Professional Documents
Culture Documents
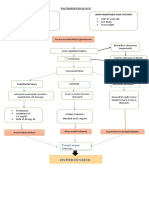
Tuberculosis: Lifestyle (Smoking) Environment Age Gender
Uploaded by
hannahleatanosornOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tuberculosis: Lifestyle (Smoking) Environment Age Gender
Uploaded by
hannahleatanosornCopyright:
Available Formats
fModifiable Risk
Lifestyle (Smoking)
Environment
Non Modifiable Risk
Age
Gender
Compromised cough/gag reflex,
mucocilary system, or immune
system
Tuberculosis
Bacteria and other pneumoniacausing agents enter the normally
sterile lung fields via inhalation or
the bloodstream
Lymphocytes and
macrophages are attracted
to these bacteria
Immune cells begin producing
antibodies and walling off the
infection by forming a type of
granuloma called a tubercule
Caseous necrosis (cheesy
appearance from a tubercule)
Tubercules change by
fibrosing and calcifying
Immune system walls off
bacteria (disease may be
arrested or rendered inactive
for long period of time)
Antibodies produced will
circulate in the blood for the
remainder of the infected
individuals life in readiness to
attack future TB bacteria
(+ TB Skin test)
Pneumonia
Signs and Symptoms:
Fever
Chills
Aching chest
Malaise
Dyspnea
Watery phlegm
Inc. WBC
Fine crackles
Hempotysis
Diagnostic Tests:
Culture and
Sensitivity
CBC:
Hct- 0.35
RBC- 3.41
Hgb- 107
Wbc- 12.2
Lymph- 0.11
Polys- 0.82
ABG:
PCO2- 40.4
PO2-36
02 sat-71
Vascular engorgement of the
capillary bed
Serous fluid leaks into the alveoli
RBC and fibrin enter the alveoli
Fibrin and disintegrating RBC/WBC
accumulate in the affected area
Enzymes digest and remove the
products of inflammation
Exudate is either coughed up or
removed by WBC
Necrosis of the lung
Respiratory Failure
Impaired gas exchange (movement
of gases into and out of the alveolar
capillary membrane)
Ventilation (movement of gases into
and out of the alveoli due to the
action of the respiratory muscles
Hypoxemic Respiratory Failure
Hypercapnic/hypoxemc
respiratory failure (unable to
Mismatching of
ventilation and
perfusion
Gas exchange cannot
take place
Carbon Dioxide
Retention
Impaired Diffusion
maintain a level of alveolar
ventilation sufficient to eliminate
carbon dioxide and keep arterial
oxygen levels within Normal range
Trauma or depression of lungs
Gas exchange between the
alveolar air and pulmonary
blood s impeded because of an
increase in the dstance for
diffusion or a decrease in the
permeability or surface area of
the repiratory membranes to
the movement of gases
Volume of fresh air moving into
and out of the lungs is
significantly reduced
Hypoventilation
Severe Hypoxemia
Increase partial carbon dioxide
Hypercapnia
Increase cerebral Blood Flow
Pulmonary vasculature
constricts in response to low
alveolar PO2
Hypoxemia
Increased respiratory drive and
sympathetic tone
Acute Right Ventricular failure
Signs and symptoms:
Dilatation of the cerebral
vessels
Signs and Symptoms
Headache
Warm flushed skin
Mild to moderate BP increase
Signs and Symptoms
Jugular Vein distension
Edema
Cyanosis
Restlessness
Confusion
Anxiety
Delirium
Fatigue
Tachypnea
Hypertension
Cardiac arrhythmias
Tremor
You might also like
- GERD Pathophysiology Cleveland ClinicDocument17 pagesGERD Pathophysiology Cleveland ClinicMavisNo ratings yet
- Global Submission On IndDocument16 pagesGlobal Submission On IndRahul PalsNo ratings yet
- Cough, Hemoptysis, Dyspnea, WheezingDocument43 pagesCough, Hemoptysis, Dyspnea, WheezingMelissa SalayogNo ratings yet
- Post-Streptococcal GlomerulonephritisDocument18 pagesPost-Streptococcal GlomerulonephritisPreciousJemNo ratings yet
- Loan Agreement TemplateDocument5 pagesLoan Agreement TemplatePratik UdaniNo ratings yet
- Urgent Motion For PostponementDocument7 pagesUrgent Motion For PostponementhannahleatanosornNo ratings yet
- Pneumonia Pathophysiology 3Document2 pagesPneumonia Pathophysiology 3billiam123No ratings yet
- Pentacam GuidelineDocument43 pagesPentacam GuidelineEvelyn SepulvedaNo ratings yet
- 2009 DARAB Rules of ProcedureDocument37 pages2009 DARAB Rules of Procedurejeckleandjerry100% (6)
- Group Case Study - Pulmonary TBDocument8 pagesGroup Case Study - Pulmonary TBCj NiñalNo ratings yet
- Drug StudyDocument7 pagesDrug StudyCharmz_asherahNo ratings yet
- Chronic Obstructive Disease by HibaDocument38 pagesChronic Obstructive Disease by HibahibaNo ratings yet
- CARPER LAD Form No. 5 LO Manifestation To Apply For RetentionDocument2 pagesCARPER LAD Form No. 5 LO Manifestation To Apply For RetentionhannahleatanosornNo ratings yet
- Cardio Alexandra Hough 2nd EditionDocument376 pagesCardio Alexandra Hough 2nd EditionManoj M100% (1)
- Case Study Pulmonary TuberculosisDocument19 pagesCase Study Pulmonary TuberculosisJester GalayNo ratings yet
- Pneumonia Teaching PlanDocument5 pagesPneumonia Teaching PlanRaghav RoyNo ratings yet
- PneumoniaDocument1 pagePneumoniaAyen FornollesNo ratings yet
- Pathophysiology Diagram of Kawasaki Disease: Precipitating Factors: Predisposing FactorsDocument2 pagesPathophysiology Diagram of Kawasaki Disease: Precipitating Factors: Predisposing FactorsAb Staholic Boii100% (1)
- SARS PathophysioDocument2 pagesSARS PathophysioLouise BravoNo ratings yet
- Sale of Property Without MaritalDocument3 pagesSale of Property Without Maritalhannahleatanosorn100% (1)
- ChickenpoxDocument1 pageChickenpoxAlvin CerezoNo ratings yet
- Memorandum of Agreement SampleDocument3 pagesMemorandum of Agreement Samplehannahleatanosorn100% (2)
- PATHOPHYSIOLOGY OF OSTEOSARCOMaDocument1 pagePATHOPHYSIOLOGY OF OSTEOSARCOMakyawNo ratings yet
- Cap MR DDHDocument32 pagesCap MR DDHLovelle LopezNo ratings yet
- Retention Right TemplateDocument22 pagesRetention Right TemplateanneNo ratings yet
- Hypertensive Crisis - PathophysiologyDocument1 pageHypertensive Crisis - Pathophysiologyaaron tabernaNo ratings yet
- Age - Weather: Aspiration of Secretions Containing MicrobesDocument4 pagesAge - Weather: Aspiration of Secretions Containing Microbeslouie john abilaNo ratings yet
- Pamantasan NG Cabuyao College of Health Allied Sciences College of NursingDocument43 pagesPamantasan NG Cabuyao College of Health Allied Sciences College of NursingSofea MustaffaNo ratings yet
- TOF (Pathophysiology)Document4 pagesTOF (Pathophysiology)Doreen Claire M. WallangNo ratings yet
- NSTEMIDocument33 pagesNSTEMIwaazalimahwahidNo ratings yet
- Community-Acquired Pneumonia: Bello, Mickaela Bianca A. Gumiran, NomerDocument37 pagesCommunity-Acquired Pneumonia: Bello, Mickaela Bianca A. Gumiran, NomerKristine-Joy Legaspi FrancoNo ratings yet
- Unit 1 5ADocument7 pagesUnit 1 5AArvin O-CaféNo ratings yet
- Acute TonsillopharyngitisDocument39 pagesAcute TonsillopharyngitisCin AtianzarNo ratings yet
- Mycobacterium Tuberculosis: Precipitating Factors: Predisposing FactorsDocument1 pageMycobacterium Tuberculosis: Precipitating Factors: Predisposing FactorsYoko Mae Yano100% (1)
- Guada A. Dumapit RN, ManDocument18 pagesGuada A. Dumapit RN, ManAnne B. BuenvenidaNo ratings yet
- Acute TonsillopharyngitisDocument17 pagesAcute TonsillopharyngitisRachel Haide NaravalNo ratings yet
- Acute Respiratory Distress SyndromDocument38 pagesAcute Respiratory Distress SyndrompatriaindraNo ratings yet
- Pathophysiology: Risk FactorsDocument4 pagesPathophysiology: Risk FactorsEdson John DemayoNo ratings yet
- USC Case 04 - SinusitisDocument9 pagesUSC Case 04 - SinusitisDisti Damelia SebayangNo ratings yet
- TB PathoPhysiologyDocument6 pagesTB PathoPhysiologyChloé Jane HilarioNo ratings yet
- Pathophysiology of Ruptured Ectopic PregnancyDocument3 pagesPathophysiology of Ruptured Ectopic Pregnancybowki namoNo ratings yet
- PneumoniaDocument4 pagesPneumoniaroscelle100% (1)
- Path o Physiology of SyphilisDocument1 pagePath o Physiology of Syphilis3S - JOCSON, DENESE NICOLE LEE M.No ratings yet
- FlashPath - Lung - Bronchopulmonary DysplasiaDocument15 pagesFlashPath - Lung - Bronchopulmonary DysplasiaHazem AliNo ratings yet
- The Difference Between Toxic and Nontoxic GoiterDocument2 pagesThe Difference Between Toxic and Nontoxic GoiterJawad Rehman100% (1)
- NCPDocument13 pagesNCPÍam KristineNo ratings yet
- Febrile SeizureDocument6 pagesFebrile SeizurepipimseptianaNo ratings yet
- Case Presentation RamosDocument35 pagesCase Presentation RamosJose Bryan NacillaNo ratings yet
- H MoleDocument2 pagesH MoleJoanna Marie Datahan EstomoNo ratings yet
- Anatomy and Phsyiology of MeningococcemiaDocument2 pagesAnatomy and Phsyiology of MeningococcemiaKevin Comahig100% (1)
- Influenza PATHOPHYSIOLOGYDocument3 pagesInfluenza PATHOPHYSIOLOGYElle RosalesNo ratings yet
- Dengue: Dengue Hemorrhagic Fever, Resulting in Bleeding, Low Levels of Blood Platelets andDocument5 pagesDengue: Dengue Hemorrhagic Fever, Resulting in Bleeding, Low Levels of Blood Platelets andFrance John Evangelista TorresNo ratings yet
- PTB NCPDocument3 pagesPTB NCPناديه المعمريNo ratings yet
- NCP DHFDocument3 pagesNCP DHFjsdc_14No ratings yet
- NCP IcuDocument2 pagesNCP IcuDiana MuañaNo ratings yet
- Pulmonary TuberculosisDocument46 pagesPulmonary Tuberculosisroseann_808100% (1)
- Lecture and Lab Guide Cells and TissuesDocument137 pagesLecture and Lab Guide Cells and TissuesSkarlon BalagtasNo ratings yet
- LeptospirosisDocument13 pagesLeptospirosis천사천사No ratings yet
- Thyroid Papillary Carcinoma CaseDocument6 pagesThyroid Papillary Carcinoma CaseRandy F BabaoNo ratings yet
- Pathophysiology of BurnsDocument7 pagesPathophysiology of BurnsTemahlungwaneNo ratings yet
- ChickenpoxDocument16 pagesChickenpoxJeet ThuraiNo ratings yet
- Chronic GastritisDocument7 pagesChronic GastritisDivina AquinoNo ratings yet
- NCP Poststreptococcal GlomerulonephritisDocument12 pagesNCP Poststreptococcal GlomerulonephritisScarlet ScarletNo ratings yet
- BPHDocument81 pagesBPHFlo Neri BerondoNo ratings yet
- Concept Map WK 10 LesterDocument1 pageConcept Map WK 10 Lesterapi-277683144No ratings yet
- Leptospirosis: Causes, Incidence, and Risk FactorsDocument6 pagesLeptospirosis: Causes, Incidence, and Risk FactorsJackii DoronilaNo ratings yet
- Cap MRDocument4 pagesCap MRKit BarcelonaNo ratings yet
- Pathophysiology of HyperthyroidismDocument4 pagesPathophysiology of HyperthyroidismKitty YuffieNo ratings yet
- Discharge Care Plan: MedicineDocument2 pagesDischarge Care Plan: MedicineFau Fau DheoboNo ratings yet
- Clinical Physiology of Respiration: Dr. M Qathar RF TDocument76 pagesClinical Physiology of Respiration: Dr. M Qathar RF TTiwi Lestari TiwiNo ratings yet
- Respiration CH 43.Dr SarahDocument59 pagesRespiration CH 43.Dr Sarahaiman siddiquiNo ratings yet
- Lower Respiratory Disorders Part 1Document70 pagesLower Respiratory Disorders Part 1Joseph Krafft100% (1)
- Promissory NoteDocument1 pagePromissory NotehannahleatanosornNo ratings yet
- BAR Requirement Form (Repeater) PDFDocument6 pagesBAR Requirement Form (Repeater) PDFAlhaimah MadzamanNo ratings yet
- Waiver of Rights Water DistrictDocument2 pagesWaiver of Rights Water DistricthannahleatanosornNo ratings yet
- GP 2016 Election Watchers' TrainingDocument126 pagesGP 2016 Election Watchers' TraininghannahleatanosornNo ratings yet
- SUPERIOR MOTOR CORPORATION Request For AlarmDocument1 pageSUPERIOR MOTOR CORPORATION Request For AlarmhannahleatanosornNo ratings yet
- Entry of AppearanceDocument1 pageEntry of AppearancehannahleatanosornNo ratings yet
- Resolution NoDocument1 pageResolution NohannahleatanosornNo ratings yet
- Seven CluesDocument14 pagesSeven ClueshannahleatanosornNo ratings yet
- 10 Philippine Herbal Medicines Approved by DohDocument38 pages10 Philippine Herbal Medicines Approved by DohhannahleatanosornNo ratings yet
- How Well Do You Know The BrideDocument1 pageHow Well Do You Know The BridehannahleatanosornNo ratings yet
- Would You Rather 2Document10 pagesWould You Rather 2hannahleatanosornNo ratings yet
- Perlas-Bernabe CasesDocument15 pagesPerlas-Bernabe CaseshannahleatanosornNo ratings yet
- Authority To Secure Election ReturnDocument1 pageAuthority To Secure Election ReturnhannahleatanosornNo ratings yet
- The Pretrial BriefDocument11 pagesThe Pretrial BriefhannahleatanosornNo ratings yet
- A Intercessory PrayerDocument1 pageA Intercessory Prayerhannahleatanosorn0% (1)
- Promissory Note - : (P 230,000.00) Payable Within A Period of ONE (1) YearDocument1 pagePromissory Note - : (P 230,000.00) Payable Within A Period of ONE (1) YearhannahleatanosornNo ratings yet
- Affidavit of ResidenceDocument1 pageAffidavit of ResidencehannahleatanosornNo ratings yet
- Contents of PreDocument1 pageContents of PrehannahleatanosornNo ratings yet
- Be It Enacted by The Senate and House of Representatives of The Philippines in Congress AssembledDocument42 pagesBe It Enacted by The Senate and House of Representatives of The Philippines in Congress AssembledJo BaNo ratings yet
- Resolution Amending Rule 141 (Legal Fees) of The Rules of CourtDocument12 pagesResolution Amending Rule 141 (Legal Fees) of The Rules of CourthannahleatanosornNo ratings yet
- AO 7 S 2011Document47 pagesAO 7 S 2011hannahleatanosornNo ratings yet
- Petition For Notarial Commission SAMPLEDocument3 pagesPetition For Notarial Commission SAMPLEhannahleatanosornNo ratings yet
- My Reading LogDocument3 pagesMy Reading LoghannahleatanosornNo ratings yet
- World Kidney Program 2022: ProspectusDocument3 pagesWorld Kidney Program 2022: ProspectusNuranisaNo ratings yet
- Wilcock 2008Document11 pagesWilcock 2008Nadia SaiNo ratings yet
- Arthur Steindler: Pes Cavus (1921), He Analyzed The Muscle ImbalDocument3 pagesArthur Steindler: Pes Cavus (1921), He Analyzed The Muscle Imbalisaac b-127No ratings yet
- Lacosamide: A Novel Antiepileptic and Anti-Nociceptive Drug On The BlockDocument5 pagesLacosamide: A Novel Antiepileptic and Anti-Nociceptive Drug On The BlockFarhatNo ratings yet
- NaspubDocument6 pagesNaspubdesi permatasariNo ratings yet
- Pathophysiology ExaminationDocument6 pagesPathophysiology ExaminationPractice Medi-nursingNo ratings yet
- DRUG STUDY Durano Aireen E.Document4 pagesDRUG STUDY Durano Aireen E.Doneva Lyn MedinaNo ratings yet
- Access Corporate Fact SheetDocument2 pagesAccess Corporate Fact SheetMattNo ratings yet
- Respiratory SystemDocument7 pagesRespiratory SystemNgọc Mai Khanh NguyễnNo ratings yet
- Presentation On Postpartum ComplicationsDocument24 pagesPresentation On Postpartum ComplicationsBeulah DasariNo ratings yet
- Tarun Kumar ReportDocument1 pageTarun Kumar Reportnavdeep madheshiyaNo ratings yet
- Hyperparathyroidism A Forgotten Cause of Musculoskeletal PainDocument3 pagesHyperparathyroidism A Forgotten Cause of Musculoskeletal PainPhuoc TranNo ratings yet
- Effect of Iron Containing Supplements On Rats DenDocument6 pagesEffect of Iron Containing Supplements On Rats Dendhea hutabaratNo ratings yet
- RameyDocument15 pagesRameyPharmacist DinaNo ratings yet
- List of PM&DC Recognized JournalsDocument14 pagesList of PM&DC Recognized JournalsSanaa AhmedNo ratings yet
- Drotaverine: Solution For Injection - 40 MG / 2 MLDocument1 pageDrotaverine: Solution For Injection - 40 MG / 2 MLZarbakht AliNo ratings yet
- Hypokalemia - A Clinical UpdateDocument12 pagesHypokalemia - A Clinical UpdateRushi PatelNo ratings yet
- ACNS Standardized Critical Care EEG Examples 2021Document36 pagesACNS Standardized Critical Care EEG Examples 2021CNo ratings yet
- Pediatric Asthma Situation in Chengdu, China, During The COVID-19 Pandemic: An Observational StudyDocument10 pagesPediatric Asthma Situation in Chengdu, China, During The COVID-19 Pandemic: An Observational StudyzainabNo ratings yet
- BodyBallancer Lipo Brochure PDFDocument2 pagesBodyBallancer Lipo Brochure PDFRoss Gale100% (1)
- DMT Consensus MS CoalitionDocument73 pagesDMT Consensus MS CoalitionDeepaNo ratings yet
- Fs 15Document8 pagesFs 15api-299490997No ratings yet
- Glossopharyngeal Nerve Injury Following Tonsillectomy 5542Document4 pagesGlossopharyngeal Nerve Injury Following Tonsillectomy 5542Kenza SeddikNo ratings yet
- Malaria: Health Education HFT 201 By: Sophia Kol, MDDocument10 pagesMalaria: Health Education HFT 201 By: Sophia Kol, MDTith SeavmeyNo ratings yet
- Utility of Fine Needle Aspiration Cytology of Lymph Nodes: Dr. Ripunjaya Mohanty, Dr. Anne WilkinsonDocument6 pagesUtility of Fine Needle Aspiration Cytology of Lymph Nodes: Dr. Ripunjaya Mohanty, Dr. Anne WilkinsonAmanda AlmaNo ratings yet