatrikDocument24 pagesECMO Monitoring - PediatrikIsran IsRanNo ratings yet
- Basic Mechanical Ventilation 2014Document62 pagesBasic Mechanical Ventilation 2014dragon66No ratings yet
- 2011 BLS HCP Exam BinderDocument24 pages2011 BLS HCP Exam Bindermag griffNo ratings yet
- CPR ACLS Study GuideDocument18 pagesCPR ACLS Study GuideJohn Phamacy100% (1)
- CONCEPT - QuestionsDocument2 pagesCONCEPT - Questionsgreen_archerNo ratings yet
- Mitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandMitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Antrim ED Handbook 2019Document238 pagesAntrim ED Handbook 2019Chris Jardine LiNo ratings yet
- Tachyarrhythmias When Should I Refer?Document25 pagesTachyarrhythmias When Should I Refer?Cindy Seow Sieng TengNo ratings yet
- Megacode Testing Checklist: Scenarios 1/3/8 Bradycardia Pulseless VT PEA PCACDocument6 pagesMegacode Testing Checklist: Scenarios 1/3/8 Bradycardia Pulseless VT PEA PCACberril_fannyNo ratings yet
- Pathophysiology Course: Muscle (More Uid) Body Fat (Less Uid) Gender (Men Retain More Uid) AgeDocument1 pagePathophysiology Course: Muscle (More Uid) Body Fat (Less Uid) Gender (Men Retain More Uid) AgePaola OrtizNo ratings yet
- Respiratory Therapy Cave - Ventilator Graphics Cheat SheetDocument2 pagesRespiratory Therapy Cave - Ventilator Graphics Cheat SheetMarwa El-DegwiNo ratings yet
- PFT NotesDocument8 pagesPFT NotesJade Louise FkshmNo ratings yet
- Critical Thinking in Respiratory Care Practice PDFDocument17 pagesCritical Thinking in Respiratory Care Practice PDFFernando MorenoNo ratings yet
- ICU One Pager EVD V11Document1 pageICU One Pager EVD V11Mohamed Mahmoud100% (1)
- Registered Respiratory TherapistDocument3 pagesRegistered Respiratory Therapistapi-76909521No ratings yet
- Advanced Cardiac Life SupportDocument37 pagesAdvanced Cardiac Life SupportRoy Acosta GumbanNo ratings yet
- ACLS Study Guide for Saving LivesDocument19 pagesACLS Study Guide for Saving LivesCARTAGENA1No ratings yet
- 2 Respiretory SystemDocument19 pages2 Respiretory SystemJ WobNo ratings yet
- Scape Vs FospeDocument5 pagesScape Vs FospeDr. FarhanNo ratings yet
- Invasive Devices On CXRDocument1 pageInvasive Devices On CXRLaurensia Erlina NataliaNo ratings yet
- Internship Manual For MBBSDocument29 pagesInternship Manual For MBBSKoustav ChakrabortyNo ratings yet
- NON-INVASIVE VENTILATION GUIDEDocument1 pageNON-INVASIVE VENTILATION GUIDENicholas HelmstetterNo ratings yet
- 19-Respiratory MedicineDocument2 pages19-Respiratory MedicineIbrahimFikryNo ratings yet
- 6 DefibrillationDocument22 pages6 DefibrillationrohithNo ratings yet
- Notes For Clincal CasesDocument12 pagesNotes For Clincal CasesMandeepNo ratings yet
- Pulmo ThromboembolismDocument34 pagesPulmo ThromboembolismAlexander Santiago ParelNo ratings yet
- Acls Course HandoutsDocument8 pagesAcls Course HandoutsRoxas CedrickNo ratings yet
- Neurological Assessment Guide for Respiratory CareDocument33 pagesNeurological Assessment Guide for Respiratory CareArifurRahman100% (1)
- Neurologic Assessment RationaleDocument16 pagesNeurologic Assessment RationaleflorenzoNo ratings yet
- Agenda Bls-AclsDocument2 pagesAgenda Bls-AclsespegehNo ratings yet
- Megacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...Document1 pageMegacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...krgduraiNo ratings yet
- Atelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Document10 pagesAtelectasis: Contraction Atelectasis (Or Cicatrization Atelectasis)Gan BangNo ratings yet
- 8.the Atls ProtocolDocument57 pages8.the Atls ProtocolReuben DutiNo ratings yet
- PALS Pulseless Arrest Algorithm: Kleinman, M. E. Et Al. Circulation 2010 122:S876-S908Document3 pagesPALS Pulseless Arrest Algorithm: Kleinman, M. E. Et Al. Circulation 2010 122:S876-S908YONE LENINNo ratings yet
- PALS Precourse Self-Assessment Score ReportDocument3 pagesPALS Precourse Self-Assessment Score ReportAde Novian ParmudityaNo ratings yet
- Best Practice in ShockDocument30 pagesBest Practice in ShockFoungZanz D. LuffyzNo ratings yet
- Cardiac/Cardiogenic Shock: Clinical Practice GuidelinesDocument3 pagesCardiac/Cardiogenic Shock: Clinical Practice GuidelinesAnonymous Yo0mStNo ratings yet
- The Ins and Outs of Ventilation 2. Mechanical VentilatorsDocument9 pagesThe Ins and Outs of Ventilation 2. Mechanical VentilatorsjhonvetNo ratings yet
- Symptom Flow Chart (Difficulty Breathing)Document2 pagesSymptom Flow Chart (Difficulty Breathing)Jeff ZhouNo ratings yet
- Vascular Responses to PathogensFrom EverandVascular Responses to PathogensFelicity N.E. GavinsNo ratings yet
- BT ReactionsDocument1 pageBT ReactionsFilipino Nurses CentralNo ratings yet
- Writing Smart GoalsDocument3 pagesWriting Smart Goalsapi-248460396No ratings yet
- EXO Miracles in December Sheet Music TranscriptionDocument7 pagesEXO Miracles in December Sheet Music TranscriptionNajwa MNoor100% (2)
- English Essay FamilyDocument1 pageEnglish Essay FamilyFrances Albaña TevesNo ratings yet
- EKG Quick Reference Chart PDFDocument4 pagesEKG Quick Reference Chart PDFrodney subaranNo ratings yet
- Ecg PediaDocument2 pagesEcg PediaAdrian Ulu100% (1)
- ZOLL-M2 BrochureDocument2 pagesZOLL-M2 BrochureManzar SaleemNo ratings yet
- Aria2 Script.23555Document18 pagesAria2 Script.23555MD Saif SiddNo ratings yet
- Cardiac Arrhythmia GuideDocument93 pagesCardiac Arrhythmia GuideEdalyn CapiliNo ratings yet
- An Interesting Case of "Trigeminal Tachycardia"Document3 pagesAn Interesting Case of "Trigeminal Tachycardia"ABDULLAH ALHASANNo ratings yet
- Kuliah Pakar EKG - Ferdy Lainsamputty (@unsrit)Document31 pagesKuliah Pakar EKG - Ferdy Lainsamputty (@unsrit)akreditasi pkmkakas22No ratings yet
- ACLS Tachycardia Algorithm For Managing Stable TachycardiaDocument4 pagesACLS Tachycardia Algorithm For Managing Stable TachycardiaizkalotlNo ratings yet
- Prescriber - 2020 - Barton - Classification and Choice of Antiarrhythmic TherapiesDocument7 pagesPrescriber - 2020 - Barton - Classification and Choice of Antiarrhythmic TherapiesCarlos Eduardo GómezNo ratings yet
- Conduction System of Heart and Temporary PacemakerDocument23 pagesConduction System of Heart and Temporary Pacemakersmruti prakash SahuNo ratings yet
- Brugada Review Jacc 2018 PDFDocument14 pagesBrugada Review Jacc 2018 PDFanon422No ratings yet
- Mechanisms of Cardiac Arrhythmias From Automatici+Document24 pagesMechanisms of Cardiac Arrhythmias From Automatici+Malar MannanNo ratings yet
- Ecg Level 3 Precise Calculation of Cardiac AxisDocument44 pagesEcg Level 3 Precise Calculation of Cardiac Axismoneer chanceNo ratings yet
- 2014 CCM Review Notes Jon-Emile S. Kenny M.D, 2014Document142 pages2014 CCM Review Notes Jon-Emile S. Kenny M.D, 2014PkernNo ratings yet
- Cardiopulmonary Arrest Simulation LabDocument3 pagesCardiopulmonary Arrest Simulation LabJessica Mason100% (2)
- Normal ECGDocument2 pagesNormal ECGGeneon100% (1)
- Unipulse400 Manual Rev2 PDF 61951fd308992Document97 pagesUnipulse400 Manual Rev2 PDF 61951fd308992Álvaro TorresNo ratings yet
- Flash CardsDocument35 pagesFlash CardsMihaela AlexandraNo ratings yet
- Ventricular ArrhythmiaDocument37 pagesVentricular Arrhythmiaelhassia elhassiaNo ratings yet
- Conducting System of The HeartDocument68 pagesConducting System of The HeartNilay PatelNo ratings yet