Professional Documents
Culture Documents
Use of Blood Components
Uploaded by
Ian FordeCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Use of Blood Components
Uploaded by
Ian FordeCopyright:
Available Formats
Use of blood components
December 2009
Contents:
Short name
Detailed name
1. Short name
Use of blood components
2. Detailed name
Blood components transfused per patient.
3. Short
definition
Number of blood components transfused per
patient during selected tracer procedures in the
hospital.
Short definition
Rationale
Operational definition
Previous PATH experience
Data source
Domain
Type of indicator
Adjustment/ stratification
Sub-indicators
Related indicators
Interpretation
Guidelines
References
4. Rationale
(including
justification,
strengths and
limits)
Rationale:
- Blood transfusions are common in surgical
patients (1). However, attitudes toward blood
transfusion have changed in the last decade.
Although transfusion can be lifesaving, recent
evidence suggests that their use is associated
with increased morbidity and mortality and
therefore, current transfusion practices may
require re-evaluation (2,3).
- Despite evidence supporting more restrictive use
of blood, the use of transfusions among surgical
patients has increased during the last decade (4).
- Patients are concerned about the safety of blood
transfusion and payers about the costs of blood
transfusion. There is still insufficient information
on the clinical use of blood in elective surgery
and there are large recorded variations in
transfusion practices. Studies have demonstrated
high variability in red blood cell (RBC)
transfusions and blood loss in standard surgical
procedures (5-7).
- Demand for blood products is growing and it
often exceeds the resources of the local blood
bank, thereby disrupting both the planning and
the nature of surgical protocols. Therefore, it is
necessary to streamline blood ordering and
transfusion practice.
- A number of studies showed over-ordering of
blood
components
by
surgeons
or
by
anesthesiologists.
PAGE 2
USE OF BLOOD COMPONENTS
1.
Over-ordering of blood has to be minimised: Demanding large quanti
of blood each day, of which little is ultimately used commits valua
supplies and resources both in technician time and reagents.
The ready availability of blood components often results in liberal use
blood. In adults, blood loss of up to 20% (about one liter for an avera
person with 70 kg of body weight) is well tolerated in the majority
patients, provided that the circulatory volume is compensated w
colloids or crystalloids). Transfusion of red cell concentrates
recommended only if there is >30% blood loss (8, 9).
Blood transfusion carries a number of well-recognized risks a
complications and blood products have become more expens
because of their specific preparation procedures. Surgical techniq
awareness of the problem and restriction of transfusion trigger h
become an important factor affecting the transfusion therapy and blo
loss management.
The transfusion trigger has shifted from the optimal Hb level of 10 g
which has been considered as a gold standard for a long time. Curr
evidence indicates that for most patients more restrictive transfusion
more effective (10).
An expert consensus conference convened by United States Food a
Drug Administration concluded that transfusion was likely to
necessary when the Hb value dropped below 7 g/dl and unlikely to
necessary when it was greater than 10 g/dl (11).
Strengths
There is a strong association of RBC transfusion with mortality a
postoperative morbidity. RBC transfusion increases risk for mortality a
several morbidities in surgical patients (3,12,13). Benchmarking transfus
activity may help to decrease the inappropriate use of blood products, red
the cost of care and optimize the use of voluntary donors gift.
Limitations
There might be substantial differences in the blood components practices
across hospitals and across countries, which may reduce the comparability o
the results. Furthermore, blood transfusion may be affected by the local sup
of blood products, in a way that a serious shortage may cause underrepresentation of the blood components use, especially in countries that are
often facing blood donor shortage periods.
USE OF BLOOD COMPONENTS
2. Operational
definition
PAGE 3
Numerator
The amount of intra- and postoperative blood components transfused for
patients involved in denominator.
Definition of component for transfusion: A component for transfusion
prepared either from whole blood donation (450+/- 10%) mL or collected
aphaeresis. One unit means component derived from whole blood donat
(450+/- 10%) mL. For platelet aphaeresis, the number of units collected fr
the donor in one session should be shown on the label or contained in
product information leaflet (Guide to the preparation, use and qua
assurance of blood components, Recommendation No. R (95) 15, Counci
Europe, 2008).
PAGE 4
USE OF BLOOD COMPONENTS
3.
Denominator
All patients who underwent selected elective surgical procedures in a giv
time period (based on the DRG code, see below) for which intra-operat
and/or postoperative transfusion was requested.
Exclusion
(1) Patients known to have pre-existing abnormalities of the coagulat
system (documented by history of bleeding and/or preoperative internatio
normalised ratio >1.5 or prothrombin time (PT) <=0.35; thrombocyte co
<50 000/l).
(2) Patients submitted to more than one type of surgical procedure during
same hospital episode.
(3) Re-operated patients for the same type of procedure.
Tracer procedures (Australian DRG codes): Elective surgical procedu
selected because they are frequently performed and often involve or mi
involve blood transfusion:
Aortofemoral bypass unilateral (AF) DRG 32708-00
Primary unilateral total knee replacement (TKR) DRG 49518
Primary unilateral total hip replacement, cemented or non-cemen
(THR) DRG 49318-00
Transurethral prostatectomy (TURP) for prostate adenoma DRG 372
00
Coronary artery bypass graft (CABG) surgery DRG 38497; 38500; 3850
4. Previous
Not applicable
PATH
experience
5. Data source
Prospective data collection during two months or at least consecutive
cases (April-May 2010), based on the patients clinical file and administrat
discharge information. The files of the hospital transfusion service might
useful to compare the record of requests and transfusion complications
each patient.
If possible retrospective data collection during the entire year period, cover
possible seasonal changes in the blood components use.
Data on individual level: protocols of surgery and anaesthesiology. This
based on the requirement that every blood component must be well record
either subject to various laws or other regulations that control the collecti
preparation and the use of blood components.
Data collection tool
A layout of a data collection Excel sheet is proposed.
USE OF BLOOD COMPONENTS
6. Domain
PAGE 5
Clinical effectiveness
Safety
Responsive governance
7. Type of
indicator
Outcome measure
PAGE 6
USE OF BLOOD COMPONENTS
8. Adjustment/
stratification
Stratification can be done at country or hospital level to explain local variat
over time or differences between hospitals. Data for adjustment/stratificat
is presented at the data collection forms shown as follows:
-
age,
sex,
preoperative Hb <=90 g/L or >90 g/L,
preoperative data, intra-operative data, early post-operative (within
hours) and post-operative (after 24 hours, within hospitalization) da
(Appendix A)
If only 30 cases are observed, stratification is problematic.
It is recommended to obtain the clinicians agreement to participate
providing data (this is due to the multiple treatment approaches, includ
anaesthesiology, surgery, clinical transfusion service and possibly ot
departments).
9. Subindicators
For the analysis and better understanding of variations in transfusion pract
it is suggested to define, for each patient underwent the procedure if
blood components including red blood cells, plasma, platelets have be
transfused previous to the operation, during the operation, within po
operative period within 24 hours after surgery to the patient discharge.
Also, to develop better understanding on the reasons for variations
transfusion practice and design appropriate recommendation for improving
is suggested to define if patient received autologous blood transfusion.
The number of patients underwent the procedure without blood transfusion
any blood components should also be computed )
At the level of each procedure which means at the level of patient record
number of red cell units cross-matched and the number of units transfus
Based on these data the following 3 indices could be calculated:
Calculation for each procedure including the following:
C/T ratio: Cross-match (C) to Transfusion ratio = No. of red cell units crossmatched / No. of units transfused. A C/T ratio of <=2.5 is indicative of
significant blood usage. A C/T ratio of >2.5 means that less than 40% of cros
matches are transfused) (18).
Transfusion Probability (%T): No. of patients transfused x 100 / No.
patients cross-matched. (A value of 30 is indicative of significant blood usa
(19).
Transfusion Index (TI): No. of units transfused / No. of patients cro
matched. (A value of 0.5 is indicative of significant blood utilization).
average number of units used per patient cross-matched by T I signifies
appropriateness of number of units ordered. It is suggested that a proced
that uses <0.5 units of blood per procedure does not require a preoperat
6
USE OF BLOOD COMPONENTS
PAGE 7
cross-match.
10.Related
indicators
- Length of hospital stay,
The following indicator are not computed in the frame of PATH09 but if
monitored in the hospital, it might be relevant to relate to:
- Patient expectations
-Training expenditure
PAGE 8
USE OF BLOOD COMPONENTS
11.Interpretatio
n
Improvement involves better coordination of care (surgery, blood bank
hospital transfusion service, anesthesiology and nursing) and m
appropriate use of blood.
Studies report wide variations in blood utilization between and wit
countries, even within the same hospital. Variations mainly reflect lo
practices despite the number of published guidelines concerning the optim
use of blood and blood components in different clinical settings. In turn,
means that the interpretation must be performed cautiously, taking i
account all possible modifying effects.
Other factors to take into account are: The use of technologies to decre
perioperative allogenic blood transfusion, including pharmaceutical drugs su
as aprotinin, desmopresin, tranexamic acid, erythropoietin and autolog
transfusion
techniques
such
as
ANH
(autologous
normovole
haemodilution), ICS (Intraoperative Cell Sarver), PAD (Preoperative autolog
donation) and POS (Postoperative salvage) (14,15). The administration
antifibrinolytic (tranexamic acid) in total hip replacement is effective
reducing the blood loss and transfusion requirements, especially in wom
and also effective in total knee replacement surgery (16,17).
12.Guidelines
Guidelines on the Management of Massive Blood Loss. British Journal of
Haematology 2006; 135(5): 634-41.
Guidelines for the use of fresh-frozen plasma, cryoprecipitate and
cryosupernatant. Brit J Haematol 2004,126,11-28.
Guidelines for policies on Alternatives to Allogeneic Blood Transfusion.
Transfusion Medicine 2007; 17(5): 35465.
Guidelines For The Use Of Platelet Transfusions. British Journal of Haematolo
2003; 122(1): 10-23.
The clinical use of red cell transfusion. British Journal of Haematology 2001;
113(1): 24-31.
Guidelines for autologous transfusion. II. Peri-operative haemodilution and c
salvage. British Journal of Anaesthesia 1997; 78: 768-71.
Guidelines for implementation of a maximum surgical blood order schedule.
Clinical and Laboratory Haematology 1990; 12: 321-27.
Practice Guidelines for Blood Transfusion: A Compilation from Recent PeerReviewed Literature. American red Cross, April, 2007.
USE OF BLOOD COMPONENTS
13.References
PAGE 9
1. Vamvakas EC. Epidemiology of red blood cell utilization. Transfus Med
1996;10(1):44-61.
2. Marik PE, Corwin HL. Efficacy of red blood cell transfusion in the critically il
systematic review of the literature. Crit Care Med 2008;36:2667-74.
3. Reevers BC, Murfy GJ. Increased mortality, and cost associated with red blood
transfusion after cardiac surgery. Curr Opin anaesthesiol 2008;21(5):669-73.
4. Pham JC, Catlett CL, Berenholtz SM, Haut ER. Change in use of allogeneic red bl
cell transfusions among surgical patients. J Am Coll Surg 2008;207(3):352-9.
5. Gombotz H, Rehak PH, Shander A, Hofman A. Blood use in elective surgery:
Austrian benchmark study. Transfusion 2007; 47(8):1468-80.
6. Sirchia G, Giovanetti AM, McClelland DBL, Fracchia GN. Safe and Good Use of Bl
in Surgery (SANGUIS). European Commission 1994.
7. OSTHEO Investigation, Transfusion 2003;43(4):459-69
8. WHO publication number WHO/BTS/99-3: The clinical use of blood: Handbo
WHO Blood Transfusion Safety: Geneva; 2001.
9. Hogman CF, Bagge L, Thoren L. The use of blood components in surg
transfusion therapy. World J Surgery 1987;11:2-13.
10. Carson JL, Hill S, Carless P, Hebert P, Henry D. Transfusion triggers: A system
review of the literature. Transfusion Med Rev 2002:16:187-99.
11. Gettinger A. Transfusion in the preoperative period: A consideration of the r
and benefits as a guide to determine when and who to transfuse.
ACCS:2005.p.158-62).
12. Kertai MD, Tiszai-Szucs T, Varga KS, Hermann C, Acsady G, Gal J. Intraopera
use of packed red blood cell transfusion and mortality in patients undergo
abdominal or thoracoabdominal aortic aneurysm surgery. J Cardiovasc S
(Torino) 2009;
13. Bernard AC, Davenport DL, Chang PK, Vaughan TB, Zwischenberger
Intraoperative transfusion of 1 U to 2 packed red blood cells is associated w
increased 30-day mortality, surgical-site infection, pneumonia, and sepsis
general surgery patients. J Am Coll Surg 2009;208(5):937
14.Katz E, Gaitini L, Samri M, Egoz N, Fergusson D, Laupacis A. The use of
technologies to decrease peri-operative allogenic blood transfusion: results of
practice variation in Israel. Isr Med Assoc J 2001;3(11) 809-12
15.Cohrane Database syst Rev 2007;17(4):CD0018862
16. Rajesparan K, Blant LC, Ahmad M, Field RE. The effect of an intravenous bolu
tranexamic acid on blood loss in total hip replacement. J Bone Joint Surg
2009;91(6):776-83
17. Camarasa Godoy MA, Serra-Prat M, Palomera Fanegas E. Effectiveness
tranexamic acid in routine performance of total knee replacement surgery. Rev
Anestesiol Reanim 2008;55(2):75-80).
18. Friedman BA, Oberman HA, Chadwick AR, Kingon KI. The maximum surgical bl
order schedule and surgical blood use in the United States. Transfu
1976;380:387.
19. Mead JH, Anthony CD, Sattler M. Haemotherapy In Elective Surgery: an incide
report, review of literature, and alternatives for guideline appraisal. Am J Clin P
9
PAGE 10
USE OF BLOOD COMPONENTS
1980;74:223-227.
10
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Cancer Fighting StrategiesDocument167 pagesCancer Fighting StrategiesCaptainjillNo ratings yet
- Young Schema TheoryDocument14 pagesYoung Schema TheoryMike F MartelliNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Vanessa Tarot BookletDocument36 pagesVanessa Tarot BookletClassic Bobby100% (2)
- Fundamentals of EU Regulatory Affairs, Fifth Edition Comparative MatrixDocument42 pagesFundamentals of EU Regulatory Affairs, Fifth Edition Comparative Matrixasifmdzakaria57% (7)
- Biosimilars PathwayDocument13 pagesBiosimilars Pathwaytamara_0021No ratings yet
- Cardiac MarkersDocument23 pagesCardiac MarkersAsmaaYLNo ratings yet
- What Is Cerebral PalsyDocument16 pagesWhat Is Cerebral PalsyIan FordeNo ratings yet
- List of CAPE 2012 Scholarships Recipients by SchoolsDocument13 pagesList of CAPE 2012 Scholarships Recipients by SchoolsIan FordeNo ratings yet
- OD-PRO-HSE-032 Safety To Work at Height - Rev.01Document31 pagesOD-PRO-HSE-032 Safety To Work at Height - Rev.01aymenmoataz100% (1)
- Cardiovascular ADocument3 pagesCardiovascular AAutumn AllisonNo ratings yet
- Periodontics PDFDocument195 pagesPeriodontics PDFدينا حسن نعمة100% (1)
- Thyroid Disease GuideDocument65 pagesThyroid Disease GuideIan FordeNo ratings yet
- TB Teaching PlanDocument5 pagesTB Teaching PlanTrisha Fae Loyola Balagot100% (1)
- RIFLE ClassificationDocument7 pagesRIFLE ClassificationIan FordeNo ratings yet
- A HX of Acute Abd. PainDocument15 pagesA HX of Acute Abd. PainIan FordeNo ratings yet
- Physics Unit 1 Paper 2 2009Document10 pagesPhysics Unit 1 Paper 2 2009gabrielleNo ratings yet
- Benefits of BreastfeedingDocument20 pagesBenefits of BreastfeedingIan FordeNo ratings yet
- Graves' Disease Graves Has Been Credited As Having Recognized The Association Between Hyperthyroidism and Diffuse Enlargement of The GlandDocument3 pagesGraves' Disease Graves Has Been Credited As Having Recognized The Association Between Hyperthyroidism and Diffuse Enlargement of The GlandIan FordeNo ratings yet
- Plummer Vinson Syndrome FlashcardsDocument2 pagesPlummer Vinson Syndrome FlashcardsIan FordeNo ratings yet
- Peds BLSDocument5 pagesPeds BLSIan FordeNo ratings yet
- Unit1paper2 2005 CapeDocument10 pagesUnit1paper2 2005 CapeashtigosineNo ratings yet
- Growth ChartDocument4 pagesGrowth ChartGenevieve Caecilia Linda KartonoNo ratings yet
- Plummer Vinson Flashcards (IncompleteDocument2 pagesPlummer Vinson Flashcards (IncompleteIan FordeNo ratings yet
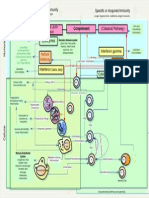
- Immunology Clerkship Review mdsc3314Document6 pagesImmunology Clerkship Review mdsc3314Ian FordeNo ratings yet
- Mini-Clinical Evaluation Ecercise (CEX) - Medical StudentsDocument2 pagesMini-Clinical Evaluation Ecercise (CEX) - Medical StudentsIan FordeNo ratings yet
- Top 10 AnemiasDocument23 pagesTop 10 AnemiasPierfelice CutrufelliNo ratings yet
- Write UpDocument2 pagesWrite UpIan FordeNo ratings yet
- Who Asked The First Question: The Origins of Human Choral Singing, Intelligence and SpeechDocument460 pagesWho Asked The First Question: The Origins of Human Choral Singing, Intelligence and SpeechTheHakeemTNo ratings yet
- A Hitchhiker's Guide To The Immune SystemDocument1 pageA Hitchhiker's Guide To The Immune SystemIan FordeNo ratings yet
- Anatomy Lab ScheduleDocument2 pagesAnatomy Lab ScheduleIan FordeNo ratings yet
- AQA CHEM1 W QP Jan11Document16 pagesAQA CHEM1 W QP Jan11ooh704No ratings yet
- 4037 s03 QP 1Document8 pages4037 s03 QP 1linusshyNo ratings yet
- Kindergarten q1 Week10 v2Document33 pagesKindergarten q1 Week10 v2Aryan Angela Dela CruzNo ratings yet
- Nutrition Counseling And Dietary InstructionDocument5 pagesNutrition Counseling And Dietary Instructionnicoleangela ubasroselloNo ratings yet
- ASCGULF Company: Mohammad Gousu Basha ShaikDocument3 pagesASCGULF Company: Mohammad Gousu Basha ShaikmohammadgouseNo ratings yet
- Buku Koding 1Document74 pagesBuku Koding 1indra_igrNo ratings yet
- General Duties and Responsibilities of An Electrical Engineer in Construction IndustryDocument2 pagesGeneral Duties and Responsibilities of An Electrical Engineer in Construction Industryumer100% (1)
- Effect of Smoking On HalitosisDocument5 pagesEffect of Smoking On HalitosisMaria JabbarNo ratings yet
- STERILE PARENTERAL FORMULATIONSDocument85 pagesSTERILE PARENTERAL FORMULATIONSShalimashalu100% (1)
- Assisted SuicideDocument30 pagesAssisted SuicideAlex Mini AndraNo ratings yet
- Hydrogen Sulphide Safety Around RigDocument14 pagesHydrogen Sulphide Safety Around RigmohammedNo ratings yet
- Invega Sustenna PIDocument13 pagesInvega Sustenna PIAisha SyedNo ratings yet
- Calamba Doctors' College: Virborough Subdivision, Parian, Calamba City, LagunaDocument15 pagesCalamba Doctors' College: Virborough Subdivision, Parian, Calamba City, LagunaJasthen Audrey StamboughNo ratings yet
- Slide PPT PrismaDocument31 pagesSlide PPT PrismaUlul Azmi AdnanNo ratings yet
- Annex 6: Guidance On Good Manufacturing Practices (GMP) : Inspection ReportDocument5 pagesAnnex 6: Guidance On Good Manufacturing Practices (GMP) : Inspection Reportumarn1582No ratings yet
- AMEE 2023 Final Programme OverviewDocument2 pagesAMEE 2023 Final Programme OverviewMohamed IshagNo ratings yet
- CHN Assignment (Community Health Nursing)Document21 pagesCHN Assignment (Community Health Nursing)binjuNo ratings yet
- Douglas Crucey, A043 446 797 (BIA June 12, 2017)Document20 pagesDouglas Crucey, A043 446 797 (BIA June 12, 2017)Immigrant & Refugee Appellate Center, LLCNo ratings yet
- Ar-Afff 3 MSDS LCFDocument5 pagesAr-Afff 3 MSDS LCFMark YeNo ratings yet
- Tugas Jurnal TeksolDocument6 pagesTugas Jurnal TeksolNovita IndahNo ratings yet
- What is pancytopenia and its causesDocument33 pagesWhat is pancytopenia and its causesDabogski FranceNo ratings yet
- Acy 087Document14 pagesAcy 087johnsmithdosNo ratings yet