Professional Documents
Culture Documents
URT 2012 Handout
Uploaded by
SaraHussienCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
URT 2012 Handout
Uploaded by
SaraHussienCopyright:
Available Formats
24/03/1436
Antimicrobial
Regimen
Selection
MIU, Infectious diseases, CDC
Prior to the discovery of penicillin
in 1927 by Sir Alexander Fleming;
Patients with infected wounds
often had to have a wounded limb
amputated.
Most patients faced death from
their infection.
Today, despite the presence of a
large number of antibiotic classes,
mortality due to infectious
diseases is increasing ????
Microbial resistance
Solution ????????
Appropriate antibiotic
regimen selection
Role of the clinical pharmacist
MIU, Infectious diseases, CDC
Terminologies
Infections are either
Exogenous.
i. Endogenous Infection:
Endogenous
or
Alteration of normal flora OR disruption of host
defense.
Do we have bacteria in our bodies? Colonizing Bacteria
ii. Exogenous Infections:
Infections acquired from an external source.
Colonization versus Infection.
Virulence versus Resistance.
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
24/03/1436
Skin
Staphylococcus
epidermidis/ aureus
Micrococci, Diphteroids.
Mouth
Oral anaerobes
Vridans streptococci
URT
Maroxella catarrhalis
Streptococcus pneumonia
Heamophilus influenza
LRT
Sterile
Other sterile anatomic
MIU,sites:
Infectious diseases, CDC
CSF, blood & urine.
Guiding Principles When
Prescribing Antimicrobials
Make Correct Diagnosis
Do No Harm
MIU, Infectious diseases, CDC
What is the Appropriate Decision
if a Culture is Required?
Infection suspected
Cultures taken
Empiric
Antibiotic started
Definitive
Culture results reviewed
Antibiotic revised if necessary
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
24/03/1436
Empiric
vs.
Infection not well defined
Definitive
Infection well defined
Narrow spectrum
One, seldom two drugs
Less adverse reactions
Less expensive
(best guess)
Broad spectrum
Multiple drugs
More adverse reactions
More expensive
Definitive Therapy (15%)
Empiric Therapy (85%)
MIU, Infectious diseases, CDC
Infections Where Cultures are
Routinely Useful
Complicated urinary tract infections (urine)
Blood stream infections (Blood)
Bone and joint infections
Meningitis ( CSF)
Endocarditis (blood)
Lower respiratory tract infection (sputum, blood)
MIU, Infectious diseases, CDC
Infections Where Cultures Are NOT
Routinely Useful
Intra-abdominal abscess.
Uncomplicated lower urinary tract
infection.
Infected diabetic foot ulcers.
Sinusitis
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
24/03/1436
Justification for Antimicrobial
Combinations
To cover many bacteria for empiric therapy.
To achieve a synergistic antibacterial effect.
To prevent the emergence of resistance.
MIU, Infectious diseases, CDC
Concentration
Concentration-Dependent
Versus Time-Dependant Killing
Conc dep (Peak to MIC ratio
MIC
Time. Dep
(Time over MIC
ratio)
Time
MIU, Infectious diseases, CDC
Concentration dependant; Aminoglycosides, Flouroquinolones
Susceptibility testing
Once the pathogen is identified susceptibility testing can be performed.
The minimum inhibitory
concentration (MIC).
The lowest concentration that
inhibit visible bacterial growth
after 24 hrs
Break point.
The concentration of AB
achieved in the serum after
a standard dose
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
24/03/1436
Susceptibility testing
Once the pathogen is identified susceptibility testing can be performed.
The minimum inhibitory
concentration (MIC).
Break point.
Breakpoint and MIC values determine if the
organism is susceptible (S), intermediate
(I), or resistant (R) to an antimicrobial.
If MIC is below BP
If MIC is above BP
If MIC
BP diseases, CDC
MIU,=
Infectious
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
24/03/1436
Reasons for Antimicrobial Failure
Use for non-bacterial infections.
The wrong antibiotic was selected.
The patient has immune system defects.
The patient did not take the medication
properly compliance.
The antibiotic did not penetrate to the
site of infection.
Infectious
diseases, CDC
The bacteriaMIU,
was
resistant.
Resistance Problems from
Antibiotic Overuse
Gram-negative
cephalosporin.
Staphylococcus
(MRSA)
bacilli
aureus
from 3rd generation
from
Methicillin
Enterococcus from vancomycin use (VRE).
Streptococcus pneumoniae from penicillin.
MIU, Infectious diseases, CDC
Upper Respiratory Tract
Infections
Otitis media
Sinusitis
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
24/03/1436
The respiratory tract is the most common site for
infection by pathogens.
Most Upper respiratory tract infections
are viral & self limited
Otitis media, sinusitis and pharyingitis
Guidelines reduce AB use for viral URIs
Excess AB use for URTIs MIU,
Infectious diseases, CDC
bacterial resistance
Otitis media
Middle ear infection and inflammation
Most prevalent in young children
(0.5 5 years of age)
Most cases are viral &spontaneously resolve
Recurrence is common
OM
AOM
OME
Acute otitis media MIU, Infectious
Otitis
media with effusion
diseases, CDC
AOM:Infection & inflammation of the middle ear
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
24/03/1436
Otitis Media
AOM
OME
Acute Otitis Media
Otitis Media with Effusion
Rapid onset of signs & The presence of middle ear
fluids without symptoms of
symptomatic
acute illness
Presence of effusion.
the TM is typically retracted
Inflammation (indicated
or in the neutral position
by erythema or otalgia)
Tympanocentesis
TM is usually bulging
or
Tympanostomy tube insertion
ABs are useful
Effusions can be present up to 6 months
after acute episode of AOM.
MIU, Infectious diseases, CDC
Etiology
Common bacteria ( + virus)
Streptococcus pneumoniae
30-60% have reduced penicillin
susceptibility (PRSP)
Multi-drug resistance [ amoxicillin
and erythromycin, Clindamycin and
Floroquinolones. ]
Haemophilus influenzae (1-5 yr old)
up to 50% are b-lactamase positive
Moraxella catarrhalis
almost 100% b-lactamase positive
MIU, Infectious diseases, CDC
Why are children more susceptible to
AOM than adults ?
Their eustachian tubes are
shorter, more flaccid, and
more horizontal than adults.
Their immune system is still
developing
Their adenoids are larger
than adults, interfering with
the eustachian tube opening
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
24/03/1436
Risk factors
1. Day care attendance
2. Family history of AOM
3. Supine positioning during feeding allows
reflux to eutachian tube
4. Lower socioeconomic status
5. Smokers in the household
6. Craniofacial abnormality/ cleft palate
MIU, Infectious diseases, CDC
Clinical Presentation
symptoms
Young children:
- ear tugging
- irritable sleeping
- poor eating habits
Older patients
- ear pain
- ear fullness
- impaired hearing
MIU, Infectious diseases, CDC
Clinical Presentation and Diagnosis of
AOM
1. Middle ear effusion
Bulging membrane
Limited or absent mobility
Purulence
Opaque or cloudy, obscuring
visibility of middle ear
Severe: Otorrhea (middle ear
perforation with fluid
drainage
Pneumatic Otoscope
And
2. Signs of inflammation
Fever (< 25% of children)
Distinct erythema
otalgia
MIU, Infectious diseases, CDC
Normal tympanic membrane
AOM
MIU, Infectious diseases, CDC
24/03/1436
Diagnosis
How can you tell that AOM is severe
Severe AOM:
- Moderate to severe ear pain otalgia
- Otalgia > 48 hrs
- Fever 39C
Nonsevere AOM:
- Mild ear pain
- Fever < 39C
MIU, Infectious diseases, CDC
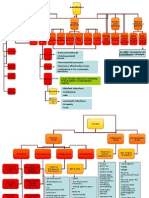
Confirmed AOM
( effusion and inflammation)
Approaches
Delayed AB
Immediate AB
Observationwatchful waiting
AOM with nonsevere symptoms
AOM with severe symptoms
- Bulging TM
According to age:
- Perforation
- 2 yrs: delayed AB
- Otorrhea
Children < 6 months,
- 6 months- 2 years, with
Children > 6 months,
unilateral AOM, or mild
with no reliable follow up
symptoms; delayed AB
6 months- 2 years, with
MIU, Infectious diseases,bilateral
CDC
AOM;
Non-pharmacological therapy
Watchful waiting and observation involves
monitoring for 48 to 72 hours after diagnosing
AOM to :
attenuate microbial resistance
to see if spontaneous resolution will occur
avoid unnecessary adverse events and costs of AB
External heat or cold to reduce postauricular pain
Analgesics are recommended in the first days
Corticosteroids, antihistamines and decongestants
are not recommended
MIU, Infectious diseases, CDC
10
MIU, Infectious diseases, CDC
24/03/1436
AOM Adjunctive Treatment
Otalgia/pain relief
Analgesics
Acetamenophen (paracetamol)
Ibuprofen ( longer action, but not < 6 months)
Topical anesthetics
Benzocaine drops (relief in 30 min)
Preferred over systemic analgesics
The decongestants, antihistamines and
corticosteroids have no beneficial role
MIU, Infectious diseases, CDC
Age < 6 months
Age > 2 yrs
MIU, Infectious diseases, CDC
Mild symptoms
MIU, Infectious diseases, CDC
11
MIU, Infectious diseases, CDC
24/03/1436
Ig E -mediated
Amox taken within
30 days
MIU, Infectious diseases, CDC
FIGURE 692. Treatment algorithm for uncomplicated AOM in children 2 months to 12 years of age.
Otitis media Treatment
Failure after 3 days of therapy
Lack of clinical improvement after 3 days
of therapy in :
signs and symptoms of ear infection
ear pain
fever
tympanic membrane findings: redness, bulging,
otorrhea
MIU, Infectious diseases, CDC
Clindamycin+/- 3rd gen. cephaosporin
0r Tymanocentesis
Tympanostomy
tubes
MIU,
Infectious diseases,
CDCfor persistent OME
12
MIU, Infectious diseases, CDC
24/03/1436
Failure after 3 days of therapy
MIU, Infectious diseases, CDC
MIU, Infectious diseases, CDC
AOM Treatment
Avoid in children under 2 months:
Ceftriaxone
Erythromycin-sulfisoxazole
Trimethoprim- sulfamethoxazole
bilirubin displacement risk kernicterus
MIU, Infectious diseases, CDC
13
MIU, Infectious diseases, CDC
24/03/1436
AOM Treatment
Duration of therapy: according to age &
severity;
< 2yrs or severe/ recurrent symptoms; 10-day
[recurrent infections, is defined as 3 isolated episodes of otitis media in 6 month,
with resolution of each episode or 4 or more episodes of AOM in a 12-month
period that includes at least 1 episode in the preceding 6 months]
2-5 yrs, mild-moderate symptoms: 7 days
> 6 yrs mild-moderate symptoms 5 -7 days
[Exceptions: azithromycin(3-5d ) and
ceftriaxone
(3 d)]
MIU, Infectious diseases, CDC
AOM Prevention
Vaccination
Pneumococcal vaccine (Pneumovax)
Influenza vaccine Haemophilus
influenzae type B vaccine (children 2
years old)
Minimize risk factors
Tobacco smoke
Bottle feeding
Antibiotic prophylaxis is no longer recommended
for otitis-prone children
because of increasing
MIU, Infectious diseases, CDC
resistance
Patient Cases
A 5-month-old infant who was born at term and is
otherwise healthy was treated for her first case of otitis
media with amoxicillin 45 mg/kg/day for 7 days. On
follow-up examination, her pediatrician noticed fullness
in the middle ear and a cloudy tympanic membrane
with decreased mobility. She is now afebrile and eating
well. Which is the best recommendation regarding her
treatment?
A. No antibiotics warranted at this time.
B. High-dose (90 mg/kg/day) amoxicillin for 7 days.
C. Decongestant and antihistamine daily until
resolution.
D. Azithromycin. MIU, Infectious diseases, CDC
14
MIU, Infectious diseases, CDC
24/03/1436
A 4-year-old boy receives a diagnosis of his
fourth case of otitis media within 12
months. He has not shown evidence of
hearing loss or delay in language skills.
Which is the best intervention at this point?
A. Giving long-term antibiotic prophylaxis.
B. Inserting tympanostomy tubes.
C. Administering high-dose amoxicillin and
ensuring that he is up-to-date on his
pneumococcal and influenza vaccines.
Infectious diseases, CDC
D. No antibioticMIU,
therapy
warranted
A 3years-old boy presents to clinic with his
mother for a chief complaint of tugging of right
ear. His mother explained that he attends day
care and has been suffering from frequent
episodes of difficulty in sleeping associated with
excessive crying and a severe fever (39.2 ). After
consulting her pediatrician, he inspected the
child's ears and noticed that both tympanic
membranes are mobile, not bulging, but
erythematous. The child has no penicillin allergy.
What are the risk factors in this case for bacterial OM?
What is your suggested diagnosis for the presented case,
indicating criteria for AOM and severity?
Select the most appropriate treatment approach in this case.
MIU, Infectious diseases, CDC
Outcome evaluation
Assess improvement of Signs and symptoms
within 72 hrs of therapy.
Children may not improve during the first 24 hrs,
but stabilize afterwards
Presence of middle ear effusion with no symptoms
may sustain for 3 months, reevaluation is a must
Assess hearing and speech abilities
MIU, Infectious diseases, CDC
15
MIU, Infectious diseases, CDC
24/03/1436
Sinusitis
Infection or inflammation of the paranasal sinuses and
mucosal linings of the nasal passages for up to 4 weeks
Rhinosinusitis
Affects about 1 billion of people annually
Acute sinusitis: lasting < 4 weeks, resolves completely
Subacute: 4-12 weeks
Chronic: > 12 weeks
Recurrent acute: > 4 episodes per year
Occurrence related to viral URTI ( rhinovirus, influenza
virus), nasal allergies, non-allergic rhinitis, environmental
MIU, Infectious diseases, CDC
irritant
MIU, Infectious diseases, CDC
Sinusitis Common bacteria
Streptococcus pneumoniae
50-60%
Haemophilus influenzae
Moraxella catarrhalis
20%
Anaerobes
0-10%
Bacteroides
Peptostreptococcus spp.
Streptococcus pyogenes
Staphylococcus aureus
5%
5%
Chronic infections are commonly polymicrobial
90 % are viral, < 10 % bacterial
MIU, Infectious diseases, CDC
16
MIU, Infectious diseases, CDC
24/03/1436
Pathophysiology
Rhinosinusitis is
caused by mucosal
inflammation and
local damage to
mucociliary clearance
mechanisms as a result
of viral infection or
allergy
MIU, Infectious diseases, CDC
Acute Bacterial Rhinosinusitis (ABRS)
MIU, Infectious diseases, CDC
Diagnosis
At least 2 major symptoms or
1 major + >2 minor symptoms
MIU, Infectious diseases, CDC
17
MIU, Infectious diseases, CDC
24/03/1436
Diagnosis of ABRS
Clinical diagnosis of ABRS:
a viral URI that has not resolved after 10 days, worsens after 5 to 7
days with signs and symptoms of acute infection
Radiography: for abscess or intracranial complication
Paranasal sinus puncture: Gold Standard
not routinely performed but may be useful for complicated/chronic
cases
Lab /culture: not recommended
for routine
diagnosis
MIU, Infectious diseases,
CDC
How to differentiate between
viral and bacterial sinusitis
MIU, Infectious diseases, CDC
Clinical Presentation and Diagnosis
Complications
Periorbital cellulitis
Meningitis
MIU, Infectious diseases, CDC
18
MIU, Infectious diseases, CDC
24/03/1436
General approach to Treatment
Initial management of rhinosinusitis is
watchful waiting that focuses on symptom
relief for patients with uncomplicated mild
disease lasting less than 10 days.( mild pain,
Temp< 38.3
Routine antibiotic use is not recommended
for all patients because viral sinusitis is selflimiting and bacterial infection resolves
spontaneously in many cases.
MIU, Infectious diseases, CDC
Who should receive an Antibiotic?
Antibiotic therapy should be reserved for
persistent, worsening, or severe ABRS:
Patients with severe disease regardless of duration.
(e.g., evidence of systemic toxicity with a temp of 39C or higher and
a threat of suppurative complications)
Patients with mild to moderately severe
symptoms based on clinical judgment that have
persisted for greater than 10 days or worsened after
5 -7 days
Empirical selection is often employed and should
MIU, Infectious diseases, CDC
target likely pathogens
Treatment algorithm for ABRS in children
10-14 days
Amox-Clav
45 mg/Kg/d
bid
Amox-Clav
90 mg/Kg/d
bid
Clinda+(cifixime
or Cefopodoxime)
Or Levo
Clinda+ (cifixime
or Cefopodoxime)
Or Levo (type 1)
MIU, Infectious diseases, CDC
B-lactam allergy
19
MIU, Infectious diseases, CDC
24/03/1436
Treatment algorithm for ABRS in Adults
5-7 days
+ Severe infection
Amox-Clav
2 g bid
Or Doxy 100
bid or 200 qd
Amox-Clav
500 mg Tid
Or 875 mg bid
Levo 500 mg qd
Or Moxi 400 mg qd
Amox-Clav,2g bid
Levo 500 mg qd
Or Moxi 400 mg qd
MIU, Infectious diseases, CDC
B-lactam allergy
Antimicrobial regimen for ABRS in adults
Doxy 100 bid or 200 qd
Levo 500 mg qd
Or Moxi 400 mg qd
5-7 days
MIU, Infectious diseases, CDC
Nonpharmacologic Therapy
Intranasal saline irrigations
moisturize the nasal canal and impair crusting of
secretions along and promote ciliary function
Humidifiers
vaporizers
saline nasal sprays or drops
MIU, Infectious diseases, CDC
20
MIU, Infectious diseases, CDC
24/03/1436
Adjunctive (supportive) Therapy
Analgesics and antipyretics: fever and pain of sinus
pressure
( acetaminophen and NSAID)
Decongestant lack evidence for effectiveness
For allergic patients only
Antihistamines should be avoided as they thicken
mucus and impair its clearance but they may be useful
in patients with predisposing allergic rhinitis or chronic
sinusitis
Intranasal corticosteroid are for allergic patients and
those with chronic sinusitis
MIU, Infectious diseases, CDC
Outcome evaluation
Clinical improvement should be evident by 7 days of therapy
demonstrated by reduction in nasal congestion and discharge,
and improvements in facial pain or pressure and other
symptoms.
Patients should be monitored for common adverse events.
Referral is also important for:
Recurrent / chronic sinusitis
Failure with first- or second-line therapy
Acute disease in immunocompromised patients.
MIU, Infectious diseases, CDC
A 5 years old boy presents to the clinic with
mild nasal congestion, sinus pain and
pressure that have begun 4 days ago for the
first time. He is coming to you to fill a
prescription of
Rx: Amoxicillin , Loratadin
Do you agree on dispensing this prescription?
If 7 days have passes and the patient did not
improve, will the prescription be appropriate?
MIU, Infectious diseases, CDC
21
MIU, Infectious diseases, CDC
24/03/1436
A 15 yrs-old man presents with mild S&S of
definite ABRS for the first time that have lasted
for more than 7 days with no obvious
improvement. He comes to your pharmacy to fill
the following prescription and declares having
experienced severe urticaria from penicillin and
denies having received an antibiotic in the
previous period.
What are your recommendations in this case? Indicate a
first line and second line therapy. ( He is given Sulfa/
Trimeth) or a macrolide
What are classes of drugs that are not recommended in this
case (Telithromycin and Floroqinolones, Clindamycin and
probably Doxycycline).
What is the duration of therapy? 10 to 14 days.
MIU, Infectious diseases, CDC
22
MIU, Infectious diseases, CDC
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- 41 How To Cure DiseaseDocument60 pages41 How To Cure DiseaseEdie M Murgia0% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- SCHWARTZ Surgical InfectionDocument25 pagesSCHWARTZ Surgical InfectionAlexandra Niken Larasati78% (9)
- Introduction to Sulphonamides: History, Mechanism of Action, and UsesDocument49 pagesIntroduction to Sulphonamides: History, Mechanism of Action, and UsesGunjan Yadav100% (5)
- AntibioticsDocument6 pagesAntibioticsyezan27100% (8)
- Albuterol Drug StudyDocument7 pagesAlbuterol Drug StudyMaria Charlene OrpillaNo ratings yet
- PPC14 Infectious DiseasesDocument48 pagesPPC14 Infectious DiseasesSaraHussienNo ratings yet
- Nutrition Board MIU 14-3-2015Document41 pagesNutrition Board MIU 14-3-2015SaraHussienNo ratings yet
- Last Antibiotic Classes For CDC (Mona + Yasmine)Document7 pagesLast Antibiotic Classes For CDC (Mona + Yasmine)SaraHussienNo ratings yet
- Pediatrics 2013 Lieberthal Peds.Document40 pagesPediatrics 2013 Lieberthal Peds.SaraHussienNo ratings yet
- Clin Infect Dis. 2012 Chow Cid Cir1043Document41 pagesClin Infect Dis. 2012 Chow Cid Cir1043SaraHussienNo ratings yet
- Acid Base Discorders MIU BCPS 2015Document95 pagesAcid Base Discorders MIU BCPS 2015SaraHussienNo ratings yet
- Aki Miu BCPS 2015Document52 pagesAki Miu BCPS 2015SaraHussienNo ratings yet
- AOM, Sinusitis Guidelines ChartsDocument5 pagesAOM, Sinusitis Guidelines ChartsSaraHussienNo ratings yet
- Acid Base Discorders MIU BCPS 2015Document95 pagesAcid Base Discorders MIU BCPS 2015SaraHussienNo ratings yet
- Aki Miu BCPS 2015Document52 pagesAki Miu BCPS 2015SaraHussienNo ratings yet
- Renal Anatomy & Physiology MIU BCPS 2015Document61 pagesRenal Anatomy & Physiology MIU BCPS 2015SaraHussienNo ratings yet
- CDC - Clostridium Difficile InfectionDocument1 pageCDC - Clostridium Difficile InfectionSaraHussienNo ratings yet
- CDC STD Yasmin CDC FinalDocument15 pagesCDC STD Yasmin CDC FinalSaraHussienNo ratings yet
- UTIsDocument25 pagesUTIsSaraHussienNo ratings yet
- OsteomyelitisDocument23 pagesOsteomyelitisSaraHussienNo ratings yet
- Viral Hepatitis MIU BCPS 2015Document67 pagesViral Hepatitis MIU BCPS 2015SaraHussienNo ratings yet
- Careplan Week2Document2 pagesCareplan Week2api-302138606No ratings yet
- Activity in Kirby Bauer MethodDocument2 pagesActivity in Kirby Bauer MethodMaui Vecinal de GuzmanNo ratings yet
- Shahid 2009Document15 pagesShahid 2009Priyankan MajumderNo ratings yet
- Opportunity, Challenge and Scope of Natural Products in Medicinal ChemistryDocument434 pagesOpportunity, Challenge and Scope of Natural Products in Medicinal ChemistryCamilla Karen Fernandes Carneiro100% (1)
- Reading Guide V 4.0 EUCAST Disk TestDocument24 pagesReading Guide V 4.0 EUCAST Disk TestmotibaNo ratings yet
- Phytochemical Screening and Antibacterial Activities of Vernonia Ambigua, Vernonia Blumeoides and Vernonia Oocephala (Asteraceae)Document7 pagesPhytochemical Screening and Antibacterial Activities of Vernonia Ambigua, Vernonia Blumeoides and Vernonia Oocephala (Asteraceae)linubinoiNo ratings yet
- In This Issue: Wound Infection and ColonisationDocument7 pagesIn This Issue: Wound Infection and ColonisationSeftiana WahyuniNo ratings yet
- DunnoDocument5 pagesDunnoLunariaNo ratings yet
- Spain, Towards A Pig Factory Farm Nation?Document6 pagesSpain, Towards A Pig Factory Farm Nation?Food and Water WatchNo ratings yet
- Redefining Susceptibility Testing Categories S, I and R.: Gunnar Kahlmeter and The EUCAST Steering CommitteeDocument54 pagesRedefining Susceptibility Testing Categories S, I and R.: Gunnar Kahlmeter and The EUCAST Steering CommitteeRuth RachitaNo ratings yet
- Warfarin INR Antibx InteractionDocument3 pagesWarfarin INR Antibx InteractionSheila UlinaNo ratings yet
- Guia de Interpretacion Resultados MicrobiologicosDocument19 pagesGuia de Interpretacion Resultados MicrobiologicosJuhaydith Hernandez AzuajeNo ratings yet
- Farmakologi Antibiotik: Guinanti Novettiandari Kepan Iteraan Klinik Senior Interna Rsud CiamisDocument80 pagesFarmakologi Antibiotik: Guinanti Novettiandari Kepan Iteraan Klinik Senior Interna Rsud CiamisguiguinantiNo ratings yet
- Id Resident TDDocument2 pagesId Resident TDapi-534214500No ratings yet
- Cross-Reactivity To MeropenemDocument3 pagesCross-Reactivity To Meropenemthao hoangNo ratings yet
- Update Stok PT KMD 28Document41 pagesUpdate Stok PT KMD 28Olan ArsNo ratings yet
- Rifaximin For The Treatment of TDDocument11 pagesRifaximin For The Treatment of TDAnkur AgrawalNo ratings yet
- Antibacterial Antibiotic AgentsDocument13 pagesAntibacterial Antibiotic AgentsEmmanuel coleteNo ratings yet
- Nama Prinsipal Kode Produk Nama Produk Unit Stok HnappnDocument4 pagesNama Prinsipal Kode Produk Nama Produk Unit Stok HnappnNoperitaNo ratings yet
- Daftar Atc DDD Antibiotik Who 2018Document14 pagesDaftar Atc DDD Antibiotik Who 2018tri tanayawatiNo ratings yet
- Detection of Methicillin Resistance in Staphylococcus Species From Clinical SamplesDocument6 pagesDetection of Methicillin Resistance in Staphylococcus Species From Clinical SamplesOpenaccess Research paperNo ratings yet
- Amoxicillin + Clavulanic AcidDocument37 pagesAmoxicillin + Clavulanic Acidsanish tiwariNo ratings yet
- Evolution of MedicineDocument6 pagesEvolution of MedicineAssignmentLab.comNo ratings yet
- Cell Wall Synthesis - BacterialProteinSynthesis - AntimicrobialsDocument99 pagesCell Wall Synthesis - BacterialProteinSynthesis - AntimicrobialsJoslin Roz GalileaNo ratings yet
- Herbal PlantsDocument50 pagesHerbal PlantsrozendavidNo ratings yet