Professional Documents
Culture Documents
Ozone in Ostoarthritis
Uploaded by
AhmedSalahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ozone in Ostoarthritis
Uploaded by
AhmedSalahCopyright:
Available Formats
1
The effect of local ozone
injection on knee
osteoarthritis
ESSAY
Submitted to the Naval and Underwater
Institute
Military Medical Academy
In partial fulfillment of the requirements
Of the master degree of the Naval and
Underwater Medicine
By
Colonel Doctor / Ahmed Salah Ahmed
Abdel Aal
/
MBBH
Faculty of Medicine
Alexandria University
The Naval and Underwater Medicine Institute
Military Medical Academy
2014
Supervisors
Prof. Dr. / Diaa F. Mohaseb /
Chairman of Physical Medicine
Rheumatology and Rehabilitation Department
Faculty of Medicine
Alexandria University
Commodore Dr. / Ehab Elsayed Kamel /
President of the Naval
Hyperbaric Institute
Naval Forces
Commodore Dr. / Khalid Mahrous Salem /
Consultant of Orthopedic Surgery
The Armed Forces
Acknowledgment
I wish to express my deepest thanks, greatest
appreciation and gratitude to Professor / Diaa
Fahmy Mohaseb, Chairman of Physical medicine,
Rheumatology and Rehabilitation, Faculty of
Medicine for his unlimited help.
I wish to express my deepest thanks and greatest
appreciation to Commodore Doctor / Ehab Elsayed
Kamel, Chairman of Naval Hyperbaric Medicine
Institute for his magnificent support and
supervision.
I wish to express my deepest thanks and greatest
gratitude to Commodore Doctor / Khalid Mahrous
Salem, the Military Orthopedic Consultant, for his
extra-ordinary unlimited help.
I wish to express my deepest thanks to my
superiors Professor Dr. / Ziad Fahmy , Admiral
doctor/ Hani Salah , Admiral doctor
/ Ahmed Fathy and Admiral Doctor/ Khalid Eltobgy
for their unlimited help and support.
Lastly, I wish to express my deepest thanks to all
doctors, nurses, officers and members of NHMI for
the kind and help
Index
N
o
1
2
3
4
5
6
7
8
9
1
0
1
1
1
2
1
3
1
4
Subject
Index of figures
Index of tables
Introduction
What is ozone?
Physical and chemical properties of ozone
Is ozone toxic?
Generation of ozone
How does ozone act?
Administration of ozone
Side effects of ozone
Pag
e
5
6
7
7
9
10
11
15
19
22
Osteoarthritis
29
Causes of osteoarthritis
30
Classification of osteoarthritis
32
Pathophysiology of osteoarthritis
33
1
5
1
6
1
7
1
8
1
9
2
0
2
1
2
2
2
3
2
4
2
5
2
6
2
7
2
8
2
9
3
0
3
1
3
2
3
3
3
Is osteoarthritis a process of cartilage aging?
34
Molecules responsible for degrading cartilage
35
Risk factors of osteoarthritis
38
Clinical picture of osteoarthritis
40
Grading of osteoarthritis
43
Differential diagnosis of osteoarthritis
45
Treatment of osteoarthritis
47
Rheumatoid arthritis
55
Clinical picture of rheumatoid arthritis
58
Causes of rheumatoid arthritis
63
Pathophysiology of rheumatoid arthritis
64
Phases of rheumatoid arthritis
65
Diagnosis of rheumatoid arthritis
66
Criteria of rheumatoid arthritis
68
Differential diagnosis of rheumatoid arthritis
70
Management of rheumatoid arthritis
73
Intra-articular ozone injection in knee joint
82
Clinical experience
87
Recommendation
91
References
92
4
3
5
103
Index for Figure
12
13
13
14
14
4
5
15
18
19
20
21
21
22
22
31
31
8
9
10
11
12
13
14
15
41
42
42
43
16
17
18
19
45
46
20
21
The mechanism for ozone
generation
The mechanism for ozone
generation
Medical Ozone Equipment Generator
model 20134
Longevity EXT120-T Ozone Generator
Votex Model SST1 Medical Ozone
Generator
Ozonosan photonik plus ozone
generator
Variable mechanisms of ozone
actions
Benefits of ozone use
Intra-articular ozone injection
Local ozone bag
Local ozone bag
Preparation of ozonated water
Major autohemotherapy
Normal anatomy of knee joint
Different pathological changes
occurring in O.A
Stages of knee osteoarthritis
Plain x ray early O.A knee joint
Plain x ray late O.A knee joint
Plain x ray of pathological changes
O.A knee
Anatomical changes in O.A knee
Pathological changes in RA and OA
50
22
57
57
62
62
23
24
25
26
69
27
70
28
72
29
72
30
knee
Ozone intra-articular injection
knee joint
Common joints affected by R.A
Common joints affected by R.A
Characters of rheumatoid arthritis
Effects of rheumatoid arthritis on
different organs
Plain x ray rheumatoid arthritis
right hand
Rheumatoid arthritis ulnar
deviation
Plain x ray rheumatoid arthritis
knee joint
Rheumatoid arthritis knee joint
deformity
Index for Tables
page
24
Table
numbe
r
1
25 ,26
,27
28
Table name
Different indications of
ozone use
Different methods of ozone
applications and their
indications
Contraindications of
systemic ozone applications
78
79
80
81
Comparison between OA ,
RA , OP risk factors
Comparison between OA ,
RA , OP physical effects
Comparison between OA ,
RA , OP treatment options
Comparison between OA ,
RA , OP pain management
Introduction
What is ozone?
Ozone (from the Greek means to give off a smell) is an
alternate version of oxygen. Oxygen in the air we breathe
is actually two molecules of oxygen attached together, or
O2. Ozone is an activated form of oxygen where there
are actually three atoms of oxygen attached together,
forming a molecule that is O3. Ozone (O3) behaves
completely
differently
than
O2.
Ozone
is
far more energetic and oxidative than Oxygen, which is
what makes it so valuable to us for so many applications,
such as Air Purification, Water Purification, and Medical
Ozone Therapy Applications. (1, 2)
Historical Notes
Christian Friedrich Schonbein (17991868) discovered
ozone in 1840, when working with a voltaic pile in the
presence of oxygen, he noticed the emergence of a gas
with an electric and pungent smell that could be a sort
of super-active oxygen". We can smell it during a
thunderstorm because the electric discharge of lightning
between the clouds and the earth, catalyses the formation
of ozone from atmospheric oxygen. Although Schonbein
had probably guessed that ozone could be used as
disinfectant, his discovery did not save him when he
contacted a Bacillus anthrax infection while exploring a
chemical method for preserving meat. The concept that
ozone derives from oxygen when an electric discharge was
generated by a voltaic arc was practically applied by the
chemist Werner von Siemens, who invented the so called
super-induction tube (Siemenss tube), consisting of two
interposed electrode plates set at a high voltage which, in
the presence of oxygen, could generate some ozone. It
became possible to produce ozone at will and clarify that
ozone is indeed a very reactive, unstable and unstorable
gas that had to be produced instantly from oxygen and
used at once. Industrial ozone generators could then be
used for industrial application and disinfection of water,
after it was shown the potent and broad bactericidal
activity of ozone. Today nobody doubts about its strong
disinfectant properties and there are more than 3,000
municipal treatment facilities in the world. As the need of
water increases daily and it is indispensable to prevent the
spread of infectious diseases, the importance of ozone for
practical applications becomes immense. (3, 4)
10
The International Ozone Association (IOA) carefully
supervises all the applications and publishes a scientific
journal Ozone Science and Engineering. So far, one weak
point has been not to pay enough attention to the medical
applications because this is not IOAs main purpose.
The first medical application seems to have been the use
of ozone for treating gaseous, post-traumatic gangrene in
German soldiers during the 1st world war.
However a big step forward was the invention of a reliable
ozoniser for medical use by the physicist Joachim Hansler
(19081981).
The idea to use ozone in medicine developed slowly
during the last century and it was stimulated by the lack
of antibiotics and the disinfectant properties of ozone.
Not surprisingly a Swiss dentist, E.A. Fisch (18991966)
was the first to use ozone in his practice. By a twist of
fate, Dr. E. Payr (18711946), a surgeon had to be treated
for a gangrenous pulpit and soon realized the efficacy of
the ozone treatment in surgery to become so enthusiastic
to report his results at the 59th Congress of the German
Surgical Society in Berlin (1935) and wrote:
which
other disinfectant would be tolerated better than ozone?
The positive results in 75% of patients, the simplicity, the
hygienic conditions and inequity of the method are some
of the many advantages.
In 1936, in France, Dr. P. Aubourg proposed to use the
insufation of oxygen- ozone into the rectum to treat
chronic colitis and fistulae. How could ozone be
administered for internal use? It seems that Dr. Payr was
the first to inject gas with a small glass syringe directly
into the vein but he was very careful in slowly delivering a
small volume of gas. Unfortunately this route was later on
adopted by charlatans and technicians without any
medical qualification who, by injecting large volume (up to
11
500 ml in 2 h) have often caused lung embolism mostly
due to oxygen and even death. (5)
Although this practice has been prohibited since 1984,
some cosmetic workers still use it in third-world countries
and certainly it represents one good reason for prohibiting
all at once the use of ozone.
In most States of USA, the FDA has forbidden the use of
ozone and this fact has negatively inuenced a correct
development of ozone therapy that, however, is more or
less tolerated in other parts of the world. It is regretful that
brilliant pioneers as Fisch, Payr, Aubourg and Dr. H. Wolff
(19271980), the inventor of ozonated auto-hemotherapy,
have been betrayed by a horde of unscrupulous and false
doctors.
If
that
was
not enough, another serious obstacle has been created in
the USA by the ruling dogma that ozone is always toxic
any way you deal with it. This was the phrase that one of
the best ozone chemists wrote in 1995.
It is well known nowadays that the use of the correct
doses of ozone will be tolerated by the anti-oxidant
system of the body to achieve the preferable affects of
ozone therapy and avoid its toxic effects. (6)
Physical and chemical Properties of Ozone
Ozone is a natural but unstable molecule. The pure gas
has a soft sky-blue color with a pungent, acrid smell. The
molecule is composed of three oxygen atoms (O3) and,
the molecular weight, in comparison to the oxygen
diatomic molecule (32.00) is of 48.00.Ozonehas a cyclical
structure with a distance among oxygen atoms of 1.26
and exists in several states in dynamic equilibrium. (7)
It has 10 folds higher solubility in water than oxygen.
This greater solubility of ozone in water allows its
immediate reaction with any soluble compounds and
biomolecules present in biological uids.
12
It is believed that during ozone generation, a trace of
singlet oxygen (O) may be formed but again its practical
(8)
significance
remains
negligible.
Among oxidant agents, ozone is the third strongest, after
uorine and persulphate, a fact that explains its high
reactivity.
Ozone is formed from pure oxygen via an endothermic
process allowed by very high voltage gradients set up
between the electrodes of the Siemens tube: "3 O2 +
68,400 cal 2 O3"
This reaction is reversible, so O3 decomposes to O2 within
20 to 25 minutes according to temperature as it
decomposes faster in hot weather. This shows the
instability of the O3 molecule and how hard to store it. (9, 10)
Is Ozone toxic?
The dogma that Ozone is toxic depends on the effect of
Ozone on the lungs ,eyes ,nose and ,to a lesser extent, the
skin because particularly the respiratory mucosa does not
contain enough neutralizing substances for this murderous
acid mixture .Indeed the respiratory tract lining uids
(RTLFs), that amounts to only 2040 ml dispersed as an
aqueous film layer over the alveolar space of about 70m2
is easily overwhelmed by this acidic mixture of strong
oxidants .Particularly children ,asthmatic and other
broncho-pulmonary patients are at risk and the ozone . (11)
The chaotic human activities such as industrial processes,
vehicular traffic have led to a dangerous environmental
pollution of the air present in the troposphere, which
extends 817 km from the earths surface. Exaggerated
anthropogenic emissions of nitrogen monoxide (NO) and
13
dioxide (NO2), of carbon monoxide (CO), of methane
(CH4), sulphuric acid and other acid compounds have
favored an almost intolerable increase of ozone
concentration up to 0.3 mcg/l or more. This excessively
high Ozone concentration is toxic to the mucous lining of
the upper respiratory tract and eye conjunctiva. Although,
lower concentrations of Ozone show lesser effect on these
systems while produce highly beneficial effects on other
target organs. (12, 13)
How
Ozone
Is
Generated
Concentrations Measured?
and
Its
Owing to ozone instability, it needs to be generated only
when needed and used at once. Generation of ozone can
be achieved by:
(1)UV radiation
(2) An electrochemical process
(3) By corona discharge
It must be noted that the first two methods yield a low
ozone output and a poor regulation of production .The
ozone therapist must have an ozone generator that is
safe, atoxic and reproducible. The instrument must be
built with the best ozone-resistant materials, such as Inox
316 L, stainless steel, pure titanium grade2, Pyrex glass,
Teon, Viton and polyurethane avoiding any material that
could be released due to ozone oxidation. It is strongly
suggested to purchase only a generator that allows to
measure in real time the ozone concentration by mean of
a reliable photometer .Unused ozone cannot be dispersed
14
into the environment and it must be decomposed to
oxygen by catalytic reaction inside the indispensable
destructor that contains heavy metal oxides maintained
at about +70 .(14)
The medical ozone generator consists of 24 high voltage
tubes connected in series to an electronic programme
able to set up voltage differences between 4,000 and
13,000 V .In the corona discharge ozonator, the ozone is
formed when oxygen passes through a gap between high
voltage and ground electrodes to create energy in the
denominated corona. The energy from the electric
discharge allows the breakdown of oxygen molecules into
oxygen atoms which, in the presence of an excess of
oxygen molecules, form the three-atom ozone molecule
.The generator is fed with pure medical oxygen and, at
the supply nozzle, a gas mixture composed of no more
than 5% ozone and 95% oxygen can be collected at a
slightly positive pressure. The synthesis of ozone is
allowed by the energy released by the electric discharge
while the decomposition of ozone is accompanied by
energy release. For medical purposes, air cannot be used
because, by containing 78% nitrogen, the final gas
mixture will contain, beside oxygen and ozone, a variable
amount of highly toxic NOx (NO, NO2). (14)
The ozone concentration
parameters:
1. The Voltage:
is
determined
by
three
The final ozone concentration increases with the voltage,
although in a non-proportional manner.
2. The space between the electrodes:
This serves to modulate a gradual increase of the ozone
concentration.
3. The Oxygen flow:
15
This is expressed as a volume of liters per minute (l/min)
and normally can be regulated from 1 up to about 10
l/min. The final ozone concentration is inversely
proportional to the oxygen ow; hence, per time unit, the
higher the oxygen ow, the lower the ozone
concentration. (15)
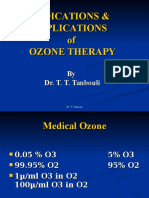
Figure (1) the Mechanism of Ozone Generation
16
Figure (2) The Mechanism of Ozone Generator
Figure (3) Medical Ozone Equipment Generator
model 20134
17
Figure (4) Longevity EXT120-T Ozone Generator
Figure (5) Votex Model SST1 Medical Ozone
Generator
18
Figure (6) Ozonosan photonik plus ozone
generator
The criteria for calculating the ozone dose
are
the
following:
(A) Total volume of the gas mixture composed of oxygen
and
ozone.
(B) Ozone concentration, expressed as micrograms per
ml
(mcg/ml).
(C) Barometric pressure (mmHg), if different from
normal.
For safety reasons we must avoid
hyperbaric pressure.
So, The Total Ozone Dose Is Equivalent to the Gas Volume
(ml)
multiplied by the Ozone Concentration (mcg/ml) (15)
How Does Ozone Act?
The administration of ozone causes a number of
biochemical,
pharmacological
and
psycho-neuroimmunological reactions to take place in a patient who is
an essential part of the process .Although oxygen
represents the bulk (9598%) of the gas mixture, by
considering the enormous dilution of the small reinfused
19
oxygenated-ozonated blood with venous blood, it has a
negligible role. While, only thanks to oxygen we can live
,this gas has a negative effect on the long run because
cell respiration allows the formation of reactive oxygen
species (ROS), among which, hydroxyl radical (OH ) is
one of the most destructive radical compounds for
precious enzymes and DNA.(16)
At rest, a human being produces about 5 g of anion
superoxide (O2), which is the father of several radical
molecules.
Anion superoxide is physiologically produced in the
mitochondria, from Complex I and II but other ROS, such
as hydrogen peroxide, hypochloric acid and nitric oxide
are continuously generated by various oxidases and
myeloperoxidase and, in trace amounts, have a crucial
defensive role against pathogens. On the other hand
almost everyone knows that during ageing, the metabolic
disorders (atherosclerosis, diabetes, cell degeneration)
can be worsened by an excessive production of ROS and,
only in part, we can prevent their damageable effects.
Ironically, even the partial lack of oxygen (hypoxia),
observed in ischemic vascular diseases, and represents
the cause of death due to limb ischemia, heart infarction
and stroke. Moreover, hypoxia enhances neoplastic
metastasis and ultimately leads to death.
Ozone (synthesized in the stratosphere to protect against
UV radiation) can be produced with a medical
generator .ozone is one of the most potent oxidants (third
in the chemical scale).so, it is so important to distinguish
the therapeutic from the toxic dose. (17)
First of all, ozone, as any other gas, readily dissolves in
the water either of the plasma (the liquid part of blood),
or into the extracellular uids, or into the thin layer of
water covering the skin and particularly the mucosa of
the respiratory tract, gut, vagina, and other organs.
20
At normal temperature and atmospheric pressure, owing
to its high solubility and depending upon its relative
pressure, ozone dissolves into the water but, unlike
oxygen, does not equilibrate with the ozone remaining in
the gas phase. This happens because ozone, being a
potent oxidant, reacts immediately with a number of ions
and biomolecules present in biological uids, namely
antioxidants, proteins, carbohydrates and preferentially,
polyunsaturated fatty acids (PUFAs) bound to albumin. In
fact phospholipids and cholesterol present either in cell
membranes or/and lipoproteins are shielded by
antioxidants and albumin molecules.
The reaction of ozone with so many molecules implies
several fundamental processes occurring at the same
time: some of the ozone dose is unavoidably consumed
during oxidation of ascorbic and uric acids, sulphydryl
(SH)-groups of GSH, proteins and glycoproteins present in
the water of plasma .The other fundamental and well
characterized reaction is known as Lipid Peroxidation. In
the hydrophilic plasma environment, one mole of an
unsaturated
olefin
(particularly
arachidonic
acid
transported by albumin or present in plasma triglycerides
and chylomicrons) and one mole of ozone give rise to two
moles of aldehydes and one mole of hydrogen peroxide
(H2O2). In the next few minutes,
Ozone Is Exhausted
and Only ROS (Mostly Hydrogen Peroxide) and LOPs are
Responsible for the Successive and Multiple Biochemical
Reactions Happening in Different Cells All over the Body.
(18)
So, some of ozone dose is neutralized by the antioxidants
present in plasma and only the reaction with PUFA is
responsible for the biological and therapeutic effects. ROS
are responsible for what is called as the early phase
reactions while LOPs are responsible for the late ones. The
pharmacodynamics of Hydrogen Peroxide (H2O2) which is
the most important member of ROS shows that as soon as
21
ozone dissolves in the plasmatic water and reacts with
PUFAs, the concentration of H2O2 rapidly increases then
decreases because the unionized molecule diffuses
quickly into erythrocytes, leukocytes and platelets. As
soon as H2O2 enters the cells, it undergoes reduction to
water in the intracellular uid with the presence of
powerful antioxidant enzymes such as catalase,
glutathione perioxidase and free reduced glutathione.
H2O2 is recognized as an intracellular signaling molecule
able to activate a tyrosine kinase which phosphrylates a
transcription factors (KB, NFKB) which allows the
synthesis of different types of proteins. This critical step
corresponds to a controlled ,acute and transient oxidative
stress necessary for biological activation, without
concomitant toxicity, provided that the ozone dose is
compatible with the blood antioxidant capacity .While
ROS are responsible for immediate biological effects ,LOPs
are important as late effectors, when the blood returns
into the circulation upon reinfusion. LOPs can reach any
organ, particularly the bone marrow where, after binding
to receptors in submicromolar concentrations, elicit the
adaptation to the repeated acute oxidative stress, which
is the hallmark of ozonated autohemotherapy. Upon
prolonged therapy, LOPs activity will culminate in the up
regulation of antioxidant enzymes, appearance of
oxidative stress proteins (haemo- oxygenase I as a typical
marker) and probable release of stem cells, which
represent crucial factors explaining some of the
(19)
extraordinary
effects
of
ozone
therapy.
.
It must be emphasized that blood exposed to ozone
undergoes a transitory oxidative stress absolutely
necessary to activate biological functions without
detrimental effects. The stress must be adequate (not
subliminal) to activate physiological mechanisms, but not
excessive to overwhelm the intracellular antioxidant
22
system and cause damage. Thus, an excessive ozone
dose (>160 mcg/ml gas per ml of blood) or incompetence
in manipulating this gas can be deleterious. On the other
hand, very low ozone doses (below the threshold), are
fully neutralized by the wealth of plasma antioxidants and
can produce only a placebo effect. (20)
.
The concept that ozone therapy is endowed with an
acute oxidative stress bothers the opponents of this
approach because they consider it as a damage inicted
to the patients, possibly already under a chronic oxidative
stress. Moreover .The therapeutic response achieved after
these repeated oxidative stresses can be envisaged as a
preconditioning effect eventually able to re equilibrate the
redox system altered by pathogenetic stimuli. (21)
Figure (7) Variable Mechanisms of Ozone Action
23
Figure (8) Benefits of Ozone Use
How is ozone administrated?
Except for the inhalation route (prohibited by tracheobronchial-pulmonary toxicity), many parenteral and
topical routes are used to administer ozone without toxic
effects and minimal discomfort.
Ozone can be administrated both through systemic and
local routes.
Systemic use of ozone includes:
Major ozone autohemotherapy.
Minor ozone autohemotherapy.
Rectal insufflations.
Quasi total body exposure to ozone-oxygen (sauna).
Local ozone use can be through
Ozone bags.
Intra-lesional injection.
Ozone cream.
24
Ozonated water fomentation.
Inter-articular injection.
The central aim of ozone therapy is to give a precise,
atoxic shock to an organ which for various reasons has
gone astray; the hope is that repeated ,timely shocks will
readjust several biological functions by means of many
messengers (ROS, LOPs and autacoids generated by
ozone) delivered by circulating blood to the whole body.
(21,22)
Figure (9) Intra-articular Injection of Ozone
25
Figure (10) Local Ozone Bag (one leg)
Figure (11) Local Ozone Bag (both legs)
26
Figure (12) Preparation of Ozonated Water
Figure (13) Major Autohemotherapy
The potential toxicity of ozone therapy:
Side effects and contraindications
As other medical approaches using potent drugs, ozone
therapy may present some risks, which can be avoided if
the ozone therapist is theoretically and practically well
prepared. The use of judicious ozone doses related to the
antioxidant capacity of tissues and body uids excludes
the risk of Citotoxicity and mutagenicity .Adverse effects,
noted with the use of PVC bags and an excess of citrate,
are now totally avoided with the use of the optimized
method using ozone-resistant glass bottles .Great care
must be exercised when injecting the gas mixture directly
into the Para-vertebral muscles: if this is done correctly,
27
most patients comply well with the therapy. There are a
few cases when ozone therapy is contraindicated and,
whenever possible, we must follow the patients during
subsequent years and note any possible toxicity or new
pathologies. (23, 24)
Contraindications of ozone therapy include:
A patient with a significant deficiency of G-6PD. Favism
is a hemolytic disease observed in some people lacking
the enzyme. This enzyme provides crucial reducing
equivalents able to abolish excessive oxidation and
intensive hemolysis
Pregnancy, particularly the early phase, to exclude any
mutagenic risk, although it is unlikely.
Patients being treated with ACE inhibitors.
Abnormal
situations
with
hyperthyroidism,
thrombocytopenia
and
serious
cardio-vascular
instability.
Allergy to ozone(25)
28
indications
Underlying effects
1. Arterial Circulatory
disorders
O2-release effect
Activation of
RBC metabolism
2. External Ulcer and
skin lesions
Disinfection
Wound cleansing
improved wound
healing
3. Pathological
intestinal conditions
colitis
Proctatitis
Disinfection
Immune activation
anti-inammatory
processes
fistulas
4. Infections
and virus caused
diseases
Immune modulation
5. Additive therapy in
carcinogenic conditions
Immune activation
6. Geriatric conditions
O2-release effect
Immune- and enzyme
29
activation
7. Rheumatic diseases
inammatory
conditions
degenerative
conditions
8. Dentistry
anti-inammatory
processes
Activation of
antioxidative capacity
Immune modulation
Disinfection
Wound cleansing
improved wound
healing
Table (1) Different Indications of Ozone
applications
Indication
Mechanism
of action
1. Systemic applications
Arterial
circulatory
disorders
Major
autohemotherapy
as an
extracorporeal
Activation of
red blood cell
metabolism
with increase
of 2,3-DPG
and ATP plus
resultant
30
blood treatment
and intravenous
reinfusion of the
patients own
blood.
improvement
in O2-release
Infections,
Immune
activation,
additive
therapy in
carcinoma
patients,
geriatric field
Activation of
immunocomp
etent cells
with release
of cytokines,
such as
Interferon and
Interleukins.
Modulation of
immune
system with
increase of
IFN-, TGF-
Rheumatic
arthritis
Rectal insufflation
Arterial
circulatory
disorders
(stage II)
general
Immune
activation,
Increase of
the
antioxidative
capacity by
activation of
SOD, GSHPx,
Catalase ...
see above
31
adjuvant
cancer
therapy.
Hepatitis
A,B,C
Minor
autohemotherapy
as extracorporeal
blood treatment
and intramuscular
injection.
Allergies,
acne,
furunculosis.
Adjuvant
cancer
therapy.
Non-specific
activation of
the immunesystem
general
stimulation.
2. Topical application
Transcutanous gas
bath in ozone
resistant plastic
bag
Low-pressure
application with
suction cup or in
Ulcus cruris;
dermatosis,
fungus
infections
Microbicidal
effect of
ozone:
bactericidal,
fungicidal,
virus
inactivating
effect
Decubitus,
diabetic
gangrene
badly healing
wounds,
fistulas,
wound
cleansing
improved
wound
healing
Immune
32
plastic boot
radiation
damage
activation
(TGF-)
Proctatitis;
colitis
Antiinammatory
effect,
better O2supply,
wound
healing effect
e.g. Candida
infection
fungicidal
effect
Rheumatoid
arthritis,
Knee
arthritis,
Gonarthrosis;
traumatic
knee
disorders
antiammator
y effect,
activation of
SOD as
radical
scavenger,
activation of
immunocomp
etent and
cartilage
cells,
release of
TGF-
Rectal Insufflation
Vaginal
Insufflation
Intra-articular
injection (mainly
knee and
shoulder)
"Blistering"
paravertebral
injection and
intramuscular
injections (in
combination with
tonanalgetic
Myotraumati
c syndrome,
myogelosis,
trigger points
Activation of
cell
metabolism,
ATP-increase
Activation of
33
treatment)
Ozonized water as
spray or
compresses
drop wise
application
Ozonized water as
spray,
or rinsing with O3water
Topical treatment
antioxidants
fresh lesions,
burns,
fungus
infections,
herpes
Wound
cleansing,
antiinammatory
effects,
activation of
cell
metabolism,
Immune
activation
(TGF-)
Otitis
Immune
activation
(TGF-)
Dental
medicine:
following
tooth
extractions,
buccal
infections
(e.g.
Candida)
parodontosis
Disinfection,
wound
healing effect,
see above.
Fungus
infections,
bacterial
infections,
burns, skin
Fungicidal
and
bactericidal
effect,
wound
34
lesions.
healing.
Contraindications
"Contra applications"
Thyrotoxicosis or
hyperthyroidism
Glucose-6-PhosphateDehydrogenasedeficiency (Favism)
Direct gas injections:
intravenous injections:
strictly prohibited.
intra-arterial injections
(arterial femoralis): not
rejected on very special
conditions
Table (2) Different Method of Ozone Applications and their
Indications
Table (3) Contraindications of Systemic Ozone Application
35
Osteoarthritis
Definition:
Osteoarthritis (OA) also known as degenerative arthritis
or degenerative
joint disease or osteoarthrosis, is a
group of mechanical abnormalities involving degradation
of joints, including articular
cartilage and subchondral
bone.
Osteoarthritis is the most common form of arthritis,
affecting millions of people around the world. Often called
wear-and-tear arthritis, osteoarthritis occurs when the
protective cartilage on the ends of bones wears down over
.time
While osteoarthritis can damage any joint in the body, the
disorder most commonly affects joints in hands, neck,
.lower back, knees and hips
Osteoarthritis gradually worsens with time, and no cure
exists. But osteoarthritis treatments can slow the
progression of the disease, relieve pain and improve joint
function. (26)
Etymology
OA is derived from the Greek word part osteo-, meaning
"of the bone", combined with arthritis: arthr-, meaning
"joint", and -itis, the meaning of which has come to be
associated with inammation. The -itis of OA could be
36
considered misleading as inammation is not a
conspicuous feature. Some clinicians refer to this condition
as osteoarthrosis to signify the lack of inammatory
response. (26)
Epidemiology
Globally approximately 250 million people have
osteoarthritis of the knee (3.6% of the population). OA
affects nearly 27 million people in the United States,
accounting for 25% of visits to primary care physicians,
and half of all NSAID prescriptions. It is estimated that
80% of the population have radiographic evidence of OA
by
age65,
although
only
60%
of
those
will
have symptoms. In the United States, hospitalizations for
.OA increased from 322,000 in 1993 to 735,000 in 2006
As of 2004, OA globally causes moderate to severe
.disability in 43.4 million people
In the United States, there were approximately 964,000
hospitalizations for osteoarthritis in 2011, a rate of 31
stays per 10,000 populations. It was the second-most
expensive condition seen in U.S. hospital stays in 2011. By
payer, it was the second-most costly condition billed to
Medicare and private insurance. (27)
What causes osteoarthritis?
Primary osteoarthritis, osteoarthritis not resulting from
injury or disease, is mostly a result of natural aging of the
joint. With aging, the water content of the cartilage
decreases, and the protein component of cartilage
degenerates. Eventually, cartilage begins to degenerate
by aking or forming tiny crevasses. In advanced
osteoarthritis, there is a total loss of the cartilage cushion
between the bones of the joints. Repetitive use of the
worn joints over the years can irritate and iname the
37
cartilage, causing joint pain and swelling. Loss of the
cartilage cushion causes friction between the bones,
leading to pain and limitation of joint mobility.
Inammation of the cartilage can also stimulate new bone
outgrowths (spurs, also referred to as osteophytes) to form
around the joints. Osteoarthritis occasionally can develop
in multiple members of the same family, implying a
hereditary (genetic) basis for this condition.
Secondary osteoarthritis is a form of osteoarthritis that is
caused by another disease or condition. Conditions that
can lead to secondary osteoarthritis include obesity,
repeated trauma or surgery to the joint structures,
abnormal
joints
at
birth
(congenital
abnormalities), gout, diabetes,
and
other
hormone
.disorders
Obesity causes osteoarthritis by increasing the mechanical
stress on the joint and therefore on the cartilage. In fact,
next to aging, obesity is the most significant risk factor for
osteoarthritis of the knees. The early development of
osteoarthritis of the knees among weight lifters is believed
to be in part due to their high body weight. Repeated
trauma to joint tissues (ligaments, bones, and cartilage) is
believed to lead to early osteoarthritis of the knees in
soccer players and army military personnel. Interestingly,
studies have not found an increased risk of osteoarthritis
in long-distance runners. (28)
Crystal deposits in the cartilage can cause cartilage
degeneration and osteoarthritis. Uric acid crystals cause
arthritis in gout, while calcium pyrophosphate crystals
cause arthritis in pseudo-gout. (29)
Some people are born with abnormally formed joints
(congenital abnormalities) that are vulnerable to
mechanical wear, causing early degeneration and loss of
joint cartilage. Osteoarthritis of the hip joints is commonly
related to structural abnormalities of these joints that had
.been present since birth
38
Hormone disturbances, such as diabetes and growth
hormone disorders, are also associated with early cartilage
wear and secondary osteoarthritis. (29)
Figure (14) Normal Anatomy of Knee Joint
Figure (15) Different Pathological Changes
Occurring in Osteoarthritis
Classification of osteoarthritis
Primary (1
A number of studies have shown that there is a greater
prevalence
of
the
disease
among siblings and
39
especially identical
twins,
indicating
a
hereditary
basis. Although a single factor is not generally sufficient to
cause the disease, about half of the variation in
.susceptibility has been assigned to genetic factors
As early human ancestors evolved into bipeds, changes
occurred in the pelvis, hip joint and spine which increased
the risk of osteoarthritis. Additionally genetic variations
that increase the risk were likely not selected against
because usually problems only occur after reproductive
.success
The development of OA is correlated with a history of
previous joint injury and with obesity, especially with
respect to knees. Since the correlation with obesity has
been observed not only for knees but also for non-weight
bearing joints and the loss of body fat is more closely
related to symptom relief than the loss of body weight, it
has been suggested that there may be a metabolic link to
.body fat as opposed to just mechanical loading
Changes in sex hormone levels may play a role in the
development of OA as it is more prevalent among postmenopausal women than among men of the same age. A
study of mice found natural female hormones to be
protective
while
injections
of
the
male
.hormone dihydrotestosterone reduced protection
:Secondary (2
As a result of certain disorders which lead to same
:pathology as OA. These include
Alkaptonuria.
Congenital disorders of joints
Diabetes Mellitus.
Ehlers-Danlos Syndrome
40
Hemochromatosis and Wilson's disease
Inammatory diseases such as Perthes' disease and
Lyme disease)
All chronic forms of arthritis as costochondritis , gout
and rheumatoid arthritis. In gout, uric acid crystals
cause the cartilage to degenerate at a faster pace.
Injury to joints or ligaments (such as the ACL), as a
result of an accident or orthopedic operations.
Ligamentous deterioration or instability may be a
factor.
Marfan syndrome
Obesity
Septic arthritis (infection of a joint)(29)
What causes osteoarthritis?
Primary osteoarthritis, osteoarthritis not resulting from
injury or disease, is mostly a result of natural aging of the
joint. With aging, the water content of the cartilage
increases,
and
the protein makeup
of
cartilage
degenerates. Eventually, cartilage begins to degenerate
by aking or forming tiny crevasses. In advanced
osteoarthritis, there is a total loss of the cartilage cushion
between the bones of the joints. Repetitive use of the
worn joints over the years can irritate and iname the
cartilage, causing joint pain and swelling. Loss of the
cartilage cushion causes friction between the bones,
leading to pain and limitation of joint mobility.
Inammation of the cartilage can also stimulate new bone
outgrowths (spurs, also referred to as osteophytes) to form
around the joints. Osteoarthritis occasionally can develop
41
in multiple members of the same family, implying a
hereditary (genetic) basis for this condition. (30)
Pathophysiology of osteoarthritis
While OA is a degenerative joint disease that may cause
gross cartilage loss and morphological damage to other
joint tissues, more subtle biochemical changes occur in
the earliest stages of OA progression. The water content
of healthy cartilage is finely balanced by compressive
force driving water out & swelling pressure drawing water
in. Collagen fibers exert the compressive force, whereas
the GibbsDonnan effect & cartilage proteoglycans create
osmotic pressure which tends to draw water in. However
during onset of OA, the collagen matrix becomes more
disorganized and there is a decrease in proteoglycan
content within cartilage. The breakdown of collagen fibers
results in a net increase in water content. This increase
occurs because whilst there is an overall loss of
proteoglycans (and thus a decreased osmotic pull), it is
outweighed by a loss of collagen. Without the protective
effects of the proteoglycans, the collagen fibers of the
cartilage can become susceptible to degradation and thus
exacerbate
the
degeneration. Inammation of
the
surrounding joint capsule can also occur, though often
mild (compared to what occurs in rheumatoid arthritis).
This can happen as breakdown products from the cartilage
are released into the synovial space, and the cells lining
the joint attempt to remove them. New bone outgrowths,
called "spurs" or osteophytes, can form on the margins of
the joints, possibly in an attempt to improve the
congruence of the articular cartilage surfaces. These bone
changes, together with the inammation, can be both
painful and debilitating. (31)
?Is OA a primary disease of cartilage
Cartilage is
compressive
a unique
properties
tissue
which
with viscoelastic and
are imparted by its
42
extracellular matrix, composed predominantly of type
IIcollagen and proteoglycans. (32)
Constituents of cartilage
% Cellular : chondrocytes 1-2
-1
% Liquid phase : 70 - 80
-2
% Solid phase : 20 30
-3
It is formed from two main constituents which are
type 2 collagen and proteoglycans mainly aggrecan
Under normal conditions, this matrix is subjected to a
dynamic remodeling process in which low levels of
degradative and synthetic enzyme activities are balanced,
such that the volume of cartilage is maintained. In OA
cartilage, however, matrix degrading enzymes are over
expressed, shifting this balance in favor of net
degradation, with resultant loss of collagen and
.proteoglycans from the matrix
Presumably in response to this loss, chondrocytes initially
proliferate and synthesize enhanced amounts of
proteoglycan and collagen molecules. As the disease
progresses, however, reparative attempts are outmatched
by progressive cartilage degradation. Fibrillation, erosion
and cracking initially appear in the superficial layer of
cartilage and progress over time to deeper layers,
resulting eventually in large clinically observable erosions.
OA, in simplistic terms, therefore, can be thought of as a
process of progressive cartilage matrix degradation to
which an ineffectual attempt at repair is made. (33)
?Is OA simply a process of aging cartilage
A critical question is whether OA is truly a disease or a
natural consequence of aging. Several differences
between aging cartilage and OA cartilage have been
43
described, suggesting the former. For example, although
denatured type II collagen is found in both normal aging
and OA cartilage, it is more predominant in OA. In
addition, OA and normal aging cartilage differ in the
amount of water content and the in ratio of chondroitinsulfate to keratin sulfate constituents. The expression of a
chondroitin-sulfate epitope (epitope 846) in OA cartilage,
that is otherwise only present in fetal and neonatal
cartilage, provides further evidence that OA is a distinct
pathologic process. A final but important distinction is that
degradative enzyme activity is increased in OA, but not in
normal aging cartilage. (34)
Molecules
which
are
responsible
for
degrading cartilage matrix
The primary enzymes responsible for the degradation of
.cartilage are the matrix metalloproteinases (MMPs)
:The protease group is
Collagenases
Stromelysins
Gelatinases
:The protease inhibitor group is
TIMP 1
TIMP 2
2 - macroglobulin
These enzymes are secreted by both synovial cells and
chondrocytes and are categorized into three general
categories: a) Collagenases; b) Stromelysins; and, c)
Gelatinases. Under normal conditions, MMP synthesis and
44
activation are tightly regulated at several levels. They are
secreted as inactive proenzymes that require enzymatic
cleavage in order to become activated. Once activated,
MMPs become susceptible to the plasma-derived MMP
inhibitor, alpha-2-macroglobulin, and to tissue inhibitors of
MMPs (TIMPs) that are also secreted by synovial cells and
chondrocytes. In OA, synthesis of MMPs is greatly
enhanced and the available inhibitors are overwhelmed,
resulting in net degradation. Interestingly, stromelysin can
serve as an activator for its own proenzyme, as well as for
procollagenase and prostromelysin, thus creating a
positive feedback loop of pro MMP activation in cartilage.
(35)
Factors which are responsible for inducing
metalloprotease synthesis
One candidate is interleukin-1 (IL-1). IL-1 is a potent proinammatory cytokine that, in vitro, is capable of inducing
.chondrocytes and synovial cells to synthesize MMPs
Regulation of cartilage synthesis and
:degradation
IL- and TNF alpha promote cartilage degradation by
: enhancing
MMP synthesis
Prostanoid synthesis
Chondrocyte apoptosis
IL- receptor antagonist (IL-1 ra) and TIMP can
counteract these degradative processes
-2
-1
45
: Growth factors promote cartilage repair by
-3
Enhancing expression of IL-1 ra , type collagen and
proteoglycans
Down regulating expression of IL-1 receptors
Enhancing Chondrocyte proliferation
(36)
Furthermore, IL-1 suppresses the synthesis of type II
collagen and proteoglycans, and inhibits transforming
growth factor- stimulated Chondrocyte proliferation. The
presence of IL-1 RNA and protein has been confirmed in
OA joints. Thus, IL-1 may not only actively promote
cartilage degradation, but may also suppress attempts at
repair, in OA. In addition to these effects, IL-1 induces
nitric oxide production, Chondrocyte apoptosis, and
prostaglandin synthesis, which further contribute to
cartilage deterioration. Under normal conditions, an
endogenous IL-1 receptor antagonist regulates IL-1
activity. A relative excess of IL-1 and/or deficiency of the
IL-1 receptor antagonist could conceivably result in the
cartilage destruction that is characteristic of OA. It is likely
that other cytokines or particulate material from damaged
cartilage may also contribute to this inammatory,
degradative process. (37)
Can cartilage repair itself?
Growth factors are produced locally in cartilage and
synovium and are likely to contribute to local cartilage
remodeling by stimulating the de novo synthesis of
collagen and proteoglycans. Transforming growth factor
(TGF) is the best characterized and most potent of the
Chondrocyte growth factors. Not only does TGF stimulate
de novo matrix synthesis, but it also counteracts cartilage
degradation
by
down
regulating
IL-1
46
receptor expression and by increasing IL-1 receptor
antagonist release and TIMP expression. Insulin-like
growth factor (IGF-1) and basic fibroblast growth factor (bFGF) are also present in OA cartilage and likely to
contribute to reparative attempts, although, as noted,
degradation ultimately outstrips repair in OA cartilage. (38,
39)
Risk factors for Osteoarthritis:
1. Age
In demographic studies, age is the most consistently
identified risk factor for OA, regardless of the joint
being studied. Prevalence rates for both radiographic
OA and, to a lesser extent, symptomatic OA rise
steeply after age 50 in men and age 40 in women.
OA is rarely present in individuals less than 35 years
of age, and secondary causes of OA or other types of
arthritis should strongly be considered in this
population.
2. SEX:
Female gender is also a well-recognized risk factor for
OA. Hand OA is particularly prevalent among women.
47
In addition, polyarticular OA and isolated knee OA are
slightly more common in women than men, while hip
OA occurs more commonly in men. Interestingly,
women are more likely to report pain in all affected
joints, including the hip, than men.
3. OBESITY:
Cohort studies have demonstrated a clear
association of obesity with the development of
radiographic knee OA in women and a weaker
association with hip OA. Whether obesity is a risk
factor for the development of hand OA remains
controversial. Regardless, this remains one of the
most important modifiable risk factors for OA and
patients should be counseled appropriately.
4. JOINT STRESS:
Occupation-related repetitive injury and physical
trauma contribute to the development of secondary
(non-idiopathic) OA, sometimes occurring in joints
that are not affected by primary (idiopathic) OA,
such as the metacarpophalangeal joints, wrists and
ankles. Although the prevalence of knee OA is
greater in adults who have engaged in occupations
that require repetitive bending and strenuous
activities, an association with regular, intense
exercise remains controversial. While early studies in
joggers failed to find a higher prevalence of OA of
the knee in joggers compared to non-joggers, a
recent study of the Framingham data base in elderly
48
adults provided the first longitudinal association
between high level of physical activity and incident
knee OA. Low-impact and recreational exercises are
unlikely to constitute a risk factor for knee OA, and
are likely to benefit the cardiovascular system. Prior
menisectomy is a significant risk factor in men for
the development of OA in the knee
.
5. GENETICS:
Twin studies have demonstrated an important role
for genetics in the development of OA. In some
cases, this is associated with a particular genetic
syndrome, such as Stickler syndrome or familial
chondrocalcinosis. Genome-wide studies continue to
evaluate for particular chromosomes, particularly
those involved in bone or articular cartilage structure
and metabolism, and associations of familial OA. (40,
41)
Signs and Symptoms
OA is diagnosed by a triad of typical symptoms, physical
findings and radiographic changes. The American College
of Rheumatology has set forth classification criteria to aid
in the identification of patients with symptomatic OA that
.include, but do not rely solely on, radiographic findings
1. SYMPTOMS:
Patients with early disease experience localized joint
pain that worsens with activity and is relieved by
rest, while those with severe disease may have pain
at rest. Weight bearing joints may lock or give
49
way due to internal derangement that is a
consequence of advanced disease. Stiffness in the
morning or following inactivity (gel phenomenon)
rarely exceeds 30 minutes. Patients have pain which
is generally worse at the end of the day compared to
the beginning (because symptoms become worse
with use / activity). (42, 43)
2. SIGNS / EXAMINATION FINDINGS:
Physical findings in osteoarthritic joints include bony
enlargement,
crepitus, cool effusions,
and
decreased range of motion. Tenderness on palpation
at the joint line and pain on passive motion are also
common, although not unique to OA. Notably
absent in OA is the boggy synovitis seen
in inammatory arthritis (such as rheumatoid
arthritis) or the intense, hot inammation of
crystalline arthropathies. The distribution of joint
involvement in OA is important as well. Knees and
hips are common sites (because they are weightbearing joints). Hands can be involved, particularly
the distal and proximal interphalangeal joints where
bony enlargements can become quite dramatic and
are referred to as Heberdens and Bouchards nodes.
The base of the thumb (first carpometacarpal joint) is
frequently involved in OA and can even become
swollen and may be mistaken for wrist involvement.
(44)
3. X RAY / IMAGING FINDINGS:
Radiographic findings in OA include osteophyte
formation, joint space narrowing, subchondral
sclerosis and cysts. The presence of an osteophyte is
the most specific radiographic marker for OA
50
although it is indicative of relatively advanced
disease.
Peri-articular osteoporosis and
erosions
should not be demonstrated in OA and the presence
of such should prompt investigation for an alternative
diagnosis. Although conventional x-rays are the most
inexpensive and readily accessible method of
imaging to confirm a diagnosis of OA, magnetic
resonance imaging (MRI) is becoming an increasingly
important diagnostic tool. Compared to conventional
x-rays which only can show bony changes, MRI has
the benefit of providing information about cartilage,
peri articular structures (tendons), and can show
edema in the subchondral bone. MRI is being
investigated as a tool to assess the progression of OA
(natural history) as researchers continue to try and
develop therapies to treat OA. (45)
Figure (16) Stages of Knee Osteoarthritis
51
Figure (17) Plain X Ray (Antero-Posterior View)
Early Knee Osteoarthritis
52
Figure (18) Plain X Ray (Antero-Posterior View) Late
Knee Osteoarthritis
53
Figure (19) Plain X Ray (Antero-Posterior View)
Pathological Changes of Knee Osteoarthritis
Grading of Osteoarthritis
A number of classification systems are used for grading of
.osteoarthritis
OA can be classified into either primary or secondary
depending on whether or not there is an identifiable
.underlying cause
Both primary generalized nodal OA and erosive OA (EOA,
also called inammatory OA) are sub-sets of primary OA.
EOA is a much less common, and more aggressive
inammatory form of OA which often affects the distal
interphalangeal joints of the hand and has characteristic
.articular erosive changes on x-ray
WOMAC grading (Western Ontario McMaster
University)
The Western Ontario and McMaster Universities
Osteoarthritis Index (WOMAC) is used to assess pain,
stiffness, and physical function in patients with hip and / or
knee osteoarthritis (OA)
Stage i: there is softening of the cartilage of the
surfaces of the knee. This may not show on X-ray.
54
Stage ii: the cartilage starts to wear away and shows
as a narrowed joint space.
Stage iii: osteophytes are seen. Stage 2 and 3 may
merge and be difficult to separate.
Stage iv: is the "bone-on-bone" with very narrow joint
space, lots of osteophytes, and distortion of the joint
Outerbridge classification
Outerbridge classification system is used for classification
.of chondral damage in the knee
Grade 0: normal cartilage;
Grade I: cartilage with softening and swelling;
Grade II: a partial-thickness defect with fissures on
the surface that do not reach subchondral bone or
exceed 1.5 cm in diameter;
Grade III: fissuring to the level of subchondral bone
in an area with a diameter more than 1.5 cm;
Grade IV: exposed subchondral bone(46)
55
Figure (20) Anatomical Changes in Knee
Osteoarthritis
Differential Diagnosis of Osteoarthritis
If a patient has the typical symptoms and radiographic
features described above, the diagnosis of OA is relative
straightforward and is unlikely to be confused with other
entities. However, in less straightforward cases, other
:diagnoses should be considered
1. Periarticular structure derangement:
Periarticular pain that is not reproduced by passive
motion or palpation of the joint should suggest an
alternate etiology such as bursitis, tendonitis or
periostitis.
2. Inflammatory arthritis:
56
If the distribution of painful joints includes MCP,
wrist, elbow, ankle or shoulder, OA is unlikely, unless
there are specific risk factors (such as occupational,
sports-related, history of injury). Prolonged stiffness
(greater than one hour) should raise suspicion for
an inammatory
arthritis such
as rheumatoid arthritis.
Marked
warmth
and
erythema in a joint suggests a crystalline etiology.
Arthrocentesis (aspiration of the joint) can help aid in
distinguishing between these types of arthritis if the
diagnosis is not clear by history, physical exam, and
radiographs. If there is any suggestion of an infected
joint, it should be aspirated and the uid sent for
culture as well.
3. Other inflammatory / systemic conditions:
Weight loss, fatigue, fever and loss of appetite
suggest a systemic illness such as polymyalgia
rheumatica, rheumatoid arthritis, lupus or sepsis or
malignancy. (47)
57
Figure (21) Different Pathological Changes in
Rheumatoid Arthritis and Degenerative
Osteoarthritis
Treatment of Osteoarthritis
Pharmacological Therapies
Intra-articular Therapies
Non-pharmacological Management
Surgical Management
Functional Assessment
Future Directions
58
Current treatment for OA is limited to control
of symptoms. At this time, there are no
pharmacological agents capable of retarding
the progression of OA or preventing OA. This is
a fundamental and important area of
current research. In 2011, treatment is focused
on relief of pain, maintenance of quality of life,
and preservation of functional independence.
(48)
The use of interleukin 1 beta antagonists to
counteract the activation of the protienases
and consequently inhibit or slow the process of
cartilage degradation has been tried. the
results are promising but not yet confirmed
Pharmacological Therapy
:Acetaminophen
Several studies have shown acetaminophen to
be superior to placebo and equivalent to non
steroidal anti-inammatory agents (NSAIDs) for
the short-term management of OA pain. At
present, acetaminophen (up to 4,000 mg/daily)
is the recommended initial analgesic of choice
for symptomatic OA. (ACR Guidelines-Guidelines
for Medical Management of OA of the knee)
However, many patients eventually require
NSAIDs or more potent analgesics to control
.pain
(1
59
Non-steroidal Anti-inflammatory (2
:Agents (NSAIDs)
NSAIDs have been an important treatment for
the symptoms
of OA for a very long time. The
mechanism by which NSAIDs exert their antiinammatory and analgesic effects is via inhibition of
the
prostaglandin-generating
enzyme,
cyclooxygenase (COX). In addition to their
inammatory
potential,
prostaglandins
also
contribute to important homeostatic functions, such
as maintenance of the gastric lining, renal blood ow,
and platelet aggregation. Reduction of prostaglandin
levels in these organs can result in the wellrecognized
side
effects
of
traditional nonselective NSAIDs
(ibuprofen,
naprosyn,
and
indomethacin) that is, gastric ulceration, renal
insufficiency, and prolonged bleeding time. The
elderly are at higher risk for these side effects. Other
risk factors for NSAID-induced GI bleed include prior
peptic ulcer disease and concomitant steroid use.
Potential renal toxicities of NSAIDs include azotemia,
proteinura, and renal failure requiring hospitalization.
Hematologic and cognitive abnormalities have also
been reported with several NSAIDs. Therefore, in
elderly patients, and those with a documented
history of NSAID-induced ulcers, traditional nonselective NSAIDs should be used with caution, usually
in lower dose and in conjunction with a proton pump
inhibitor. Renal function should be monitored in the
elderly. In addition, prophylactic treatment to reduce
risk of gastrointestinal ulceration, perforation and
bleeding is recommended in patients > 60 years of
age with: prior history of peptic ulcer disease;
anticipated duration of therapy of > 3 months;
moderate to high dose of NSAIDs; and, concurrent
60
corticosteroids. The
development
of
selective
cyclooxygenase-2 (COX-2) inhibitors offers a strategy
for the management of pain and inammation that is
.likely to be less toxic to the GI tract
:COX-2 Inhibitors (3
Cyclooxygenase-2 (COX-2) inhibitors are a class of
NSAIDs) that recently received Food and Drug
Administration (FDA) approval. These specific COX-2
inhibitors are effective for the pain and inammation
of OA. Their theoretical advantage, however, is that
they will cause significantly less toxicity than
conventional NSAIDs, particularly in the GI tract.
NSAIDs exert their anti-inammatory effect primarily
by inhibiting an enzyme called cyclooxygenase
(COX), also known as prostaglandin (PG) synthase.
COX catalyzes the conversion of the substrate
.molecule, arachidonic acid, to prostanoids
: Pathway of prostanoid synthesis
Arachidonic acid under action of COX-1 and COX-2
: will give rise to
PGE2
PGD2
Prostacyclin
PG2
thromboxane
61
Prostanoids consist of prostaglandins E, D and F 2a,
prostacyclin
and
thromboxane.
The
major
inammatory vasoactive prostanoids are PGE2 and
prostacyclin. Thromboxane is critical for platelet
clotting, while PGD2 is involved in allergic reactions
.and PGF2a in uterine contraction
:Other Oral Analgesic Agents (4
For patients who cannot tolerate NSAIDs or COX-2
inhibitors other analgesics alone or in combination
may be appropriate. Tramadol, a non-NSAID/COX2
non-opioid pain medication, can be effective to
manage pain symptoms alone or in combination with
acetaminophen. Opioids should be a last resort for
pain management, often in late-stage disease, given
their many side effects including constipation,
somnolence, and potential for abuse. (51)
:Topical Agents (5
Topical analgesic therapies include topical capsaicin
and methyl salicylate creams. There is an FDA
approved topical NSAID for the treatment of OA,
diclofenac gel, which can be particularly useful for
patients who are intolerant to the gastrointestinal
.side effects of NSAIDs
:Intra-articular Therapies
The judicious use of intra-articular glucocorticoid
injections is appropriate for OA patients who cannot
tolerate, or whose pain is not well controlled by, oral
analgesic and anti-inammatory agents. Periarticular
injections may effectively treat bursitis or tendonitis
that can accompany OA. The need for four or more
intra-articular injections suggests the need for
62
orthopedic Intra-articular intervention. Intra-articular
injection of hyaluronate preparations has been
demonstrated in several small clinical trials to reduce
pain in OA of the knee. These injections are given in a
series of 3 or 5 weekly injections (depending on the
specific preparation) and may reduce pain for up to 6
months in some patients. (50)
Figure (22) Ozone Intra-Articular Injection in Knee
Osteoarthritis
Non-pharmacological Management
Weight reduction in obese patients has been shown
to significantly relieve pain, presumably by reducing
biomechanical
stress
on
weight bearing joints.
Exercise has also been shown to be safe and
beneficial in the management of OA. It has been
suggested that joint loading and mobilization are
essential for articular integrity. In addition,
quadriceps weakness, which develops early in OA,
may contribute independently to progressive
articular damage. Several studies in older adults with
symptomatic knee OA have shown consistent
improvements in physical performance, pain and selfreported disability after 3 months of aerobic or
resistance exercise. Other studies have shown that
63
resistive strengthening improves gait, strength and
overall function. Low-impact activities, including
water-resistive exercises or bicycle training, may
enhance peripheral muscle tone and strength and
cardiovascular endurance, without causing excessive
force across, or injury, to joints. Studies of nursing
home and community-dwelling elderly clearly
demonstrate that one additional important benefit of
exercise is a reduction in the number of falls. (48)
Surgical Management
Patients in who function and mobility remain
compromised despite maximal medical therapy, and
those in whom the joint is structurally unstable,
should be considered for surgical intervention.
Patients in whom pain has progressed to
unacceptable levels-that is, pain at rest and/or
nighttime pain-should also be considered as surgical
candidates. Surgical options include arthroscopy,
osteotomy and arthroplasty. Arthroscopic removal of
intra-articular
loose
bodies
and
repair
of
degenerative menisci may be indicated in some
patients with knee OA. Tibial osteotomy is an option
for some patients who have a relatively small varus
angulation (less than 10 degrees) and stable
Ligamentous support. Total knee arthroplasty is
recommended for patients with more severe varus,
or any valgus, deformity and Ligamentous instability.
Arthroplasty is also indicated for patients who have
had ineffective pain relief following a tibial
osteotomy, and for those with advanced hip OA.
Patients who have not yet developed appreciable
muscle weakness, generalized or cardiovascular
64
deconditioning and who would medically withstand
the stress of surgery are ideal surgical candidates. In
contrast, full mobility and function may not be
realistically expected in patients with significant
cognitive
impairment
or
symptomatic
cardiopulmonary disease, since these conditions can
.impede post-operative rehabilitation
Functional Assessment
Several questionnaires have been established as
validated, reliable research instruments for assessing
functional outcomes in patients with arthritis. These
include the Lequesne index, the Western Ontario
McMaster Arthritis scale (WOMAC), activities of daily
living (ADL), etc. Several performance-based tests of
function can be done rapidly and easily in the office,
however, and may be more sensitive in predicting
impending disability than direct questions about
disability and impairment. Such measures include
grip strength, a timed walk, sequential chair-stands,
and others listed below.(49)
65
Functional assessment measures
Osteoarthritis specific indices
Lequesne Algofunctional Index
-1
Western Ontario McMaster University osteoarthritis
index (WOMAC)
-2
:General measures of function
: Self report
-a
Kaiz Activities of daily living
Instrumental Activities of daily living
Geriatric arthritis impact scale
Objective Performance upper body
Grip strength
Pinch strength
Dexterity
:Objective performance lower body
Balance
-b
-c
Speed and motility
Gait evaluation
These tests can provide the clinician with valuable
information on the patients current level of function,
66
as well as serve longitudinally to assess decline in
function
Future Directions
Osteoarthritis is the most prevalent articular disease
in the elderly. Disease markers that will detect early
disease and agents that will slow down or halt
disease progression are critically needed. Current
management should include safe and adequate pain
relief using systemic and local therapies, and should
include medical and rehabilitative interventions that
limit functional deterioration. Research is continuing
to focus on the pathophysiology of OA as we are in
need of strategies to slow the progression of OA or
reverse the process.(51)
67
Rheumatoid Arthritis (RA)
It is the second important and second common form
of arthritis after osteoarthritis
Rheumatoid
arthritis (RA)
is
an autoimmune
disease that results in a chronic, systemic inammatory
disorder that may affect many tissues and organs, but
principally attacks exible (synovial) joints. It can be a
disabling and painful condition, which can lead to
substantial loss of functioning and mobility if not
adequately treated. (52)
The process involves an inammatory response of the
capsule around the joints (synovium) secondary to
swelling (turgescence) of synovial cells, excess synovial
uid, and the development of fibrous tissue (pannus) in
the synovium. The pathology of the disease process often
leads
to
the
destruction
of
articular
cartilage
and ankylosis (fusion) of the joints. RA can also produce
diffuse inammation in the lungs, the membrane around
the heart (pericardium), the membranes of the lung
(pleura), and white of the eye (sclera), and also nodular
lesions, most common in subcutaneous tissue. Although
the cause of RA is unknown, autoimmunity plays a big
part, and RA is a systemic autoimmune disease. It is
a clinical diagnosis made on the basis of symptoms,
.physical exam, radiographs (X-rays) and labs
68
Treatments are pharmacological and non-pharmacological.
Non-pharmacological
treatment
includes physical
therapy, orthoses ,occupational therapy and nutritional
therapy but these do not stop the progression of joint
destruction.
Analgesics
(painkillers)
and
antiinammatory drugs,
including steroids,
suppress
symptoms,
but
do
not
stop
the
progression
of joint destruction
either. Disease-modifying
antirheumatic drugs (DMARDs) slow or halt the progress of the
disease. The newer biologics are DMARDs. The evidence
for complementary
and
alternative
medicine (CAM)
treatments for RA related pain is weak, with the lack of
high quality evidence leading to the conclusions that their
use is currently not supported by the evidence. Patients
should inform their health care provider of any CAM
.treatments and continue taking traditional treatments
About 0.6% of the United States adult population has RA,
women two to three times as often as men. Onset is most
frequent during middle age, but people of any age can be
affected. (53)
The name is based on the term "rheumatic fever", an
illness which includes joint pain and is derived from the
Greek word -rheuma (nom.), -rheumatos
(gen.) ("ow, current"). The suffix -oid ("resembling") gives
the translation as joint inammation that resembles
rheumatic fever. The first recognized description of RA was
made in 1800 by Dr. Augustine Jacob Landr-Beauvais
.(17721840) of Paris
Epidemiology
RA affects between 0.5 and 1% of adults in the developed
world with between 5 and 50 per 100,000 people newly
developing the condition each year. In 2010 it resulted in
.about 49,000 deaths globally
Onset is uncommon under the age of 15 and from then on
the incidence rises with age until the age of 80. Women
.are affected three to five times as often as men
69
Some Native American groups have higher prevalence
rates (56%) and people from the Caribbean region have
.lower prevalence rates
The age at which the disease most commonly starts is in
women between 40 and 50 years of age, and for men
somewhat later. RA is a chronic disease, and although
rarely, a spontaneous remission may occur, the natural
course is almost invariably one of persistent symptoms,
waxing and waning in intensity, and a progressive
deterioration of joint structures leading to deformations
and disability. (53)
Figure (23) Common Joints Affected By
Rheumatoid Arthritis
70
Figure (24) Common Joints Affected By
Rheumatoid Arthritis
Signs and Symptoms
RA primarily affects joints; however it also affects
other organs in 1525% of individuals. It can be difficult to
determine whether disease manifestations are directly
caused by the rheumatoid process itself, or from side
effects of the medications used to treat it for
example, lung
fibrosis from methotrexate or osteoporosis from
.corticosteroids
Joints
Arthritis of joints involves inammation of the synovial
membrane. Joints become swollen, tender and warm, and
stiffness limits their movement. With time, multiple joints
71
are affected (it is a polyarthritis). Most commonly involved
are the small joints of the hands, feet and cervical, but
larger joints like the shoulder and knee can also be
involved. Synovitis can lead to tethering of tissue with loss
of movement and erosion of the joint surface causing
deformity and loss of function. (54)
RA typically manifests with signs of inammation, with the
affected joints being swollen, warm, painful and stiff,
particularly early in the morning on waking or following
prolonged inactivity. Increased stiffness early in the
morning is often a prominent feature of the disease and
typically lasts for more than an hour. Gentle movements
may relieve symptoms in early stages of the disease.
These signs help distinguish rheumatoid from noninammatory problems of the joints, often referred to
as osteoarthritis or "wear-and-tear" arthritis. In arthritis of
non-inammatory causes, signs of inammation and early
morning stiffness are less prominent with stiffness
typically less than one hour, and movements induce pain
caused by mechanical arthritis. The pain associated with
RA is induced at the site of inammation and classified as
nociceptive as opposed to neuropathic. The joints are
often affected in a fairly symmetrical fashion, although
this is not specific, and the initial presentation may be
asymmetrical. (60)
As the pathology progresses the inammatory activity
leads to tendon tethering and erosion and destruction of
the joint surface, which impairs range of movement and
leads to deformity. The fingers may suffer from almost any
deformity depending on which joints are most involved.
Specific deformities, which also occur in osteoarthritis,
include ulnar deviation, boutonniere deformity, swan neck
deformity and "Z-thumb." "Z-thumb" or "Z-deformity"
consists of hyperextension of the interphalangeal joint,
fixed exion and sublaxation of the metacarpophalangeal
joint and gives a "Z" appearance to the thumb.
The hammer toe deformity may be seen. In the worst
case, joints are known as arthritis mutilans due to the
mutilating nature of the deformities. (56)
72
Lungs
Fibrosis of the lungs is a recognized response to
rheumatoid disease. It is also a rare but well recognized
consequence
of
therapy
(for
example
with methotrexate and
leunomide). Caplan's
syndrome describes lung nodules in individuals with RA
and additional exposure to coal dust. Pleural effusions are
also associated with RA. Another complication of RA
is Rheumatoid Lung Disease. It is estimated that about
one quarter of Americans with RA develop Rheumatoid
Lung Disease. (57)
Kidneys
Renal amyloidosis can occur as a consequence of chronic
inammation. RA
may
affect
the
kidney glomerulus directly
through
a vasculopathy or
a mesangial infiltrate but this is less well documented
(though this is not surprising, considering immune
complex-mediated
hypersensitivities
are
known
for pathogenic deposition of immune complexes in organs
where blood is filtered at high pressure to form other
uids, such as urine and synovial uid). Treatment
with Penicillamine and gold salts are recognized causes
of membranous nephropathy. (58)
Heart and blood vessels
People with RA are more prone to atherosclerosis, and risk
of myocardial
infarction (heart
attack)
and stroke is
markedly increased. Other possible complications that
may
arise
include: pericarditis, endocarditis,
left
ventricular failure, valvulitis and fibrosis. Many people with
RA do not experience the same chest pain that others feel
when they have angina or myocardial infarction. To reduce
cardiovascular risk, it is crucial to maintain optimal control
of the inammation caused by RA (which may be involved
73
in causing the cardiovascular risk), and to use exercise
and
medications
appropriately
to
reduce
other
cardiovascular risk factors such as blood lipids and blood
pressure. Doctors who treat RA patients should be
sensitive to cardiovascular risk when prescribing antiinammatory medications, and may want to consider
prescribing routine use of low doses of aspirin if the
gastrointestinal effects are tolerable. (59)
Skin
The rheumatoid nodule, which is sometimes cutaneous, is
the feature most characteristic of RA. It is a type of
inammatory reaction known to pathologists as a
"necrotizing granuloma". The initial pathologic process in
nodule formation is unknown but may be essentially the
same as the synovitis, since similar structural features
occur in both. The nodule has a central area of fibrinoid
necrosis that may be fissured and which corresponds to
the fibrin-rich necrotic material found in and around an
affected synovial space. Surrounding the necrosis is a
layer
of palisading macrophages and fibroblasts,
corresponding to the intimal layer in synovium and a cuff
of connective
tissue containing
clusters
of lymphocytes and plasma
cells,
corresponding
to
the subintimal zone in synovitis. The typical rheumatoid
nodule may be a few millimeters to a few centimeters in
diameter and is usually found over bony prominences,
such as the olecranon, the calcaneal tuberosity, the
metacarpophalangeal joint, or other areas that sustain
repeated mechanical stress. Nodules are associated with a
positive RF (rheumatoid factor) titer and severe erosive
arthritis. Rarely, these can occur in internal organs or at
.diverse sites on the body
Several forms of vasculitis occur in RA. A benign form
occurs as micro infarcts around the nail folds. More severe
forms include livedo reticularis, which is a network
(reticulum) of erythematosus to purplish discoloration of
the skin caused by the presence of an obliterative
.cutaneous capillaropathy
74
Other,
rather
rare,
skin
associated
symptoms
include pyoderma gangrenosum, Sweet's syndrome, drug
reactions, erythema nodosum, lobe panniculitis, atrophy of
finger skin, palmar, diffuse thinning (rice paper skin), and
skin fragility (often worsened by corticosteroid use). (61,62,63)
Ocular
The eye is directly affected in the form of episcleritis which
when
severe
can
very
rarely
progress
to
perforating scleromalacia. Rather more common is the
indirect effect of keratoconjunctivitis sicca, which is a
dryness
of
eyes
and
mouth
caused
by lymphocyte infiltration of lacrimal and salivary glands.
When severe, dryness of the cornea can lead
to keratitis and loss of vision. Preventive treatment of
severe dryness with measures such as nasolacrimal
duct blockage is important. (64, 65, 66)
Hepatic
Cytokine production in joints and/or hepatic (liver) Kupffer
cells leads to increased activity of hepatocytes with
increased production of acute-phase proteins, such as Creactive protein, and increased release of enzymes such
as alkaline phosphatase into
the
blood.
In Felty's
syndrome, Kupffer cell activation is so marked that the
resulting increase in hepatocyte activity is associated with
nodular hyperplasia of the liver, which may be palpably
enlarged. Although Kupffer cells are within the
hepatic parenchyma, they are separate from hepatocytes.
As a result there is little or no microscopic evidence
of hepatitis (immune-mediated
destruction
of
hepatocytes). Hepatic involvement in RA is essentially
asymptomatic.
Hematological
Anemia is by far the most common abnormality of the
blood cells which can be caused by a variety of
mechanisms. The chronic inammation caused by RA
leads to raised hepcidin levels, leading to anemia of
chronic disease where iron is poorly absorbed and also
sequestered into macrophages. RA may also cause a warm
autoimmune hemolytic anemia.[18] The red cells are of
normal size and color (normocytic and normochromic). A
75
low white blood cell count (neutropenia) usually only
occurs in patients with Felty's syndrome with an enlarged
liver and spleen. The mechanism of neutropenia is
complex. An increased platelet count (thrombocytosis)
occurs when inammation is uncontrolled. (67)
Lymphoma
The incidence of lymphoma is increased in RA, although it
is still uncommon. , (68)
Neurological
Peripheral neuropathy and mononeuritis multiplex may
occur. The most common problem is carpal tunnel
syndrome caused by compression of the median nerve by
swelling around the wrist. Atlanto-axial sublaxation can
occur,
owing
to
erosion
of
the odontoid
process and/or transverse ligaments in the cervical spine's
connection to the skull. Such an erosion (>3mm) can give
rise to vertebrae slipping over
one
another
and
compressing the spinal cord. Clumsiness is initially
experienced, but without due care this can progress
to quadriplegia. (69)
Constitutional symptoms
Constitutional symptoms including fatigue ,low grade
fever
,
malaise
, morning
stiffness, loss
of
appetite and loss of weight are common systemic
manifestations seen in patients with active RA. (70)
Osteoporosis
Local osteoporosis occurs in RA around inamed joints. It
is postulated to be partially caused by inammatory
cytokines. More general osteoporosis is probably
contributed to by immobility, systemic cytokine effects,
and local cytokine release in bone marrow and
corticosteroid therapy.
76
Figure (25) Characters of Rheumatoid
Arthritis
Figure (26) Effects of Rheumatoid Arthritis on
Different Organs
Causes (etiology)
RA is a form of autoimmunity, the causes of which are still
not completely known. It is a systemic (whole body)
77
disorder principally affecting synovial tissues. There is no
evidence that physical and emotional effects or stress
could be a trigger for the disease. The many negative
findings suggest that either the trigger varies, or that it
might in fact be a chance event inherent with the immune
response. (71)
Half of the risk for RA is believed to be genetic. It is
strongly associated with the inherited tissue type major
histocompatibility complex (MHC) antigen HLA-DR4 (most
specifically DR0401 and 0404), and the genes PTPN22 and
PADI4hence family history is an important risk factor.
Inheriting the PTPN22 gene has been shown to double a
person's susceptibility to RA. PADI4 has been identified as
a major risk factor in people of Asian descent, but not in
those
of
European
descent. First-degree
relatives'
prevalence
rate
is
23%
and
disease genetic
concordance in monozygotic twins is approximately 1520
%.( 72)
Smoking is the most significant non-genetic risk with RA
being up to three times more common in smokers than
non-smokers, particularly in men, heavy smokers, and
those who are rheumatoid factor positive. Modest alcohol
.consumption may be protective
Epidemiological studies have confirmed a potential
association between RA and two herpes virus infections:
Epstein Barr (EBV) and Human Herpes Virus 6 (HHV-6).
Individuals with RA are more likely to exhibit an abnormal
immune response to EBV and have high levels of anti-EBV
antibodies. (73)
Vitamin D deficiency is common in those with RA and may
be causally associated. Some trials have found a
decreased risk for RA with vitamin D supplementation
.while others have not
Vitamin D deficiency is more common in patients with
rheumatoid
arthritis
than
in
the
general
population. However, whether vitamin D deficiency is a
cause or a consequence of the disease remains
78
unclear. 1, 25-dihydroxyvitamin D3 (1,25D), an active
metabolite of vitamin D, affects bone metabolism
indirectly through control of calcium and phosphate
homeostasis. Interaction between 1,25D and the vitamin D
receptor (VDR) affects the production of RANKL and delays
osteoclastogenesis. (75)
Pathophysiology
The key pieces of evidence relating to pathogenesis are
:the following
1.
A genetic link with HLA-DR4 and related allotypes
of MHC Class II and the T cell-associated protein PTPN22.
2.
An undeniable link to the pathogenesis of vascular
disease of many types, including the possibility of a strong
causal connection to rheumatoid vasculitis, a typical
feature of this condition.
3.
A remarkable deceleration of disease progression in
many cases by blockade of the cytokine TNF (alpha).
4.
A similar dramatic response in many cases to
depletion of B lymphocytes, but no comparable response
to depletion of T lymphocytes.
5.
A more or less random pattern of whether and when
individuals predisposed are affected.
6.
The presence of auto-antibodies to IgGFc, known
as rheumatoid factors (RF), and antibodies to citrullinated
peptides (ACPA).
7.
8.
Initial site of disease is synovial membrane
Women (30 to 50 years) are more commonly
affected(76)
These data suggest that the disease involves abnormal B
cellT cell interaction, with presentation of antigens by B
79
cells to T cells via HLA-DR eliciting T cell help and
consequent production of RF and ACPA. Inammation is
then driven either by B cell or T cell products stimulating
release of TNF and other cytokines. The process may be
facilitated by an effect of smoking on citrullination but the
stochastic (random) epidemiology suggests that the rate
limiting step in genesis of disease in predisposed
individuals may be an inherent stochastic process within
the immune response such as immunoglobulin or T cell
receptor gene recombination and mutation. (77)
If TNF release is stimulated by B cell products in the form
of RF or ACPA -containing immune complexes, through
activation of immunoglobulin Fc receptors, then RA can be
seen as a form of Type III hypersensitivity. If TNF release is
stimulated by T cell products such as interleukin-17 it
might
be
considered
closer
to type
IV
hypersensitivity although this terminology may be getting
somewhat dated and unhelpful. The debate on the relative
roles of immune complexes and T cell products in
inammation in RA has continued for 30 years. There is
little doubt that both B and T cells are essential to the
disease. However, there is good evidence for neither cell
being necessary at the site of inammation. This tends to
favor immune complexes (based on antibody synthesized
elsewhere) as the initiators, even if not the sole
perpetuators of inammation. Moreover, work by Thurlings
and others in Paul-Peter Tak's group and also by Arthur
Kavanagh's group suggest that if any immune cells are
relevant locally they are the plasma cells, which derive
from B cells and produce in bulk the antibodies selected at
.the B cell stage
Although
TNF
appears
to
be
the
dominant,
other cytokines (chemical mediators) are likely to be
involved in inammation in RA. Blockade of TNF does not
benefit all patients or all tissues (lung disease and nodules
may get worse). Blockade of IL-1, IL-15 and IL-6 also have
beneficial
effects
and IL-17 may
be
important.
Constitutional symptoms such as fever, malaise, loss of
80
appetite and weight loss are also caused by cytokines
.released into the blood stream
As with most autoimmune diseases, it is important to
distinguish between the cause(s) that trigger the process,
and those that may permit it to persist and progress. (78)
Phases
Initiation phase It is due to non specific
inammation
Amplification phase Due to T cell activation
Chronic inammatory phase Due to cytokines IL1,
TNF-alpha and IL6
Abnormal immune response
The factors that allow an abnormal immune response,
once initiated, to become permanent and chronic, are
becoming more clearly understood. The genetic
association with HLA-DR4, as well as the newly discovered
associations with the gene PTPN22 and with two additional
genes, all implicate altered thresholds in regulation of the
adaptive immune response. It has also become clear from
recent studies that these genetic factors may interact with
the most clearly defined environmental risk factor for RA,
namely cigarette smoking. Other environmental factors
also appear to modulate the risk of acquiring RA, and
hormonal factors in the individual may explain some
features of the disease, such as the higher occurrence in
women, the not-infrequent onset after child-birth, and the
slight modulation of disease risk by hormonal medications.
Exactly how altered regulatory thresholds allow the
triggering of a specific autoimmune response remains
uncertain. However, one possibility is that negative
feedback mechanisms that normally maintain tolerance of
self are overtaken by aberrant positive feedback
81
mechanisms for certain antigens such as IgG Fc bound by
RF and citrullinated fibrinogen bound by ACPA (79)
Once the abnormal immune response has become
established (which may take several years before any
symptoms
occur),
plasma
cells
derived
from
B lymphocytes produce rheumatoid factors and ACPA of
the IgG and IgM classes in large quantities. These are not
deposited in the way that they are in systemic lupus.
Rather, they activate macrophages through Fc receptor
and complement binding, which seems to play an
important role in the intense inammatory response
present in RA. This contributes to inammation of the
synovium, in terms of edema, vasodilatation and
infiltration by activated T-cells (mainly CD4 in nodular
aggregates and CD8 in diffuse infiltrates). Synovial
macrophages and dendritic cells further function as
antigen presenting cells by expressing MHC class II
molecules, leading to an established local immune
reaction in the tissue. The disease progresses in concert
with formation of granulation tissue at the edges of the
synovial lining (pannus) with extensive angiogenesis and
production of enzymes that cause tissue damage. Modern
pharmacological treatments of RA target these mediators.
Once the inammatory reaction is established, the
synovium thickens, the cartilage and the underlying bone
begin to disintegrate and evidence of joint destruction
accrues (81, 82)
Diagnosis
Blood tests
When RA is clinically suspected, immunological studies are
required, such as testing for the presence of rheumatoid
factor (RF, a non-specific antibody). A negative RF does
not rule out RA; rather, the arthritis is called seronegative.
This is the case in about 15% of patients. During the first
year of illness, rheumatoid factor is more likely to be
negative with some individuals converting to seropositive
status over time. RF is also seen in other illnesses, for
82
example Sjgren's syndrome, hepatitis C, systemic lupus
erythematosus, chronic infections and in approximately
10% of the healthy population, therefore the test is not
very specific.(83)
Because of this low specificity, new serological tests have
been developed, which test for the presence of the anticitrullinated protein antibodies (ACPAs) or anti-CCP. Like
RF, these tests are positive in only a proportion (67%) of
all RA cases, but are rarely positive if RA is not present,
giving it a specificity of around 95%. As with RF, there is
evidence for ACPAs being present in many cases even
before onset of clinical disease. (84)
The most common tests for ACPAs are the anti-CCP (cyclic
citrullinated peptide) test and the Anti-MCV assay
(antibodies against mutated citrullinated Vimentin).
Recently a serological point-of-care test (POCT) for the
early detection of RA has been developed. This assay
combines the detection of rheumatoid factor and anti-MCV
for diagnosis of RA and shows a sensitivity of 72% and
.specificity of 99.7%
Also, several other blood tests are usually done to allow
for other causes of arthritis, such as lupus erythematosus.
The erythrocyte
sedimentation
rate (ESR), C-reactive
protein, full blood count, renal function, liver enzymes and
other immunological tests (e.g., antinuclear antibody/ANA)
are all performed at this stage. Elevated ferritin levels can
reveal hemochromatosis, a mimic of RA, or be a sign
of Still's disease, a seronegative, usually juvenile, and
variant of rheumatoid arthritis. (85)
Imaging
Signs
of
destruction
and
inammation
on ultrasonography and magnetic resonance imaging in
the second metacarpophalangeal joint in established RA.
X-rays of the hands and feet are generally performed in
people with a polyarthritis. In RA, there may be no
changes in the early stages of the disease, or the x-ray
83
may demonstrate juxta-articular osteopenia, soft tissue
swelling and loss of joint space. As the disease advances,
there may be bony erosions and sublaxation. X-rays of
other joints may be taken if symptoms of pain or swelling
.occur in those joints
Other medical imaging techniques such as magnetic
resonance imaging (MRI) and ultrasound are also used in
.RA
There have been technical advances in ultrasonography.
High-frequency transducers (10 MHz or higher) have
improved the spatial resolution of ultrasound images;
these images can depict 20% more erosions than
conventional radiography. Also, color Doppler and power
Doppler ultrasound, which show vascular signals of active
synovitis depending on the degree of inammation, are
useful in assessing synovial inammation. This is
important, since in the early stages of RA, the synovium is
primarily affected, and synovitis seems to be the best
predictive marker of future joint damage. (83)
Criteria
In 2010 the 2010 ACR / EULAR Rheumatoid Arthritis
.Classification Criteria were introduced
These new classification criteria overruled the "old" ACR
criteria of 1987 and are adapted for early RA diagnosis.
The "new" classification criteria, jointly published by
the American College of Rheumatology (ACR) and
the European
League
Against
Rheumatism (EULAR)
establish a point value between 0 and 10. Every patient
with a point total of 6 or higher is unequivocally classified
as RA patient, provided he has synovitis in at least one
joint and given that there is no other diagnosis better
84
explaining the synovitis. Four areas are covered in the
:diagnosis
joint
involvement,
designating
the metacarpophalangeal joints, proximal interphalangeal
joints, the interphalangeal joint of the thumb, second
through fifth metatarsophalangeal joint and wrist as small
joints,
and shoulders, elbows, hip
joints, knees,
and ankles as large joints:
Involvement of 1 large joint gives 0 points
Involvement of 210 large joints gives 1 point
Involvement of 13 small joints (with or without
involvement of large joints) gives 2 points
Involvement of 410 small joints (with or without
involvement of large joints) gives 3 points
Involvement of more than 10 joints (with
involvement of at least 1 small joint) gives 5 points
serological parameters including the rheumatoid
factor as well as ACPA "ACPA" stands for "anticitrullinated protein antibody":
Negative RF and negative ACPA gives 0 points
Low-positive RF or low-positive ACPA gives 2
points
High-positive RF or high-positive ACPA gives 3
points
acute phase reactants: 1 point for elevated
erythrocyte
sedimentation
rate, ESR,
or
elevated CRP value (c-reactive protein)
duration of arthritis: 1 point for symptoms lasting six
weeks or longer(86)
The new criteria accommodate to the growing
understanding of RA and the improvements in diagnosing
RA and disease treatment. In the "new" criteria serology
and autoimmune diagnostics carries major weight, as
ACPA detection is appropriate to diagnose the disease in
an early state, before joints destructions occur.
Destruction of the joints viewed in radiological images was
a significant point of the ACR criteria from 1987. This
criterion no longer is regarded to be relevant, as this is
85
just the type of damage that treatment is meant to avoid.
(87)
The criteria are not intended for the diagnosis for routine
clinical care; they were primarily intended to categorize
research (classification criteria). In clinical practice, the
:following criteria apply
two or more swollen joints
morning stiffness lasting more than one hour for at
least six weeks
The
detection
of rheumatoid
factors or autoantibodies against ACPA such
as
auto-antibodies
to mutated
citrullinated
Vimentin can
confirm
the
suspicion of RA. A negative autoantibody result does not
exclude a diagnosis of RA.(88)
86
Figure (27) Plain X ray (Postero-anterior View)
Rheumatoid Arthritis Right Hand
Figure (28) Rheumatoid Arthritis Both Hands
Differential diagnoses
Several other medical conditions can resemble RA, and
usually need to be distinguished from it at the time of
:diagnosis
Crystal induced arthritis (gout, and pseudo-gout)
usually involves particular joints (knee, MTP1, heels) and
can be distinguished with aspiration of joint uid if in
doubt. Redness, asymmetric distribution of affected joints,
pain occurs at night and the starting pain is less than an
hour with gout.
Osteoarthritis distinguished with X-rays of the
affected joints and blood tests, age (mostly older
patients), starting pain less than an hour, a-symmetric
87
distribution of affected joints and pain worsens when using
joint for longer periods.
Systemic lupus erythematosus (SLE) distinguished
by specific clinical symptoms and blood tests (antibodies
against double-stranded DNA)
One
of
the
several
types
of psoriatic
arthritis resembles RA nail changes and skin symptoms
distinguish between them
Lyme disease causes erosive arthritis and may
closely resemble RA it may be distinguished by blood
test in endemic areas
Reactive arthritis (previously Reiter's disease)
asymmetrically involves heel, sacroiliac joints, and large
joints
of
the
leg.
It
is
usually
associated
with urethritis, conjunctivitis, iritis, painless buccal ulcers,
and keratoderma blennorrhagica.
Ankylosing spondylitis this involves the spine,
although a RA-like symmetrical small-joint polyarthritis
may occur in the context of this condition.
Hepatitis
C
RA-like
symmetrical
small-joint
polyarthritis may occur in the context of this condition.
Hepatitis C may also induce Rheumatoid Factor autoantibodies
Rarer causes that usually behave differently but may
:cause joint pains
Sarcoidosis, amyloidosis, and Whipple's disease can
also resemble RA.
Hemochromatosis may cause hand joint arthritis.
Acute rheumatic fever can be differentiated from RA
by a migratory pattern of joint involvement and evidence
of antecedent streptococcal infection. Bacterial arthritis
(such as streptococcus) is usually asymmetric, while RA
usually involves both sides of the body symmetrically.
Gonococcal arthritis (another bacterial arthritis) is
also initially migratory and can involve tendons around the
wrists and ankles.(90,91)
88
Monitoring progression
The progression of RA can be followed using scores such
as Disease Activity Score of 28 joints (DAS28). It is widely
used as an indicator of RA disease activity and response to
treatment, but it is not always a reliable indicator of
treatment effect. The joints included in DAS28 are
(bilaterally): proximal
interphalangeal
joints (10
joints),metacarpophalangeal
joints (10), wrists (2), elbows (2), shoulders (2)
and knees (2). When looking at these joints, both the
number of joints with tenderness upon touching (TEN28)
and swelling (SW28) are counted. In addition,
the erythrocyte sedimentation rate (ESR) is measured.
Also, the patient makes a subjective assessment (SA) of
disease activity during the preceding 7 days on a scale
between 0 and 100, where 0 is "no activity" and 100 is
"highest activity possible". With these parameters, DAS28
:is
calculated
as
From this formula, the progression of the disease, the
effectiveness of the treatment can be measured (92)
89
Figure (29) Plain X- ray (Posteroanterior and Lateral
(Views) Rheumatoid Arthritis Knee
Figure (30) Rheumatoid Arthritis Knees
90
Management
There is no cure for RA, but treatments can improve
symptoms and slow the progress of the disease. Diseasemodifying treatment has the best results when it is started
.early and aggressively
The goals of treatment are to minimize symptoms such as
pain and swelling, to prevent bone deformity (for example,
bone erosions visible in X-rays), and to maintain day-today functioning. This can often be achieved using two
main classes of medications: analgesics such as NSAIDs,
and disease-modifying antirheumatic drugs (DMARDs). RA
should generally be treated with at least one specific antirheumatic medication. The use of benzodiazepines (such
as diazepam) to treat the pain is not recommended as it
does not appear to help and is associated with risks.
Analgesics, other than NSAIDs, offer lesser, but some
benefit with respect to pain, whilst not causing the same
level of gastrointestinal irritation. (93)
Lifestyle
Regular exercise is recommended as both safe and useful
to maintain muscles strength and overall physical
function. It is uncertain if specific dietary measures have
.an effect
Disease modifying agents
Disease-modifying antirheumatic drugs (DMARD) are the
primary treatment for RA. They are a diverse collection of
drugs, grouped by use and convention. They have been
found to improve symptoms, decrease joint damage, and
improve overall functional abilities. They should be started
very early in the disease as when they result in disease
91
remission in approximately half of people and improve
.outcomes overall
The most commonly used agent is methotrexate with
other frequently used agents including Sulfasalazine and
leunomide. Sodium
aurothiomalate (Gold)
and cyclosporin are less commonly used due to more
common adverse effects. Agents may be used in
combinations. (94)
Methotrexate is the most important and useful DMARD
and is usually the first treatment. Adverse effects should
be
monitored
regularly
with
toxicity
including
gastrointestinal, hematologic, pulmonary, and hepatic.
Side effects such as nausea, vomiting or abdominal pain
can be reduced by taking folic acid. The most common
undesirable effect is that it increases liver enzymes in
almost 15% of people. It is thus recommended that those
who consistently demonstrate abnormal levels of liver
enzymes or have a history of liver disease or alcohol use
undergo liver biopsies. Methotrexate is also considered
a teratogenic drug and as such, it is recommended that
women of childbearing age should use contraceptives to
avoid pregnancy and to discontinue its use if pregnancy is
.planned
Biological agents should generally only be used if
methotrexate and other conventional agents are not
effective after a trial of three months. These agents
include: tumor necrosis factor alpha (TNF) blockers such
as iniximab; interleukin
1 blockers
such
as anakinra, monoclonal antibodies against B cells such
as rituximab,
T
cellcostimulation
blocker
such
as abatacept among others. They are often used in
.combination with either methotrexate or leunomide
TNF blockers and methotrexate appear to have similar
effectiveness when used alone and better results are
obtained when used together. TNF blockers appear to
have equivalent effectiveness with etanercept appearing
to be the safest. Abatacept appears effective for RA with
20% more people improving with treatment than
92
without. There however is a lack of evidence to distinguish
between the biologics available for RA. Issues with the
biologics include their high cost and association with
infections including tuberculosis. (95)
Anti-inammatory agents
NSAIDs reduce both pain and stiffness in those with RA.
Generally they appear to have no effect on people's long
term disease course and thus are no longer first line
agents. NSAIDs should be used with caution in those
.with gastrointestinal, cardiovascular, or kidney problems
COX-2 inhibitors, such as celecoxib, and NSAIDs are
equally effective. They have a similar gastrointestinal risk
as a NSAIDs plus a proton pump inhibitor. In the elderly
there is less gastrointestinal intolerance to celecoxib than
to NSAIDs alone. There however is an increased risk
of myocardial infarction with COX-2 inhibitors. Anti-ulcer
medications are not recommended routinely but only in
.those high risk of gastrointestinal problems
Glucocorticoids can be used in the short term for are-ups,
while waiting for slow-onset drugs to take effect. Injection
of glucocorticoids into individual joints is also effective.
While long-term use reduces joint damage it also results in
osteoporosis and susceptibility to infections, and thus is
not recommended. (96)
Surgery
In early phases of the disease, an arthroscopic or
open synovectomy may be performed. It consists of the
removal of the inamed synovia and prevents a quick
destruction of the affected joints. Severely affected joints
may require joint replacement surgery, such as knee
replacement. Postoperatively, physiotherapy is always
necessary. (97)
Alternative medicine
93
There has been an increasing interest in the use of
complementary and alternative medicine interventions for
the treatment of pain in rheumatoid arthritis. While there
have been multiple studies showing beneficial effects in
RA on a wide variety of CAM modalities, these studies are
often affected by publication bias and are generally not
high quality evidence such as randomized controlled
trials (RCTs), making definitive conclusions difficult to
reach.(98)
The National Center for Complementary and Alternative
Medicine has concluded, "In general, there is not enough
scientific evidence to prove that any complementary
health approaches are beneficial for RA, and there are
safety concerns about some of them. Some mind and
body practices and dietary supplements may help people
with RA manage their symptoms and therefore may be
beneficial additions to conventional RA treatments, but
there
is
not
enough
evidence
to
draw
conclusions." A systematic review of CAM modalities
(excluding fish oil) found "The major limitation in reviewing
the evidence for CAMs is the paucity of RCTs in the area.
The available evidence does not support their current use
in the management of RA." One review suggests that of
the various alternative medicine treatments evaluated,
only acupuncture, bee
venom
acupuncture,
herbal
remedies, dietary omega-3 fatty acids, and pulsed
electromagnetic field therapy have been studied with RCTs
and show promise in treating the pain of RA, though no
definitive conclusions could be reached.(99)
Dietary supplements
The American College of Rheumatology states that no
herbal medicines have health claims supported by high
quality evidence and thus they do not recommend their
use. There is no scientific basis to suggest that herbal
supplements advertised as "natural" are safer for use than
conventional medications as both are chemicals. Herbal
medications, although labeled "natural", may be toxic or
fatal if consumed. Some evidence supports omega-3 fatty
94
acids and gamma-linolenic acid in RA. The benefit from
omega-3 appears modest but consistent, though the
current evidence is not strong enough to determine that
supplementation with omega-3 polyunsaturated fatty
acids (found in fish oil) is an effective treatment for
RA. Gamma-linolenic acid, which may reduce pain, tender
.joint count and stiffness, is generally safe
The following natural herbal treatment show promise as
treatments for RA, based on preliminary studies: boswellic
acid,
curcumin,
Devil's
claw, Euonymus
.alatus, and Thunder god vine (Tripterygium wilfordii)
Herbal supplements can often have significant side
effects, and can interact with prescription medications
being taken at the same time. These risks are often
exacerbated by the false general belief by patients that
herbal supplements are always safe and the hesitancy by
patients in reporting the use of herbal supplements to
physicians. (100)
Manual therapies
The evidence for acupuncture is inconclusive with it
.appearing to be equivalent to sham acupuncture
Prevention
There is no known prevention for the condition. Reduction
of risk factors and aggressive treatment after diagnosis
.are recommended actions
Prognosis
The course of the disease varies greatly. Some people
have mild short-term symptoms, but in most the disease is
progressive for life. Around 20%30% will have
subcutaneous nodules (known as rheumatoid nodules);
.this is associated with a poor prognosis
Prognostic factors
95
,Poor prognostic factors include
Persistent synovitis
Early erosive disease
Extra-articular findings
rheumatoid nodules)
(including
subcutaneous
Positive serum RF findings
Positive serum anti-CCP auto-antibodies
Carrier-ship of HLA-DR4 "Shared Epitope" alleles
Family history of RA
Poor functional status
Socioeconomic factors
Elevated
acute
phase
response
(erythrocyte
sedimentation rate [ESR], C-reactive protein [CRP])
Increased clinical severity.
Mortality
RA is known to reduce the lifespan of patients by
anywhere from three to 12 years. Positive responses to
treatment may indicate a better prognosis. A 2005 study
by the Mayo Clinic noted that RA sufferers suffer a doubled
risk of heart disease, independent of other risk factors
such as diabetes, alcohol abuse, and elevated cholesterol,
blood pressure and body mass index. The mechanism by
which RA causes this increased risk remains unknown; the
presence of chronic inammation has been proposed as a
contributing factor. It is possible that the use of new
biologic drug therapies extends the lifespan of people with
RA and reduces the risk and progression of
96
atherosclerosis. This is based on cohort and registry
studies, and still remains hypothetical. It is still uncertain
whether biologics improve vascular function in RA or not.
There was increase in total cholesterol and HDLc levels
and no improvement of the atherogenic index. (100)
Table (4) Comparison between Osteoporosis,
Osteoarthritis and Rheumatoid Arthritis (Risk
Factors)
97
Risk Factors
osteoporosi osteoarthriti
s
s
Age-related
Menopause
Family history
Use of certain
medications (e.g.,
glucocorticoids,
seizure medications)
Calcium deficiency
or inadequate
vitamin D
Inactivity
Overuse of joints
X
Excessive alcohol
Anorexia nervosa
Excessive weight
Smoking
Rheumatoid arthritis
98
Table (5) Comparison between Osteoporosis,
Osteoarthritis and Rheumatoid Arthritis (Physical
Effects)
Physical
Effects
Affects
entire
skeleton
osteopor osteoarth Rheumat
osis
ritis
oid
arthritis
X
Affects
joints
Is an
autoimmu
ne disease
Bony
spurs
Enlarged
or
malformed
joints
Height
loss
99
Table (6) Comparison between Osteoporosis,
Osteoarthritis and Rheumatoid Arthritis (Treatment
Options)
Treatment
Options
Osteopor Osteoarthr Rheumat
osis
itis
oid
Arthritis
Raloxifene
Bisphosphonates
Calcitonin
Parathyroid
hormone
Estrogen/hormon
e therapy
RANK ligand
(RANKL) inhibitor
Calcium and
vitamin D
Weight
management
100
Glucocorticoids
NSAIDs
X
X
Methotrexate
Diseasemodifying
antirheumatic
drugs, biologic
response
modifiers, tumor
necrosis factor
inhibitors.
Table (7) Comparison between Osteoporosis,
Osteoarthritis and Rheumatoid Arthritis (Pain
Management)
Pain Management
Osteoporosi
s
Osteoarthritis
Rheumatoid
Arthritis
Pain medication
(e.g., NSAIDS,
narcotics, muscle
relaxants)
Rehabilitation
Support groups
Exercises: postural
Exercises:
isometric, isotonic,
isokinetic
101
Joint splinting
Physical therapy
Passive exercises
Hip fracture
surgical repair (may
include hip
replacement
depending on type
of fracture)
Joint replacement
surgery (usually for
pain, malformation,
or impaired
mobility)
Heat and cold
Massage therapy
Acupuncture
Intra-articular ozone injection in
osteoarthritis
At 2012 , Professor Chen H , in Shanghai faculty of
medicine , China had performed an experimental theory
on rats with rheumatoid arthritis .The objectives of this
study were to observe the therapeutic effect of ozone (O3)
of
different
concentrations
on
rat
with rheumatoid arthritis (RA), and to investigate the role
of O3 in regulating the level of TNF- (tumor necrosis
factor), TNF-R1 (tumor necrosis factor receptor 1), and
TNF-R2. Forty-eight Wistar rats were randomly divided into
eight groups. There are five O3 groups which were marked
by 10, 20, 30, 40, and 50 gamma /mL, respectively,
102
control group, oxygen group, and RA model group. RA was
induced in all rats by hypodermic injection of collagen II
and completes Freund's adjuvant except that in the control
group. At 21 days after modeling, the rats in oxygen group
were given an injection of oxygen in the knee joint weekly
for 3 weeks, and the rats in O3 groups were injected the
concentration of O3 as they marked weekly for 3 weeks.
The thickness of hind paw, as well as the serum and
synovial levels of TNF-, TNF-R1, and TNF-R2 was
observed. At the end of treatments, the thickness of the
hind paws in O3-40 group is much less compared to RA
group (P < 0.01). The serum levels of TNF-, TNF-R1, and
TNF-R2 showed no significant difference among all the
groups (P > 0.05). However, the synovial levels of TNF-
and TNF-R2 in O3-40 and O3-50 groups are lower than
those in RA group (P < 0.01). The synovial level of TNF-R1
in O3-40 group is higher than that in RA group (P < 0.05).
In conclusion, intra-articular injection of O3 at 40 g/mL
can effectively suppress the joint swelling caused by RA.
This mechanism is probably mediated by down-regulating
synovial TNF- and TNF-R2 and up-regulating TNF-R1 in
the joint. (101)
In Healthy Healing Center 2011, Professor John Mathew
had tried a combination of physiotherapy and intraarticular ozone injections on a resistant case of 60 years
old female patient who was diagnosed as osteoarthritis
right knee 5 years earlier. This patient had tried different
techniques to help her painful swollen right knee. The
effect of these techniques were never satisfactory for
her .at last her orthopedic surgeon had decided joint
replacement as the best way to relief her pains. Professor
John started her treatment as follows:
One intra-articular ozone injection per week for ten
weeks into the right knee (2cc at a concentration of 20
microgram per milliliter)
Infra Red Heat therapy on the right knee after every
treatment session
Daily supplementation with active calcium and
magnesium salts, as well as capsules containing
chondroitin sulphate and glucosamine
103
Initially use of two walking sticks instead of one, in
order to also relieve the left knee of the extra burden.
Weight management through a diet plan with the
intention to help her achieve a more ideal weight for her
height of 50 Kgs to 60 Kgs.
And these were the results:
1.
After 4 sessions or two weeks of treatment, the
pain in her right knee decreased. The muscles started to
get loosened up, facilitating a smoother movement of the
knee joint. She found it easier to walk.
2.
For the first time in years, she could put some
weight on the right knee after 12 sessions, or six weeks of
treatment. She also could walk for longer stretches than
before. The swelling around the knee joint was
considerably reduced by then, too.
3.
After 20 sessions she was able to ex the knee
to 90 degrees and could keep that posture for 10 to 15
minutes. At this point in the development, she started to
use a bicycle for about half an hour per day, at low speed.
The swelling in the knee had disappeared altogether. She
also felt energetically and emotionally stable and stronger
that before.
4.
After 40 sessions or six months of treatment she
was able to walk without the support of a stick. She had
also lost 18 Kgs and now weighed 70 Kgs. She suspended
the treatment for a while, however continued following the
established diet plan.
When she consulted the orthopedic surgeon, he told her
that according to present clinical signs and symptoms she
did not need knee replacement surgery any longer. (102)
In 2006, at the Orthopedic and Neurological Recovery and
Rehabilitation Unit, S. Anna Hospital; Brescia. Professor
Benvenuti had treated acute and chronic disease of the
large joints (knee, shoulder, and hip) by intra and periarticular injections of micro-doses of an oxygen ozone gas
mixture. The patients were assessed before and after
treatment. In addition to a resolution of joint pain, patients
had a good functional recovery of their daily activities and
the treatment was well-tolerated.
He treated 100 cases that were diagnosed as knee
osteoarthritis by injecting micro-doses of oxygen ozone
mixture (30 to 50 gamma / ml). The injections were given
104
twice weekly for 10 successive weeks' .the results were
magnificent as 95 % of the patients improved perfectly at
the end of the sessions. One week after the first treatment
session there was a rapid reduction of joint swelling and
pain with a recovery of bilateral joint function (exion
120). At the end of the five weekly injections knee
swelling had subsided with almost total remission of pain
and a complete recovery of function (going up and down
stairs, walking, putting on socks) (103)
In 2014, at Faculty of medicine, University Ovidius
Constanta by Dr. Iliescu M. This study was aimed at
showing the evolution of the pain and of the body system
functioning in knee osteoarthritis for patients who were
given ozone therapy only, compared to the patients who
followed the physiotherapy in the Balneary Sanatorium
Vraja Marii in Eforie South. Taking into account that the
physiotherapy treatment is contra-indicated or restricted
to patients with chronic rheumatologic diseases and who,
in many cases, show associated cardio-vascular pathology
(high blood pressure, coronary disease, AVC after-effects,
etc.), ozone therapy can be an efficient alternative. This
study was carried out in the period between 01.07.2013
and 15.12.2013, within the Balneary Sanatorium Vraja
Marii Eforie South. There have been included in the study
100 patients with clinical symptomatology of primary
bilateral knee osteoarthritis, diagnosed according to the
criteria of the American College of Rheumatology, with
radiological modifications on Kellgren- Lawrence (II-III)
scale, with functional result effected by filling in the
questionnaire WOMAC, patients aged between 50 and 65
years old, with the average duration of the disease longer
than 12 months. There have not been included the
patients with secondary gonarthrosis (gout, rheumatoid,
polyarthritis, psoriasis arthritis, TBC arthritis, etc.). They
used doses of 2-5 g/ml, 40-50 ml 03. Several infiltrations
at the knee level are given, in doses of maximum 5 ml on
injection point [8, 9]. At the end of the infiltrations the
patient is invited to move several times in successive
exion/extension motions for a better distribution of the
gas at the level of articulation and also at the level of
recurrences. 12 treatment sessions for each patient.
Physiotherapy in the form of hydro-thermotherapy, mud
105
and paraffin packing. The evaluation of the patients was
done on the first day and after 4 weeks by means of index
score of the arthrosis (Western Ontario and MC Master
Universities Osteoarthritis Index- WOMAC). Both physical
therapy and ozone therapy are efficient in reducing the
pain, proven by the WOMAC score for patients with knee
osteoarthritis, having radiological score Kellgren- Lawrence
2, with unsatisfactory response to the therapy with nonsteroid and condroprotective anti-inammatory drugs. The
ozone therapy, even when used as the only therapy,
brings further benefits, considerably relieving the pain and
the WOMAC score and having a high impact upon the
functional systems and quality of life. It also shows a
major advantage for the patients with contraindications
for physiotherapy, it is a low invasive procedure, well
tolerated by the patient and with considerably low costs
related to its results. (104)
The main goals of treatment of osteoarthritis are to relief
pain, achieve optimal joint function and mobility and
educate the patients regarding avoidance of precipitating
and aggravating factors. (105)
Invasive managements are possibly better for those
patients showing no or mild improvement after
conservative treatment for 3 6 months , mild or no
radiological deformity , pain , stiffness and physical
.disability score by WOMAC less than 2
Intra-articular injection of steroids, lignocaine and
hyaluronic acid has been tried showing moderate effect.
(106)
The intra-articular injection of ozone oxygen mixture in
the therapeutic concentration (30 micrograms / ml of
ozone in oxygen) shows great response in relief of pain,
stiffness and physical disability without any significant
.adverse effect
106
Ozone has excellent analgesic and anti-inammatory
effects as it blocks phosphodiesterase A2 which is
responsible for articular inammation. (107)
A course of 6 intra-articular injections of ozone in
concentrations 7 - 10 ml in 10 ml of oxygen associated
with 12 injections of peri-articular injections of
concentrations 3 -5 ml in 10 ml of oxygen has been tried
in the treatment of degenerative osteoarthritis showing
marked improvement in pain relief and physical
. instability
This
course
should
be repeated yearly to achieve
.maximum benefits of ozone therapy
In cases of rheumatoid arthritis, the association of
systemic
ozone
therapy
either
through
major
autohemotherapy or rectal insufflations will help against
the autoimmune pathophysiology of the disease. (108)
The use of intra-articular ozone injection is effective as a
line of treatment of chronic arthritis. It produces analgesic,
anti-inammatory and Immunoregulatory effects.
1- In osteoarthritis :
It shows anti-inammatory effect as it produces the
following:
It decreases IL-1 and TNF alpha factors which are
responsible for MMP synthesis, Prostanoid synthesis
and Chondrocyte apoptosis.
It acts as a growth factor promoting cartilage repair
by:
a) Enhancing expression of IL-1 ra
b) Enhancing expression of proteoglycans
c) Enhancing Chondrocyte proliferation(109)
2-In Rheumatoid Arthritis :
It decreases B lymphocytes activation
inhibiting the activation of HLA DR
through
107
It decreases TNF alpha released by B lymphocytes.
TNF alpha is responsible for inammation of joints
It decreases plasma cells formation produced by B
lymphocytes. Plasma cells are responsible for the
rerelease of IL1, IL5 and IL6 which are responsible for
immune complex inammation at the joint site. (110)
The use of intra-articular ozone is safe showing almost no
side effects. It also decreases the need of medical
treatment with its hepatic, renal and gastrointestinal
toxicity.
Intra-articular ozone is considered as a cheap method for
relieving pain and disability of osteoarthritis. Compared
with the cost of medical treatment and physiotherapy, it
can help the patient to continue his independent life. (111)
Clinical experience
In the Naval Hyperbaric Medical Institute, we manage the
patients of knee osteoarthritis with intra-articular ozone
injections. Over the last 18 months, 100 patients were
given the intra-articular ozone injections.
108
Description of patients
The treated group was formed of:
1) 95 females and 5 males
2) 70 patients were degenerative osteoarthritis and 30
patients were rheumatoid arthritis
3) 90 patients were complaining from bilateral knee
osteoarthritis.
68
patients
of
the
degenerative
osteoarthritis group were bilateral while 22 patients from
the rheumatoid arthritis group were bilateral.
4) All patients complaining from bilateral osteoarthritis
received intra-articular and peri-articular ozone injections
in both knees in the same cession.
5) The sum of joints treated with ozone injections was 190
joints.
Methods of diagnosis and follow up:
Patients were diagnosed as osteoarthritis by the following
measures:
1) Clinical examination:
Patients were examined for presence of:
a) Pain
b) Swelling
c) Crepitus
d) Range of movement
e) Stiffness
2) Radiological examination:
Plain x-ray knee was done to reveal the criteria of
osteoarthritis:
109
a) Narrowing of the intra-articular space
b) Line of sclerosis
c) Presence of osteophytes
3) Laboratory tests which included:
a) Complete blood count
b) Erythrocyte sedimentation rate
c) C reactive protein
d) Serum uric acid
e) Rheumatoid factor (Rose Walaar test)
These tests were made at days 0, 6, 12
Protocol of ozone administration:
Intra-articular ozone injections were done as follow:
1) 6 intra-articular ozone injections with concentrations
ranging from 70 100 gammas per injection.
2) 12 peri-articular ozone injections with concentrations
ranging from 30 50 gammas per injection
3) In the early 6 cessions, patient received both intraarticular and peri-articular injections
4) In the late 6 cessions, patients received only the periarticular injections
5) follow up by clinical examination, radiological
investigation and laboratory investigations was done on
days 6 and 12
110
Results
1) 75 patients showed improvement in their clinical
examination and laboratory investigations after the first
course with a percentage of 75 % success
2) 20 patients showed mild improvement and they
received a second course after 3 weeks that revealed
improvement in 14 patients raising the results to 89 %
3) 5 patients showed no improvement what so ever after
the first course with a percentage of 5%
4) 6 patients showed no more improvement after second
course
5) Out of the 75 improved patients, 60 patients were
degenerative osteoarthritis while 15 patients were
rheumatoid arthritis.
6) Out of the non improved patients, 4 were rheumatoid
arthritis and one patient was degenerative osteoarthritis.
7) Out of the 20 patients who received a second course, 9
patients were degenerative osteoarthritis while 11
patients were rheumatoid arthritis.
8) Out of the 14patients who improved after the second
course, 8 patients were degenerative osteoarthritis and 6
patients were rheumatoid arthritis.
9) Out of the 25 patients who did not improve after the
first course, 22 patients were obese
10) Out of the 11 patients who did not respond to
treatment, 7 patients were obese.
11) 40 patients returned after one year complaining of
appearance of manifestations of osteoarthritis. Those
patients received another course of intra-articular ozone
therapy and all of them improved.
111
12) Patients with bilateral arthritis from degenerative
osteoarthritis or rheumatoid arthritis show almost the
same response in both knees.
Analysis of the results
1) Degenerative osteoarthritis showed marked response to
intra-articular ozone therapy
2) Rheumatoid arthritis showed fair respond to intraarticular ozone therapy
3) Obesity delays the response of osteoarthritis to intraarticular ozone therapy. Obese patients mostly need to
repeat the course after 3 weeks.
4) Rheumatoid arthritis patients may need the
combination of the systemic ozone therapy and the local
intra-articular ozone therapy.
5) The ozone therapy should be repeated every year to
maintain a good response.
112
Recommendations
After the study of the nature and properties of ozone
and the pathogenesis of both degenerative
osteoarthritis and Rheumatoid arthritis, the following
recommendations should be considered:
The intra-articular ozone injection is safe and
effective in both degenerative osteoarthritis and
rheumatoid arthritis.
Intra-articular ozone therapy should be considered as
an adjuvant therapy in treatment of degenerative
osteoarthritis and rheumatoid arthritis.
Medical treatment and physiotherapy should be
continued during treatment with intra-articular ozone
injections.
The intra-articular ozone injection course can be
repeated after 3 months in non responding cases.
Patients with degenerative osteoarthritis and
rheumatoid arthritis should be advised to receive
intra-articular ozone course every year to maintain
the improvement in their condition. However, if there
is no symptoms, follow up yearly is advised.
113
Obese patients should undergo weight reduction
before receiving the intra-articular ozone.
Patients with rheumatoid arthritis can receive both
systemic ozone administrations (rectal insufflations)
in addition to the local intra-articular ozone injection.
The addition of systemic ozone with its immuneregulatory properties will help the improvement of
both
the
articular
and
the
extra-articular
manifestations of rheumatoid arthritis.
References
1)
Rubin, Mordecai B. (2001). "The History of
Ozone.
The
Schnbein
Period,
1839
1868" (PDF). Bull. Hist. Chem. 26 (1). Retrieved
2008-02-28.
2)
Streng, A. G. (1961). "Tables of Ozone
Properties". Journal
of
Chemical
Engineering
Data6 (3): 431436.
3)
Today in Science History". Retrieved 2006-0510.
4)
Jacques-Louis Soret (1865). "Recherch sur la
densit de l'ozone". Comptes rendus de l'Acadmie
des sciences 61: 941.
5)
6)
"Ozone FAQ". Global Change Master Directory.
Retrieved 2006-05-10.
Brown, Theodore L.; LeMay, H. Eugene, Jr.;
Bursten, Bruce E.; Burdge, Julia R. (2003) [1977].
"22". In Nicole Folchetti. Chemistry: The Central
Science (9th Ed.). Pearson Education. pp. 882
883. ISBN 0-13-066997-0.
7)
Mack, Kenneth M.; Muenter, J. S. (1997). "Stark
and Zeeman properties of ozone from molecular
114
beam
spectroscopy". Journal
of
Chemical
Physics 66 (12): 52785283.
8)
Horvath M., Bilitzky L., Huttner J. (1995). Ozone.
Elsevier. pp. 4449. ISBN 0-444-99625-7.
9)
Bocci V. (2005).Ozone. A New Medical Drug
10)
Housecroft, C. E.; Sharpe, A. G. (2004). Inorganic
Chemistry (2nd Ed.). Prentice Hall. p. 439. ISBN 9780130399137.
11)
"Measured
Ozone
Depletion". OzoneInformation.com. Archived from the original on 201309-14. Retrieved 2014-01-22
12)
Hoffmann, Ronald (January 2004). "The Story of
O". American Scientist 92 (1): 23.
13)
http://www.webmd.com/vitamins supplements /
ingredient mono-1233ozone%20therapy .asp x ?
active
ingredient
id
=
1233&activeingredientname=ozone%20therapy
14)
The Use of Ozone in Medicine: A Practical
Handbook by Renate Viebahn. Medicine Biologica;
Auage: 3rd (Mrz 1999)
15)
Oxygen Healing Therapies : For Optimum Health
and Vitality by Nathaniel Altman Healing Arts Press;
Revised & enlarged edition (September 1, 1998)
16)
Awatchi Y.C. Ansari G.A. Awatchi S. (2005)
Regulation of 4-hydroxynonenal mediated signaling
by Glutathione S-transferase. Methods Enzymol
404,379-407.
17)
Bocci V. (2002) Oxygen-Ozone Therapy. A
Critical Evaluation, 404 pp. Khwer Academic
Publisher, Dordrecht, the Netherlands.
18)
Bocci v. (2005) Ozone. A new Medical Drug. 295
pp. Springer, Dordrecht, the Netherlands, 2005.
19)
Bocci V. (2007). The Case of Oxygen Ozone
Therapy. Brit J Biomed Sci64, 553-560.
20)
Renate Viebahn-Haensler, The Use of Ozone in
Medicine, 4th English edition (Iffezheim: Odrei
Publishers, 2002), 44-47
115
21)
Ed
McCabe, Flood
Your
Body
with
Oxygen (Miami Shores: Energy Publications, 2003),
297.
22)
G. A. Boyarinov et al., Dissolution of Ozone in
Physiological Saline, Proceeding of the 3rd AllRussian scientific-practical conference: Ozone &
Methods of Efferent Therapy in Medicine (Nizhniy
Novgorod, 1998), 6-9.
23)
S.N. Gorbunov ET. al., "The Use of Ozone in the
Treatment of Children Suffered Due to Different
Catastrophies," Ozone in Medicine: Proceedings
Eleventh Ozone World Congress (Stamford, CT:
International Ozone Association, Pan American
Committee, 1993), M-3-31-33
24)
S.N. Gorbunov ET. al., "The Use of Ozone in the
Treatment of Children Suffered Due to Different
Catastrophies," Ozone in Medicine: Proceedings
Eleventh Ozone World Congress (Stamford, CT:
International Ozone Association, Pan American
Committee, 1993), M-3-31-33
25)
Diaz, S., Menendez, S., Eng, L., and Fernandez,
I., 1995, No increase in sister chromatid exchanges
and micronuclei frequencies in human lymphocytes
exposed to ozone in vitro, in Proceedings Ozone in
Medicine 12th World Congress of the International
Ozone Association, 15th to 18th May 1995, Lille
France (International Ozone Association, Ed.),
Instaprint S.A., Tours, pp. 4352
26)
Conaghan P. "Osteoarthritis National clinical
guideline for care and management in adults" (PDF).
Retrieved 2008-04-29.
27)
Centers for Disease Control and Prevention
(CDC) (February 2001). "Prevalence of disabilities
and associated health conditions among adults-United States, 1999". MMWR Morb. Mortal. Wkly.
Rep. 50 (7): 1205. PMID 11393491.
116
28)
E Figueiredo EC, Figueiredo GC, Dantas RT
(December
2011).
"Inuncia
de
elementos
meteorolgicos
Na
dor
de
pacientes
com
osteoartrite: Reviso da literatura" [Inuence of
meteorological elements on osteoarthritis pain: a
review of the literature]. Rev Bras Rheumatol (in
Portuguese) 51 (6):
622
8. Doi:
10.1590
/S048250042011000600008. PMID 22124595.
29)
Valdes AM, Spector TD (August 2008). "The
contribution
of
genes
to
osteoarthritis".
Rheumatology Diseases Clinic North Am. 34 (3):
581603.
30)
Van der Kraan, PM; van den Berg, WB (April
2008). "Osteoarthritis in the context of ageing and
evolution. Loss of chondrocyte differentiation block
during ageing." Ageing Research Reviews 7 (2): 106
13.
31)
Valdes AM, Spector TD (August 2008). "The
contribution
of
genes
to
osteoarthritis".
Rheumatology Diseases Clinic North Am. 34 (3):
581603.
32)
Spector TD, MacGregor AJ (2004). "Risk factors
for osteoarthritis: genetics". Osteoarthr. Cartil. 12
Suppl A: S39-44. Doi: 10.1016 /j.joca.2003.09.005.
PMID 14698640.
33)
http://www.webmd.com/osteoarthritis/guide/und
erstanding-arthritis-basics
34)
Ee P, Rooney PJ, Sturrock RD, Kennedy AC, Dick
WC. The etiology and pathogenesis of osteoarthrosis:
a review. Semin Arthritis Rheum. Spring 1994;
3(3):189-218.
Loughlin J. The genetic epidemiology of human
primary osteoarthritis: current status. Expert Rev Mol
.Med. May 24 2005; 7(9):1-12. [Medline]
(35
Altman R., Asch E., Bloch D., Bole G., Bornstein D.,
Brandt K., et al. (1996) Development of criteria for
(36
117
the classification and reporting of osteoarthritis.
Classification of osteoarthritis of the knee. Diagnostic
and Therapeutic Criteria Committee of the American
Rheumatism Association. Arthritis Rheum 29: 1039
1049
Andriacchi T., Mundermann A., Smith R., Alexander
E., Dyrby C., Koo S. (2004) A framework for the in
vivo pathomechanics of osteoarthritis at the
knee. Ann Biomed Eng 32: 447457
(37
attur M., Patel I., Patel R., Abramson S., Amin A.
(1998) Autocrine production of IL-1 beta by human
osteoarthritis-affected cartilage and differential
regulation of endogenous nitric oxide, IL-6,
prostaglandin E2, and IL-8. Proc Assoc Am
Physicians 110: 6572
(38
ayral X., Pickering E., Woodworth T., Mackillop N.,
Dougados M. (2005) Synovitis: a potential predictive
factor
of
structural
progression
of
medial
tibiofemoral knee osteoarthritis results of a 1 year
longitudinal
arthroscopic
study
in
422
patients. Osteoarthritis Cartilage 13: 361367
(39
Blaney Davidson E., van der Kraan P., van den Berg
W. (2007) TGF-beta and osteoarthritis. Osteoarthritis
Cartilage 15: 597604
(40
bondeson J., Blom A., Wainwright S., Hughes C.,
Caterson B., van den Berg W. (2010) The role of
synovial macrophages and macrophage-produced
mediators in driving inammatory and destructive
responses in osteoarthritis. Arthritis Rheum 62: 647
657
(41
Osteoarthritis. 9 April 2013. Mayo Foundation for
Medical Education and Research. Retrieved April 17,
(42
118
2013,
from http://www.mayoclinic.com/health/osteoarthritis
./DS00019
Viscosupplementation: Managed Care Issues for
Osteoarthritis of the Knee. May 2007. Journal of
Managed Care Pharmacy. Retrieved April 17, 2013,
fromhttp://www.amcp.org/data/jmcp/May07_suppl.pd
.f
(43
Osteoarthritis. Feb 2012. American College of
Rheumatology. Retrieved April 21, 2013, from
http://www.rheumatology.org/practice/clinical/patient
.s/diseases_and_conditions/osteoarthritis.asp
(44
Petersson IF, Boegrd T, Saxne T et-al. Radiographic
osteoarthritis of the knee classified by the Ahlbck
and Kellgren & Lawrence systems for the
tibiofemoral joint in people aged 35-54 years with
chronic knee pain. Ann. Rheumatology Diseases.
1997; 56 (8): 493-6
(45
Altman R., Asch E., Bloch D., Bole G., Bornstein D.,
Brandt K., et al. (1996) Development of criteria for
the classification and reporting of osteoarthritis.
Classification of osteoarthritis of the knee. Diagnostic
and Therapeutic Criteria Committee of the American
Rheumatism Association. Arthritis Rheum 29: 1039
1049
(46
Hart DJ, Spector TD. The classification and
assessment of osteoarthritis. In: Silman AJ, Symmons
DPM, eds. Classification and assessment of
rheumatic diseases: Part I. London: Baillire Tindall,
.1995: 407-32
(47
48)
Sawitzke AD, et al. The effect of glucosamine
and/or chondroitin sulfate on the progression of knee
osteoarthritis:
A
report
from
the
119
glucosamine/chondroitin arthritis intervention trial.
Arthritis & Rheumatism. 2008; 58:3183.
Fransen M, Crosbie J, Edmonds J. Physical therapy is
effective for patients with osteoarthritis of the knee:
a randomized controlled clinical trial. J Rheumatol
2001;28(1):156-164.PM:11196518
(49
Clegg DO, Reda DJ, Harris CL et al. Glucosamine,
chondroitin sulfate, and the two in combination for
painful knee osteoarthritis N Engl J Med
2006;354(8):795-808. PM:16495392
(50
Beaulieu AD, Peloso PM, Haraoui B et al Once-daily,
controlled-release Tramadol and sustained-release
diclofenac relieve chronic pain due to osteoarthritis:
a randomized controlled trial. Pain Res Manag 2008;
13(2): 103-110. PM:18443672
(51
Handout on Health: Rheumatoid Arthritis". National"
Institute of Arthritis and Musculoskeletal and Skin
Diseases. April 2009. Retrieved 2013-03-26
(52
53)
Landr-Beauvais
AJ
(1800). La
goutte
asthnique
primitive
(doctoral
thesis).
Paris. Reproduced in Landr-Beauvais AJ (2001). "The
first description of rheumatoid arthritis. Unabridged
text of the doctoral dissertation presented in
1800". Joint Bone spine 68 (2): 13043.
Turesson C, O'Fallon WM, Crowson CS, Gabriel SE,
Matteson
EL
(2003). "Extra-articular
disease
manifestations in rheumatoid arthritis: incidence
trends and risk factors over 46 years". Ann.
Rheumatology Diseases 62 (8): 7227. Robbins,
(54
120
Stanley Leonard; Kumar, Vinay; Abbas, Abdul K.;
Cotran, Ramzi S.; Fausto, Nelson (2010). "Robbins
and Cotran pathologic basis of disease". In Vinay
Kumar, Abul K. Abbas, Nelson Fausto. Robbins
Pathology Series (Elsevier). p. 205.ISBN 978-1-4160.3121-5
http://www.webmd.com/rheumatoid arthritis / guide /
.rheumatoid-arthritis-symptoms
(55
Rheumatoid Lung Disease What Is Rheumatoid
Lung Disease?" Arthritis.about.com. February 27,
.2011. Retrieved March 3, 2011
(56
57)
De
Groot
K
(August
2007).
"[Renal
manifestations in rheumatic diseases]".Internist
(Berl) 48 (8): 77985. Avia-Zubieta JA, Choi HK,
Sadatsafavi M, Etminan M, Esdaile JM, Lacaille D
(2008). "Risk of cardiovascular mortality in patients
with rheumatoid arthritis: a meta-analysis of
observational
studies". Arthritis
Rheum. 59 (12):
16901697.Doi: 10.1002/art.24092. PMID 19035419.
58)
Scott DL, Wolfe F, Huizinga TW (Sep 25, 2010).
"Rheumatoid arthritis". Lancet 376 (9746): 1094
108.
Cutaneous
manifestations
associated
with
rheumatoid arthritis.[Rheumatol Int. 2009]
(59
The spectrum of cutaneous lesions in rheumatoid
arthritis: a clinical and pathological study of 43
patients.[J Cutan Pathol. 2003]
(60
Cutaneous vasculitis update: neutrophilic muscular
vessel and eosinophilic, granulomatous, and
lymphocytic
vasculitis
syndromes.[Am
J
Dermatopathol. 2007]
(61
121
62)
Fujita M, Igarashi T, Kurai T, et al. Correlation
between dry eye and rheumatoid arthritis activity.
Am J Ophthalmol 2005; 140:808
63)
Sarnat
RL,
Jampol
LM.
Hyperviscosity
retinopathy secondary to polyclonal gammopathy in
a patient with rheumatoid arthritis. Ophthalmology
2006; 93:124.
Blendis LM, Parkinson MC, Shilkin KB, Williams R.
Nodular regenerative hyperplasia of the liver in
Felty's syndrome. Q J Med. 1994 Jan;43(169):25-32
(64
65)
Baer AN, Dessypris EN, Krantz SB. The
pathogenesis of anemia in rheumatoid arthritis: a
clinical and laboratory analysis. Semin Arthritis
Rheum 2009; 19:209.
66)
Papadaki HA, Kritikos HD, Valatas V, et al.
Anemia of chronic disease in rheumatoid arthritis is
associated with increased apoptosis of bone marrow
erythroid cells: improvement following anti-tumor
necrosis factor-alpha antibody therapy. Blood 2002;
100:474.
67)
Singleton JD, West SG, Reddy VV, Rak KM.
Cerebral vasculitis complicating rheumatoid arthritis.
South Med J 2005; 88:470.
68)
Chowdhry V, Kumar N, Lachance DH, et al. An
unusual presentation of rheumatoid meningitis. J
Neuroimaging 2005; 15:286.
69)
Starosta
MA,
Brandwein
SR.
Clinical
manifestations and treatment of rheumatoid
pachymeningitis. Neurology 2007; 68:1079.
70)
http://www.niams.nih.gov/Health_Info/Bone/Oste
oporosis/Conditions_Behaviors/osteoporosis_arthritis.
asp
Franklin J, Lunt M, Bunn D, Symmons D, Silman A
(2006). "Incidence of lymphoma in a large primary
(71
122
care derived cohort
polyarthritis". Annals
of
cases of inammatory
of
the
Rheumatic
.Diseases 65 (5): 617622
Efthimiou P, Kukar M (2010). "Complementary and
alternative medicine use in rheumatoid arthritis:
proposed mechanism of action and efficacy of
commonly
used modalities.
Rheumatology
international 30 (5):
57186.
http://www.nhs.uk/Conditions/Rheumatoid-arthritis
/Pages /Causes.aspx
(72
http://www.hopkinsarthritis.org/arthritis-info/
rheumatoid-arthritis/ra-pathophysiology-2
(73
74)
Firestein GS. Etiology and pathogenesis of
rheumatoid arthritis. In: Ruddy S, Harris E, Sledge C
(Eds): Kelly's Textbook of Rheumatology. 6th ed.
Philadelphia: WB Saunders, 2001, 921-966.
Kirkham BW, Lassere MN, Edmonds JP, et al: Synovial
membrane cytokine expression is predictive of joint
damage progression in rheumatoid arthritis. A twoyear prospective study (the DAMAGE Study Cohort).
Arthritis Rheum. 2006, 54: 1122-1131
(75
Harris ED. Clinical features of rheumatoid arthritis.
In: Ruddy S, Harris E, Sledge C (Eds): Kelly's Textbook
of Rheumatology. 6th ed. Philadelphia: WB Saunders,
2001, 967-1000
(76
77)
Gonzalez-Juanatey C, Llorca J, Testa A, et al:
Increased
prevalence
of
severe
subclinical
atherosclerotic findings in
long-term treated
rheumatoid arthritis patients without clinically
evident atherosclerotic disease. Medicine. 2003, 82:
407-413.
123
Vaudo G, Marchesi S, Gerli R, et al: Endothelial
dysfunction in young patients with rheumatoid
arthritis and low disease activity. Ann Rheum Dis.
2004, 63: 31-35
(78
http://www.rheumatology.org/practice/clinical/patient
/s/diseases_and_conditions/rheumatoid_arthritis
(79
80)
Whiting PF, Smidt N, Sterne JA, et al. Systematic
review: accuracy of anti-citrullinated Peptide
antibodies for diagnosing rheumatoid arthritis. Ann
Intern Med 2010; 152:456.
81)
Finckh A, Liang MH. Anti-cyclic citrullinated
peptide antibodies in the diagnosis of rheumatoid
arthritis: bayes clears the haze. Ann Intern Med
2007; 146:816.
82)
Lee DM, Schur PH. Clinical utility of the anti-CCP
assay in patients with rheumatic diseases. Ann
Rheumatology Diseases 2003; 62:870.
83)
Aletaha D, Neogi T, Silman AJ, et al. 2010
rheumatoid arthritis classification criteria: an
American College of Rheumatology/European League
Against Rheumatism collaborative initiative. Ann
Rheum Dis 2010; 69:1580.
84)
Maksymowych
WP,
Suarez-Almazor
ME,
Buenviaje H, et al. HLA and cytokine gene
polymorphisms in relation to occurrence of
palindromic rheumatism and its progression to
rheumatoid arthritis. J Rheumatol 2002; 29:2319.
85)
Mekinian A, Braun T, Decaux O, et al.
Inammatory
arthritis
in
patients
with
myelodysplastic
syndromes:
a
multicenter
retrospective study and literature review of 68 cases.
Medicine (Baltimore) 2014; 93:1.
SugimotoH,
rheumatoid
Takeda A, Hyodo K. Early-stage
arthritis: prospective study of the
(86
124
effectiveness
of
MR
imaging
for
diagnosis.Radiology2000; 216: 569575
StoneM, Bergin D, Whelan B, Mahrer M, Murray J,
McCarthy C. Power Doppler ultrasound assessment
of rheumatoid hand synovitis. J Rheumatol2001;
28: 19791982
(87
NarvaezJA, Narvaez J, Roca Y, Aguilera C. MR imaging
assessment of clinical problems in rheumatoid
arthritis. Eur Radiol2002; 12: 18191828
(88
Goodman, A. New Rheumatoid Arthritis Guidelines
Released. Medscape Medical News. Available
athttp://www.medscape.com/viewarticle/806789.
Accessed June 26, 2013
(89
Smolen J, on behalf of the EULAR Task Force. Session
10:
update
of
EULAR
rheumatoid
arthritis
management recommendations. Presented at:
EULAR 2013, the Annual Congress of the European
League Against Rheumatism; Madrid, Spain; June 15,
2013
(90
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT,
Bingham CO 3rd, et al. 2010 Rheumatoid arthritis
classification criteria: an American College of
Rheumatology/European
League
Against
Rheumatism collaborative initiative. Arthritis Rheum.
Sep 2010;62(9):2569-81
(91
Anderson J, Caplan L, Yazdany J, et al, for the
American College of Rheumatology. Rheumatoid
arthritis disease activity measures: American College
of Rheumatology Recommendations for use in
clinical practice. Arthritis Care Res (Hoboken).
2012;64:640-7
(92
125
American College of Rheumatology/The European
League against Rheumatism. The 2011 ACR/EULAR
definitions of remission in rheumatoid arthritis
clinical
trials.
Available
at
http://www.rheumatology.org/
practice
/clinical
/classification /ra/ra_remission_2011.asp. Accessed
May 21, 2012
(93
Van der Heijde D, Tanaka Y, Fleischmann R, Keystone
E, Kremer J, and Zerbini C, et al. Tofacitinib (CP690,550) in patients with rheumatoid arthritis
receiving methotrexate: twelve-month data from a
twenty-four-month phase III randomized radiographic
study. Arthritis Rheum. Mar 2013;65(3):559-70
(94
Van der Heijde D, Tanaka Y, Fleischmann R, Keystone
E, Kremer J, and Zerbini C, et al. Tofacitinib (CP690,550) in patients with rheumatoid arthritis on
methotrexate: 12-Month data from a 24-month
Phase 3 randomized radiographic study. Arthritis
Rheum. Jan 24 2013
(95
Callhoff J, Wei A, Zink A, Listing J. Impact of biologic
therapy on functional status in patients with
rheumatoid arthritis--a meta-analysis. Rheumatology
(Oxford). Dec 2013;52(12):2127-35
(96
Solomon SD, Wittes J, Finn PV, et al, for the Cross
Trial Safety Assessment Group. Cardiovascular risk of
celecoxib in 6 randomized placebo-controlled trials:
the cross trial safety analysis. Circulation. Apr 22
2008;117(16):2104-13
(97
Nam JL, Villeneuve E, Hensor EM, Conaghan PG, Keen
HI, Buch MH, et al. Remission induction comparing
iniximab and high-dose intravenous steroid,
followed
by
treat-to-target:
a
double-blind,
randomized, controlled trial in new-onset, treatment-
(98
126
naive, rheumatoid arthritis (the IDEA study). Ann
Rheum Dis. Aug 29 2013
99)
Chen H1, Yu B, Lu C, Lin Q. Rheumatol Int. 2013
May; 33(5):1223-7.
100) http://healthyhealingcentergoa.blogspot.com/20
11/06/intra-articular-ozone-injections-as.html
101) P. Benvenuti. Oxygen-Ozone Treatment of the
Knee, Shoulder and Hip. Rivista Italiana di OssigenoOzonoterapia 5: 135-144, 2006
102) Ciobotaru Camelia, Iliescu Madalina, Mandru
Tatiana, Panait Marilena, Arghir OanaThe role of
ozone therapy in maintaining the articular function
and in relieving the pain for patients with knee
osteoarthritis . ARS Medica Tomitana - 2014; 1(76):
10.2478/arsm-2014-0005
Bocci V et Al: Ozonoterapia. Comprensione de I
meccamismi di ozione e possibilita theraputiche. I Ed
.Milano. Casa Editrice Ambrosiana 2000 730
(103
Ikonomidis ST. Iliakis E et Al: Non operative
treatment of knee osteoarthritis with topical
injections of medical oxygen ozone mixture. A
double blind clinical trial. Rivista Italiana di Ossigene
. ozonoterapia 1: 37-40, 2002
(104
Zhang W, Moskowitz RW, Nuki G et Al. ORASI
recommendations for the management of hip and
knee osteoarthritis, Part 2: ORASI evidence-based,
expert consensus guidelines. Osteoarthritis Cart.
.2008; 16:137-62
(105
De Lucas JC. Intra-articular Ozone Injections.
Indications, techniques and clinical experience. Rev
.Soc Esp. Dolor .2005; 12 N. Extra. 2:37-47
(106
Greene, W. Essentials
2nd edition. American
(107
of
Musculoskeletal Care.
Academy of Orthopedic
Surgeons. 2001
127
(108
Mellion,
M.,
Walsh,
M., Shelton,
G.
The
nd
Team Physician Handbook. 2 edition. Mosby.2007
(109
Reid,
D.
Sports Injury
Assessment and
.
.Rehabilitation. Churchill Livingstone. 2002
) ( .
.
. 3
. 48
128
.
.
.
.
.
) 64000(
.
.
:
= =
129
:
-1
-2
-3
-4
-5
-6
-7
) 5
(
.
)) superoxide dismutase
130
.
.
131
132
133
2014
You might also like
- The New Oxygen Prescription: The Miracle of Oxidative TherapiesFrom EverandThe New Oxygen Prescription: The Miracle of Oxidative TherapiesRating: 5 out of 5 stars5/5 (16)
- Hydrogen Medicine: Combining Oxygen, Hydrogen, and Co2From EverandHydrogen Medicine: Combining Oxygen, Hydrogen, and Co2Rating: 5 out of 5 stars5/5 (2)
- The-Story-of-Ozone-Sixth EditionDocument56 pagesThe-Story-of-Ozone-Sixth Editionyackov100% (1)
- Ozone Therapy Is Safest Known TherapyDocument35 pagesOzone Therapy Is Safest Known Therapyherdin2008100% (1)
- Bio-Xidative Therapies Ozone Oxygen H2o2Document240 pagesBio-Xidative Therapies Ozone Oxygen H2o2santana2013100% (5)
- Ozone Therapy in PracticeDocument42 pagesOzone Therapy in PracticeANNINOS45100% (1)
- Oxygen/ Ozone: IntegratingDocument4 pagesOxygen/ Ozone: IntegratingaksarfNo ratings yet
- Ozone TherapyDocument15 pagesOzone Therapyebar86100% (5)
- Ozone - A Wide Spectrum Healer by Gary Null PHDDocument20 pagesOzone - A Wide Spectrum Healer by Gary Null PHDangelakimba100% (4)
- Ozone Therapy in Dental PracticeDocument14 pagesOzone Therapy in Dental PracticekarthikNo ratings yet
- Ozone TherapyDocument24 pagesOzone TherapyDadoBabylobas100% (2)
- Medical Ozone Therapy MilestonesDocument8 pagesMedical Ozone Therapy MilestonesAdrian Alex100% (2)
- Ozone TherapyDocument42 pagesOzone Therapyonyak100% (1)
- Eliminating Chronic Fatigue & More With Ozone TherapyDocument10 pagesEliminating Chronic Fatigue & More With Ozone TherapyDr. Mark Stengler100% (2)
- Medical Ozone TherapyDocument3 pagesMedical Ozone Therapykrishna2205No ratings yet
- Italia Final Version - Ozone Therapy in Covid-19 - 18 July 2021 - Maria Emilia Gadelha SerraDocument155 pagesItalia Final Version - Ozone Therapy in Covid-19 - 18 July 2021 - Maria Emilia Gadelha SerraCybelle LiraNo ratings yet
- Ozone Therapy Indications and ApplicationsDocument22 pagesOzone Therapy Indications and ApplicationsAcupuntura de Equinos50% (2)
- Ozone Ear Insufflation 2Document3 pagesOzone Ear Insufflation 2blackcat54No ratings yet
- The Story of OzoneDocument58 pagesThe Story of OzoneTee R Taylor100% (1)
- Medical Ozone Therapy Applications and IndicationsDocument22 pagesMedical Ozone Therapy Applications and Indicationsweb3351No ratings yet
- Ozone Unsung Hero by Navy Captain - Ajit VadakayilDocument153 pagesOzone Unsung Hero by Navy Captain - Ajit Vadakayilsudhir shahNo ratings yet
- Ozone Therapy in Female InfertilityDocument6 pagesOzone Therapy in Female InfertilityzafarNo ratings yet
- Ozone Ear InsufflationDocument4 pagesOzone Ear Insufflationblackcat54No ratings yet
- 145641335X-Principles and Applications of Ozone Therapy - A Practical Guideline For Physicians by M D HM 0Document6 pages145641335X-Principles and Applications of Ozone Therapy - A Practical Guideline For Physicians by M D HM 0dinofoxiNo ratings yet
- 2018 Clinical Ozone TheraphyDocument8 pages2018 Clinical Ozone TheraphyEmre ÇebiNo ratings yet
- Ozono ProtocolosDocument9 pagesOzono ProtocolosJust meNo ratings yet
- Oxygen-Ozone Therapy - A Critical Evaluation PDFDocument446 pagesOxygen-Ozone Therapy - A Critical Evaluation PDFScott100% (3)
- 0207 ProlotherapyDocument36 pages0207 ProlotherapyRia PuputNo ratings yet
- Mold Toxins Richard Loyd MDDocument4 pagesMold Toxins Richard Loyd MDOliver QueenNo ratings yet
- The Miracle of Ozone TherapyDocument3 pagesThe Miracle of Ozone Therapydhesmarleni100% (1)
- Ozone Therapy in Holistic MedicineDocument9 pagesOzone Therapy in Holistic MedicineAnonymous DqeRRe50% (2)
- Ozone Therapy For Complex Regional Pain SyndromeDocument5 pagesOzone Therapy For Complex Regional Pain SyndromeRafael BohnenbergerNo ratings yet
- Ultimate Fountain of Youth ProtocolDocument12 pagesUltimate Fountain of Youth ProtocolChristian100% (1)
- Hydrogen Therapy For Diabetic Erectile DysfunctionDocument4 pagesHydrogen Therapy For Diabetic Erectile DysfunctionIhorNo ratings yet
- Ozone GeneratorDocument16 pagesOzone GeneratorEduardo BarbosaNo ratings yet
- Beck Protocol HandbookDocument87 pagesBeck Protocol Handbookatideva100% (2)
- A Metaanalysis of The Effectiveness and Safety of Ozone Treatments For Herniated Lumbar DiscsDocument51 pagesA Metaanalysis of The Effectiveness and Safety of Ozone Treatments For Herniated Lumbar DiscsPazhanisamy MurugaianNo ratings yet
- Electrotherapy in The Treatment of Cancer and VirusesDocument178 pagesElectrotherapy in The Treatment of Cancer and VirusespitumestresNo ratings yet
- The Amazing Schweitzer FormulaDocument3 pagesThe Amazing Schweitzer FormulaCarlos SolergibertNo ratings yet
- MB 0457Document14 pagesMB 0457Isabel RosendoNo ratings yet
- Understanding PleomorphismDocument20 pagesUnderstanding PleomorphismDavid100% (2)
- Dr. James Howenstine - Simple Cure For TinnitusDocument4 pagesDr. James Howenstine - Simple Cure For Tinnitussuni3dayNo ratings yet
- Dr. Katz'S Aktivoxigen Ozonator: Specifically Designed To Rapidly Ozonate Liquids & OilsDocument16 pagesDr. Katz'S Aktivoxigen Ozonator: Specifically Designed To Rapidly Ozonate Liquids & Oilstyber100100% (3)
- Ozone Science & Nikola Tesla - Ozone History & Nikola TeslaDocument64 pagesOzone Science & Nikola Tesla - Ozone History & Nikola Teslakrishna2205100% (4)
- The Wolff-Chaikoff Effect: Questioning the 'Crying Wolf' NarrativeDocument7 pagesThe Wolff-Chaikoff Effect: Questioning the 'Crying Wolf' NarrativeMo'men El-MassryNo ratings yet
- Methode EBOODocument37 pagesMethode EBOOjohanNo ratings yet
- 2.about - Humic Fulvic - Substances.1Document35 pages2.about - Humic Fulvic - Substances.1BrianNo ratings yet
- Biomedx BEV Station BrochureDocument2 pagesBiomedx BEV Station BrochurebiomedxNo ratings yet
- IodineDocument7 pagesIodinePetra JobovaNo ratings yet
- Ozon Madrid - Declaration PDFDocument24 pagesOzon Madrid - Declaration PDFututel100% (1)
- Oxygen-Ozone Autohaemotherapy and Intravescical Oxygen-Ozone Insufflations in Treatment of Recurrent and Interstitial Cystitis: Preliminary ResultsDocument3 pagesOxygen-Ozone Autohaemotherapy and Intravescical Oxygen-Ozone Insufflations in Treatment of Recurrent and Interstitial Cystitis: Preliminary ResultsSabrina JonesNo ratings yet
- Dokumen - Tips - Detoxification Healing Dietrich KlinghardtDocument23 pagesDokumen - Tips - Detoxification Healing Dietrich KlinghardtakiniramNo ratings yet
- Binders - What Are They and Why Use Them-5nov'22-FinalDocument5 pagesBinders - What Are They and Why Use Them-5nov'22-Finalvitaolga7No ratings yet
- Darkfield Images Bicom2000Document9 pagesDarkfield Images Bicom2000Brigitte Nolan100% (1)
- KEROSENE - A Universal Healer by Walter LastDocument9 pagesKEROSENE - A Universal Healer by Walter LastĀryaFaṛzaneḥ100% (2)
- Petroleum enDocument4 pagesPetroleum enz987456321100% (1)
- The Different Types of Electrotherapy DevicesDocument4 pagesThe Different Types of Electrotherapy DevicescassianohcNo ratings yet
- Electricity For Health PDFDocument49 pagesElectricity For Health PDFlpsiahaan100% (5)
- Adhaota Vasica (Malabar Nut)Document7 pagesAdhaota Vasica (Malabar Nut)ABHINABA GUPTANo ratings yet
- Social Relationships in Middle and Late AdolescentDocument9 pagesSocial Relationships in Middle and Late AdolescentNesta Norhyl BayonaNo ratings yet
- MedEx FAQDocument2 pagesMedEx FAQJee CHIUN CHENNo ratings yet
- International Congress 1263Document12 pagesInternational Congress 1263AksMastNo ratings yet
- r147229149 Jenny Valdirio CUR147229149Document1 pager147229149 Jenny Valdirio CUR147229149Jenny Valdirio PozzoNo ratings yet
- Introduction of PhobiaDocument2 pagesIntroduction of PhobiawoodenskyNo ratings yet
- KAP regarding BSE among womenDocument30 pagesKAP regarding BSE among womenrandika wijesooriyaNo ratings yet
- Internal MedicineDocument5 pagesInternal MedicineFırat GüllüNo ratings yet
- Marijuana Fact SheetDocument1 pageMarijuana Fact Sheetapi-355176759No ratings yet
- Snodgrass (1980) A Standardized Set of 260 Pictures. Norms For Name Agreement, Image Agreement, Familiarity, and Visual ComplexityDocument42 pagesSnodgrass (1980) A Standardized Set of 260 Pictures. Norms For Name Agreement, Image Agreement, Familiarity, and Visual ComplexityΜακίν Ξηροί ΚαρποίNo ratings yet
- Blood Typing PDFDocument3 pagesBlood Typing PDFFrances Lau Yee ChinNo ratings yet
- Monthly Current Affairs Quiz - January 2023: Follow UsDocument244 pagesMonthly Current Affairs Quiz - January 2023: Follow UsSubhankar BasakNo ratings yet
- ASCGULF Company: Mohammad Gousu Basha ShaikDocument3 pagesASCGULF Company: Mohammad Gousu Basha ShaikmohammadgouseNo ratings yet
- Definition of Sexual Abuse of ChildrenDocument2 pagesDefinition of Sexual Abuse of ChildrenRadhika RathoreNo ratings yet
- Dynamic Learning Plan 2-Lesson 2Document27 pagesDynamic Learning Plan 2-Lesson 2Cyrah OntiverosNo ratings yet
- Commentary: Novel Application For G Protein - Biased Mu Opioid Receptor Agonists in Opioid Relapse PreventionDocument2 pagesCommentary: Novel Application For G Protein - Biased Mu Opioid Receptor Agonists in Opioid Relapse PreventionIntan AyuNo ratings yet
- Cancer Lesson Plan For High SchoolDocument7 pagesCancer Lesson Plan For High SchoolUm IbrahimNo ratings yet
- Nursing Process in Drug TherapyDocument60 pagesNursing Process in Drug TherapyYra JhaneNo ratings yet
- Occurrence and Health Risk Assessment of Pharmaceutical and Personal Care Products (PPCPS) in Tap Water of ShanghaiDocument8 pagesOccurrence and Health Risk Assessment of Pharmaceutical and Personal Care Products (PPCPS) in Tap Water of ShanghaiTiago TorresNo ratings yet
- ACTION PLAN FOR JUVENILE PRISONERS IN ILOILO CITYDocument22 pagesACTION PLAN FOR JUVENILE PRISONERS IN ILOILO CITYJohn Christian LopezNo ratings yet
- Mds Periodontics Thesis TopicsDocument7 pagesMds Periodontics Thesis Topicsamyholmesmanchester100% (2)
- Lection 8 SyphilisDocument39 pagesLection 8 SyphilisAtawna AtefNo ratings yet
- Exercise Chart: Warm UpDocument1 pageExercise Chart: Warm UpJeremy van der MerweNo ratings yet
- Annex 2 7d PEMAPS QuestionnaireDocument5 pagesAnnex 2 7d PEMAPS QuestionnaireAlma PustaNo ratings yet
- Non-Steroid Analgesic, Antipyretic, Anti-Inflammatory and Anti-Allergy DrugsDocument217 pagesNon-Steroid Analgesic, Antipyretic, Anti-Inflammatory and Anti-Allergy DrugsAstri DesmayantiNo ratings yet
- Health Disparities BrochureDocument2 pagesHealth Disparities Brochureapi-276375030100% (1)
- Nursing Abbreviations, Acronyms and Symbols QuizDocument3 pagesNursing Abbreviations, Acronyms and Symbols QuizAjeng Citra S SeptiyantriNo ratings yet
- Planning and Design of A Cell and Tissue Culture Laboratory: Christopher B. MorrisDocument2 pagesPlanning and Design of A Cell and Tissue Culture Laboratory: Christopher B. MorrisSubaNo ratings yet
- Administering Blood Transfusion GuideDocument1 pageAdministering Blood Transfusion GuideKyla ManarangNo ratings yet
- Trends, issues, and magnitude of psychiatric nursingDocument4 pagesTrends, issues, and magnitude of psychiatric nursingsona0% (1)