Professional Documents
Culture Documents
The Mechanisms of Inflammation in Gout and Pseudogout (CPP-induced Arthritis)
Uploaded by
Melisa WalkerOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Mechanisms of Inflammation in Gout and Pseudogout (CPP-induced Arthritis)
Uploaded by
Melisa WalkerCopyright:
Available Formats
review
Reumatismo, 2011; 63 (4): 230-237
The mechanisms of inflammation in gout
and pseudogout (CPP-induced arthritis)
N. Busso1, H.-K. Ea2
DAL, Service de Rhumatologie, Centre Hospitalier Universitaire Vaudois, University of Lausanne,
Switzerland;
2
INSERM, UMR-S 606, Hospital Lariboisire, and Univ. Paris Diderot (UFR de Mdecine),
Sorbonne Paris Cit, France
1
SUMMARY
Recent advances have stimulated new interest in the area of crystal arthritis, as microcrystals can be considered
to be endogenous danger signals and are potent stimulators of immune as well as non-immune cells. The best
known microcrystals include urate (MSU), and calcium pyrophosphate (CPP) crystals, associated with gout
and pseudogout, respectively.
Acute inflammation is the hallmark of the acute tissue reaction to crystals in both gout and pseudogout. The
mechanisms leading to joint inflammation in these diseases involve first crystal formation and subsequent coating with serum proteins. Crystals can then interact with plasma cell membrane, either directly or via membrane
receptors, leading to NLRP3 activation, proteolytic cleavage and maturation of pro-interleukin-1 (pro-IL1)
and secretion of mature IL1. Once released, this cytokine orchestrates a series of events leading to endothelial
cell activation and neutrophil recruitment. Ultimately, gout resolution involves several mechanisms including
monocyte differentiation into macrophage, clearance of apoptotic neutrophils by macrophages, production of
Transforming Growth Factor (TGF-) and modification of protein coating on the crystal surface. This review
will examine these different steps.
Key words: urate, calcium pyrophosphate crystals, gout, pseudogout, inflammasome, IL1, danger signals, syk
kinase.
Reumatismo, 2011; 63 (4): 230-237
n INTRODUCTION
Corresponding author:
Nathalie Busso
DAL, Service de Rhumatologie
CHUV, Nestl 05-5029
1011 Lausanne, Switzerland
E-mail: Nathalie.Busso@chuv.ch
230
Reumatismo 4/2011
yperuricemia is the metabolic abnormality underlying gout, an inflammation of the joints that was already
recognized by the ancient Greeks (e.g.
Hippocrates and his aphorisms on gout,
5th century BC). Gout has continued to
fascinate physicians and scientists over
the centuries. The link with hyperuricemia
as the underlying metabolic abnormality
started with the identification of uric acid
in 1776, and progressed through to the
famous thread test that Garrod used in
1848 to demonstrate that blood in gouty
patients contained significant quantities
of urate. In 1961, McCarty and Hollander
published their observations that crystals
obtained from the joints of gout patients
were composed of monosodium urate (1).
For many, the clinical problem of gout and
its treatment would appear to be solved.
However, to our surprise, the subject is still
proving to be a rewarding topic for clinical
investigation, and recent research has led
to a renewal of interest in the mechanisms
underlying the metabolic abnormality, as
well as possible links between hyperuricemia and cardiovascular and metabolic
disorders.
Calcium pyrophosphate (CPP) deposition occurs mainly in joint cartilage and
intervertebral disc, specifically in hyaline
and fibro-cartilage. In order to clarify and
to provide a uniform definition of CPP
deposition (CPPD) disease, the European
League Against Rheumatism (EULAR)
task force has recently compiled two sets
of recommendations concerning first the
diagnosis and terminology, and second the
management of the disease (2, 3). Thus,
CPPD is the umbrella term for all instances
of CPP crystal occurrence, and chondrocalcinosis (CC) means cartilage calcification,
The mechanisms of inflammation in gout and pseudogout (CPP-induced arthritis)
identified by imaging or histological examination. CC is not always due to CPPD
and may occur as an isolated finding in an
apparently otherwise normal joint, or coexist with structural changes resembling osteoarthritis. Several types and dimensions of
CPP crystals have been identified in synovial fluid (SF) including monoclinic and
triclinic dihydrated CPP crystals (m-CPP
and t-CPP: Ca2P2O7, 2H2O) (4). Although
often asymptomatic, CPP crystal deposition can be associated with osteoarthritis,
acute mono- or oligo-articular arthritis and,
more rarely, chronic polyarthritis and destructive arthropathy (2). Acute mono-or
oligo-articular arthritis secondary to CPP
crystal deposition can mimic gout attacks
and has, therefore, been initially referred
to as pseudogout. Interestingly, both MSU
and CPP crystal-induced inflammation resolve themselves spontaneously.
Last but not least, based on the discovery of
the inflammasome and of its activation by
MSU and CPP crystals, research has produced new treatments that may be of great
relevance to patients suffering from gout,
and eventually also pseudogout.
n MSU and CPP crystal
formation
MSU crystallizes when its plasma concentration exceeds its solubility (around
7 mg/dL, or 420 mol/L). Concentration
may not be the only determinant, since we
know from clinical observation that patients with hyperuricemia can be asymptomatic, sometimes for long periods before
the first presentation of gout, so there must
be modifying factors present in biological
fluids that affect urate solubility. In vitro,
several factors have been described as influencing urate solubility, including pH,
temperature, ionic strength and the binding
of urate to plasma macromolecules (5). Not
only is the solubility of urate influenced by
its binding to plasma proteins, but also its
inflammatory potential (see below).
The mechanisms of CPP crystal deposition
in human cartilage are still not clear and involve chondrocyte alterations and extracel-
review
lular matrix (ECM) modifications. Recognized risk factors of cartilage mineralization are aging, osteoarthritis, previous joint
trauma or injury, metabolic disease and familial predisposition (6). Cartilage calcification depends on cartilage cells (chondrocytes), ECM proteins and ECM concentration of Ca2+, inorganic phosphate (Pi), and
inorganic pyrophosphate (PPi). Extracellular PPi is produced either de novo through
the extracellular metabolism of nucleotides
or originates from the release of intracellular PPi (7). The concentration of extracellular PPi depends chiefly on four proteins:
membrane glycoprotein-1 or PC-1, tissue
non-specific alkaline phosphatase (ALP),
the PPi transmembrane transporter ANK
and CD73 protein (7, 8). Extracellular PPi
concentration is increased by PC-1, ANK
and CD73 and decreased by ALP, which
hydrolyzes PPi. PC-1, ANK and ALP expression is modulated by cytokines and
growth factors, as well as by Pi and PPi
ions. Thus, TGF-b increases ANK expression and CPP crystal formation (9), whereas insulin growth factor-1 has the opposite
effect (10). Similarly, intracellular PPi decreases the transcription of both ANK and
PC-1 mRNAs, whereas Pi has the opposite
effect (6).
n Cellular recognition
of crystals
The cells interacting and responding to
crystals are leukocytes, in particular neutrophils and macrophages, but also endothelial cells, synoviocytes and mast
cells (11, 12). Resident macrophages are
of particular interest, as they have been
reported to play a role in initiating the tissue response to MSU in a mouse peritonitis model (13). Mast cells also deserve
a mention, as in the peritonitis model
of gout, depletion of peritoneal mast
cells attenuated the neutrophil inflammatory response (14). Finally, resident
macrophages and mast cells are able to
release IL-1 upon crystal activation of
the NALP3 inflammasome (see below).
These results suggest that these cells parReumatismo 4/2011
231
review
N. Busso, H.-K. Ea
ticipate in the acute response of tissue to
MSU and CPPD crystals and contribute to
neutrophil recruitment. Thus, inflammation initiation would depend on resident
cells, which have been partly identified,
whereas the amplification of the inflammatory reaction includes mast cells,
macrophages, monocytes, endothelial
cells and PNN. The essential questions
are: how are crystals recognized by cells
and what cellular signaling is involved
in their response? The first mechanism
in the interaction between crystals and
cells involves phagocytosis which was
shown to be essential for the activation of
neutrophils and macrophages, and in the
case of macrophages, Toll-like receptors
(TLRs) may play a role. TLRs are pivotal
sensors of danger signals and infection on
leukocytes, and are an integral part of the
innate immune system (15). In this context, MSU crystals may be a danger signal released from injured cells that trigger innate immune responses via TLRs.
Experimental evidence is available which
shows a role for TLR2 and TLR4 in MSU
recognition by monocyte/macrophages, as
the presence of TLR2 and TLR4 exacerbated MSU crystal-induced IL-1 production and PMN recruitment in the murine
air pouch model (16). Similarly, CPP and
MSU crystals trigger nitric oxide production through TLR-2 activation in articular
chondrocytes (17). However, these results
should be viewed with caution since another group found that none of the known
TLRs were essential in the murine peritonitis model (18).
A second mechanism may involve a direct
interaction between crystals and cell membrane leading to intracellular signaling
cascades. Indeed, atomic force microscopy
has shown that specific interaction of MSU
crystals with dendritic cell membrane occurs (19). This interaction led to activation
of the tyrosine kinase Syk that might mediate either internalization of the crystal or a
cellular response to the binding of the crystal (20, 21). However, there is still no evidence for direct binding of MSU crystals to
other cell membranes apart from dendritic
cell membranes. Finally, there are no re232
Reumatismo 4/2011
ports to date of direct interactions between
CPP crystals and cell membranes and Syk
activation.
A third mechanism involves proteins coated at the crystal surface. Indeed, several
proteins have been identified on both MSU
and CPP crystal surfaces, including complement fractions such as C1q, C5 and C6,
IgG and IgM immunoglogulins, Fc fragment of Ig, apolipoproteins E (ApoE), high
density lipoproteins and low density lipoproteins (22-25).
These coating proteins play an important
role in the inflammatory reaction and its
resolution. Thus, the complement fraction stimulates PNN recruitment, whereas
ApoE protein promotes inflammation resolution (26). For instance, knee joint inflammation induced by MSU crystal injection
was inhibited in C6 deficient rabbits which
displayed less IL-8 production and PNN
influx in the knee (27). Finally, opsonization of IgG and/or complement fractions
also favor crystal phagocytosis and cell activation.
n MSU and CPP activation
of NLRP3 inflammasome
and secretion of IL-1
Proinflammatory cytokines undoubtedly
play a critical role in orchestrating the inflammatory reaction to MSU crystals. Recent attention has focused in particular on
the role of IL-1. IL-1 is the prototypic
inflammatory cytokine and exerts different types of action on cells and tissues. The
cytokine is produced as an inactive promolecule by immune cells such as macrophages, monocytes and dendritic cells, and
is then cleaved into the active p17 form of
IL-1 to be secreted out of the cell. Cleavage of pro-IL-1 is catalyzed by caspase-1
(also known as IL-1- converting enzyme,
ICE). Caspase-1 is a member of the family of inflammatory caspases that include
caspase-4, caspase-5, caspase-11 and caspase-12; in the context of IL-1 processing, caspase-1 accounts for the main activity that requires the formation of a molecular platform known as the inflammasome
The mechanisms of inflammation in gout and pseudogout (CPP-induced arthritis)
(28). Other pathways of IL-1 processing
independent of caspase-1 have been described, implicating neutrophil-derived and
mast cell-derived proteases (29, 30).
The NLRP3 inflammasome is a cytoplasmic protein complex composed of NLRP3,
a protein of the NLRP (or NALP) family,
an adapter ASC protein as well as the inflammatory caspase-1. The ASC adapter
contains a PYD domain that mediates interaction with a homologous domain on
NLRP, as well as a CARD domain that
interacts with caspase-1 (Figure 1). The
group of Tschopp discovered that many
review
inorganic particles, including MSU and
CPP crystals, are capable of activating the
NLRP3 inflammasome to process and secrete active IL-1 as well as IL-18 (31).
The list of NRLP3 triggers is still growing,
and includes alum, hemozoin and DNA.
Macrophages deficient for components of
the NLRP3 inflammasome were unable to
secrete active IL-1 following stimulation
with MSU and CPP crystals. Moreover,
MSU-induced peritonitis was decreased in
ASC-deficient or caspase-1-deficient mice.
Colchicine, a drug commonly used in the
treatment of acute gout, was found to block
Figure 1 - Initiation and amplification of joint inflammation by crystals. Crystals into the joint
cavity are covered by serum proteins (C3a, C5a et C5b-9) and/or immunoglobulin G (IgG) and
activate resident cells such as macrophages and mast cells, or eventually also non-hematopoietic cells (such as synoviocytes and endothelial cells) (step 1). These cells will produce
inflammatory cytokines and chemokines such as IL1, IL8 and MCP-1, which in turn will activate endothelial cells (which will then start to express E-selectin) and stimulate monocyte and
polymorphonuclear neutrophil cell (PNN) infiltrate (step 2). Infiltrating cells will also contribute
to further IL-1 and IL-8 secretion (step 3) thereby amplifying the inflammatory reaction by
recruiting additional inflammatory cells (step 4).
Reumatismo 4/2011
233
review
N. Busso, H.-K. Ea
IL-1 maturation, probably by influencing
crystal endocytosis and/or presentation of
crystals to the inflammasome. The results
show that MSU crystals initiate an inflammatory cascade, the starting point being
the release of active IL-1 from monocytes
and macrophages.
These findings, however, also raise questions about the steps that connect cellular
contact with crystals with inflammasome
activation, processes that are still not completely understood. It may involve general
mechanisms shared by other inflammasome activators, such as potassium efflux
that is regulated by K+ channels like P2X7,
or by the sensing of reactive oxygen species that are released during cell stress and
the release of lysosomal contents such as
cathepsin B. The different mechanisms involved in crystal cellular recognition and
activation of NLRP3 inflammasome are
summarized in Figure 2.
In a study published in 2010, Joosten et
al. provide important new insights into
the mechanisms underlying gout inflammation (30). It is known that patients can
have MSU deposits that are clinically quiescent, indicating that there is further regu-
Figure 2 - Crystal activation of the NLRP3 inflammasome. NLRP3 or cryopyrin is composed
of three distict domains (NACHT-LRR-PYD domains) and belongs to the NOD-like receptors
involved in innate immunity. The inflammasome, formed by NLRP3 (NLRP3 inflammasome),
binds to ASC (apoptosis-associated speck-like protein containing a CARD). ASC in turn will
bind to caspase-1 (Cas-1), previously known as interleukin-converting enzyme (ICE). Different mechanisms are involved in the inflammasome activation: direct crystal interaction with
the cell membrane and subsequent tyrosine kinase Syk activation; crystal interaction with
cell membrane receptors such as TLR (Toll-like receptor) and phagocytosis of crystals. Upon
phagocytosis, crystals induce K+ efflux via ATP binding to P2X7R, reactive oxygen species
(ROS) generation and lysosomal damage (probably via cathepsin B release). These events
lead to NLRP3 inflammasome activation. The resulting autocatalytic activation of caspase-1
then induces pro-IL1 (Mw 35 kD) cleavage into biologically active IL-1 (Mw 17 kD). Although
Syk kinase activation is independent of inflamamsome activation, lysosomal damage may be
a common step for both pathways. Finally, there is as yet no evidence for CPP crystal binding
and Syk activation.
234
Reumatismo 4/2011
The mechanisms of inflammation in gout and pseudogout (CPP-induced arthritis)
lation at the level of the tissue response to
urate crystals. It is important to underline
here that reports claiming that MSU crystals are potent inducers of IL-1 production have been performed in cell lines that
were pre-activated with PMA or LPS. Such
pre-activation is necessary for the induction of both IL-1 mRNA and pro IL-1.
In experiments using pure MSU alone, no
cytokine was released. It was convincingly
demonstrated that free fatty acids C18:0
acting on Toll-like receptor 2 (TLR-2) can
synergize with MSU crystals in order to
induce inflammasome activation and cytokine release.
This demonstrates that the release of FFAs
after food ingestion or alcohol consumption represents the missing link between
metabolic changes, inflammasome activation, and gout attacks (30).
n Mechanisms secondary
to IL-1 release
We have seen above that, through a series of steps that are still not well understood, MSU crystals activate the NLRP3
inflammasome of phagocytes, resulting in
processing and secretion of IL-1.
The subsequent recruitment of inflammatory leukocytes to the site, most probably
mediated by endothelial activation, can
account for the subsequent release of inflammatory mediators and the recognized
inflammatory manifestations of acute gout
(Figure 1).
Although crystals have been shown to induce multiple cytokines and chemokines
that promote gouty inflammation, including tumor necrosis factor- (TNF-), IL6, CXC-chemokine ligand (CXCL) 1 and
CXCL8 (also known as IL-8), it has been
suggested that these are produced in a hierarchical manner, secondary to IL-1 release. For instance, in experimental MSUinduced inflammation, IL-1 has a more
central role than TNF- (32). Nevertheless,
in different experimental settings, a role for
CXCL8 has been clearly demonstrated in
both CPP and MSU crystal-induced inflammation (33-35).
review
Mechanisms underlying spontaneous resolution of acute inflammation
Despite the rapid onset and the severity
of crystal-associated inflammation, there
is a self-limiting factor in the gout crisis
and a return ad integrum of the affected
joint. The first explanation provided for the
resolution of inflammation is the nature of
the coating of the crystals. Indeed, it was
shown that crystals coated with IgG fragments were more inflammatory than naked
crystals (36), whereas crystals coated with
ApoB and ApoE could contribute in part
to the resolution of acute gouty arthritis
(37). Another mechanism involved in the
resolution of microcrystal-induced arthritis flares involves the physiological transformation of monocyte into macrophage.
Indeed, when macrophages were differentiated in vitro, they became less proinflammatory in their response to MSU crystals,
even though they retained their capacity
for phagocytosis (38). The difference in the
cellular response seems also to be linked to
the state of the macrophage and the phenotypic variations of macrophages (M1
and M2 macrophages) (39). The switch
monocyte-macrophage has been observed
during gout flare resolution and is associated not only with a decrease in the synthesis
of proinflammatory cytokines (IL-1, IL-6,
TNF-), but also with an increased production of anti-inflammatory cytokines (IL10 and TGF-) (40). Hence macrophages
start to produce TGF-, a key cytokine in
this anti-inflammatory process (41). This
TGF- can thus reduce endothelial cell activation, thus limiting PNN and monocyte
recruitment and also cytokine expression,
such as IL-1 and its receptor. In addition
TGF- secretion is stimulated by macrophagic clearance of apoptotic neutrophils.
In this context it should be noted that apoptotic neutrophil clearance can be favored
by type 2 transglutaminase (42). In conclusion, the autoregulation of inflammation by
phagocytes together with differential coating of MSU crystals may explain the selflimiting nature of acute gout, as well as the
fact that the presence of MSU crystals in a
joint is not always accompanied by inflammatory response
Reumatismo 4/2011
235
review
N. Busso, H.-K. Ea
Abbreviations
ASC, apoptosis-associated speck-like protein containing a caspase recruitment domain; IL, interleukin; MSU, monosodium
urate; NALP3, NACHT-containing, LRRcontaining and PYD-containing protein;
NF, nuclear factor; TLR, Toll-like receptor;
TNF-, tumour necrosis factor-. TGF-,
Transforming Growth Factor-; ECM, extracellular matrix.
n REFERENCES
1. Shi Y, Mucsi AD, Ng G. Monosodium urate
crystals in inflammation and immunity. Immunol Rev 2010; 233: 203-17.
2. Zhang W, Doherty M, Bardin T, et al. European League Against Rheumatism recommendations for calcium pyrophosphate deposition. Part I: terminology and diagnosis. Ann
Rheum Dis 2011; 70: 563-70.
3. Zhang W, Doherty M, Pascual E, et al. EULAR recommendations for calcium pyrophosphate deposition. Part II: management.
Ann Rheum Dis 2011; 70: 571-75.
4. Swan A, Heywood B, Chapman B, et al. Evidence for a causal relationship between the
structure, size, and load of calcium pyrophosphate dihydrate crystals, and attacks of pseudogout. Ann Rheum Dis 1995; 54: 825-30.
5. Kippen I, Klinenberg JR, Weinberger A, Wilcox WR. Factors affecting urate solubility in
vitro. Ann Rheum Dis 1974; 33: 313-7.
6. Ea HK, Nguyen C, Bazin D, et al. Articular
cartilage calcification in osteoarthritis: insights into crystal-induced stress. Arthritis
Rheum 2011; 63: 10-8.
7. Terkeltaub RA. Inorganic pyrophosphate generation and disposition in pathophysiology.
Am J Physiol Cell Physiol 2001; 281: C1C11.
8. St Hilaire C, Ziegler SG, Markello TC, et al.
NT5E mutations and arterial calcifications. N
Engl J Med 2011; 364: 432-42.
9. Cailotto F, Bianchi A, Sebillaud S, et al. Inorganic pyrophosphate generation by transforming growth factor-beta-1 is mainly dependent
on ANK induction by Ras/Raf-1/extracellular
signal-regulated kinase pathways in chondrocytes. Arthritis Res Ther 2007; 9: R122.
10. Hirose J, Ryan LM, Masuda I. Up-regulated
expression of cartilage intermediate-layer
protein and ANK in articular hyaline cartilage
from patients with calcium pyrophosphate
dihydrate crystal deposition disease. Arthritis
Rheum 2002; 46: 3218-29.
11. Busso N, So A. Mechanisms of inflammation
in gout. Arthritis Res Ther 2010; 12: 206.
236
Reumatismo 4/2011
12. So A, Busso N. A magic bullet for gout? Ann
Rheum Dis 2009; 68: 1517-9.
13. Martin WJ, Walton M, Harper J. Resident
macrophages initiating and driving inflammation in a monosodium urate monohydrate
crystal-induced murine peritoneal model of
acute gout. Arthritis Rheum 2009; 60: 281-9.
14. Getting SJ, Flower RJ, Parente L, et al. Molecular determinants of monosodium urate
crystal-induced murine peritonitis: a role for
endogenous mast cells and a distinct requirement for endothelial-derived selectins. J Pharmacol Exp Ther 1997; 283: 123-30.
15. Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol 2004; 4: 499-511.
16. Liu-Bryan R, Scott P, Sydlaske A, et al. Innate immunity conferred by Toll-like receptors 2 and 4 and myeloid differentiation factor
88 expression is pivotal to monosodium urate
monohydrate crystal-induced inflammation.
Arthritis Rheum 2005; 52: 2936-46.
17. Liu-Bryan R, Pritzker K, Firestein GS, Terkeltaub R. TLR2 signaling in chondrocytes drives
calcium pyrophosphate dihydrate and monosodium urate crystal-induced nitric oxide generation. J Immunol 2005; 174: 5016-23.
18. Chen CJ, Shi Y, Hearn A, et al. MyD88-dependent IL-1 receptor signaling is essential
for gouty inflammation stimulated by monosodium urate crystals. J Clin Invest 2006; 116:
2262-71.
19. Ng G, Sharma K, Ward SM, et al. Receptorindependent, direct membrane binding leads
to cell-surface lipid sorting and Syk kinase activation in dendritic cells. Immunity 2008; 29:
807-18.
20. Popa-Nita O, Proulx S, Pare G, et al. Crystalinduced neutrophil activation: XI. Implication
and novel roles of classical protein kinase C. J
Immunol 2009; 183: 2104-14.
21. Popa-Nita O, Rollet-Labelle E, Thibault N, et
al. Crystal-induced neutrophil activation. IX.
Syk-dependent activation of class Ia phosphatidylinositol 3-kinase. J Leukoc Biol 2007;
82: 763-73.
22. Burt HM, Jackson JK, Rowell J. Calcium pyrophosphate and monosodium urate crystal
interactions with neutrophils: effect of crystal size and lipoprotein binding to crystals. J
Rheumatol 1989; 16: 809-17.
23. Terkeltaub R, Tenner AJ, Kozin F, Ginsberg
MH. Plasma protein binding by monosodium
urate crystals. Analysis by two-dimensional
gel electrophoresis. Arthritis Rheum 1983; 26:
775-83.
24. Terkeltaub RA, Dyer CA. Martin J, Curtiss
LK. Apolipoprotein (apo) E inhibits the capacity of monosodium urate crystals to stimulate
neutrophils. Characterization of intraarticular
apo E and demonstration of apo E binding to
urate crystals in vivo. J Clin Invest 1991; 87:
20-6.
The mechanisms of inflammation in gout and pseudogout (CPP-induced arthritis)
25. Terkeltaub RA, Santoro DA, Mandel G, Mandel N. Serum and plasma inhibit neutrophil
stimulation by hydroxyapatite crystals. Evidence that serum alpha 2-HS glycoprotein is
a potent and specific crystal-bound inhibitor.
Arthritis Rheum 1988; 31: 1081-9.
26. Popa-Nita O, Naccache PH. Crystal-induced
neutrophil activation. Immunol Cell Biol
2010; 88: 32-40.
27. Tramontini N, Huber C, Liu-Bryan R, et al.
Central role of complement membrane attack
complex in monosodium urate crystal-induced
neutrophilic rabbit knee synovitis. Arthritis
Rheum 2004; 50: 2633-9.
28. Martinon F. Mechanisms of uric acid crystalmediated autoinflammation. Immunol Rev
2010; 233: 218-32.
29. Joosten LA, Netea MG, Fantuzzi G, et al.
Inflammatory arthritis in caspase 1 gene-deficient mice: contribution of proteinase 3 to
caspase 1-independent production of bioactive
interleukin-1beta. Arthritis Rheum 2009; 60:
3651-62.
30. Joosten LA, Netea MG, Mylona E, et al. Engagement of fatty acids with Toll-like receptor
2 drives interleukin-1beta production via the
ASC/caspase 1 pathway in monosodium urate
monohydrate crystal-induced gouty arthritis.
Arthritis Rheum 2010; 62: 3237-48.
31. Martinon F, Petrilli V, Mayor A, et al. Gout-associated uric acid crystals activate the NALP3
inflammasome. Nature 2006; 440: 237-41.
32. So A, De Smedt T, Revaz S, Tschopp J. A pilot
study of IL-1 inhibition by anakinra in acute
gout. Arthritis Res Ther 2007; 9: R28.
33. Nishimura A, Akahoshi T, Takahashi M, et
al. Attenuation of monosodium urate crystalinduced arthritis in rabbits by a neutralizing
antibody against interleukin-8. J Leukoc Biol
1997; 62: 444-9.
34. Terkeltaub R, Baird S, Sears P, et al. The
murine homolog of the interleukin-8 receptor CXCR-2 is essential for the occurrence
of neutrophilic inflammation in the air pouch
model of acute urate crystal-induced gouty
review
synovitis. Arthritis Rheum 1998; 41: 900-9.
35. Hachicha M, Naccache PH, McColl SR. Inflammatory microcrystals differentially regulate the secretion of macrophage inflammatory protein 1 and interleukin 8 by human neutrophils: a possible mechanism of neutrophil
recruitment to sites of inflammation in synovitis. J Exp Med 1995; 182: 2019-25.
36. Ginsberg MH, Kozin F. Mechanisms of cellular interaction with monosodium urate crystals. IgG-dependent and IgG-independent
platelet stimulation by urate crystals. Arthritis
Rheum 1978; 21: 896-903.
37. Ortiz-Bravo E, Sieck MS, Schumacher HR Jr.
Changes in the proteins coating monosodium
urate crystals during active and subsiding inflammation. Immunogold studies of synovial
fluid from patients with gout and of fluid obtained using the rat subcutaneous air pouch
model. Arthritis Rheum 1993; 36: 1274-85.
38. Landis RC, Yagnik DR, Florey O, et al. Safe
disposal of inflammatory monosodium urate
monohydrate crystals by differentiated macrophages. Arthritis Rheum 2002; 46: 3026-33.
39. Martin WJ, Shaw O, Liu X, et al. 2011. MSU
crystal-recruited non-inflammatory monocytes differentiate into M1-like pro-inflammatory macrophages in a peritoneal murine model of gout. Arthritis Rheum 2011; 63: 1322-32.
40. Yagnik DR, Evans BJ, Florey O, et al. Macrophage release of transforming growth factor
beta1 during resolution of monosodium urate
monohydrate crystal-induced inflammation.
Arthritis Rheum 2004; 50: 2273-80.
41. Liote F, Prudhommeaux F, Schiltz C, et al.
1996. Inhibition and prevention of monosodium urate monohydrate crystal-induced acute
inflammation in vivo by transforming growth
factor beta1. Arthritis Rheum 1996; 39: 1192-8.
42. Rose DM, Sydlaske AD, Agha-Babakhani A,
et al. 2006. Transglutaminase 2 limits murine
peritoneal acute gout-like inflammation by
regulating macrophage clearance of apoptotic neutrophils. Arthritis Rheum 2006; 54:
3363-71.
Reumatismo 4/2011
237
You might also like
- BS en 61331-3-2014Document32 pagesBS en 61331-3-2014Ebi Rahmani100% (1)
- Microsurgery BookDocument335 pagesMicrosurgery BookProforVictor100% (2)
- At The Crossroads of Gout and Psoriatic Arthritis: "Psout"Document9 pagesAt The Crossroads of Gout and Psoriatic Arthritis: "Psout"ireneardianiNo ratings yet
- The Performance Wellness SeminarDocument8 pagesThe Performance Wellness SeminarMirelaAlexandraNo ratings yet
- Best Aid To OphthalmologyDocument501 pagesBest Aid To OphthalmologyMilthon Catacora Contreras67% (3)
- Clinical ReflectionDocument3 pagesClinical ReflectionNaomi MasudaNo ratings yet
- Research PaperDocument28 pagesResearch PaperhlwNo ratings yet
- Mechanism of Action of ColchicineDocument15 pagesMechanism of Action of ColchicineCatalina BanuNo ratings yet
- In Ammation and Atherosclerosis: Signaling Pathways and Therapeutic InterventionDocument24 pagesIn Ammation and Atherosclerosis: Signaling Pathways and Therapeutic InterventionZahroNo ratings yet
- 1 s2.0 S1063458422008536 MainDocument8 pages1 s2.0 S1063458422008536 Mainabo_youssof20047438No ratings yet
- 99 Jawien AOP61Document14 pages99 Jawien AOP61AsnikNo ratings yet
- ARS 2013 5198 Cordero - 1PDocument13 pagesARS 2013 5198 Cordero - 1PcynthiahpNo ratings yet
- Ministry of Education and Scientific Research) ) Al-Muthanna University College of Medicine) )Document10 pagesMinistry of Education and Scientific Research) ) Al-Muthanna University College of Medicine) )Hussein H. MahmoodNo ratings yet
- CC 12031Document200 pagesCC 12031Arti Tyagita KusumawardhaniNo ratings yet
- Systemic Disorders Associated With Peripheral Corneal UlcerationDocument4 pagesSystemic Disorders Associated With Peripheral Corneal UlcerationYoga KharismaNo ratings yet
- 2019 - Update Treatment CPPDDocument12 pages2019 - Update Treatment CPPDYENNo ratings yet
- Izab 277Document10 pagesIzab 277MartinaNo ratings yet
- Neutrophils Induce Paracrine Telomere Dysfunction and Senescence in ROS-dependent MannerDocument19 pagesNeutrophils Induce Paracrine Telomere Dysfunction and Senescence in ROS-dependent MannerValen EstevezNo ratings yet
- Association de Granulomatose Eosinophilique Avec Polyangeiteavec Rectocolite Hemorragique: A Propos Dun CasDocument5 pagesAssociation de Granulomatose Eosinophilique Avec Polyangeiteavec Rectocolite Hemorragique: A Propos Dun CasIJAR JOURNALNo ratings yet
- What's New in ShockDocument3 pagesWhat's New in ShockSteph FergusonNo ratings yet
- Gout 2Document15 pagesGout 2Huynh Dao Mai AnhNo ratings yet
- P Primary Open-Angle PatofisDocument2 pagesP Primary Open-Angle Patofisleonblizzara696No ratings yet
- The Potential of Adiponectin in Driving ArthritisDocument11 pagesThe Potential of Adiponectin in Driving ArthritisdionysiaNo ratings yet
- Artificially Cultivated Ophiocordyceps Sinensis AlleviatesDocument17 pagesArtificially Cultivated Ophiocordyceps Sinensis AlleviatesHoang IceNo ratings yet
- Rosenthal 2016Document10 pagesRosenthal 2016RONALD. D VIERA .MNo ratings yet
- Old and New Therapeutic Strategies in Systemic SclerosisDocument6 pagesOld and New Therapeutic Strategies in Systemic SclerosisJosé Javier Morales NúñezNo ratings yet
- Atherosclerosis en DiabetesDocument11 pagesAtherosclerosis en DiabetesAlexis Jesus GomezNo ratings yet
- Acute DistressDocument15 pagesAcute Distresspablopg_5No ratings yet
- Intermittent Hypoxia-Activated Cyclooxygenase Pathway: Role in AtherosclerosisDocument10 pagesIntermittent Hypoxia-Activated Cyclooxygenase Pathway: Role in AtherosclerosisaditNo ratings yet
- 5-Aminolevulinic Acid-Mediated Sonodynamic Therapy Inhibits RIPK1/RIPK3-Dependent Necroptosis in THP-1-Derived Foam CellsDocument13 pages5-Aminolevulinic Acid-Mediated Sonodynamic Therapy Inhibits RIPK1/RIPK3-Dependent Necroptosis in THP-1-Derived Foam Cellsdevi eraNo ratings yet
- BioFactors - 2023 - Lopes - Erythrocytes Surface Properties and Stiffness Predict Survival and Functional Decline in ALSDocument14 pagesBioFactors - 2023 - Lopes - Erythrocytes Surface Properties and Stiffness Predict Survival and Functional Decline in ALSAna Catarina De Oliveira Da Silv LaborinhoNo ratings yet
- Luteolin Decreases Atherosclerosis in LDL Receptor Deficient Mice Via A Mechanism Including Decreasing AMPK SIRT1 Signaling in MacrophagesDocument7 pagesLuteolin Decreases Atherosclerosis in LDL Receptor Deficient Mice Via A Mechanism Including Decreasing AMPK SIRT1 Signaling in Macrophagesأياد المشهدانيNo ratings yet
- Biomedicines: Relapsing Polychondritis: An Updated ReviewDocument14 pagesBiomedicines: Relapsing Polychondritis: An Updated ReviewThane ManoonNo ratings yet
- Research Article: TNF-Alpha Levels in Tears: A Novel Biomarker To Assess The Degree of Diabetic RetinopathyDocument7 pagesResearch Article: TNF-Alpha Levels in Tears: A Novel Biomarker To Assess The Degree of Diabetic RetinopathytiaraleshaNo ratings yet
- Reactive Oxygen and Nitrogen Species in Sepsis-Induced Hepatic Microvascular DysfunctionDocument10 pagesReactive Oxygen and Nitrogen Species in Sepsis-Induced Hepatic Microvascular DysfunctionGiosué Reyes HernandezNo ratings yet
- Kidney Research and Clinical Practice: Jürgen FloegeDocument8 pagesKidney Research and Clinical Practice: Jürgen FloegeAnita PrastiwiNo ratings yet
- Research Progress in Prevention and Cure of Fibrosis by Traditional Chinese MedicineDocument6 pagesResearch Progress in Prevention and Cure of Fibrosis by Traditional Chinese MedicineAmanda BrennanNo ratings yet
- Pathophysiology of Pulmonary Complications of Acute PancreatitisDocument10 pagesPathophysiology of Pulmonary Complications of Acute PancreatitisAmri AdhyatmaNo ratings yet
- The Role of Curcumin in Liver Diseases: HepatologyDocument13 pagesThe Role of Curcumin in Liver Diseases: HepatologyAbraham TheodoreNo ratings yet
- EndhotheliumDocument18 pagesEndhotheliumDzikrul Haq KarimullahNo ratings yet
- Science Abe4832 FullDocument20 pagesScience Abe4832 FullsussanNo ratings yet
- Pulmonary Hypertension: Advances in Pathogenesis and TreatmentDocument12 pagesPulmonary Hypertension: Advances in Pathogenesis and Treatmentbdalcin5512No ratings yet
- Moura 2017Document15 pagesMoura 2017SANTIAGO URIBE GOMEZNo ratings yet
- Leptin As An Open Secret in The Physiopathology of Rheumatic DiseasesDocument3 pagesLeptin As An Open Secret in The Physiopathology of Rheumatic DiseasesEduardoNo ratings yet
- El Glucocalix en La SepsisDocument8 pagesEl Glucocalix en La SepsisAndrea GaytánNo ratings yet
- HHS Public Access: Highlighting Diabetes - The Epidemic ContinuesDocument14 pagesHHS Public Access: Highlighting Diabetes - The Epidemic ContinuesRidhaNo ratings yet
- 2028 Full PDFDocument8 pages2028 Full PDFdhineyNo ratings yet
- Julia Nur Faridha SDocument9 pagesJulia Nur Faridha SJulia Nur Faridha SeptyaniNo ratings yet
- 1 s2.0 S0954611120302389 MainDocument6 pages1 s2.0 S0954611120302389 Mainlidi booksNo ratings yet
- Molecular Pathways of Chronic Kidney Disease Progression: SciencedirectDocument4 pagesMolecular Pathways of Chronic Kidney Disease Progression: SciencedirectJosué VelázquezNo ratings yet
- Obesity and Osteoarthritis: More Complex Than Predicted!Document3 pagesObesity and Osteoarthritis: More Complex Than Predicted!Linda FatrisiaNo ratings yet
- Insight Into Glomerular Filtration and Albuminuria - NEJMDocument10 pagesInsight Into Glomerular Filtration and Albuminuria - NEJMasalizwa ludlalaNo ratings yet
- Benzing-2021-Insights Into Glomerular FiltrationDocument10 pagesBenzing-2021-Insights Into Glomerular FiltrationNguyen LequyenNo ratings yet
- Possible Mechanisms of Disease Development in Tuberous SclerosisDocument7 pagesPossible Mechanisms of Disease Development in Tuberous Sclerosisplastioid4079No ratings yet
- "Ample": Advance Trauma and Live Support 9 EditionDocument3 pages"Ample": Advance Trauma and Live Support 9 EditionYoga PribadiNo ratings yet
- End-Stage Renal Disease With Erythrocytosis: A Case Report On A Rare Association of Crescentic Glomerulonephritis and JAK2-Positive Polycythemia VeraDocument6 pagesEnd-Stage Renal Disease With Erythrocytosis: A Case Report On A Rare Association of Crescentic Glomerulonephritis and JAK2-Positive Polycythemia VeraPolito SoytiNo ratings yet
- Bollenbecker Et Al 2022 Lung Kidney Interactions and Their Role in Chronic Kidney Disease Associated Pulmonary DiseasesDocument16 pagesBollenbecker Et Al 2022 Lung Kidney Interactions and Their Role in Chronic Kidney Disease Associated Pulmonary DiseaseshilyalivaNo ratings yet
- Pparγ Gene and AtherosclerosisDocument9 pagesPparγ Gene and AtherosclerosisisaNo ratings yet
- Toxicology and Applied Pharmacology: Séin O'Connell, Craig Slattery, Michael P. Ryan, Tara McmorrowDocument10 pagesToxicology and Applied Pharmacology: Séin O'Connell, Craig Slattery, Michael P. Ryan, Tara McmorrowDoyin AwodeleNo ratings yet
- Ce Lu Last Ronco SaraDocument15 pagesCe Lu Last Ronco SaraEduardo SoaresNo ratings yet
- Guarana Et Al 2022 PDFDocument10 pagesGuarana Et Al 2022 PDFAndersonFelixNo ratings yet
- The Inflammatory ProcessDocument7 pagesThe Inflammatory ProcessDaniul ConuiNo ratings yet
- Rheumatology Cutolo RheumatologyDocument8 pagesRheumatology Cutolo RheumatologyAlina BanicaNo ratings yet
- Manuscript 232Document9 pagesManuscript 232Shelin AmandaNo ratings yet
- Cancer Fighting StrategiesDocument6 pagesCancer Fighting StrategiesDahneel RehfahelNo ratings yet
- Perioperative Management of AdrenalectomyDocument13 pagesPerioperative Management of AdrenalectomyTJ LapuzNo ratings yet
- Incision and Drainage of AbscessesDocument25 pagesIncision and Drainage of Abscessesjaphetnwapi100% (1)
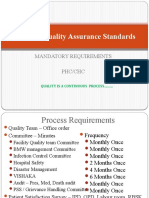
- National Quality Assurance Standards: Mandatory Requirements PHC/CHCDocument14 pagesNational Quality Assurance Standards: Mandatory Requirements PHC/CHCSathish KumaarNo ratings yet
- Clinical Guideline For Management of Gallstones Pathology in AdultsDocument11 pagesClinical Guideline For Management of Gallstones Pathology in AdultsrintyosoNo ratings yet
- Cataract SurgeryDocument2 pagesCataract SurgeryndrabramsNo ratings yet
- PostpartumDocument3 pagesPostpartumMuhammad RifaiNo ratings yet
- The History of Immunology and VaccinesDocument32 pagesThe History of Immunology and VaccinesClement del RosarioNo ratings yet
- Roles and Responsibilities of ASHADocument3 pagesRoles and Responsibilities of ASHAmohanpskohli8310No ratings yet
- Hirayama Disease and HomoeopathyDocument11 pagesHirayama Disease and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (3)
- What Are Thrombosed External Hemorrhoids?Document3 pagesWhat Are Thrombosed External Hemorrhoids?Hanine HassanNo ratings yet
- Quiz 5 - PSY1001 Introductory PsychologyDocument6 pagesQuiz 5 - PSY1001 Introductory Psychologymrsdenison0% (1)
- Indian Chilhood CirrhosisDocument28 pagesIndian Chilhood CirrhosisBelbi MolNo ratings yet
- Mommy's MedicineDocument3 pagesMommy's Medicinekcs.crimsonfoxNo ratings yet
- MSDS Berkat Saintifindo PDFDocument27 pagesMSDS Berkat Saintifindo PDFDianSelviaNo ratings yet
- Bone, Joint and Muscle Injuries: Freida Michelle Bonnit-Taja, RN, ManDocument45 pagesBone, Joint and Muscle Injuries: Freida Michelle Bonnit-Taja, RN, ManFreida Michelle BonnitNo ratings yet
- HIV and PregnancyDocument9 pagesHIV and PregnancyUm HamoOdNo ratings yet
- LHPCDocument23 pagesLHPCChristine AzmiNo ratings yet
- MCQ Cat-1Document16 pagesMCQ Cat-1vijayalakshmiNo ratings yet
- 7051N3M126Q411U7Document69 pages7051N3M126Q411U7naldihasibuanNo ratings yet
- Maharashtra University of Health SciencesDocument6 pagesMaharashtra University of Health SciencesArun UdayakumarNo ratings yet
- By - Derina FixDocument1 pageBy - Derina FixSellyta HasugianNo ratings yet
- Importance and Applicability of Strotas in Treatment of DiseaseDocument9 pagesImportance and Applicability of Strotas in Treatment of DiseaseAshutosh JhaNo ratings yet
- Chapter 16 BLOODDocument2 pagesChapter 16 BLOODJennyNo ratings yet