Professional Documents
Culture Documents
Rabipur - (EMC) Print Friendly
Uploaded by
shreyas_chandor3802Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rabipur - (EMC) Print Friendly
Uploaded by
shreyas_chandor3802Copyright:
Available Formats
8/29/2014
Rabipur - (eMC) print friendly
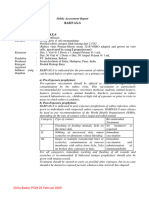
Rabipur
Summary of Product Characteristics Updated 10-Jun-2010 | Novartis Vaccines
1. Name of the medicinal product
Powder and solvent for solution for injection
Rabies vaccine, inactivated
2. Qualitative and quantitative composition
After reconstitution, 1 dose (1 ml) contains:
Rabies virus* (Inactivated, strain Flury LEP)....................= 2.5 IU
* produced on puri?ed chick embryo cells
For a list of excipients, see section 6.1.
3. Pharmaceutical form
Powder and solvent for solution for injection.
A clear colourless solution results after reconstitution of the white freeze-dried powder with the clear and colourless
solvent.
4. Clinical particulars
4.1 Therapeutic indications
a) Pre-exposure prophylaxis (before possible risk of exposure to rabies)
b) Post-exposure prophylaxis (after known or possible exposure to rabies)
Consideration should be given to national and/or WHO guidance regarding the prevention of rabies.
4.2 Posology and method of administration
Posology
The recommended single intramuscular dose is 1 ml in all age groups.
Whenever possible according to vaccine availability, it is recommended that one type of cell culture vaccine should be
used throughout the course of pre- or post-exposure immunisation. However, adherence to the recommended schedules
is of critical importance for post-exposure prophylaxis, even if another type of cell culture vaccine has to be used.
PRE-EXPOSURE PROPHYLAXIS
Primary immunisation
In previously unvaccinated persons, an initial course of pre-exposure prophylaxis consists of three doses (each of 1 ml)
administered on days 0, 7 and 21 or 28.
Booster doses
The need of intermittent serological testing for the presence of antibody 0.5 IU/ml (as assessed by the Rapid FocusFluorescent inhibition Test) and the administration of booster doses should be assessed in accordance with official
recommendations.
The following provides general guidance:
Testing for neutralising antibodies at 6-month intervals is usually recommended if the risk of exposure is high (e. g.
Laboratory staff working with rabies virus).
In persons who are considered to be at continuing risk of exposure to rabies (e.g. veterinarians and their assistants,
wildlife workers, hunters), a serological test should usually be performed at least every 2 years, with shorter intervals if
appropriate to the perceived degree of risk.
In above mentioned cases, a booster dose should be given should the antibody titre fall below 0.5 IU/ml.
Alternatively, booster doses may be given at official recommended intervals without prior serological testing, according
to the perceived risk. Experience shows that reinforcing doses are generally required every 2-5 years.
Rabipur may be used for booster vaccination after prior immunisation with human diploid cell rabies vaccine.
http://www.medicines.org.uk/emc/print-document?documentId=14933
1/8
8/29/2014
Rabipur - (eMC) print friendly
POST-EXPOSURE PROPHYLAXIS
Post-exposure immunisation should begin as soon as possible after exposure and should be accompanied by local
measures to the site of inoculation so as to reduce the risk of infection. Official guidance should be sought regarding the
appropriate concomitant measures that should be taken to prevent establishment of infection (see also section 4.4).
Previously fully immunised individuals
For WHO exposure categories II and III, and in category I cases where there is uncertainty regarding the correct
classication of exposure (see Table l below), two doses (each of 1 ml) should be administered, one each on days 0 and
3. On a case by case basis, schedule A (see Table 2 below) may be applied if the last dose of vaccine was given more
than two years previously.
Table 1: Immunisation schedules appropriate to different type of contact, exposure and recommended post-exposure
prophylaxis (WHO 2004)
Category
Type of contact with a suspect Type of exposure
or confirmed rabid domestic or
wilda) animal, or animal
unavailable for testing
Recommended post-exposure
prophylaxis
Touching or feeding of animals
None, if reliable case history is
available.
None
Licks on intact skin
In case of unreliable case history,
treat according to schedule A (see
Table 2).
Touching of inoculated animal lure
with intact skin
II
Nibbling of uncovered skin
Minor
Minor scratches or abrasions
without bleeding
Touching of inoculated animal lure
with skin damaged
Administer vaccine immediately b)
Stop treatment if animal remains
healthy throughout an observation
period of 10 days c) or if animal is
proven to be negative for rabies by
reliable laboratory using
appropriate diagnostic techniques
In case of uncertainty and/or
exposure in a high-risk area,
administer active and passive
treatment as in schedule B (see
Table 2).
III
Single or multiple transdermal
Severe
bites or scratches, licks on broken
skin
Administer rabies immunoglobulin
and vaccine immediately b) as in
schedule B (see Table 2).
Contamination of mucous
membrane with saliva (i.e. licks)
Stop treatment if animal remains
healthy throughout an observation
period of 10 days c) or if animal is
proven to be negative for rabies by
reliable laboratory using
appropriate diagnostic techniques
Exposure to bats d)
Touching of inoculated animal lure
with mucous membrane or fresh
skin wound
a) Exposure to rodents, rabbits and hares seldom, if ever, requires specic anti-rabies post-exposure prophylaxis.
b) If an apparently healthy dog or cat in or from a low-risk area is placed under observation, the situation may warrant
delaying initiation of treatment.
c) This observation period applies only to dogs and cats. Except in the case of threatened or endangered species, other
domestic and wild animals suspected as rabid should be humanely killed and their tissues examined for the presence of
rabies antigen using appropriate laboratory techniques.
d) Post-exposure prophylaxis should be considered when contact between a human and a bat has occurred unless the
exposed person can rule out a bite or scratch, or exposure to a mucous membrane.
http://www.medicines.org.uk/emc/print-document?documentId=14933
2/8
8/29/2014
Rabipur - (eMC) print friendly
Individuals unimmunised or with uncertain immune status
Depending on the WHO category as in Table l, treatment according to schedules A or B (see Table 2 below) may be
required for previously unimmunised persons and for those who have received fewer than 3 doses of vaccine or who have
received a vaccine of doubtful potency.
Table 2: Post-exposure prophylaxis of subjects with no or uncertain immune status
Schedule A
Schedule B
Active immunisation after exposure is required
Active and passive immunisation after exposure are
required
One injection of Rabipur i.m. on days: 0, 3, 7, 14, 28 (5doses schedule)
Give Rabipur as in schedule A + l 20 IU/kg body weight
human rabies immunoglobulin* concomitantly with the rst
dose of Rabipur. If HRIG is not available at the time of the
Or One dose of Rabipur is given into the right deltoid
rst vaccination it must be administered not later than 7
muscle and one dose into the left deltoid muscle on day 0,
days after the first vaccination
and one dose is applied into the deltoid muscle on days 7
and 21 (2-1-1 regimen). In small children the vaccine is to
be given into the thighs.
* Observe manufacturer's instructions regarding administration
Immunocompromised patients and patients with a particularly high risk of contracting rabies
For immunocompromised patients, those with multiple wounds and/or wounds on the head or other highly innervated
areas, and those for whom there is a delay before initiation of treatment, it is recommended that:
- The days 0, 3, 7, 14 and 28 immunisation regimen should be used for these cases
-Two doses of vaccine may be given on day 0. That is, a single dose of 1 ml vaccine should be injected into the right
deltoid and another single dose into the left deltoid muscle. In small children, one dose should be given into the
anterolateral region of each thigh.
Severely immunosuppressed patients may not develop an immunologic response after rabies vaccination. Therefore,
prompt and appropriate wound care after an exposure is an essential step in preventing death. In addition, rabies
immune globulin should be administered in all immunosuppressed patients experiencing Category II and Category III
wounds.
In immunocompromised patients, the neutralising antibody titre should be measured 14 days after the rst injection.
Patients with a titre that is less than 0.5 IU/ml should be given another two doses of vaccine simultaneously and as soon
as possible. Further checks on the antibody titre should be made and further doses of vaccine should be administered
as necessary.
In all cases, the immunisation schedule must be followed exactly as recommended, even if the patient does not present
for treatment until a considerable time has elapsed since exposure.
Method of Administration
The vaccine should be given by intramuscular injection into the deltoid muscle, or into the anterolateral region of the
thigh in small children.
It must not be given by intra-gluteal injection.
Do not administer by intravascular injection (see Section 4.4).
4.3 Contraindications
Post-exposure prophylaxis
There are no contraindications to vaccination when post-exposure prophylaxis is indicated. However, subjects
considered to be at risk of a severe hypersensitivity reaction should receive an alternative rabies vaccine if a suitable
product is available (see also section 4.4 regarding previous hypersensitivity reactions).
Pre-exposure prophylaxis
Rabipur should not be administered to subjects with a history of a severe hypersensitivity reaction to any of the
ingredients in the vaccine. Note that the vaccine contains polygeline and residues of chicken proteins, and may contain
traces of neomycin, chlortetracycline and amphotericin B (see also section 4.4).
http://www.medicines.org.uk/emc/print-document?documentId=14933
3/8
8/29/2014
Rabipur - (eMC) print friendly
Vaccination should be delayed in subjects suffering from an acute febrile illness. Minor infections are not a
contraindication to vaccination.
4.4 Special warnings and precautions for use
As with all vaccines, appropriate medical treatment should be immediately available for use in the rare event of an
anaphylactic reaction to the vaccine.
A history of allergy to eggs or a positive skin test to ovalbumin does not necessarily indicate that a subject will be
allergic to Rabipur. However, subjects who have a history of a severe hypersensitivity reaction to eggs or egg products
should not receive the vaccine for pre-exposure prophylaxis. Such subjects should not receive the vaccine for postexposure prophylaxis unless a suitable alternative vaccine is not available, in which case all injections should be
administered with close monitoring and with facilities for emergency treatment.
Similarly, subjects with a history of a severe hypersensitivity reaction to any of the other ingredients in Rabipur such as
polygeline (stabilizer), or to amphotericin B, chlortetracycline or neomycin (which may be present as trace residues)
should not receive the vaccine for pre-exposure prophylaxis. The vaccine should not be given to such persons for postexposure prophylaxis unless a suitable alternative vaccine is not available, in which case precautions should be taken as
above.
Do not administer by intravascular injection
If the vaccine is inadvertently administered into a blood vessel there is a risk of severe adverse reactions, including
shock.
After contact with animals which are suspected carriers of rabies, it is essential to observe the following procedures
(according to WHO 1997):
Immediate wound treatment
In order to remove rabies virus, immediately cleanse wound with soap and ush thoroughly with water. Then treat with
alcohol (70%) or iodine solution. Where possible, bite injuries should not be closed with a suture, or only sutured to
secure apposition.
Tetanus vaccination and rabies immunoglobulin administration
Prophylaxis against tetanus should be implemented when necessary.
In cases of indicated passive immunisation, as much of the recommended dose of human rabies immunoglobulin (HRIG)
as anatomically feasible should be applied as deeply as possible in and around the wound. Any remaining HRIG should
be injected intramuscularly at a site distant from the vaccination site, preferably intragluteally. For detailed information
please refer to the SmPC and/or package insert of HRIG.
4.5 Interaction with other medicinal products and other forms of interaction
Patients who are immunocompromised, including those receiving immunosuppressive therapy, may not mount an
adequate response to rabies vaccine. Therefore, it is recommended that serological responses should be monitored in
such patients and additional doses given as necessary (see section 4.2 for details).
Administration of rabies immunoglobulin may be necessary for management but may attenuate the effects of
concomitantly administered rabies vaccine. Therefore, it is important that rabies immunoglobulin should be administered
once only for treating each at-risk exposure and with adherence to the recommended dose.
Other essential inactivated vaccines may be given at the same time as Rabipur. Different injectable inactivated vaccines
should be administered into separate injection sites.
4.6 Pregnancy and lactation
No cases of harm attributable to use of Rabipur during pregnancy have been observed. While it is not known whether
Rabipur enters breast milk, no risk to the breast-feeding infant has been identied. Rabipur may be administered to
pregnant and breastfeeding women when post-exposure prophylaxis is required.
The vaccine may also be used for pre-exposure prophylaxis during pregnancy and in breastfeeding women if it is
considered that the potential benet outweighs any possible risk to the fetus/infant.
4.7 Effects on ability to drive and use machines
http://www.medicines.org.uk/emc/print-document?documentId=14933
4/8
8/29/2014
Rabipur - (eMC) print friendly
The vaccine is unlikely to produce an effect on ability to drive and use machines.
4.8 Undesirable effects
In clinical studies the most commonly reported solicited adverse reactions were injection site pain (30 - 85%, mainly
pain due to injection) or injection site induration (15 - 35 %). Most injection site reactions were not severe and resolved
within 24 to 48 hours after injection. Furthermore, the following undesirable effects were observed in clinical trials and/or
during the post-marketing period:
Standard system organ class
Frequency
Adverse reactions
General disorders and administration
site condition
Very common> 1/10
Injection site pain, injection site
reaction, injection site induration,
injection site swelling
Common> 1/100, < 1/10
Asthenia, malaise, fever, chills,
fatigue, inuenza like illness, injection
site erythema
Uncommon >1/1.000, <1/100
Dizziness
Rare> 1/10.000, < 1/1.000
Circulatory reactions (such as
palpitations or hot ush)
Cardiac disorders
Blood and lymphatic system disorders Common> 1/100, < 1/10
Lymphadenopathy
Ear and labyrinth disorders
Very rare < 1/10.000
Vertigo
Eye disorders
Rare> 1/10.000, < 1/1.000
Visual disturbance
Common> 1/100, < 1/10
Headache
Rare> 1/10.000, < 1/1.000
Paraesthesia
Very rare < 1/10.000
Nervous system disorders (such as
paresis or Guillain-Barr-Syndrome)
Skin disorders
Common> 1/100, < 1/10
Rash
Immune system disorders
Very rare < 1/10.000
Allergic reactions (such as
anaphylaxis, bronchospasm, oedema,
urticaria or pruritus), Serum-sickness
like symptoms
Nervous system disorders*
Musculosceletal and connective tissue Common> 1/100, < 1/10
disorders
Myalgia, arthralgia
Gastrointestinal disorders
Gastrointestinal disorder (such as
nausea or abdominal pain)
Common> 1/100, < 1/10
* Statistically there is no indication of increasing frequencies of primary manifestations or triggered attacks of
autoimmune diseases (e.g. multiple sclerosis) after vaccination. However, in individual cases it cannot be absolutely
excluded that a vaccination may trigger an episode in patients with corresponding genetic disposition. According to the
current state of scientic knowledge vaccinations are not the cause of autoimmune diseases.
4.9 Overdose
No symptoms of overdose are known.
5. Pharmacological properties
5.1 Pharmacodynamic properties
ATC-Code: J07B G01
http://www.medicines.org.uk/emc/print-document?documentId=14933
5/8
8/29/2014
Rabipur - (eMC) print friendly
Pre-exposure Prophylaxis
In clinical trials with previously unimmunised subjects, almost all subjects achieve a protective antibody titre ( 0.5
IU/ml) by day 28 of a primary series of three injections of Rabipur when given according to the recommended schedule
by the intramuscular route.
As antibody titres slowly decrease, booster doses are required to maintain antibody levels above 0.5 IU/ ml. However,
persistence of protective antibody titres for 2 years after immunisation with Rabipur without additional booster has been
found to be 100 % in clinical trials.
In clinical trials, a booster dose of Rabipur elicited a 10-fold or higher increase in Geometric Mean Titres (GMTs) by day
30. It has also been demonstrated that individuals who had previously been immunised with Human Diploid Cell Vaccine
(HDCV) developed a rapid anamnestic response when boosted with Rabipur.
Persistence of antibody titres has been shown for 14 years in a limited number (n = 28) of subjects tested.
Nevertheless, the need for and timing of boosting should be assessed on a case by case basis, taking into account
official guidance (see also section 4.2).
Post-exposure Prophylaxis
In clinical studies, Rabipur elicited neutralising antibodies ( 0.5 IU/ml) in 98% of patients within 14 days and in 99-100%
of patients by day 28 38, when administered according to the WHO-recommended schedule of ve intramuscular
injections of 1 ml, one each on days 0, 3, 7, 14 and 28.
Concomitant administration of either Human Rabies Immunoglobulin (HRIG) or Equine Rabies Immunoglobulin (ERIG)
with the rst dose of rabies vaccine caused a slight decrease in GMTs. However, this was not considered to be clinically
relevant.
5.2 Pharmacokinetic properties
Not applicable.
5.3 Preclinical safety data
Preclinical data including single-dose, repeated dose and local tolerance studies revealed no unexpected ndings and no
target organ toxicity. No genotoxicity and reproductive toxicity studies have been performed.
6. Pharmaceutical particulars
6.1 List of excipients
Powder:
Solvent:
Trometamol
Water for injections
Sodium chloride
Disodium edetate
Potassium-L-glutamate
Polygeline
Sucrose
6.2 Incompatibilities
In the absence of compatibility studies, Rabipur must not be mixed in the same syringe with other medicinal products.
No interactions with concomitant administration of other vaccines have been reported.
6.3 Shelf life
4 years
6.4 Special precautions for storage
http://www.medicines.org.uk/emc/print-document?documentId=14933
6/8
8/29/2014
Rabipur - (eMC) print friendly
Store in a refrigerator (2C - 8C). Do not freeze.
6.5 Nature and contents of container
Pack containing:
Powder in a vial (type I glass) with stopper (chlorobutyl)
1 ml solvent for solution in an ampoule (type I glass)
with or without injection syringe (polypropylen with polyethylen plunger)
Not all pack sizes may be mark eted.
6.6 Special precautions for disposal and other handling
The vaccine should be visually inspected both before and after reconstitution for any foreign particulate matter and or
change in physical appearance. The vaccine must not be used if any change in the appearance of the vaccine has taken
place.
A clear colourless solution results after reconstitution of the white freeze-dried powder with the clear and colourless
solvent.
The powder for solution should be reconstituted using the solvent for solution supplied and carefully agitated prior to
injection. The reconstituted vaccine should be used immediately.
During manufacturing, the vial is sealed under vacuum. Therefore to prevent problems in withdrawing the reconstituted
vaccine from the vial after reconstitution of the vaccine, it is recommended to unscrew the syringe from the needle to
eliminate the negative pressure. After that, the vaccine can be easily withdrawn from the vial. It is not recommended to
induce excess pressure, since overpressurization will create the problems in withdrawing the proper amount of the
vaccine.
Any unused vaccine or waste material should be disposed of in accordance with local requirements.
7. Marketing authorisation holder
Novartis Vaccines and Diagnostics GmbH
P.O. Box 16 30
35006 Marburg
Germany
8. Marketing authorisation number(s)
PL 16033/0008
9. Date of first authorisation/renewal of the authorisation
12/05/2003 // 12/05/2008
10. Date of revision of the text
December 2009
RA10TJA008 April 2010
Company Contact Details
Novartis Vaccines
http://www.novartis.com
Address
Frimley Business Park, Frimley, Camberley, Surrey,
GU16 7SR
Fax
+44 (0)1276 698 460
Medical Information e-mail
http://www.medicines.org.uk/emc/print-document?documentId=14933
Telephone
+44 (0)1276 694 490
Medical Information Direct Line
+44 (0)8457 451 500
Medical Information Fax
+44 (0)1517 055 669
7/8
8/29/2014
Rabipur - (eMC) print friendly
service.uk@novartis.com
http://www.medicines.org.uk/emc/print-document?documentId=14933
8/8
You might also like
- Verorab PDFDocument8 pagesVerorab PDFเด็กชายท็อปปิ้ง ชอบกลิ้งเข้าคณะเภสัชศาสตร์No ratings yet
- Chirorab Prescribing InformationDocument2 pagesChirorab Prescribing Informationsr bNo ratings yet
- World Health Organization: WHO/EMC/ZOO/96.6Document25 pagesWorld Health Organization: WHO/EMC/ZOO/96.6silveoNo ratings yet
- Rabivax-S: Public Assessment ReportDocument8 pagesRabivax-S: Public Assessment ReportElsafani FaddiasyaNo ratings yet
- WHO _ RabiesDocument5 pagesWHO _ RabiesSatish Kumar DashNo ratings yet
- Rabies prevention and treatmentDocument8 pagesRabies prevention and treatmentenvadNo ratings yet
- Vero CellDocument2 pagesVero CellYawar AbbasNo ratings yet
- Post-Exposure Prophylaxis (PEP) : Rabies Exposure May Be Classified As Per WHO Into Three CategoriesDocument7 pagesPost-Exposure Prophylaxis (PEP) : Rabies Exposure May Be Classified As Per WHO Into Three CategoriesPramod KumarNo ratings yet
- National Rabies Control Programme GuidelineDocument7 pagesNational Rabies Control Programme GuidelineHari Pawan Kishore GarimellaNo ratings yet
- Treatment For RabiesDocument10 pagesTreatment For RabiesJomarNo ratings yet
- Revised Guidelines On The Management of Animal BiteDocument25 pagesRevised Guidelines On The Management of Animal BiteDarlene Anne Notario Jumawan100% (1)
- Rabies Vaccination and Post-Exposure ProphylaxisDocument5 pagesRabies Vaccination and Post-Exposure ProphylaxisJulian HuningkorNo ratings yet
- Vero RabDocument8 pagesVero RabHandoyo KooNo ratings yet
- Summary Product Charecteristics: Rabies Vaccine For Human Use, (Vero-Cell) Freeze-Dried (Speeda Vaccine)Document4 pagesSummary Product Charecteristics: Rabies Vaccine For Human Use, (Vero-Cell) Freeze-Dried (Speeda Vaccine)Ryll Dela CruzNo ratings yet
- PEP Prophylaxis Guideline 15 12 2014 PDFDocument27 pagesPEP Prophylaxis Guideline 15 12 2014 PDFjessicacookNo ratings yet
- JR Bagian TristanDocument4 pagesJR Bagian TristanTristan GantengNo ratings yet
- Canigen l4 Epar Product Information - en PDFDocument21 pagesCanigen l4 Epar Product Information - en PDFKris Pam Gorion PerezNo ratings yet
- Rabies ImmunizationDocument40 pagesRabies Immunizationruiza corcinoNo ratings yet
- Pentaxim-Pi-Sg Pen 0118 Spc0914Document10 pagesPentaxim-Pi-Sg Pen 0118 Spc0914walkrogNo ratings yet
- Manage Animal Bites & Prevent RabiesDocument10 pagesManage Animal Bites & Prevent RabiesWilly WizeNo ratings yet
- HBVAXPRO LeafletDocument100 pagesHBVAXPRO LeafletEllaNo ratings yet
- Animal BiteDocument51 pagesAnimal BiteJo-Ann Marie MendozaNo ratings yet
- WHO Guide For Rabies Pre and Post Exposure Prophylaxis in HumansDocument29 pagesWHO Guide For Rabies Pre and Post Exposure Prophylaxis in HumansMacky YongcoNo ratings yet
- Annex I Summary of Product CharacteristicsDocument81 pagesAnnex I Summary of Product CharacteristicsDesNo ratings yet
- Brand NameDocument5 pagesBrand NameJunrey AbarcaNo ratings yet
- Rabies PreventionDocument40 pagesRabies PreventionPranab MajumdarNo ratings yet
- AJMedP-4-11 SRD EDA V1 EDocument31 pagesAJMedP-4-11 SRD EDA V1 ELjupce GorgievskiNo ratings yet
- InfanrixhexaDocument18 pagesInfanrixhexacoleviper95No ratings yet
- Vaccine Timing CDCDocument40 pagesVaccine Timing CDCanindita.prasidha.parameswariNo ratings yet
- Animal Bite Module 2021Document20 pagesAnimal Bite Module 2021ERMED OFC R2TMCNo ratings yet
- Health Teaching RabiesDocument4 pagesHealth Teaching RabiesMeryl Encarnacion100% (1)
- Updated Guidelines on Management of Animal Bite PatientsDocument15 pagesUpdated Guidelines on Management of Animal Bite PatientsKaren ArchesNo ratings yet
- Nuvaxovid Epar Product Information enDocument31 pagesNuvaxovid Epar Product Information enKiss TiborNo ratings yet
- Guia de Vacunacion FelinaDocument5 pagesGuia de Vacunacion FelinaRaul KimNo ratings yet
- Rabies 052612Document80 pagesRabies 052612May Grace Noriega RolleNo ratings yet
- Vaccination SchedulesDocument3 pagesVaccination SchedulesJeffrey CarvajalNo ratings yet
- Guideline For Animal Bite Management FAQ-2021Document10 pagesGuideline For Animal Bite Management FAQ-2021apurva pareekNo ratings yet
- Brand Name: Verorab Contents: Indication / ActionDocument3 pagesBrand Name: Verorab Contents: Indication / ActionAbdelmar SusulanNo ratings yet
- Infanrix Ipv Pi AuDocument16 pagesInfanrix Ipv Pi Ausamm1982No ratings yet
- Rabies GuidelinesDocument21 pagesRabies Guidelineslotski100% (2)
- Vero RabDocument5 pagesVero RabMimiNo ratings yet
- Infanrix-Hexa SMPC 09 2020Document15 pagesInfanrix-Hexa SMPC 09 2020walkrogNo ratings yet
- Intra-dermal Rabies Vaccination TrainingDocument36 pagesIntra-dermal Rabies Vaccination Trainingimmunity100% (1)
- Sinopharm Vaccine - Guidelines - 06 - 06 - 2021updateDocument18 pagesSinopharm Vaccine - Guidelines - 06 - 06 - 2021updateChinthana චින්තනNo ratings yet
- Infanrix Hexa SMPC 2016 08 16Document14 pagesInfanrix Hexa SMPC 2016 08 16walkrogNo ratings yet
- Rabies PEP Guide - 2018Document1 pageRabies PEP Guide - 2018محمد ابراهيمNo ratings yet
- Rabies in the Philippines: Causes, Symptoms, Prevention and TreatmentDocument17 pagesRabies in the Philippines: Causes, Symptoms, Prevention and TreatmentJoshua VillarbaNo ratings yet
- Rabies and Intradermal Rabies Vaccination: Alan C. Jackson, MDDocument32 pagesRabies and Intradermal Rabies Vaccination: Alan C. Jackson, MDLemuel GuevarraNo ratings yet
- Nervous Tissue Anti-Rabies Vaccine For Human UseDocument2 pagesNervous Tissue Anti-Rabies Vaccine For Human UseLet BNo ratings yet
- AO RabiesDocument21 pagesAO RabiesChristopher Owen T. JOCSONNo ratings yet
- Dog Bite Show NotesDocument5 pagesDog Bite Show NotesLakshay ChananaNo ratings yet
- Annex I Summary of Product CharacteristicsDocument18 pagesAnnex I Summary of Product CharacteristicsfrankyNo ratings yet
- Leaflet Rotarix Liquid gds15 Ipi11Document10 pagesLeaflet Rotarix Liquid gds15 Ipi11zeinfahmi16No ratings yet
- Varilrix Serbuk Injeksi 2000 PFU, Dosis - Vaksin Varisela - Zoster - DKI9676701044A1 - 2018 - 3Document8 pagesVarilrix Serbuk Injeksi 2000 PFU, Dosis - Vaksin Varisela - Zoster - DKI9676701044A1 - 2018 - 3rianaNo ratings yet
- Introduction: Hepatitis A Maurice HillemanDocument19 pagesIntroduction: Hepatitis A Maurice Hillemanahmed solimanNo ratings yet
- 6.2017. Rabies Post Exposure VaccineDocument2 pages6.2017. Rabies Post Exposure VaccineKhairul NizamNo ratings yet
- Annex I Summary of Product CharacteristicsDocument33 pagesAnnex I Summary of Product CharacteristicsVimala BohoNo ratings yet
- Health Advice and Immunizations for TravelersFrom EverandHealth Advice and Immunizations for TravelersNo ratings yet
- Good Health in the Tropics: Advice to Travellers and SettlersFrom EverandGood Health in the Tropics: Advice to Travellers and SettlersNo ratings yet
- Oil and Gas March 2014Document43 pagesOil and Gas March 2014Ramya SahitiNo ratings yet
- Lecture 06Document28 pagesLecture 06shreyas_chandor3802No ratings yet
- J 17 14 Iii PDFDocument24 pagesJ 17 14 Iii PDFPrakash Ku. SamantsingharNo ratings yet
- Lecture 06Document28 pagesLecture 06shreyas_chandor3802No ratings yet
- Empowering PeopleDocument86 pagesEmpowering Peopleshreyas_chandor3802No ratings yet
- Suppose A Researcher Wishes To Test Whether The Average Writing Score (Write) Differs Significantly From 50Document7 pagesSuppose A Researcher Wishes To Test Whether The Average Writing Score (Write) Differs Significantly From 50shreyas_chandor3802No ratings yet
- Rabies - WHODocument43 pagesRabies - WHOsilveoNo ratings yet
- ETHNOBOTANY OF THE ZUÑI Stevenson PDFDocument74 pagesETHNOBOTANY OF THE ZUÑI Stevenson PDFwienslaw5804No ratings yet
- Vestil V IAC DigestDocument1 pageVestil V IAC DigestKathNo ratings yet
- English Notes on Prose PassagesDocument7 pagesEnglish Notes on Prose PassagesAdrees AhmedNo ratings yet
- LMR Book 2018Document52 pagesLMR Book 2018Mohamed ArsathNo ratings yet
- Communicable Disease NursingDocument50 pagesCommunicable Disease NursingChernobyle Tolentino BattadNo ratings yet
- World Rabies Day: Working Together To Make Rabies History!Document7 pagesWorld Rabies Day: Working Together To Make Rabies History!Dr.Kedar Karki ,M.V.Sc.Preventive Vet.Medicine CLSU PhilippinesNo ratings yet
- tmpF8F9 TMPDocument48 pagestmpF8F9 TMPFrontiersNo ratings yet
- RESOLUTION Anti RabiesDocument2 pagesRESOLUTION Anti RabiesBarangay Cupang ProperNo ratings yet
- Rabipur - (EMC) Print FriendlyDocument8 pagesRabipur - (EMC) Print Friendlyshreyas_chandor3802No ratings yet
- ASPCA Guide To Handling Pit Bulls in Shelter EnvironmentsDocument19 pagesASPCA Guide To Handling Pit Bulls in Shelter EnvironmentsDogsBite.org64% (11)
- v19 n4Document178 pagesv19 n4Jaa DeeNo ratings yet
- Category C Dog Cat Import Flowchart Apr2018Document4 pagesCategory C Dog Cat Import Flowchart Apr2018J FNo ratings yet
- Rabies: A Deadly Viral Disease Spread by Animal BitesDocument3 pagesRabies: A Deadly Viral Disease Spread by Animal BitesDavid CalaloNo ratings yet
- MICROBIOLOGY 2010 REVIEWDocument25 pagesMICROBIOLOGY 2010 REVIEWMicole Manahan100% (1)
- Introduction Scope and Historical Development of Veterinary Microbiology Lecture NotesDocument11 pagesIntroduction Scope and Historical Development of Veterinary Microbiology Lecture Noteskaran kamboj0% (1)
- RABIES Causative Agent: Rhabdovirus Mode of Transmission: Bite of RabidDocument1 pageRABIES Causative Agent: Rhabdovirus Mode of Transmission: Bite of RabidFreeNursingNotes100% (1)
- Vis RabiesDocument2 pagesVis RabiesSanjay KumarNo ratings yet
- Zoonoses transmitted between animals and humansDocument9 pagesZoonoses transmitted between animals and humansAjita RayNo ratings yet
- Project File On Human Health and Disease.Document21 pagesProject File On Human Health and Disease.Sanampreet90% (31)
- Red Tide Algae Bloom Causes Paralytic Shellfish PoisoningDocument41 pagesRed Tide Algae Bloom Causes Paralytic Shellfish PoisoningLily CentenoNo ratings yet
- Rabeis ControlDocument8 pagesRabeis ControlmohannadNo ratings yet
- PSM Park MCQsDocument91 pagesPSM Park MCQsGIST (Gujarat Institute of Science & Technology)82% (28)
- Microbial Diseases of The Nervous SystemDocument7 pagesMicrobial Diseases of The Nervous SystemAnaNo ratings yet
- IATA - USA Customs, Currency & Airport Tax Regulations DetailsDocument4 pagesIATA - USA Customs, Currency & Airport Tax Regulations DetailsMartinaNo ratings yet
- Rabies and Rabies-Related Lyssaviruses: ImportanceDocument10 pagesRabies and Rabies-Related Lyssaviruses: ImportanceSophieNo ratings yet
- Drug Form 2Document5 pagesDrug Form 2Kwesi YasayNo ratings yet
- Animal Bite Clerking SheetDocument1 pageAnimal Bite Clerking Sheetleo89azmanNo ratings yet
- Module 1b: People Who Make A DifferenceDocument29 pagesModule 1b: People Who Make A DifferenceIsobel PJ Campomanes100% (1)
- Republic of The Philippines Province of Misamis Oriental Municipality of Villanueva Barangay Poblacion 3Document11 pagesRepublic of The Philippines Province of Misamis Oriental Municipality of Villanueva Barangay Poblacion 3Lovejoy Dagasuhan100% (2)