Professional Documents
Culture Documents
Dengue Hemorrhagic Fever
Uploaded by
Ong Hooi FanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dengue Hemorrhagic Fever
Uploaded by
Ong Hooi FanCopyright:
Available Formats
1
INTRODUCTION
Dengue is a mosquito-borne disease caused by any one of four closely related
dengue viruses (DENV-1, -2, -3 and -4). Infection with one serotype of DENV provides
immunity to that serotype for life, but provides no long-term immunity to other
serotypes. Thus, a person can be infected as many as four times, once with each
serotype. Dengue viruses are transmitted from person to person by Aedes mosquitoes (
most often Aedes aegypti ) in the domestic environment.5
Dengue Haemorrhagic Fever (also known as Severe Dengue) was first
recognized in the 1950s during dengue epidemics in the Philippines and Thailand.
Today, severe dengue affects most Asian and Latin American countries and has become
a leading cause of hospitalization and death among children in these regions. Typical
cases of DHF are characterized by four major clinical manifestations : high fever,
haemorrhagic phenomena, and often, hepatomegaly and circulatory failure.1
In 2013, cases have occurred in Florida (United States of America) and Yunnan
province of China. Dengue also continues to affect several south American countries
notably Honduras, Costa Rica and Mexico. In Asia, Singapore has reported an increase
in cases after a lapse of several years and outbreaks have also been reported in Laos. In
2014, trends indicate increases in the number of cases in the Cook Islands, Malaysia,
Fiji and Vanuatu, with Dengue Type 3 (DEN 3) affecting the Pacific Island countries
after a lapse of over 10 years.1
An estimated 500 000 people with severe dengue require hospitalization each
year, a large proportion of whom are children. About 2.5% of those affected die.2
Transmission
WHO/TDR/Stammers
The Aedes aegypti mosquito is the primary vector of dengue. The virus is
transmitted to humans through the bites of infected female mosquitoes. After virus
incubation for 410 days, an infected mosquito is capable of transmitting the virus for
the rest of its life. Infected humans are the main carriers and multipliers of the virus,
serving as a source of the virus for uninfected mosquitoes. Patients who are already
infected with the dengue virus can transmit the infection (for 45 days; maximum 12)
via Aedes mosquitoes after their first symptoms appear.2
The Aedes aegypti mosquito lives in urban habitats and breeds mostly in manmade containers. Unlike other mosquitoes Ae. aegypti is a daytime feeder; its peak
biting periods are early in the morning and in the evening before dusk. Female Ae.
aegypti bites multiple people during each feeding period. Aedes albopictus, a secondary
dengue vector in Asia, has spread to North America and Europe largely due to the
international trade in used tyres (a breeding habitat) and other goods (e.g. lucky
bamboo). Ae. albopictus is highly adaptive and therefore can survive in cooler
temperate regions of Europe. Its spread is due to its tolerance to temperatures below
freezing, hibernation, and ability to shelter in microhabitats.2
Characteristics
Dengue fever is a severe, flu-like illness that affects infants, young children and
adults, but seldom causes death. Dengue should be suspected when a high fever (40C/
104F) is accompanied by two of the following symptoms: severe headache, pain
behind the eyes, muscle and joint pains, nausea, vomiting, swollen glands or rash.
Symptoms usually last for 27 days, after an incubation period of 410 days after the
bite from an infected mosquito.3
Severe dengue (DHF) is a potentially deadly complication due to plasma
leaking, fluid accumulation, respiratory distress, severe bleeding, or organ impairment.
Warning signs occur 37 days after the first symptoms in conjunction with a decrease in
temperature (below 38C/ 100F) and include: severe abdominal pain, persistent
vomiting, rapid breathing, bleeding gums, fatigue, restlessness, blood in vomit. The next
2448 hours of the critical stage can be lethal; proper medical care is needed to avoid
complications and risk of death.2,3
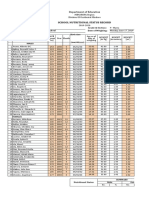
EPIDEMIOLOGY
Dengue fever (DF) is the fastest emerging arboviral infection spread by Aedes
aegypti mosquitoes with major public health consequences for millions of people
around the world, and in particular the South-East Asia and Asia-Pacific Regions of the
World Health Organization (WHO). Of the 2.5 billion people globally at risk of DF and
its severe forms dengue haemorrhagic fever (DHF) and dengue shock syndrome (DSS)
South-East Asia accounts for approximately 1.3 billion or 52%. As the disease spreads
to new geographical areas, the frequency of the outbreaks has increased along with a
rapidly changing disease epidemiology.7
A dengue epidemic requires the presence of :
The vector mosquito (usually Aedes aegypti).
The dengue virus.
A large number of susceptible human hosts.
CLASSIFICATION
The 1997 WHO classification of dengue virus infection2
The 2009 revised dengue case classification3
Grading severity of dengue haemorrhagic fever
DHF is classified into four grades of severity, where grades III and IV are
considered to be DSS. The presence of thrombocytopenia with concurrent
haemoconcentration differentiates grades I and II DHF from DF.4
Grade I: Fever accompanied by non-specific constitutional symptoms; the only
haemorrhagic manifestation is a positive tourniquet test and/or easy bruising.
Grade II: Spontaneous bleeding in addition to the manifestations of Grade I patients,
usually in the forms of skin or other haemorrhages.
Grade III: Circulatory failure manifested by a rapid, weak pulse and narrowing of pulse
pressure or hypotension, with the presence of cold, clammy skin and restlessness.
Grade IV: Profound shock with undetectable blood pressure or pulse. Grading the
severity of the disease at the time of discharge has been found clinically and
epidemiologically useful in DHF epidemics in children in the WHO Regions of the
Americas, South-East Asia and the Western Pacific, and experience in Cuba, Puerto
Rico and Venezuela suggests that grading is also useful for adult cases.4
CLINICAL FEATURES & DIAGNOSIS
WHO 1997 case definitions for DF, DHF and DSS2
Dengue Fever
Probable
- An acute febrile illness with two or more of the following manifestations: headache,
retro-orbital pain, myalgia, arthralgia, rash, haemorrhagic manifestations and leucopenia
And
- Supportive serology (a reciprocal haemagglutination-inhibition antibody titre 1280, a
comparable IgG enzyme-linked immunosorbent assay (ELISA) titre or a positive IgM
antibody test on a late acute or convalescent-phase serum specimen)
Or
- Occurrence at the same location and time as other DF cases
Confirmed
A case confirmed by one of the following laboratory criteria :
- Isolation of the dengue virus from serum or autopsy samples
- An at least four-fold change in reciprocal IgG/IgM titres to one or more dengue virus
antigens in paired samples
- Demonstration of dengue virus antigen in autopsy tissue, serum or cerebrospinal fluid
samples by immunohistochemistry, immunofluorescence or ELISA
- Detection of dengue virus genomic sequences in autopsy tissue serum or cerebrospinal
fluid samples by polymerase chain reaction (PRC)
Reportable
- Any probable or confirmed case should be reported
Dengue Hemorrhagic Fever
For a diagnosis of DHF, a case must meet all four of the following criteria :
- Fever or history of fever lasting 2-7 days, occasionally biphasic
- A haemorrhagic tendency shown by at least one of the following :
A positive tourniquet test
Petechiae, ecchymoses or purpura
Bleeding from the mucosa, gastro-intestinal tract, injection sites or other
locations
Haematemesis or melaena
- Thrombocytopenia 100,000 cells/mm3 (100x109/L)
- Evidence of plasma leakage owing to increased vascular permeability shown by:
An increase in haematocrit 20% above average for age, sex and population
A decrease in the haematocrit after intervention 20% of baseline
Signs of plasma leakage such as pleural effusion, ascites or hypoproteinaemia
Dengue Shock Syndrome
For a case of DSS, all four criteria for DHF must be met, in addition to evidence of
circulatory failure manifested by :
- Rapid and weak pulse
And
- Narrow pulse pressure (< 20 mmHg or 2-7 kPa)
Or manifested by
- Hypotension for age
And
- Cold, clammy skin and restlessness
The Course of Dengue Illness4
Febrile phase4
Patients typically develop high-grade fever suddenly. This acute febrile phase
usually lasts 27 days and is often accompanied by facial flushing, skin erythema,
generalized body ache, myalgia, arthralgia and headache. Some patients may have sore
throat, injected pharynx and conjunctival injection. Anorexia, nausea and vomiting are
common. It can be difficult to distinguish dengue clinically from non-dengue febrile
diseases in the early febrile phase. A positive tourniquet test in this phase increases the
probability of dengue. In addition, these clinical features are indistinguishable between
severe and non-severe dengue cases. Therefore monitoring for warning signs and other
clinical parameters is crucial to recognizing progression to the critical phase. Mild
haemorrhagic manifestations like petechiae and mucosal membrane bleeding (e.g. nose
and gums) may be seen. Massive vaginal bleeding (in women of childbearing age) and
gastrointestinal bleeding may occur during this phase but is not common. The liver is
often enlarged and tender after a few days of fever. The earliest abnormality in the full
blood count is a progressive decrease in total white cell count, which should alert the
physician to a high probability of dengue.
Critical phase
Around the time of defervescence, when the temperature drops to 37.538oC or
less and remains below this level, usually on days 37 of illness, an increase in capillary
permeability in parallel with increasing haematocrit levels may occur. This marks the
beginning of the critical phase. The period of clinically significant plasma leakage
usually lasts 2448 hours. Progressive leukopenia followed by a rapid decrease in
platelet count usually precedes plasma leakage. At this point patients without an
increase in capillary permeability will improve, while those with increased capillary
permeability may become worse as a result of lost plasma volume. The degree of
plasma leakage varies. Pleural effusion and ascites may be clinically detectable
depending on the degree of plasma leakage and the volume of fluid therapy. Hence
chest x-ray and abdominal ultrasound can be useful tools for diagnosis. The degree of
increase above the baseline haematocrit often reflects the severity of plasma leakage.
Shock occurs when a critical volume of plasma is lost through leakage. It is often
preceded by warning signs. The body temperature may be subnormal when shock
occurs. With prolonged shock, the consequent organ hypoperfusion results in
progressive organ impairment, metabolic acidosis and disseminated intravascular
coagulation. This in turn leads to severe haemorrhage causing the haematocrit to
decrease in severe shock. Instead of the leukopenia usually seen during this phase of
dengue, the total white cell count may increase in patients with severe bleeding. In
addition, severe organ impairment such as severe hepatitis, encephalitis or myocarditis
and/or severe bleeding may also develop without obvious plasma leakage or shock.
Those who improve after defervescence are said to have non-severe dengue. Some
patients progress to the critical phase of plasma leakage without defervescence and, in
these patients, changes in the full blood count should be used to guide the onset of the
critical phase and plasma leakage.
Those who deteriorate will manifest with warning signs. This is called dengue
with warning signs. Cases of dengue with warning signs will probably recover with
early intravenous rehydration. Some cases will deteriorate to severe dengue.
Recovery phase 4
If the patient survives the 2448 hour critical phase, a gradual reabsorption of
extravascular compartment fluid takes place in the following 4872 hours. General
well-being improves, appetite returns, gastrointestinal symptoms abate, haemodynamic
status stabilizes and diuresis ensues. Some patients may have a rash of isles of white in
the sea of red. Some may experience generalized pruritus. Bradycardia and
electrocardiographic changes are common during this stage. The haematocrit stabilizes
or may be lower due to the dilutional effect of reabsorbed fluid. White blood cell count
usually starts to rise soon after defervescence but the recovery of platelet count is
typically later than that of white blood cell count.Respiratory distress from massive
pleural effusion and ascites will occur at any time if excessive intravenous fluids have
been administered. During the critical and/or recovery phases, excessive fluid therapy is
associated with pulmonary oedema or congestive heart failure.
The various clinical problems during the different phases of dengue can be summarized
as in Table 2.1
Table 2.1 Febrile, critical and recovery phases in dengue
1 Febrile phase
Dehydration; high fever may cause neurological disturbances and febrile seizures in
young children.
2 Critical phase
Shock from plasma leakage; severe haemorrhage; organ impairment
3 Recovery phase
Hypervolaemia (only if intravenous fluid therapy has been excessive and/or has
extended into this period)
10
Severe dengue 4
Severe dengue is defined by one or more of the following:
(i) plasma leakage that may lead to shock (dengue shock) and/or fluid accumulation,
with or without respiratory distress, and/or
(ii) severe bleeding, and/or
(iii) severe organ impairment.
As dengue vascular permeability progresses, hypovolaemia worsens and results
in shock. It usually takes place around defervescence, usually on day 4 or 5 (range days
37) of illness, preceded by the warning signs. During the initial stage of shock, the
compensatory mechanism which maintains a normal systolic blood pressure also
produces tachycardia and peripheral vasoconstriction with reduced skin perfusion,
resulting in cold extremities and delayed capillary refill time. Uniquely, the diastolic
pressure rises towards the systolic pressure and the pulse pressure narrows as the
peripheral vascular resistance increases. Patients in dengue shock often remain
conscious and lucid. The inexperienced physician may measure a normal systolic
pressure and misjudge the critical state of the patient. Finally, there is decompensation
and both pressures disappear abruptly. Prolonged hypotensive shock and hypoxia may
lead to multi-organ failure and an extremely difficult clinical course (Textbox D). The
patient is considered to have shock if the pulse pressure (i.e. the difference between the
systolic and diastolic pressures) is 20 mm Hg in children or he/she has signs of poor
capillary perfusion (cold extremities, delayed capillary refill, or rapid pulse rate). In
adults, the pulse pressure of 20 mm Hg may indicate a more severe shock.
Hypotension is usually associated with prolonged shock which is often complicated by
major bleeding. Patients with severe dengue may have coagulation abnormalities, but
these are usually not sufficient to cause major bleeding. When major bleeding does
occur, it is almost always associated with profound shock since this, in combination
with thrombocytopaenia, hypoxia and acidosis, can lead to multiple organ failure and
advanced disseminated intravascular coagulation. Massive bleeding may occur without
prolonged shock in instances when acetylsalicylic acid (aspirin), ibuprofen or
corticosteroids have been taken.
11
Unusual manifestations, including acute liver failure and encephalopathy, may be
present, even in the absence of severe plasma leakage or shock. Cardiomyopathy and
encephalitis are also reported in a few dengue cases. However, most deaths from dengue
occur in patients with profound shock, particularly if the situation is complicated by
fluid overload.
Severe dengue should be considered if the patient is from an area of dengue risk
presenting with fever of 27 days plus any of the following features:
There is evidence of plasma leakage, such as:
high or progressively rising haematocrit;
pleural effusions or ascites;
circulatory compromise or shock (tachycardia, cold and clammy extremities, capillary
refill time greater than three seconds, weak or undetectable pulse, narrow pulse pressure
or, in late shock, unrecordable blood pressure).
There is significant bleeding.
There is an altered level of consciousness (lethargy or restlessness,coma, convulsions).
There is severe gastrointestinal involvement (persistent vomiting, increasing or intense
abdominal pain, jaundice).
There is severe organ impairment (acute liver failure, acute renal failure,
encephalopathy or encephalitis, or other unusual manifestations, cardiomyopathy) or
other unusual manifestations.
Laboratory Findings3
Thrombocytopenia and haemoconcentration are constant findings in DHF. A
drop in the platelet count to below 100 000 per mm3 is usually found between the third
and eighth day of illness, often before or simultaneous with changes in the haematocrit.3
A rise in the haematocrit level, indicating plasma leakage, is always present,
even in non-shock cases, but is more pronounced in shock cases. Haemoconcentration
with an increase in the haematocrit of 20% or more is considered to be definitive
evidence of increased vascular permeability and plasma leakage. It should be noted that
12
the haematocrit level may be affected either by early volume replacement or by
bleeding.3
The time-course relation-ship between a drop in the platelet count and a rapid
rise in the haematocrit appears to be unique for DHF; both changes occur before
defervescence and before the onset of shock.3,6,7
In DHF, the white-blood-cell count may be variable at the onset of illness,
ranging from leukopenia to mild leukocytosis, but a drop in the total white- blood-cell
count due to a reduction in the number of neutrophils is virtually always observed near
the end of the febrile phase of illness. Relative lymphocytosis, with the presence of
atypical lymphocytes, is a common finding before defervescence or shock. A transient
mild albuminuria is sometimes observed, and occult blood is often found in the stool. 6,7
In most cases, assays of coagulation or fibrinolytic factors show a reduction in
fibrinogen, prothrombin, factor VIII, factor XII, and antithrombin III. A reduction in
antiplasmin (plasmin inhibitor) has been noted in some cases. In severe cases with
marked liver dysfunction, reductions are observed in the levels of the prothrombin
factors hat are vitamin-K dependent, such as factors V, VII, IX and X. Partial
thromboplastin time and prothrombin time are prolonged in about one-half and onethird of DHF patients, respectively. Thrombin time is prolonged in severe cases. Platelet
function has also been found to be impaired. Serum complement levels, particularly that
of C3, are reduced.6
The other common findings are hypoproteinaemia (due to a loss of albumin),
hyponatraemia, and elevated levels of serum aspartate aminotransferase. Metabolic
acidosis may frequently be found in prolonged shock. Blood urea nitrogen is elevated at
the terminal stage of shock. X-ray examination of the chest reveals pleural effusion,
mostly on the right side, as a constant finding, and the extent of pleural effusion is
correlated with the severity of disease. In shock, bilateral pleural effusion is a common
finding.6,7
Guidance for diagnosis of DHF/DSS2
The following manifestations have been selected as indicating a provisional
diagnosis of DHF/DSS. They are not intended to be substitutes for the above case
13
definitions. The use of these criteria may help clinicians to establish an early diagnosis,
ideally before the onset of shock, as well as to avoid over diagnosis.
Clinical
The following clinical observations are important indicators of DHF/DSS:
High fever of acute onset
Haemorrhagic manifestations (at least a positive tourniquet test)
Hepatomegaly (observed in 9096% of Thai and 67% of Cuban children
with DHF)
Shock
Laboratory2
These laboratory findings support the above clinical observations:
Thrombocytopenia (100 000 cells per mm3 or less)
Haemoconcentration (haematocrit elevated at least 20% above average for age, sex
and population).
The first two clinical observations, plus one of the laboratory findings (or at least
a rising haematocrit), are sufficient to establish a provisional diagnosis of DHF.2
In monitoring haematocrit, one should bear in mind the possible effects of preexisting anaemia, severe haemorrhage or early volume replacement therapy. Moreover,
pleural effusion observed on a chest X-ray, or hypoalbuminaemia, can provide
supporting evidence of plasma leakage, the distinguishing feature of DHF. For a patient
with a provisional diagnosis of DHF, if shock is present, a diagnosis of DSS is
supported.2
TREATMENT4
A stepwise approach to the management of dengue
Step I. Overall assessment
I.1 History, including information on symptoms, past medical and family history
I.2 Physical examination, including full physical and mental assessment
14
I.3 Investigation, including routine laboratory and dengue-specific laboratory
Step II. Diagnosis, assessment of disease phase and severity
Step III. Management
III.1 Disease notification
III.2 Management decisions. Depending on the clinical manifestations and other
circumstances, patients may:
be sent home (Group A);
be referred for in-hospital management (Group B);
require emergency treatment and urgent referral (Group C).
Treatment according to groups AC
Group A patients who may be sent home
These are patients who are able to tolerate adequate volumes of oral fluids and
pass urine at least once every six hours, and do not have any of the warning signs,
particularly when fever subsides.
Ambulatory patients should be reviewed daily for disease progression
(decreasing white blood cell count, defervescence and warning signs) until they are out
of the critical period. Those with stable haematocrit can be sent home after being
advised to return to the hospital immediately if they develop any of the warning signs
and to adhere to the following action plan:
Encourage oral intake of oral rehydration solution (ORS), fruit juice and other fluids
containing electrolytes and sugar to replace losses from fever and vomiting. Adequate
oral fluid intake may be able to reduce the number of hospitalizations. [Caution: fluids
containing sugar/glucose may exacerbate hyperglycaemia of physiological stress from
dengue and diabetes mellitus.]
Give paracetamol for high fever if the patient is uncomfortable. The interval of
paracetamol dosing should not be less than six hours. Tepid sponge if the patient still
has high fever. Do not give acetylsalicylic acid (aspirin), ibuprofen or other non-
15
steroidal anti-inflammatory agents (NSAIDs) as these drugs may aggravate gastritis or
bleeding. Acetylsalicylic acid (aspirin) may be associated with Reyes Syndrome.
Instruct the care-givers that the patient should be brought to hospital immediately if
any of the following occur: no clinical improvement, deterioration around the time of
defervescence, severe abdominal pain, persistent vomiting, cold and clammy extremities,
lethargy or irritability/restlessness, bleeding (e.g. black stools or coffee-ground
vomiting), not passing urine for more than 46 hours.
Group B patients who should be referred for in-hospital management
Patients may need to be admitted to a secondary health care centre for close
observation, particularly as they approach the critical phase. These include patients with
warning signs, those with co-existing conditions that may make dengue or its
management more complicated (such as pregnancy, infancy, old age, obesity, diabetes
mellitus, renal failure, chronic haemolytic diseases), and those with certain social
circumstances (such as living alone, or living far from a health facility without reliable
means of transport).
If the patient has dengue with warning signs, the action plan should be as
follows:
Obtain a reference haematocrit before fluid therapy. Give only isotonic solutions such
as 0.9% saline, Ringers lactate, or Hartmanns solution. Start with 57 ml/kg/hour for
12 hours, then reduce to 35 ml/kg/hr for 24 hours, and then reduce to 23 ml/kg/hr
or less according to the clinical response.
Reassess the clinical status and repeat the haematocrit. If the haematocrit remains the
same or rises only minimally, continue with the same rate (23 ml/kg/hr) for another 2
4 hours. If the vital signs are worsening and haematocrit is rising rapidly, increase the
rate to 510 ml/kg/hour for 12 hours. Reassess the clinical status, repeat the
haematocrit and review fluid infusion rates accordingly.
16
Give the minimum intravenous fluid volume required to maintain good perfusion
and urine output of about 0.5 ml/kg/hr. Intravenous fluids are usually needed for only
2448 hours. Reduce intravenous fluids gradually when the rate of plasma leakage
decreases towards the end of the critical phase. This is indicated by urine output and/or
oral fluid intake that is/are adequate, or haematocrit decreasing below the baseline value
in a stable patient.
Patients with warning signs should be monitored by health care providers until the
period of risk is over. A detailed fluid balance should be maintained. Parameters that
should be monitored include vital signs and peripheral perfusion (14 hourly until the
patient is out of the critical phase), urine output (46 hourly), haematocrit (before and
after fluid replacement, then 612 hourly), blood glucose, and other organ functions
(such as renal profile, liver profile, coagulation profile, as indicated).
If the patient has dengue without warning signs, the action plan should be as
follows:
Encourage oral fluids. If not tolerated, start intravenous fluid therapy of 0.9% saline or
Ringers lactate with or without dextrose at maintenance rate. For obese and overweight
patients, use the ideal body weight for calculation of fluid infusion. Patients may be able
to take oral fluids after a few hours of intravenous fluid therapy. Thus, it is necessary to
revise the fluid infusion frequently. Give the minimum volume required to maintain
good perfusion and urine output. Intravenous fluids are usually needed only for 2448
hours.
Patients should be monitored by health care providers for temperature pattern,volume
of fluid intake and losses, urine output (volume and frequency), warning
signs,haematocrit, and white blood cell and platelet counts. Other laboratory tests (such
as liver and renal functions tests) can be done, depending on the clinical picture and the
facilities of the hospital or health centre.
17
Group C patients who require emergency treatment and urgent referral when they
have severe dengue
Patients require emergency treatment and urgent referral when they are in the
critical phase of disease, i.e. when they have:
severe plasma leakage leading to dengue shock and/or fluid accumulation with
respiratory distress;
severe haemorrhages;
severe organ impairment (hepatic damage, renal impairment,cardiomyopathy,
encephalopathy or encephalitis).
All patients with severe dengue should be admitted to a hospital with access to
intensive care facilities and blood transfusion. Judicious intravenous fluid resuscitation
is the essential and usually sole intervention required. The crystalloid solution should be
isotonic and the volume just sufficient to maintain an effective circulation during the
period of plasma leakage. Plasma losses should be replaced immediately and rapidly
with isotonic crystalloid solution or, in the case of hypotensive shock, colloid solutions.
If possible, obtain haematocrit levels before and after fluid resuscitation.
There should be continued replacement of further plasma losses to maintain
effective circulation for 2448 hours. For overweight or obese patients, the ideal body
weight should be used for calculating fluid infusion rates. A group and cross-match
should be done for all shock patients. Blood transfusion should be given only in cases
with suspected/severe bleeding. Fluid resuscitation must be clearly separated from
simple fluid administration. This is a strategy in which larger volumes of fluids (e.g.
1020 ml boluses) are administered for a limited period of time under close monitoring
to evaluate the patients response and to avoid the development of pulmonary oedema.
The degree of intravascular volume deficit in dengue shock varies. Input is typically
much greater than output, and the input/output ratio is of no utility for judging fluid
resuscitation needs during this period.
The goals of fluid resuscitation include improving central and peripheral
circulation (decreasing tachycardia, improving blood pressure, pulse volume, warm and
18
pink extremities, and capillary refill time <2 seconds) and improving end-organ
perfusion i.e. stable conscious level (more alert or less restless), urine output 0.5
ml/kg/hour, decreasing metabolic acidosis.
Treatment of shock4
The action plan for treating patients with compensated shock is as follows :
Start intravenous fluid resuscitation with isotonic crystalloid solutions at 5
10ml/kg/hour over one hour. Then reassess the patients condition (vital signs, capillary
refill time, haematocrit, urine output). The next steps depend on the situation.
If the patients condition improves, intravenous fluids should be gradually reduced to
57 ml/kg/hr for 12 hours, then to 35 ml/kg/hr for 24 hours, then to 23 ml/kg/hr,
and then further depending on haemodynamic status, which can be maintained for up to
24 -48 hours.
If vital signs are still unstable (i.e.shock persists), check the haematocrit after the first
bolus. If the haematocrit increases or is still high (>50%), repeat a second bolus of
crystalloid solution at 1020 ml/kg/hr for one hour. After this second bolus, if there is
improvement, reduce the rate to 710 ml/kg/hr for 12 hours, and then continue to
reduce as above. If haematocrit decreases compared to the initial reference haematocrit
(<40% in children and adult females, <45% in adult males), this indicates bleeding and
the need to cross-match and transfuse blood as soon as possible.
Further boluses of crystalloid or colloidal solutions may need to be given during the
next 2448 hours.
Patients with hypotensive shock should be managed more vigorously. The action
plan for treating patients with hypotensive shock is as follows :
Initiate intravenous fluid resuscitation with crystalloid or colloid solution (if available)
at 20 ml/kg as a bolus given over 15 minutes to bring the patient out of shock as quickly
as possible.
19
If the patients condition improves, give a crystalloid/colloid infusion of 10 ml/kg/hr
for one hour. Then continue with crystalloid infusion and gradually reduce to 57
ml/kg/hr for 12 hours, then to 35 ml/kg/hr for 24 hours, and then to 23 ml/kg/hr or
less, which can be maintained for up to 2448 hours.
If vital signs are still unstable (i.e.shock persists), review the haematocrit obtained
before the first bolus. If the haematocrit was low (<40% in children and adult females,
<45% in adult males), this indicates bleeding and the need to cross-match and transfuse
blood as soon as possible.
If the haematocrit was high compared to the baseline value (if not available,use
population baseline), change intravenous fluids to colloid solutions at 1020 ml/kg as a
second bolus over 30 minutes to one hour. After the second bolus, reassess the patient.
If the condition improves, reduce the rate to 710 ml/kg/hr for 12 hours, then change
back to crystalloid solution and reduce the rate of infusion as mentioned above. If the
condition is still unstable, repeat the haematocrit after the second bolus.
If the haematocrit decreases compared to the previous value (<40% In children and
adult females, <45% in adult males), this indicates bleeding and the need to cross-match
and transfuse blood as soon as possible. If the haematocrit increases compared to the
previous value or remains very high (>50%), continue colloid solutions at1020 ml/kg
as a third bolus over one hour. After this dose, reduce the rate to 710 ml/kg/hr for 12
hours, then change back to crystalloid solution and reduce the rate of infusion as
mentioned above when the patients condition improves.
Further boluses of fluids may need to be given during the next 24 hours.The rate and
volume of each bolus infusion should be titrated to the clinical response. Patients with
severe dengue should be admitted to the high-dependency or intensive care area.
Patients with dengue shock should be frequently monitored until the danger
period is over. A detailed fluid balance of all input and output should be maintained.
20
Parameters that should be monitored include vital signs and peripheral perfusion
(every 1530 minutes until the patient is out of shock, then 12 hourly). In general, the
higher the fluid infusion rate, the more frequently the patient should be monitored and
reviewed in order to avoid fluid overload while ensuring adequate volume replacement.
If resources are available, a patient with severe dengue should have an arterial line
placed as soon as practical. The reason for this is that in shock states, estimation of
blood pressure using a cuff is commonly inaccurate. The use of an indwelling arterial
catheter allows for continuous and reproducible blood pressure measurements and
frequent blood sampling on which decisions regarding therapy can be based. Monitoring
of ECG and pulse oximetry should be available in the intensive care unit.
Urine output should be checked regularly (hourly till the patient is out of shock,
then 12 hourly). A continuous bladder catheter enables close monitoring of urine
output. An acceptable urine output would be about 0.5 ml/kg/hour. Haematocrit should
be monitored (before and after fluid boluses until stable, then 46 hourly). In addition,
there should be monitoring of arterial or venous blood gases, lactate, total carbon
dioxide/bicarbonate (every 30 minutes to one hour until stable, then as indicated), blood
glucose (before fluid resuscitation and repeat as indicated), and other organ functions
(such as renal profile, liver profile, coagulation profile, before resuscitation and as
indicated).
Changes in the haematocrit are a useful guide to treatment. However, changes
must be interpreted in parallel with the haemodynamic status, the clinical response to
fluid therapy and the acid-base balance. For instance, a rising or persistently high
haematocrit together with unstable vital signs (particularly narrowing of the pulse
pressure) indicates active plasma leakage and the need for a further bolus of fluid
replacement. However, a rising or persistently high haematocrit together with stable
haemodynamic status and adequate urine output does not require extra intravenous fluid.
In the latter case, continue to monitor closely and it is likely that the haematocrit will
start to fall within the next 24 hours as the plasma leakage stops.
21
A decrease in haematocrit together with unstable vital signs (particularly
narrowing of the pulse pressure, tachycardia, metabolic acidosis, poor urine output)
indicates major haemorrhage and the need for urgent blood transfusion. Yet a decrease
in haematocrit together with stable haemodynamic status and adequate urine output
indicates haemodilution and/or reabsorption of extravasated fluids, so in this case
intravenous fluids must be discontinued immediately to avoid pulmonary oedema.
PREVENTION
There is no vaccine to prevent dengue fever. Use personal protection such as
full-coverage clothing, mosquito nets, mosquito repellent containing DEET. If possible,
travel during times of the day when mosquitos are not so active. Mosquito abatement
(control) programs can also reduce the risk of infection.
At present, the only method to control or prevent the transmission of dengue virus is to
combat vector mosquitoes through:
preventing mosquitoes from accessing egg-laying habitats by environmental
management and modification;
disposing of solid waste properly and removing artificial man-made habitats;
covering, emptying and cleaning of domestic water storage containers on a
weekly basis;
applying appropriate insecticides to water storage outdoor containers;
using of personal household protection such as window screens, long-sleeved
clothes, insecticide treated materials, coils and vaporizers;
improving community participation and mobilization for sustained vector
control;
applying insecticides as space spraying during outbreaks as one of the
emergency vector control measures;
22
active monitoring and surveillance of vectors should be carried out to determine
effectiveness of control interventions.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 10.1016/j.foodres.2014.01.057: Food Research InternationalDocument90 pages10.1016/j.foodres.2014.01.057: Food Research Internationaledywiyono2013No ratings yet
- Ningxia Red Newsletter Power With PromiseDocument4 pagesNingxia Red Newsletter Power With Promiseapi-250114946No ratings yet
- Patofisiologi Dan Diagnosa ObesitasDocument28 pagesPatofisiologi Dan Diagnosa ObesitasSitti Rosmahsari100% (1)
- Fast Food Addiction: A Major Public Health ConcernDocument12 pagesFast Food Addiction: A Major Public Health ConcernA. K. Mohiuddin100% (1)
- Cause and Effect PoroDocument2 pagesCause and Effect PoroJayson Dela Torre CortesNo ratings yet
- Science Behind Sunnah - Anas KhanDocument104 pagesScience Behind Sunnah - Anas KhanUsaid HussainNo ratings yet
- Case Scenarios 3rd Yr Head NursingDocument5 pagesCase Scenarios 3rd Yr Head NursingBianca MaeNo ratings yet
- 1.facies R Flores B N PDFDocument16 pages1.facies R Flores B N PDFDenys PQNo ratings yet
- Cardiorenal SyndromeDocument89 pagesCardiorenal SyndromeGabriyah HamzahNo ratings yet
- Ciuperci ImunitateDocument3 pagesCiuperci Imunitatedoruk19640% (1)
- SetyaningrumrahmawatyDocument3 pagesSetyaningrumrahmawatyBoh Cucu KaraengNo ratings yet
- An Insulin Index of FoodsDocument13 pagesAn Insulin Index of FoodsVInesh Raj Mohane RadjeNo ratings yet
- On-Call Plus Product Insert 3146file1Document0 pagesOn-Call Plus Product Insert 3146file1Abdul Shakur FaisalNo ratings yet
- Aaqib Nawaz 170055 Case Assignment 1 EntrepreneurshipDocument3 pagesAaqib Nawaz 170055 Case Assignment 1 Entrepreneurshipaaqib nawazNo ratings yet
- BENEFITS OF HEALTH AND FITNESSDocument2 pagesBENEFITS OF HEALTH AND FITNESSAndrew GrayNo ratings yet
- Lesson 2 q1 P.E. Active RecreationDocument79 pagesLesson 2 q1 P.E. Active RecreationIleneah BenchNo ratings yet
- Strength Training For Distance Runners: Drills, Core and Workouts To Keep Your Athletes Healthy and StrongDocument37 pagesStrength Training For Distance Runners: Drills, Core and Workouts To Keep Your Athletes Healthy and StrongSashoNo ratings yet
- MEDICAL REQUIREMENTS FOR CABIN CREWDocument8 pagesMEDICAL REQUIREMENTS FOR CABIN CREWRamBabuMeenaNo ratings yet
- Apovian 2016Document10 pagesApovian 2016Sandy PranadaNo ratings yet
- Dasar Gizi Masyarakat: DR - Dr. Joko Wahyu Wibowo, Mkes Bagian Gizi FK UnissulaDocument49 pagesDasar Gizi Masyarakat: DR - Dr. Joko Wahyu Wibowo, Mkes Bagian Gizi FK UnissulawkwkwkhhhhNo ratings yet
- Fetal Acid Base PhysiologyDocument2 pagesFetal Acid Base PhysiologyAde YonataNo ratings yet
- 2018 - 2019 Nutritional Status 9-NarraDocument4 pages2018 - 2019 Nutritional Status 9-Narraariane may malicseNo ratings yet
- Betty FriedanDocument32 pagesBetty FriedanlearningforieltsNo ratings yet
- Body Weight Work Out Plan PDFDocument1 pageBody Weight Work Out Plan PDFVivek VinayakumarNo ratings yet
- Uppercut MagazineDocument12 pagesUppercut MagazineChris Finn100% (1)
- Lesson Preview: Checking For UnderstandingDocument2 pagesLesson Preview: Checking For UnderstandingKristinelou Marie N. ReynaNo ratings yet
- Sucralose Fact SheetDocument2 pagesSucralose Fact Sheetinder12564No ratings yet
- 9 Facebook BmiDocument29 pages9 Facebook BmiDin Flores MacawiliNo ratings yet
- OBESITYDocument3 pagesOBESITYfemeritusconsultNo ratings yet
- PBL BibleDocument74 pagesPBL Biblesare77No ratings yet