Professional Documents
Culture Documents
Nursing process, safety, positioning & communication tips
Uploaded by
Nathalee WalkerOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing process, safety, positioning & communication tips
Uploaded by
Nathalee WalkerCopyright:
Available Formats
MASLOW1. Eliminate psychosocial answers if there are physiological answers present.
2. Does this make sense?
3. ABCs- Airway, breathing, circulation
NURSING PROCESS1. Recognize both assess and implement angers.
2. Read stem of question to choose to assess or implement.
3. Select best assessment or implementation.
SAFETY1. All answers must be implementations.
2. Try to answer based on knowledge; if you cant.
3. What will cause the least amount of harm to the pt?
DELEGATION1. Dont delegate assessment, teaching, evaluation, or nursing judgment.
2. Delegate care for only stable pts with expected outcomes.
3. Delegate tasks that involve standard unchanging procedures.
POSTITIONING1. Are you trying to promote or prevent?
2. What are you trying to promote or prevent?
3. Think A & P!!!
THERAPUTIC COMMUNITICATION1. No Dont worry
2. No explore answers.
3. Dont ask why?
4. No authoritarian answers
5. No focus on the nurse answers
6. No closed-ended questions.
Blood Products
In an emergency, O-negative blood can be safely administered to most
clients without serologic testing.
No solution other than normal saline solution should be added to blood
components.
As a means of avoiding septicemia, the nurse should not allow an infusion of
1 unit of blood to take longer than 4 hours; the blood-administration set
should be changed every 4 to 6 hours, or in accordance with agency policy, if
more than 1 unit is to be administered.
Blood products must be administered within 30 minutes of their being
received from the blood bank.
Never store blood in a refrigerator other than those used in blood banks
(blood bank refrigerators are equipped with controlled temperatures designed
for blood storage); if blood obtained from the blood bank is not administered
within 30 minutes, return it to the blood bank.
Vital signs and lung sounds should be checked before the transfusion, again
after the first 15 minutes, and every hour until 1 hour has elapsed since the
transfusion was completed.
The most important part of the transfusion process is confirmation of product
compatibility and verification of client identity.
A Jehovahs Witness may not receive blood or blood products.
Ensure that informed consent has been obtained before administering a
blood transfusion.
The first 15 minutes of the blood transfusion are the most critical part of the
transfusion, and the nurse must stay with the client.
Instruct the client to immediately report anything unusual while receiving the
transfusion.
If a transfusion reaction occurs, stop the transfusion immediately.
IV Therapy
An IV line provides a route of entry into the body for microorganisms.
Isotonic solutions have the same osmolality as body fluids.
The smaller the gauge of an IV device, the larger the outside diameter of the
cannula.
A microdrip chamber delivers 60 drops (gtt) per milliliter.
The IV filter should be changed at least every 72 hours (depending on agency
policy) to help prevent bacterial growth.
The IV solution should be checked against the physicians prescription for
type, amount, percent of solution, and rate of flow.
Identify conditions that contraindicate the use of a particular IV solution.
Clients with respiratory, cardiac, renal, or liver diseases; older clients; and
very young persons cannot tolerate excess fluid volume and are at risk for
fluid overload.
Change the venipuncture site every 72 hours or as specified by agency policy.
Change the IV dressing every 72 hours, when the dressing is wet or
contaminated, and as specified by the agency policy.
Change the IV tubing every 72 hours (central line tubing is changed every 24
hours) or as specified by agency policy.
The signs of thrombophlebitis include heat, redness, and tenderness at the IV
site; a hard, cordlike vein; and sluggish infusion of the IV solution.
The signs of infiltration include edema, pain, and coolness at the IV site.
Check an adults IV line every 30 minutes, a childs every 15 minutes.
For children, the maximum amount of IV fluid that may be administered in a
24-hour period varies; it is usually based on body weight, among other
factors.
Parental Nutrition
After a central venous catheter is inserted, a portable chest radiograph
should be performed to confirm correct catheter placement and to detect
pneumothorax. PN should not be initiated until it is determined that no
pneumothorax is present.
Check the components of the PN solution against the physicians prescription.
PN solution should be stored under refrigeration and administered within 24
hours of the time at which the solution was prepared. (Remove the solution
from the refrigerator 30 minutes to 1 hour before use.)
PN solution that is cloudy or darkened should not be used; instead, it should
be returned to the pharmacy.
PN is always delivered with the use of an electronic infusion device.
As a means of preventing infection and solution incompatibility, IV
medications and blood are never given through the PN line.
Before administering lipids, assess the client for an allergy to eggs or any of
the components of the lipid emulsion solution.
Examine the lipid preparation for separation of emulsion into layers or fat
globules and for the accumulation of froth; if such separation is noted, do not
use the solution and return it to the pharmacy.
Use strict aseptic technique when caring for the central venous catheter. (Not
only is the central line a possible avenue for the entry of microorganisms into
the body, but the PN solution also contains a high concentration of glucose,
making it an ideal medium for bacterial growth).
Check the blood glucose level every 4 to 6 hours or in accordance with
agency protocol.
If an air embolism is suspected, place the client in a left sidelying position
with the head lower than the feet (which traps air in right side of the heart),
administer oxygen as prescribed, and notify the physician.
To help prevent hypoglycemia, gradually decrease the infusion rate when
discontinuing PN.
Provide instructions to the client who will be receiving PN at home.
Medication Classification
Focus on the subject of the question and note whether the question is asking
about the intended effect, side effect, or adverse effect.
It is nearly impossible to learn everything about every individual medication.
Learn medications by their classifications because of the similarities that exist
among medications in a given classification (e.g., bronchodilators dilate the
bronchi of the lungs).
Learn medications belonging to a particular classification by remembering
commonalities in their names (e.g., the names of xanthine bronchodilators,
such as theophylline, end in -line). (Specific commonalities are discussed on
the next screen.)
Learn to recognize the side effects commonly associated with each class of
medications and then relate the appropriate nursing interventions to each
side effect (e.g., if a side effect is hypertension, the associated nursing
intervention would be to monitor the client's blood pressure).
Look at the medication name and use medical terminology to help determine
the medications action (e.g., lopressor lowers ["lo"] the blood pressure
["pressor"]).
Assess the client for allergies and hypersensitivity to the prescribed
medication.
Assess the client for existing medical disorders that contraindicate the
administration of a prescribed medication.
The older client and the neonate and infant are at greater risk for medication
toxicity than are the adult client.
Nursing interventions always include checking the client's vital signs,
monitoring significant laboratory results, watching for side effects of the
medication, and client education.
Many medications are contraindicated in pregnancy, during breastfeeding,
and in infants and children.
The client should avoid taking over-the-counter medications or any other
medications (e.g., herbal preparations) unless they are approved for use by
the healthcare provider.
The client should wear a Medic-Alert bracelet if he or she is taking certain
medications such as anticoagulants, oral hypoglycemics or insulin, certain
cardiac medications, corticosteroids and glucocorticoids, antimyasthenic
medications, anticonvulsants, and monoamine oxidase inhibitors.
The client should follow up with the healthcare provider as prescribed.
Androgens: Most names end with -terone (e.g., testosterone).
Angiotensin-converting enzyme (ACE) inhibitors: Most names end with
-pril (e.g., enalapril [Vasotec]).
Antidiuretic hormones: Most names end in -pressin (e.g., desmopressin
[DDAVP]).
Antilipemic medications: Many end with -statin (e.g., atorvastatin
[Lipitor]).
Antiviral medications: Most contain vir (e.g., acyclovir [Zovirax]).
Benzodiazepines: Although this class includes medications such as
alprazolam (Xanax) and chlordiazepoxide (Librium), most names such as
diazepam (Valium) end in -pam. (Another tip for identifying a benzodiazepine:
The name includes a vowel-z-vowel combination.)
Beta-adrenergic blockers: Most names end with -lol (e.g., atenolol
[Tenormin]).
Calcium channel blockers: Most names end in -pine (e.g., amiodipine
[Norvasc]); exceptions include diltiazem (Cardizem, Cardizem SR) and
verapamil (Calan, Isoptin).
Carbonic anhydrase inhibitors: Most names end in -mide (e.g.,
dorzolamide [Trusopt]). These medications are used to treat glaucoma.
Estrogens: Most names contain -est (e.g., estradiol (Estrace) or conjugated
estrogen [Premarin]).
Glucocorticoids and corticosteroids: Most names end in -sone (e.g.,
prednisone).
Histamine H2 receptor antagonists: Most names end in -dine (e.g.,
cimetidine [Tagamet]).
Nitrates: Most names contain nitr (e.g., nitroglycerin [Nitrostat]).
Pancreatic enzyme replacements: Most names contain pancre (e.g.,
pancrealipase [Pancrease]).
Proton pump inhibitors: Most names end in -zole (e.g., lansoprazole
[Prevacid]).
Sulfonamides: Most names include sulf (e.g., sulfasalazine [Azulifidine]).
Sulfonylureas: Most names end in -ide (e.g., glipizide [Glucotrol]). These
medications are used to treat diabetes mellitus.
Thiazide diuretics: Most names end in -zide (e.g., hydrochlorothiazide
[Hydrodiuril]).
Thrombolytics: Most names include -ase (e.g., alteplase [Activase]).
Thyroid hormones: Most names contain thy (e.g., levothyroxine
[Synthroid]).
Xanthine bronchodilators: Most names end in -line (e.g., theophylline).
Cardiac Disorders
Stay with the client when the client is experiencing chest pain.
The head of the bed is elevated for a client with a cardiac disorder.
Vital signs are monitored and the apical heart rate counted for 1 full minute.
Assist the client in identifying risk factors that can be modified and help the
client set goals that will promote the necessary lifestyle changes.
The client must be instructed in the use of prescribed medications.
Teach the client about necessary dietary changes; such changes are not
temporary and must be maintained for life.
Aid the client who has mobility restrictions in performing range-of-motion
exercises to prevent thrombus formation and maintain muscle strength.
Provide reassurance to the client and family.
Provide information to the client on community resources for exercise,
smoking cessation, and stress reduction.
Venous Disorders
The client with a venous disorder is usually advised to wear antiembolism
stockings during the day and evening; these should be put on after the client
awakens, before he or she gets out of bed.
The client should avoid prolonged sitting or standing, constrictive clothing,
and crossing the legs when seated.
The client should elevate the legs for 10 to 20 minutes every few hours each
day; the legs should be elevated above the level of the heart when the client
is in bed.
Avoid using the knee gatch or placing a pillow under the knees.
Avoid massaging the extremity.
If the client is on bed rest, encourage a change of position every 2 hours.
Teach the client to use intermittent sequential pneumatic compression
system (to reduce venous stasis and aid venous return of the blood to the
heart), if prescribed; usually the client is advised to apply the compression
system twice daily for 1 hour, morning and evening.
Inspect the legs for edema and measure and record the circumference of
each thigh and calf.
Plan a progressive walking program.
When performing wound care or dressing changes, keep tape off the skin by
applying tape to the dressing material.
Instruct the client to cease or avoid smoking.
Stress the importance of follow-up physician visits and laboratory studies.
The client should obtain and wear a Medic-Alert bracelet.
Arterial Disorders
Teach the client to walk to the point of claudication, stop and rest, then walk
a little farther.
Instruct the client to elevate the feet while at rest but to refrain from
elevating them above the level of the heart, because extreme elevation slows
arterial blood flow to the feet. (In severe peripheral arterial disease, a client
with edema may sleep with the affected limb hanging from the bed or sit
upright in a chair for comfort.)
The client should avoid crossing the legs, avoid exposing the extremities to
cold (which causes vasoconstriction), and wear socks or insulated shoes for
warmth at all times.
Warn the client never to apply heat directly to the limb (e.g., heating pad or
hot water), because the decreased sensitivity in the limb make it easier to
sustain a burn.
The client should inspect the skin of the extremities daily and report signs of
skin breakdown.
Advise the client to avoid the use of tobacco and caffeine because of their
vasoconstrictive effects.
Endocrine Disorders
The endocrine system consists of organs or glands that secrete hormones
and release them directly into the circulation.
Disorders of this body system can be easily understood if you remember that
they basically involve one of two situations: hypersecretion or hyposecretion
of hormones from a particular organ or gland.
When an excess of the hormone occurs, treatment is aimed at blocking
hormone release through the use of medication or surgery.
When a deficit of the hormone exists, treatment is aimed at replacement
therapy.
Therefore, when you need to answer a question on NCLEX that involves a
disorder of the endocrine system, focus on the gland and think about its
function, then determine whether the condition is one that causes an excess
or a deficit of the hormone.
Integumentary Disorders
The integumentary system provides the first line of defense against
infections; therefore, a priority intervention for a client with altered skin
integrity is to institute measures to prevent infection.
The priority psychosocial issue related to a client with an integumentary
disorder is body image disturbance.
Many of the integumentary disorders can cause pruritus, and the nurse needs
to institute measures that will relieve the discomfort associated with pruritus
and teach the client about the importance of avoiding scratching the skin.
Oncology Disorders
Priority concerns for the client with an oncological disorder include relieving
pain, monitoring for life-threatening conditions such as infection and
bleeding, and addressing end-of-life issues as appropriate.
Remember that pain is what the client says that it is; do not undermedicate
the cancer client who is in pain.
Many treatments for cancer cause bone marrow destruction; neutropenic or
bleeding precautions may need to be instituted to protect the client.
The clients personal, religious, and cultural beliefs and practices need to be
considered in the plan of care when addressing end-of-life issues.
GI Disorders
Nutrition is a primary concern for the client with a gastrointestinal disorder.
After diagnostic tests, return of the gag reflex must be confirmed before the
client is allowed to consume food or fluids.
After abdominal surgical procedures, bowel sounds must return before the
client is allowed to consume food or fluids.
Body image disturbances and social isolation issues are concerns for the
client in whom a diversion, such as an ileostomy or colostomy, has been
created.
Respiratory Disorders
Airway patency is the priority.
Oxygen is prescribed for clients with respiratory disorders.
Monitor the client for respiratory distress.
Monitor pulse oximetry readings.
Restlessness, confusion, and a decrease in the level of consciousness are
indicators of a respiratory problem.
Most respiratory disorders are marked by dyspnea, tachycardia, tachypnea,
hypotension, cyanosis, and use of, the accessory muscles for breathing.
The cause of the respiratory disorder is identified and then treated.
Encourage coughing and deep breathing; respiratory treatments and chest
physiotherapy are usually prescribed.
Place the client with a respiratory disorder in a Fowler to high Fowler position
to facilitate breathing.
Instruct the client to splint the chest to cough and to deepbreathe.
Administer pain medication as prescribed if the client is experiencing pain
after sustaining an injury.
If the client is expectorating sputum, record the color, amount, and
consistency.
Perform suctioning, if necessary, to clear airway and prevent infection
resulting from the accumulation of secretions.
Monitor the clients weight, because nutrition can be a concern with
respiratory problems.
Encourage small, frequent meals (a high-calorie, high-protein diet with
supplements) help to prevent dyspnea.
Encourage fluids, as much as 3000 mL/day unless contraindicated, to keep
secretions thin.
Activity is allowed as the client can tolerate it, but stress the importance of
rest and proper nutrition.
The client must be informed of the importance of not smoking and avoiding
passive exposure to smoke.
Stress the importance of influenza and pneumonia vaccines.
Renal Disorders
Intake and output, weight, and vital signs should be monitored closely in the
client with a kidney disorder.
The blood urea nitrogen (BUN) and creatinine levels must be monitored,
because they reflect renal function.
The nurse must be aware of any nephrotoxic medications being taken by the
client.
The manifestations of acute kidney injury and chronic kidney disease are the
result of the retention of waste and fluids and the inability of the kidneys to
regulate electrolytes.
Continuous cardiac monitoring should be instituted in the client with acute
kidney injury or chronic kidney disease, because hyperkalemia may develop,
resulting in life-threatening dysrhythmias.
Graft rejection is a primary concern after transplantation.
Eye Disorders
Safety is a priority for the client with an eye disorder.
After eye surgery, unless otherwise prescribed, the client should be
positioned with the head of the bed elevated on the nonoperative side to
prevent swelling.
After cataract surgery, the client must avoid activities that will increase
intraocular pressure.
If the client who has undergone eye surgery experiences severe eye pain, the
surgeon is notified immediately, because this could indicate an increase in
intraocular pressure.
The client with glaucoma may need to take eye medication for life to keep
the intraocular pressure at a normal level.
Bright-red drainage on a dressing after eye surgery must be reported to the
surgeon immediately, because it could indicate hemorrhage.
Ears Disorders
Risk factors for ear disorders include advancing age, infection, medications,
ototoxicity, trauma, and tumors; genetics may also play a part.
The nurse must choose an appropriate means of communication with the
client with a hearing disorder.
Safety is a priority concern for the client with an ear disorder.
Ear irrigation is contraindicated in clients with tympanic membrane
perforation or a history of perforation.
The maximal amount of irrigation solution that should be used is 50 to 70 mL.
The temperature of irrigation solution should be close to that of the body.
During irrigation, the solution is directed toward the wall of the ear canal.
Neurological Disorders
Monitor a client with a neurological disorder for signs of increased intracranial
pressure.
The earliest indicator of increased intracranial pressure is deterioration in the
level of consciousness.
Airway is always a priority for a client with a neurological disorder.
A client with a head injury should be placed in a head-elevated position.
The victim of an accident should not be moved until it has been determined
that that the person has not sustained a spinal cord injury.
Measures to ensure safety are a priority for the client with a neurological
disorder.
Promote independence in regard to self-care activities as much as possible.
Encourage discussion about the psychosocial issues that may occur as a
result of the neurological disorder (e.g., body image alterations, altered
sexual function).
Musculoskeletal Disorders
Pain is a primary concern in the care of the client with a musculoskeletal
disorder.
Promote self-care measures and work to maintain client independence.
Teach the client about the use of assistive devices, if needed, for ambulation.
Address the body image changes that occur as a result of musculoskeletal
disease or injury.
Immune Disorders
Protecting the client with an immune disorder from infection is the primary
intervention.
Standard precautions are maintained to prevent infection.
Provide protective isolation if the clients immune system is depressed.
Immunotherapy may be prescribed to stabilize the immune system.
Have resuscitation equipment available if skin testing is performed, because
the allergen may induce an anaphylactic reaction.
The infant or child infected with HIV is at risk for life-threatening opportunistic
infection; monitor the client closely for signs of infection and report these
signs immediately to the physician if they occur.
Medical Emergencies
Disseminated intravascular coagulation is an exaggerated clotting process,
and clients with sepsis, trauma, malignancy, organ destruction, hepatic
failure, or toxic reactions may be predisposed to this condition.
Oncologic emergencies (e.g., syndrome of inappropriate antidiuretic
hormone, spinal cord compression, hypercalcemia, superior vena cava
syndrome, and tumor lysis syndrome) are life-threatening situations that may
occur as a result of cancer or cancer treatment.
Assessing a victim for responsiveness is always the first step in lifesaving
efforts.
If a head, neck, or spinal cord injury is suspected, the jaw-thrust maneuver is
used to open the airway.
If the victim is younger than 1 year, use the brachial pulse to assess
circulation.
The location for hand placement for chest compressions on a child is the
same as that for an adult; in a child, use the heel of one hand.
In an infant, the breastbone is compressed 1.5 inches at a rate of 100
times/min.
Minimize interruptions when performing cardiopulmonary resuscitation (CPR).
In an infant, an airway obstruction is relieved with the use of five back blows
and five chest thrusts.
Hemodynamics
Shock is a life-threatening condition that requires immediate medical
treatment because it can cause damage to multiple organs.
An increased central venous pressure indicates an increase in blood volume
as a result of sodium and water retention, excessive IV fluids, alterations in
fluid balance, or kidney failure; a decreased central venous pressure indicates
a decrease in circulating blood volume and may be the result of fluid
imbalance, hemorrhage, or severe vasodilation with pooling of blood in the
extremities that limits venous return.
The goal of treatment for a client with decreased cardiac output is to
maintain tissue oxygenation and perfusion and improve the pumping ability
of the heart.
Ventricular tachycardia is a life-threatening condition that can lead to
ventricular fibrillation and requires immediate intervention (defibrillation and
cardiopulmonary resuscitation).
Ventricular fibrillation is rapidly fatal if not successfully terminated within 3 to
5 minutes; defibrillation is the immediate intervention.
During defibrillation, ensure that no one is touching the bed or client when
the shock is delivered.
Instruct the client with a pacemaker to keep a pacemaker identification card
in the wallet and obtain and to wear a Medic-Alert bracelet.
Hypertensive crisis is an acute and life-threatening condition requiring
immediate reduction in the blood pressure; target organ damage (i.e., brain,
heart, kidneys, retinas) may occur quickly, with death resulting from stroke,
renal failure, or cardiac disease.
In the client with an internal arteriovenous fistula or graft, palpate or
auscultate for a thrill and bruit, which indicate patency.
A primary concern for the client undergoing peritoneal dialysis is peritonitis.
Fluid & Electrolytes
Total body fluid accounts for about 60% of body weight.
A loss of 10% of body fluid in the adult is serious; a loss of 20% is fatal.
To function normally, body cells must have fluids and electrolytes in the right
compartments and in the right amounts.
Whenever an electrolyte moves out of a cell, another electrolyte moves in to
take its place.
Third-spacing is the accumulation and sequestration of trapped extracellular
fluid in an actual or potential body space as a result of disease or injury;
trapped fluid represents volume loss and is unavailable for normal
physiological processes.
Edema is an excessive accumulation of fluid in the interstitial spaces.
Fluid-volume deficit is a dehydration in which the body's fluid intake is not
sufficient to meet the body's fluid needs.
Fluid-volume excess occurs when fluid intake or fluid retention exceeds the
body's fluid needs.
Sodium imbalances are commonly associated with fluid-volume imbalances.
Potassium imbalances are potentially life threatening because every body
system is affected.
Potassium chloride is never given by way of IV push or the IM or
subcutaneous route.
The Trousseau and Chvostek signs are seen in hypocalcemia.
During the administration of magnesium, monitor the client for diminished
deep tendon reflexes, which are indicative of hypermagnesemia.
A decrease in the serum phosphorus level is accompanied by an increase in
the serum calcium level; conversely, an increase in the serum phosphorus
level is accompanied by a decrease in the serum calcium level.
Maternity & Newborn Conditions
Women infected with HIV may first demonstrate symptoms at the time of
pregnancy or contract life-threatening infection because normal pregnancy
involves some suppression of the maternal immune system.
The mother with HIV is managed as high-risk because she is vulnerable to
infection.
The mother with cardiac disease may be unable to physiologically cope with
the added plasma volume and increased cardiac output that occur during
pregnancy.
During the first trimester, insulin needs in the diabetic client decrease.
During the second and third trimesters, increases in placental hormones
cause an insulin-resistant state, requiring an increase in the diabetic mother's
insulin dose.
Causes of disseminated intravascular coagulation include abruptio placentae,
intrauterine fetal death, amniotic fluid embolism, severe preeclampsia,
sepsis, and hemorrhage.
HBV is transmitted through blood, saliva, vaginal secretions, semen, and
breast milk and across the placental barrier.
Pyridoxine (vitamin B6) should be administered with isoniazid to the pregnant
woman with tuberculosis to help prevent fetal neurotoxicity.
If a pregnant woman is not immune to rubella, she should be vaccinated
during the postpartum period and avoid becoming pregnant for at least 3
months after receiving the vaccine.
The classic signs of preeclampsia are hypertension, generalized edema, and
proteinuria.
If umbilical cord prolapse occurs, relieve cord pressure immediately by
putting a sterile gloved hand into the vagina and holding the presenting part
off the umbilical cord; place the mother in a modified Sims, Trendelenburg, or
knee-chest position to minimize pressure on the cord.
Sudden onset of painless bright-red vaginal bleeding in the second half of
pregnancy is a sign of placenta previa.
Painful dark-red vaginal bleeding occurs in placental abruption.
Regardless of the serum bilirubin level, the appearance of jaundice during the
first day of life indicates a pathological process.
Hypoglycemia, respiratory distress, hypocalcemia, and hyperbilirubinemia
can occur in an infant born to a mother with diabetes mellitus.
Pediatric Disorders
Monitor a child with a neurological disorder for signs of increased intracranial
pressure.
Aspirin is not administered to a child with varicella or influenza because of its
association with Reye syndrome; acetaminophen (Tylenol) or ibuprofen
(Motrin) is usually prescribed for the pediatric client.
Airway patency is the priority in a child experiencing a seizure.
Chlamydial conjunctivitis is rare in older children; if it is diagnosed in a child
who is not sexually active, the child should be assessed for sexual abuse.
After tonsillectomy, monitor the child for signs of hemorrhage; if hemorrhage
occurs, turn the child to one side to help prevent aspiration of blood and
notify the physician.
To help prevent spasm of the epiglottis and airway occlusion, never attempt
to visualize the posterior pharynx or to obtain a throat culture specimen in a
child with epiglottitis.
Contact precautions are necessary for the child with respiratory syncytial
virus infection.
Parents must be taught the guidelines for the administration of digoxin
(Lanoxin).
The major concerns when a child is vomiting or experiencing diarrhea are the
risk of dehydration, the loss of fluid and electrolytes, and the development of
metabolic alkalosis (with vomiting) and metabolic acidosis (with diarrhea).
Proper handwashing and standard precautions can prevent the spread of viral
hepatitis.
In the event of a poisoning, parents are advised to call the poison control
center before initiating any intervention.
If poisoning occurs, treat the child first, not the poison; assess airway,
breathing, and circulation and initiate cardiopulmonary resuscitation as
necessary.
The child with diabetes mellitus must be educated about diet therapy,
exercise, insulin administration, and complications associated with the
disorder.
Nephrotic syndrome is a kidney disorder characterized by massive
proteinuria, hypoalbuminemia, and edema.
Fractures in infancy are generally rare and warrant further investigation to
rule out child abuse.
The most common opportunistic infection in children infected with HIV is
Pneumocystis jiroveci pneumonia.
Bleeding is the primary concern in a child with hemophilia.
In the child with leukemia, the priority nursing concern is protecting the child
from infection.
Chickenpox (varicella) can be deadly to the immunocompromised child
because the child is unable to fight the illness adequately.
You might also like
- 140 Must Know Meds Demolish Nursing PharmacologyFrom Everand140 Must Know Meds Demolish Nursing PharmacologyRating: 4 out of 5 stars4/5 (18)
- Nclex 3500Document4 pagesNclex 3500chitorNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- RN Plan StudyDocument13 pagesRN Plan Studywestlake12100% (1)
- Delegation NCLEX-RNDocument3 pagesDelegation NCLEX-RNPrince K. Tailey100% (1)
- Nurse collecting data on acute MI findingsDocument6 pagesNurse collecting data on acute MI findingsNadim Khalid0% (1)
- NATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideFrom EverandNATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideNo ratings yet
- Med Surge 2 Mod 3 Study Guide2Document21 pagesMed Surge 2 Mod 3 Study Guide2Dirk Buckner100% (4)
- Med Surge 2 Mod 1 CardiacDocument13 pagesMed Surge 2 Mod 1 CardiacDirk Buckner100% (2)
- Cardiovascular Summary Saunders Comprehensive Review For The Nclex RN ExaminationDocument40 pagesCardiovascular Summary Saunders Comprehensive Review For The Nclex RN ExaminationdanicaNo ratings yet
- Q&A - Pharmacology 2Document14 pagesQ&A - Pharmacology 2eric2690100% (4)
- Every Monday in May Live Facebook ReviewDocument4 pagesEvery Monday in May Live Facebook ReviewChelle RocoNo ratings yet
- Med Surge 2 Mod 3 Study GuideDocument19 pagesMed Surge 2 Mod 3 Study GuideDirk Buckner100% (4)
- Study Guide For NCLEX-RNDocument4 pagesStudy Guide For NCLEX-RNPrince K. TaileyNo ratings yet
- Nclex-Rn Test Study GuideDocument199 pagesNclex-Rn Test Study GuideSusan BensonNo ratings yet
- Nclex Mnemonics 2020 2Document9 pagesNclex Mnemonics 2020 2Winnie OkothNo ratings yet
- NGN Workbook PDFDocument11 pagesNGN Workbook PDFramandeep kaurNo ratings yet
- Ati 2Document10 pagesAti 2KitesaMedeksa100% (6)
- Breaking Down The NCLEX QuestionsDocument2 pagesBreaking Down The NCLEX QuestionsKaloy KamaoNo ratings yet
- Nclex 2Document147 pagesNclex 2Habet Fidem100% (5)
- Medication Work Sheet For MedSurgDocument5 pagesMedication Work Sheet For MedSurgRyanMitchell100% (2)
- Select All That Apply SATADocument58 pagesSelect All That Apply SATANicholas TagleNo ratings yet
- NCLEX RNdemo PDFDocument14 pagesNCLEX RNdemo PDFHarrington KalumbwaNo ratings yet
- Nursing Nclex ExamDocument11 pagesNursing Nclex ExamDenisa Viviana MaroNo ratings yet
- Mind Web Academy - Booster 3Document8 pagesMind Web Academy - Booster 3Charis Gutierrez RodriguezNo ratings yet
- Recently Added NCLEX BooksDocument1 pageRecently Added NCLEX Bookshasan ahmd100% (2)
- The Client Should Be Instructed As Follows: Intravenous Pyelogram (IVP) Is An X-Ray of The Urinary SystemDocument25 pagesThe Client Should Be Instructed As Follows: Intravenous Pyelogram (IVP) Is An X-Ray of The Urinary SystemElizabeth SharmaNo ratings yet
- Procedures, Delegation, and EthicsDocument32 pagesProcedures, Delegation, and Ethicsnene lewisNo ratings yet
- NCLEX Study GuideDocument7 pagesNCLEX Study Guidemmgoodall22100% (3)
- Strategy DefinitionsDocument8 pagesStrategy DefinitionskwameNo ratings yet
- NCLEX Study GuideDocument2 pagesNCLEX Study GuideLogin Nurse100% (1)
- NCLEX2015Document61 pagesNCLEX2015Sara Pirman100% (2)
- Essential care considerations for common pediatric and medical conditionsDocument97 pagesEssential care considerations for common pediatric and medical conditionsMary Aurine FullanteNo ratings yet
- NCLEXstudyguidevmDocument31 pagesNCLEXstudyguidevmAnonymous vqG0paWG100% (1)
- NCLEX Notes : Raynaud's Phenomenon - Cold Temperatures or Strong Emotions CauseDocument10 pagesNCLEX Notes : Raynaud's Phenomenon - Cold Temperatures or Strong Emotions CauseDesi Marian100% (12)
- Key Concepts For An NCLEX-RN Cram SheetDocument3 pagesKey Concepts For An NCLEX-RN Cram Sheetema100% (2)
- Nclex Cheat SheetDocument9 pagesNclex Cheat Sheetsophia onuNo ratings yet
- COPD medications and interventionsDocument34 pagesCOPD medications and interventionssaroberts2202100% (1)
- Gastrointestinal: Nclex-Rn ReviewerDocument34 pagesGastrointestinal: Nclex-Rn ReviewerJohnasse Sebastian NavalNo ratings yet
- Cardiovascular Nursing Bullet Points I PDFDocument4 pagesCardiovascular Nursing Bullet Points I PDFKhalid Epping100% (3)
- The Nclex-Pn Cram Sheet: General Test Information Normal Lab ValuesDocument2 pagesThe Nclex-Pn Cram Sheet: General Test Information Normal Lab Valuesroboat96No ratings yet
- Med Surg BulletDocument12 pagesMed Surg BulletCham SaponNo ratings yet
- NCLEX nursing care plans for common diseasesDocument15 pagesNCLEX nursing care plans for common diseasesdecsag06No ratings yet
- 2pdfnclex ReviewDocument187 pages2pdfnclex ReviewgarvitaNo ratings yet
- Mark Klimek Lecture 4 Canes N CrutchesDocument4 pagesMark Klimek Lecture 4 Canes N CrutchesJohn DesirNo ratings yet
- Nclex Mnemonics.....Document25 pagesNclex Mnemonics.....A. P.100% (1)
- Nclex 2015-2Document57 pagesNclex 2015-2Margo King94% (32)
- NCLEX NotesDocument34 pagesNCLEX Notesyohans TeferiNo ratings yet
- Testing - 2 NclexDocument12 pagesTesting - 2 NclexYoke W KhooNo ratings yet
- Med Surg Notes 3Document6 pagesMed Surg Notes 3Ivy NguyenNo ratings yet
- Nclex Question and Rationale Week 4Document10 pagesNclex Question and Rationale Week 4Winnie Okoth100% (1)
- Nclex GuideDocument3 pagesNclex Guidemichegirl91No ratings yet
- Essential infection prevention guidelines and endocrine disease assessmentsDocument51 pagesEssential infection prevention guidelines and endocrine disease assessmentswhereswaldo007yahooc100% (1)
- Mark K Lecture #2Document16 pagesMark K Lecture #2Melissa Sapp100% (2)
- P and D Study GuideDocument4 pagesP and D Study GuideKenneth Smith II100% (1)
- NCLEXDocument3 pagesNCLEXEternity RealNo ratings yet
- ReMar Nurse University 2020 (VT) Student WorkbookDocument50 pagesReMar Nurse University 2020 (VT) Student WorkbookAnderson AlfredNo ratings yet
- NCLEX Notes: Aortic Aneurysm to Anti-InfectivesDocument83 pagesNCLEX Notes: Aortic Aneurysm to Anti-InfectivesMadora SamuelNo ratings yet
- Rush Prerequisite Courses For MS in PADocument1 pageRush Prerequisite Courses For MS in PANathalee WalkerNo ratings yet
- Running Head: Quality Safety Evaluation of Communication and 1Document7 pagesRunning Head: Quality Safety Evaluation of Communication and 1Nathalee WalkerNo ratings yet
- DelegationDocument3 pagesDelegationNathalee WalkerNo ratings yet
- Running Head: Senior Capstone Reflection 1Document7 pagesRunning Head: Senior Capstone Reflection 1Nathalee WalkerNo ratings yet
- BLS For HCP Student Review 2013Document3 pagesBLS For HCP Student Review 2013Heru SuwardiantoNo ratings yet
- Rush CurriculumDocument2 pagesRush CurriculumNathalee WalkerNo ratings yet
- RN SheetDocument3 pagesRN SheetNathalee WalkerNo ratings yet
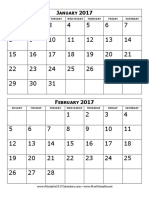
- 2017 Calendar Two Months Per PageDocument6 pages2017 Calendar Two Months Per PageRodica Avadanei-VorniceseiNo ratings yet
- Rush FAQDocument8 pagesRush FAQNathalee WalkerNo ratings yet
- Types of DietDocument1 pageTypes of DietNathalee WalkerNo ratings yet
- Rush PA BrochureDocument2 pagesRush PA BrochureNathalee WalkerNo ratings yet
- Seasons Volunteer InfoDocument7 pagesSeasons Volunteer InfoNathalee WalkerNo ratings yet
- PA School Spreadsheet 2016Document38 pagesPA School Spreadsheet 2016Nathalee WalkerNo ratings yet
- Rosalind Franklin PA CurriculumDocument33 pagesRosalind Franklin PA CurriculumNathalee WalkerNo ratings yet
- Quantitative study sessions and resourcesDocument2 pagesQuantitative study sessions and resourcesNathalee WalkerNo ratings yet
- Rosalind Franklin PA CurriculumDocument33 pagesRosalind Franklin PA CurriculumNathalee WalkerNo ratings yet
- Using Generic NamesDocument2 pagesUsing Generic NamesNathalee WalkerNo ratings yet
- CARDIODocument7 pagesCARDIORizMarie100% (7)
- Sociological Social Update - MEFDocument1 pageSociological Social Update - MEFNathalee WalkerNo ratings yet
- Psychology ArticleDocument9 pagesPsychology ArticleNathalee WalkerNo ratings yet
- Interview QuestionsDocument4 pagesInterview QuestionsNathalee WalkerNo ratings yet
- Interview QuestionsDocument4 pagesInterview QuestionsNathalee WalkerNo ratings yet
- Burns 4Document3 pagesBurns 4Nathalee WalkerNo ratings yet
- Module ExamsDocument166 pagesModule ExamsNathalee WalkerNo ratings yet
- ENDOCRINEDocument5 pagesENDOCRINERizMarie100% (3)
- ACIDDocument2 pagesACIDRizMarie100% (2)
- FINALTHOUGHTSDocument5 pagesFINALTHOUGHTSRizMarieNo ratings yet
- Fluids and ElectrolytesDocument6 pagesFluids and ElectrolytesRizMarie100% (1)
- GASTROINTESTINALDocument5 pagesGASTROINTESTINALRizMarie100% (3)
- STEMI and OMIDocument12 pagesSTEMI and OMIRavindar RaviNo ratings yet
- Is.10905.2.1984 0 PDFDocument58 pagesIs.10905.2.1984 0 PDFGowthaman MaruthamuthuNo ratings yet
- Helping Amy: A Social Worker's Treatment PlanDocument6 pagesHelping Amy: A Social Worker's Treatment PlanAngy ShoogzNo ratings yet
- CS Form No. 212 Revised Personal Data SheetDocument5 pagesCS Form No. 212 Revised Personal Data SheetKim Rose Sabuclalao85% (13)
- Nursing Care PlanDocument15 pagesNursing Care PlanMerfat Abubakar100% (1)
- Asthma Drugs PDFDocument2 pagesAsthma Drugs PDFRahmat PasaribuNo ratings yet
- Adaptations of Multifaceted GenogramDocument10 pagesAdaptations of Multifaceted Genogramvanessa waltersNo ratings yet
- Bolus Feeding in Adults A Practical GuideDocument18 pagesBolus Feeding in Adults A Practical Guideshrutee babraNo ratings yet
- Jawline Definition MovesDocument5 pagesJawline Definition Movesagonza70No ratings yet
- Nanda - Noc - Nic (NNN) : Intervensi KeperawatanDocument39 pagesNanda - Noc - Nic (NNN) : Intervensi KeperawatanChindy Surya KencanabreNo ratings yet
- 1-Safe-Comfortable PlaceDocument2 pages1-Safe-Comfortable Placeapi-273614596No ratings yet
- Pharmacology of Endocrine System-NursingDocument58 pagesPharmacology of Endocrine System-NursingRaveenmayiNo ratings yet
- The Nature of Practice in Evidence-Based PracticeDocument40 pagesThe Nature of Practice in Evidence-Based PracticeJane GilgunNo ratings yet
- Ingle's EndodonticsDocument35 pagesIngle's EndodonticsAndrei AntipinNo ratings yet
- Epilepsy Emergencies - Status Epilepticus, Acute Repetitite Seizures, and Autoimmune EncephalitisDocument23 pagesEpilepsy Emergencies - Status Epilepticus, Acute Repetitite Seizures, and Autoimmune Encephalitisnight.shadowNo ratings yet
- 47 Antimycobacterial DrugsDocument77 pages47 Antimycobacterial DrugsKriziaoumo P. OrpiaNo ratings yet
- Budwig Cancer GuideDocument116 pagesBudwig Cancer GuideStanley ChanNo ratings yet
- Inspired to Raise the Bar: OxyHelp's Superior HBOT TechnologyDocument16 pagesInspired to Raise the Bar: OxyHelp's Superior HBOT TechnologySencer SoyluNo ratings yet
- Psychological Disorders GuideDocument4 pagesPsychological Disorders GuideCarlyn HarfordNo ratings yet
- Riggenbach - CBT ToolboxDocument366 pagesRiggenbach - CBT ToolboxRam V100% (5)
- ImipramineDocument6 pagesImipramineMuhammed Faruk JambazNo ratings yet
- 1st Book Review Guidance and CounsellingDocument8 pages1st Book Review Guidance and CounsellingalabanzasaltheaNo ratings yet
- Managing Deep Caries LesionsDocument5 pagesManaging Deep Caries LesionsEmeka V. ObiNo ratings yet
- Phlebotomy Guidelines and Order of Draw: Specimen Collection ProceduresDocument3 pagesPhlebotomy Guidelines and Order of Draw: Specimen Collection ProceduresJulia Gutierrez PeñaNo ratings yet
- Nursing OncologyDocument208 pagesNursing OncologyfelxhuNo ratings yet
- Systemic Absorption of Topically Administered DrugsDocument8 pagesSystemic Absorption of Topically Administered Drugstaner_soysuren100% (2)
- Inside Product Guide 2011-2012 CentrixDocument36 pagesInside Product Guide 2011-2012 CentrixCentrix Dental RomaniaNo ratings yet
- Retinoblastoma - EyeWikiDocument11 pagesRetinoblastoma - EyeWikimay171989No ratings yet
- How Coffee Enemas WorkDocument1 pageHow Coffee Enemas WorkLeonel RodriguezNo ratings yet
- Stress Management Teaching MSCDocument56 pagesStress Management Teaching MSCSatbir GillNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Recovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyFrom EverandRecovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyRating: 4.5 out of 5 stars4.5/5 (201)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)