Professional Documents
Culture Documents
Alport Syndrome A Review
Uploaded by
RodrigoBarreraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Alport Syndrome A Review
Uploaded by
RodrigoBarreraCopyright:
Available Formats
ELS EVI E R
Clinical Eye and Vision Care 12 (2000) 139-150
www.elsevier.com/locate/clineyeviscare
Clinical review
Alport syndrome: a review
Patricia A. McCarthy, Dominick M. Maino"
Illinois College of Optometry, 3241 S. Michigan Ave., Chicago, IL 60616, USA
Accepted 28 January 2000
Abstract
Alport syndrome, a hereditary nephritis accompanied by high-tone sensorineural deafness and distinctive ocular signs was
first noted in the literature during the early 1900s. This disease is caused by a genetic defect in Type IV collagen which makes
up basement membranes in many body systems. The patient will usually have bilateral anterior lenticonus causing varied
refractive errors. You may also note yellow-white to silver flecks within the macular and midperipheral regions of the retina.
The treatment of the visual problems is an important but secondary concern due to the seriousness of the systemic disease.
Dual sensory loss, however, creates an urgent need for appropriate vision care. Due to the high risk for developmental delay
and decreased social integration, early intervention should be considered in the treatment plan. Coping strategies for the
patient (and the family) need to be addressed because of the chronicity of this syndrome. The primary care optometrist will be
challenged by the individual with Alport syndrome since a balance between oculo-visual, developmental/psycho-educational
and systemic care is required. A multi-disciplinary approach by the healthcare management team will enhance the quality of
life and positive outcomes for these patients. 0 2000 Elsevier Science Ireland Ltd. All rights reserved.
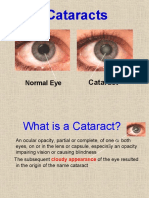
Keywords: Hereditary nephritis; Lenticonus; Alport syndrome; Deafness; Cataracts; Flecked retinopathy; Developmental delay; Early
intervention programs
1. Introduction
Alport syndrome, a hereditary nephritis accompanied by high tone sensorineural deafness and distinctive ocular signs [1-3] was first reported in the
early 1900s. Guthrie described several cases of familial idiopathic hematuria and suggested maternal genetic transmittance 141. Alport linked the hematuria
with the auditory defects and noted that the severity
of the disease corresponded to gender [5]. The ocular
signs were initially discussed by Sohar in 1954 with
50% of the cases studied demonstrating spherophakia
[6]. Flecked retinopathy involving the macular and
* Corresponding author. Tel.:
949-7358.
+ 1-312-949-7282; fax: + 1-312-
midperipheral areas may be seen upon fundus examination as well. This syndrome should be included in
the differential diagnosis of any flecked retinopathy
[1,7- 151.
Alport syndrome (AS) is caused by a genetic defect
within one of the alpha chains of the Type IV collagen molecule. Type IV collagen is a major constituent
of basement membranes throughout the body. The
anomalous basement membranes of the ocular, auditory and renal systems cause the characteristic triad
of abnormalities in these patients (i.e. hereditary
nephritis, sensorineural deafness and ocular signs)
[1,16-211. Previous authors have attempted to classify
the characteristics used to diagnose Alport syndrome
and its numerous variants. However, legitimate objections to the current diagnostic parameters exist
[1,3,22-241.
0953-4431/00/$ - see front matter 0 2000 Elsevier Science Ireland Ltd. All rights reserved.
PII: S 0 9 5 3 - 4 4 3 1( 0 0 ) 0 0 0 4 2 - 4
140
P.A. McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000)139-150
A patient presenting with signs of AS will challenge
the optometrists assessment skills due to the variable
nature of the refractive error [12]. One of the primary
concerns, however, must be the diagnosis and management of the systemic disease. A missed diagnosis
of AS in a young male can eventually be fatal due to
end stage renal disease 171. Secondary management
goals should consider developmental and perceptual
delays, management of any psychosocial anomalies,
and the creation of coping strategies for the patient
and his family. Early intervention programs (EIP)
need to be incorporated into the treatment plan on
an individual basis. Appropriate healthcare should
involve the skills of the optometrist, physician, psychologist and early intervention staff. A multi-disciplinary approach by the health-care management team
for AS patients is necessary to maximize their quality
of life and to ensure desired outcomes [25-281.
2. Etiology
2.1. Basement membrane lesion
The signs and symptoms of AS are due to defective
basement membranes in specific organ systems (i.e.
renal, auditory, and ocular systems). Basement membranes (BM) are the subcellular foundations in tissues
and are composed of Type IV collagen. These microscopic platforms are key to the appropriate separation,
maintenance and regeneration of the juxtaposing tissues [ 1,18-211. The glomerular basement membrane
(GBM) is defective in the patients renal system. The
affected kidney loses its ability to filter blood effectively [19]. The stria vascularis of the cochlea and the
lens capsule are also affected [7,29].
2.1.1. Renal system
The GBM is the location of the hallmark nonocular lesion in AS [3,30].The histological description
of this lesion varies within the literature. Thickening
of the basement membrane was initially described
during the 1970s [3]. Recent research has described
the defective membrane as a thinned area with associated regions of additional membrane layers due to
splitting of this tissue [l-31. The splitting of the
membranes coincides with proteinuria that may signify severe renal disease 121.
An interesting contradiction exists between the articles written by Churg and Rumpelt. According to
Rumpelt et al., a combination of thinning and splitting of the GBM in the same glomerulus is the
distinctive renal defect in AS. Thinning of the membrane occurs with subsequent duplication, ultimately
giving a faux layered appearance to the BM. This
lesion, seen upon electron microscopy, was noted to
be diffuse with a range of severity. Eventually, the
split tissues involved a greater area than the thinning
membrane. Neither of these basement membrane entities alone are specific for AS with thickening of the
GBM being a late stage finding [31].
In contrast, Churg et al. described the GBM abnormality as splitting with subsequent thickening of affected areas. The appearance of the renal tissue resembled kidneys previously assessed with deficits in
lipid filtration. This inference supports the hypothesis
of a GBM lesion along with the clinical signs of
hematuria and proteinuria [32].
The onset of the thickening of the GBM appears to
be the primary conflict between the definitions proposed by Rumpelt and Churg. Both studies report
areas of splitting or layering of these membranes. The
number of subjects must be considered when comparing the two studies. Rumpelt studied biopsies from 70
subjects while Churg analyzed specimens from 17
patients [31,32].
2.1.2. Auditory system
The auditory basement membrane lesions have
been difficult to discern due to problems procuring
specimens from AS patients. The stria vascularis of
the cochlea seems to show similar basement changes
to the GBM. Tissue atrophy with cellular loss and
edema may be present as well. The hair cells of the
organ of Corti are affected by this lesion with a
resultant loss of hearing at the higher frequencies
[1,2,71.
2.1.3. Visual system
The best known basement membrane within the
eye, the lens capsule, is also the thickest BM within
the human body [ll]. Streeten et al. [29] identified
three specific histological structures that are affected
in the crystalline lens capsule. First, large fractures
lined with abnormal filaments are distributed in a
honeycomb pattern throughout the central area of the
capsule. Coincident vacuoles containing osmophilic
spheres and membranes have also been identified
with cellular debris found adjacent to these breaks.
Second, the capsules epithelial cells contained distended mitochondria with cells missing from several
layers of the capsule. Third, the lens fibers next to the
thinner, affected capsule also had mitochondria1
swelling with amorphous clumping of the cytoplasm.
Although thinning of the lens capsule does occur with
age, this pathological thinning combined with abnormal epithelial cells and fibers may lead to capsule
fragility. Streeten implied the appearance of the lens
capsule lesion was similar to the Bowmans capsule
BM defect in the renal system of AS patients.
The exact etiology of the defect in these basement
P A . McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000) 139-150
membranes was not initially known. Alport 151 suggested the toxins from Streptococcus were responsible
for this renal disease. Later questions about possible
biochemical abnormalities and problems with tissue
perfusion were considered [31]. The collagenous
structure of the basement membranes became the key
to unraveling some of the uncertainty with this syndrome.
2.2. Type Wcollagen
The flexibility and stability of basement membranes
are largely due to Type IV collagen which comprises
50% (dry wt.) of these structures [3].
Type IV collagen is a non-fibrillar, triple helical
macromolecule composed of three chains. These
chains may be any one of six alpha chains that are
distributed within basement membranes (Table 1 outlines the systemic distribution of these alpha chains
[16,17,19]). Each chain is secreted by a cell and becomes part of the extracellular matrix. The distinguishing features of Type IV collagen include specific
non-collagenous areas (NC1) within the final product
and frequent interruptions within the primary structure of the alpha chains [3-9,16-19,301.
Study of the BM finally gave definitive clues to the
etiology of AS. Two important points were noted
about the alpha 5 chain of Type IV collagen: first, this
chain gives structural stability to the final collagen
molecule. Second, deficiencies within the alpha 5 chain
often cause dysfunction of all three chains of the
collagen product [30,33]. The manufacturing process
of the Type IV collagen molecule may be compromised [19]. Although alpha 5 is present in many
tissues, only some of them are affected in AS [34].
This mystery has yet to be explained.
2.3. COL4A5gene
Gene COL4A5 has been identified as the cause of
the alpha 5 chain anomalies in AS. Genetic loci for
the alpha 1 through 4 chains have been previously
identified on autosomal chromosomes. Hybridization
studies localized COLAAS to the long arm of the X
chromosome, q22-23. Confirmatory in situ studies
were also performed to further localize the gene to
Xq22 [16-181.
Thirty to 40 mutations [20,22] have been described
in the COL4A5 gene, including deletions, insertions,
rearrangements and point mutations. Several small
mutations are worth noting here because of their
catastrophic effect on the final structure of the collagen molecule. Cysteine to serine point mutations [22]
and glycine substitutions [19] disrupt the fabrication
of the collagen product. Also, any mutations within
the NC1 domains can disturb the alignment of the
141
Table 1
Localization of Type IV collagen alpha chains [16,17,19]
Alpha 1 and 2
Renal glomerular basement
membrane (GBM)
Skin
Nerve
Muscle
Vascular
Alpha 3 and 4
Renal GBM
Muscle
Vascular
Ocular
Alpha 5
Renal GBM
Skin
Ocularb
Alpha 6
Gastrointestinal
Pulmonary
Mesangial matrix
Vascular BM"
Tubular BM
Bowman's capsule
Epidermal BM
Endoneurium
Perineurium
Extrasynaptic muscle fibers
Blood vessels, specifically arterial
Distal tubule BM
Bowman's capsule
Synaptic muscle fiber BM
Aorta (low levels only with
alpha 1 & 2)
Lens capsule BM (low levels with
alpha 1 & 2)
Epidermal BM
Cornea epithelial BM
Descemet's membrane
Vascular BM of choroid
Eesophagus
Lung
"BM, basement membrane
bWithin rabbit eyes.
chains of the collagen molecule and disrupt many
intermolecular interactions [ 191. The clinical presentation of AS may parallel the severity of the mutation.
In one study, the severity of the hearing loss did
correspond with the mutation while another study
identified that no obvious correlation between genotype and phenotype existed 122,331.
3. Inheritance
Within the United States, the genetic frequency
ranges from 1/5000 to 1/10000. The higher end of
this range has been documented in the Western states
with Utah having twice the incidence of this syndrome
when compared to the rest of the US. Spontaneous
mutations have been noted in 15518% of the cases
with mutations occurring in 1/100000 gametes. Finally, AS is not biased toward any particular race or
geographic area [1,21.
3.1. X-linked inheritance
COLAAS has been definitively implicated through
X-linkage to AS [2,16-181. Currently, 85% of these
P.A. McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000)139-150
142
patients have an X-linked dominant inheritance pattern [3,21].This particular type of transmission causes
severe disease in the male patient and a varied presentation of the syndrome in females [2]. The broad
range of phenotypes for women is caused by random
inactivation of one X chromosome causing two populations of cells within organ systems (lyonization)
12,351.
3.2. Autosomal inheritance
Approximately 15% of all cases of AS are due to
autosomal inheritance [3,19,21]. Autosomal recessive
(AR) inheritance has been cited as a rare occurrence
with the lesion involving the long arm of chromosome
2. This would involve the genes of the alpha 3 and 4
chains of Type IV collagen [36]. Autosomal dominant
(AD) transmission of this syndrome is questionable
[22]. (This will be discussed later in the paper.) Atkin
et al. also has questions about AD inheritance in AS
due to a reduction in individuals advancing to severe
renal disease. Reduced penetrance with AD inheritance should result in an increased amount of end
stage renal disease (ESRD) in some AS patients as
they age. Autosomal dominance should be considered
if male-to-male inheritance is discovered within a
pedigree 111.
4. Diagnosis of Alport syndrome and variants
The diagnosis of Alport syndrome seems to offer
additional hurdles to the healthcare provider. Alportlike variants have been described [1,23,37,38]. Recognition of these variants is important for appropriate
management of the patient and their family members.
Atkin et al. 111 categorized this syndrome based on
the different phenotypic expressions, as well as the
knowledge that the severity of AS depends primarily
on the gender and the age of the patient. The principal divisions of the syndrome depend on the onset of
the renal disease (as illustrated in Table 2). (Table 3
further outlines the six types of Alport syndrome and
variants that were described by Atkin accounting for
non-renal signs and symptoms.) As can be seen (Table
Table 2
Juvenile- vs. adult-onset Alport syndrome [l]"
Characteristic
Juvenile
Adult
Inheritance
End stage
renal disease
Auditory deficit
Ocular anomalies
XD, AD
< 31 years old
XD
> 31 years old
100%
Present
Absent
50%
"XD, X-linked dominant; AD, autosomal dominant.
Table 3
Types of Alport syndrome and variants [1Ia
Characteristics
Inheritance
Adult vs. juvenile
Auditory deficit
Ocular anomalies
Subtypes
AS variant
Types
I
I1
I11
IV
VI
XD,AD
J
XD
J
XD
A
XD
A
AD
A/J
AD
J
+
+
+
+
+
-
+
-
+*
+
+
+
"XD, X - linked dominant; AD, autosomal dominant; J, juvenile; A, adult; +, present; -, absent; +*, Epstein syndrome.
31, types I and VI appear quite similar. However, the
type I male patient does not produce offspring secondary to morbidity while the type VI group can
include normal male carriers. Although this system of
classification seemed to simplify the diagnostic
process, Atkin et al. acknowledged the discordance
between the adult versus juvenile criteria [l].
Flinter et al. 1221 has a more specific standard for
definitive diagnosis of classic Alport syndrome. Seventy-five percent of these specifications listed below
must be fulfilled to make the diagnosis. A complete
case history of the disease process in family members
must be obtained before using this criterion. The
rules for the appropriate diagnosis include the following:
1. Hematuria in other family members with or without chronic renal failure (CRF).
2. A kidney biopsy with the characteristic histological lesions (i.e. thickening and splitting of the
GBM).
3. Ocular involvement, specifically, anterior lenticonus and macular flecked retinopathy.
4. Auditory involvement (high-tone sensorineural
deafness) which is progressive.
Amari claims several Alport-like variants may present without ocular involvement and must be kept in
mind when making a differential diagnosis. Hereditary nephritis without deafness or ocular involvement
is one possible variation. Second, Epstein syndrome,
also described as Type V AS, has hematological
deficits, (thrombocytfopathology), in addition to the
renal and auditory lesions. Flechtner syndrome is the
third variant worth considering which presents with
proteinuria and deafness, as well as leukocyte and
platelet abnormalities [ 1,231. Finally, an AS-like
glomerulonephritis with multiple benign tumors of
smooth muscle tissue (leiomyomatosis) has been reported by several authors. The gene associated with
diffuse leiomyomatosis (DL), COL4A6, has also been
mapped to the long arm of the X chromosome. Dele-
P A . McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000)139-150
tions of areas of COLAAS and COLAA6 have been
found in patients with this AS variant [19,23,37,38].
Leiomyomatosis, when associated with AS, presents
with cataracts in addition to hematuria and hearing
loss. This AS variant is important to the optometrist
because it is associated with cataracts. These cataracts
may have an early onset and unilateral presentation.
Twenty-five percent of these patients will have congenital lens opacifications as well. This ocular presentation is not common in patients with AS or esophageal leiomyomatosis alone [ 19,37,38].
Surprisingly, Govan [ 111 suggests that only one of
three ocular features is needed to diagnose Alport
syndrome:
1. Anterior lenticonus.
2. Flecked retinopathy of the macula.
3. Flecked retinopathy of the periphery.
This article appears to disregard the seriousness of
renal disease in this syndrome. The presence of one
of the ocular triad warrants additional systemic investigation before a firm diagnosis of AS is made.
Current variations of the definition of AS may
cause a misdiagnosis by the physician. Exclusion of
X-linked inheritance secondary to male-to-male transmission is the only definitive determination in the
current diagnostic process [24].
5. Patient presentation
5.1. Renal system
What is the typical presentation of a patient with
AS? The most significant organs affected are in the
renal system 171. Hematuria is the earliest clinical sign
[4]. This may be the primary presentation of the
syndrome in children [l]. Guthrie described the
hematuria as a constant finding with variable severity
[4]. AS males have the hematuria from birth with
approximately 80590% of the women showing this
important clinical sign [1,21. The frequency and
amount of hematuria may vary considerably from one
carrier female to another and usually will not result in
ESRD [2,21]. Lyonization probably plays a significant
role in this phenotypic presentation [2,35]. Females
who are carriers (but otherwise healthy) tend to have
intermittent microscopic hematuria 1241.
Systemic hypertension will result with continued
deterioration of the renal system (Table 4 lists a
time-line of renal events for affected individuals [22]).
The onset of auditory anomalies may start at this time
as well [22]. Focal sclerosis of the glomeruli has been
identified as a signal of advancing renal disease with
subsequent proteinuria being a manifestation of the
143
Table 4
Clinical Course of X-linked AS [22Ia
Males
5 years old
10 years old
15 years old
20 years old
25 years old
Microscopic hematuria
High-tone sensorineural deafness
Hypertension
Renal function deterioration
Chronic renal failure
Cam'evfemales
20 years old
25 years old
MA
LTR
Microscopic hematuria
Renal function deterioration (3% of carriers)
Hypertension (1/3 of carriers)
Chronic renal failure (5510% of carriers)
"MA, middle age; LTR, life-time risk.
ultrastructural changes within the GBM. This indicates the severity of the kidney dysfunction [2,30].
To definitively diagnose renal disease, electron microscopy of a kidney biopsy should be performed for
all suspected male and female patients followed by
immunofluorescent evaluation of the tissue [29].
Monoclonal antibody studies of the defective collagen
chains are able to positively identify 75580% of the
affected males and will provide a mosaic pattern in
carrier females 1301. A specific monoclonal antibody,
H51, to the NC1 region of the alpha 5 chain has been
developed. The strong positive feature of this particular antibody is the capability to use it on skin tissue
biopsies, especially if renal biopsies are unattainable
[16]. Future diagnostic assessment techniques will
probably make extensive use of molecular genetics
1301.
5.2. Auditory system
The auditory presentation of bilateral, symmetrical
hearing loss with AS is quite significant [2,7]. Most of
the AS individuals have hearing loss by age 10
[9,14,20,35,39].Auditory manifestations appear to parallel the severity of renal involvement and may be
coincident with the ocular signs [1,5,20]. Females with
AS are less severely affected and the deficit is usually
non-progressive [2,9]. Carrier identification is enhanced via audiology studies since the defect is not
normally manifest in carrier females [39].
The actual defect of the auditory system has been
narrowed down over the years. Anatomically, the middle ear is intact and unaffected 111. The brainstem
also has not shown any significant lesions and cranial
nerve VIII has been ruled out as an etiology [1,12]. A
vestibular component has been identified with this
defect. The patient may present with tinnitis and
vertigo before the detection of the auditory lesion
[1,21. The cochlea is also affected with a loss of
neurons within the organ [7].
The auditory lesion is detected using audiometry.
144
P.A. McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000)139-150
Recently, audioscans 6.e. sweep frequency audiometry using a pulse tone from 250 Hz to 8 kHz at a
30-s/octave rate) have been conducted on these
patients. Detections of very small deficiencies in middle frequency areas have been noted even in carrier
females. Audioscans along with confirmatory linkage
studies may help identify these carriers 1351.
5.3. Ksual system
Ocular anomalies have been noted in 1 1 ~ 4 3 %of
the AS patients studied [7,39,40]. Males have equal or
greater ocular involvement compared to females
[1,9,39,40]. These ocular abnormalities occur in both
the anterior and posterior segments of the globe with
the most common finding being uncorrectable refractive error due to lenticular involvement [l]. Behavioral changes may signify the onset of decreased visual acuity in younger patients. Sudden difficulties
with school, changes in social behavior and increased
mobility problems may be part of the patients presentation [41]. Ocular anomalies (primarily lens changes)
can coincide with poor kidney function which can
progress to renal failure. Lack of ocular signs in
family members is helpful in ruling out AS 1391.
(Table 5 contains a complete list of the ocular findings associated with AS [1,7-15,23,29,33,39,40,42-441.)
The most common of these signs are discussed below.
Table 5
Ocular findings in Alport syndrome
Cornea [1,7,12,39,40,43]
Posterior polymorphous dystrophya
Arcus
Anterior layer thickening
Lattice dystrophy
Recurrent epithelial corneal erosions
White limbal girdle of Vogt
Band keratopathy
Posterior polymorphous opacities
Pigment dispersion syndrome
Crystalline lens [7,9-11,23,29,33,421
Anterior lenticonusa
Posterior lenticonus
Lens coloboma
Cataracts
Anterior pole subcapsular
Anterior axial cortical
Internal lenticonus
Posterior axial
Posterior cortical
Posterior subcapsular (secondary to steroids)
Subcapsular vacuolization
Blue dot opacities
Pundus [1,7-15,44]
Flecked retinopathya
Macular
Midperipheral
Combination
decreased to absent
Foveal reflex
Epiretinal membrane
Optic disc drusen
Retinal telangiectasia
~
5.3.1. Cornea
Two prominent corneal findings frequently encountered in AS individuals are posterior polymorphous
dystrophy (PPMD) and arcus. PPMD is due to the
thickening of Descemets layer with subsequent endothelial cell changes [39]. This basement membrane
appears immature with several layers of Descemets
identified in association with the defective endothelial
cells [ 131. Obviously, compromised endothelial cells
can lead to corneal edema. Iridocorneal adhesions
and transparent membranes due to PPMD cause an
increase risk for glaucoma in these patients [41].
Arcus, although a non-specific finding, has an increased incidence associated with AS 1111. Usually,
the arcus will appear bilaterally with interpalpebral
sparing and tends to be coincident with foam cells
noted on renal biopsy [7,11].
It should be noted that certain corneal abnormalities may be observed in all renal failure patients
regardless of etiology 1451. These findings include
white limbal girdle of Vogt and band keratopathy.
Care must be taken to insure a complete differential
diagnosis of the etiology of the patients renal disease.
5.3.2. Crystalline lens
5.3.2.1. Lenticonus. Bilateral anterior lenticonus has
been noted in Alport syndrome since 1966. Lenti-
Major clinical presentation.
conus appears in men more than women during the
second to third decade of life [1,2,9,10,13,29,33].
Patients will present with variable vision depending
on the surrounding illumination. In photopic conditions, the patient will show myopia. Hyperopia and
monocular diplopia may be manifest in mesopic conditions [12].
When using a parallelepiped or optic section during
biomicroscopy, the lenticonus is seen as an axial protrusion, often conical or nipple-like, within the pupillary zone of the lens. It may also appear as an oil
drop on retroillumination of the pupillary area
[1,2,11,12,29].This lenticular anomaly may produce up
to 30 diopters of measurable myopia [7].
The primary defect for lenticonus lies within the
lens capsule. The paucity of other anterior chamber
defects rules out anomalies during embryogenesis.
The alpha 3-5 chains of Type IV collagen may be
absent or abnormally arranged causing fragility of the
capsule. Normally, the capsule is the thinnest at the
anterior pole and 3 mm radially in the periphery. The
decreased number of epithelial cells and increased
P A . McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000)139-150
capsular thinning allows bulging of the anterior cortex. Besides the anatomical problems with the capsule, manipulation of the lens due to accommodation
and normal growth causes additional stress on an
already weakened structure. This weakness can cause
the capsule to rupture with consecutive formation of
an anterior pole subcapsular cataract [1,11,26,30,42].
Anterior lenticonus is an important indicator of
poor systemic prognosis due to renal disease [7,13,39].
It has been reported that no isolated cases of ocular
changes without renal dysfunction had been noted
1241. At this point, the conscientious optometrist will
consult with a nephrologist since visual changes may
be identified before an actual AS diagnosis is determined [13,15].
5.3.2.2. Spherophakia. Spherophakia is a sudden developmental arrest of the lens with aplastic zonules
and is due to the lack of normal zonules in these
patients. Other authors, however, have suggested that
spherophakia is another name for marked lenticonus
[6,111.
5.3.2.3. Cataracts. Although cataracts are not a specific finding for AS, certain lens opacities are significant for these patients. First, anterior subcapsular
formations can occur secondarily to lens capsule rupture. Second, posterior subcapsular cataracts may appear due to steroid use with post-renal transplant
145
therapy. Third, internal lenticonus may be seen as a
posterior lamellar opacity with a posterior projection
along the visual axis [7,11,421.
5.3.2.4. Lens coloboma. Only one case of lens
coloboma has been reported. Amari et al. stated this
anomaly was not noticeable without dilation. This
defect was presented as a zonular lesion in addition to
the lens malformation. Since zonules are not made of
collagen, a questionable relationship exists between
this particular coloboma and traditional Alport syndrome. However, a correlation between lens colobomas and AS variants has not been ruled out 1231.
5.3.3. Fundus
Alport syndrome must be considered in the differential diagnosis of flecked retinopathy [ 1,7-151 (see
Tables 6 and 7 [1,46-48]). In addition, polycystic kidney disease and medullary cystic disease may cause a
similar fundus appearance [49]. (The characteristics of
these renal diseases are listed in Table 8.) The flecked
retinopathy of AS does not affect visual function of
the patient and is often noted by the clinician only if
fundus photographs are taken [1,11]. The flecks may
be seen in the macular region, midperiphery or both
with sparing of the fovea [1,7-151.
5.3.3.1. Macula. The macula is frequently affected
in AS [11,15]. Men are usually affected more than
Table 6
Differential diagnosis of inherited flecked retinopathies [1,46,47]"
Alport syndrome
Fundus
flavimaculatus
Stargardt syndrome
XD, AD, AR
Bilateral
macular to
Flecks
midperiphery, yellow
to white with ( - )
foveal reflex, pigment
changes, all retinal
levels
normal
EOG
AR
Bilateral, symmetric
fish-tail
Flecks
yellow-white,
posterior pole at RPE
level
AR
Bilateral, symmetric
fish-tail,
Flecks
beaten bronze,
central or peripheral
fundus
ERG
normal
EOG
ERG
mild
abnormal
normal to
FA
normal to
hyperfluorescent
hyper 2nd to
FA
atrophy
No significant VA
loss
Complications
red/green defects,
central scotomas,
retinal neovasc.,
cystoid mac. edema
No significant VA
loss
normal to
EOG
abnormal
normal to
ERG
abnormal
Retinitis punctata
albescens
Fundus
albipunctatus
white or
Flecks
yellow, scattered
Flecks
discrete
spots, no atrophy
transmission
FA
defects, occ. bull's
eye pattern
Complications
red/green defects,
central scotomas
normal with
EOG
time
ERG
reduced
photopic, normal
scotopic
questionable
FA
pattern
~
severely
ERG
abnormal
~
Complications
contracted fields
worse with time
VA worse than
20/200
aAbbveuiations:XD, X-linked dominant; EOG, electrooculogram; AD, autosomal dominant; FA, fluorescein angiography; AR, autosomal
recessive; ERG, electroretinogram; VA, visual acuity.
P.A. McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000)139-150
146
women during their second to third decade of life.
The flecks are yellowish white to silver, round or oval
and up to 50 p m in diameter. They are usually in a
scattered arrangement but may become confluent.
They lie within the superficial layers of the retina
following the nerve fiber layer (NFL) [1,7-9,11,12].
Retinal pigment epithelium (RPE) changes are also
noted [1,9,13].
There are four important components of the macular flecks: first, an abnormal form of the alpha 5
collagen chain seems likely due to the various retinal
membranes involved [i.e. internal limiting membrane
(ILM), external limiting membrane (ELM), Bruch's
and glia limitans of the vessels]. Second, an opaque
substance appears to be deposited without evidence
of a retinal biochemical abnormality. These deposits
may be collagen with defective alpha 5 chains. Slow
accumulation of these deposits with increasing age is
noted. Third, the deposits tend to be extracellular (if
the flecks were located intracellularly, they would
interfere with normal retinal function). This location
also coincides with other basement membrane lesions
elsewhere in the body. Finally, more than one retinal
layer may be involved with some flecks appearing to
lie deep to the ILM, following the NFL and involving
the retinal vessels [15].
It has been suggested that the macular flecks are a
product of the Miiller cells. Miiller cells are present
in all retinal layers and produce basement membranes. They also compartmentalize the NFL and
form the glia limitans of the vasculature. Normal
retinal function of AS patients indicates a purely
structural defect of the Miiller cells and macular
flecks are not evident within the fovea [15].
5.3.3.2. Midperipheral area. These flecks are similar
to those found in the macular area with a few exceptions. They can be small and round but tend to
coalesce into areas covering up to one-third of a disc
diameter [ll]. Deeper retinal layers are involved with
the flecks being located at the level of the RPE or
Bruch's membrane [9,13,15]. Occasionally, flecks may
be seen in the macular and midperipheral areas of
the same fundus with a bull's eye appearance [ll].
Three major areas of contention regarding flecked
retinopathy due to AS include the amount of vessel
involvement, the appearance on fluorescein angiography (FA) and the results of electrophysiology testing.
The vessel involvement may range from no involvement to encrusting of the vessels with the flecks in a
honey-combed pattern [11,151. FA will show variable
results as well. Some studies detected hyperfluorescence secondary to RPE disruption. Yet, no correspondence seems to exist between the window defects
and the flecks [7,11]. Particular fluorescent patterns
without evidence of leakage may become evident with
disease progression [8,91. Electrophysiology showed
the greatest inconsistencies. Different articles noted
results ranging from the electrooculogram (EOG) and
electroretinogram (ERG) being normal to both
showing subnormal results [1,8-11,141. Visually
evoked potential (VEP) latencies were increased secondary to lens changes in one article reviewed 1141.
The optometrist should realize that, as with the
cornea, electrophysiology results may be abnormally
affected by renal disease [8,11,14]. Decreased b wave
amplitudes on ERG can occur with non-AS renal
failure, dialysis and renal transplantation. Steroid use
and systemic hypertension may also change these
results. Decreased EOG findings can be due to dialysis treatment while increased VEP latencies tend to
correlate with kidney dysfunction [11,14].
5.4. Psychosocial presentation
Children with severe systemic illnesses may face
disruption of normal developmental milestones [28].
Table 7
Differential diagnosis of drug-induced flecked retinopathies [1,48]"
Aport syndrome
Tamoxifen retinopathy
Talc retinopathy
Canthaxanthin retinopathy
macula or
Flecks
midperipheral, yellow to
white with ( - ) foveal reflex,
pigment changes, all
retinal levels
PPMD, arcus
Cornea
Flecks
tiny, white,
refractile at retinal pigment
epithelial level
small, crystal,
Flecks
within vessels
Flecks
gold-dust spots in
inner retina layers
circumventing macula
EOG
ERG
Cornea
opacities
~
white, superficial
EOG
ERG
normal
normal
Complications
mac. edema
No significant VA loss
cystoid
VA
mild to moderate
defect
~
normal
small b wave
disc
Complications
neovasc., ischemia, retinal
detachment, vitreal heme
VA
normal
~
"Abbreviations: PPMD, posterior polymorphous corneal dystrophy; EOG, electrooculogram; ERG, electroretinogram; VA, visual acuity.
P A . McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000)139-150
Table 8
Diffuse familial nephropathies [49]
Polyqstic hidney disease
Adult type
Autosomal dominant
Symptoms/signs:
Abdominal pain
Palpable masses
Hematuria
Proteinuria
Urinary tract infection
Anemia
Cardiovascular involvement
Hypertension
Organ cysts
Ocular:
Retinal dystrophy
Infantile
Autosomal recessive
Symptoms/signs:
Like adult
Urogenital defects
Fatal at an early age
Medullary cystic disease
Inheritance unknown
Symptoms/signs:
Polydipsia
Polyuria
Renal salt wasting
Anemia
Hypertension
Ocular:
Congenital cataracts
Fatal by 40 years of age
Decreased vision and hearing are also high-risk factors for developmental disabilities [50]. Optometrists
need to consider additional multidisciplinary evaluation if the patient presents with signs of developmental delays 6.e. problems with general development,
motor skills, and knowledge). A careful investigation
of socialization skills in young patients should be
considered since bimodal sensory loss in AS patients
can further complicate the socialization process [27].
Children with chronic diseases suffer great psychological stress due to the disease and treatment process.
Adequate coping mechanisms are necessary to master
these added demands with strategies matching the
severity of the illness and age of onset 1281. Unfortunately, emotional regression including apathy can also
occur in young patients with chronic illnesses [51].
Families may be angry and anxious about the situation and blame the medical community for having to
deal with all the different aspects of the disease. They
may become overprotective of the ill individual as a
coping mechanism. This can prevent appropriate development of the patient both academically and socially. The stress of a chronically ill family member
147
can also cause a significant strain and a deterioration
of relationships within the family may be evident [51].
Optometrists and other members of the healthcare
team must be aware of the effect of chronic illness on
a patient and his family. The ability of the child and
his family to cope with the psychological stress of a
chronic illness should be considered when deciding on
appropriate management options [511.
6. Management of the AS patient
The management of a patient who presents with
possible ocular signs and symptoms of Alport syndrome requires a team effort from medical, behavioral, psychosocial and educational specialists. The
primary concern for the optometrist should be to
attain appropriate care for the patient and his family.
When the systemic health of the patient has been
stabilized, the patients sensory, developmental and
emotional anomalies can be appropriately addressed
[7] and several treatment goals should be established
by the healthcare management team [1-3].
Unfortunately no cure is available at this time,
systemic complications secondary to the renal disease
are minimized by controlling hypertension and protein intake [1,2]. Current treatment of ESRD requires
dialysis and/or renal transplantation. Future management of renal disease may include pharmacologic
therapy (i.e. cyclosporin A) [1,3,52]. Treatment of the
hearing deficiency will include management of the
possible ototoxicity side effects when medications for
renal problems are used [1,2]. Reduced vision secondary to lenticular changes are treated with topical
mydriatics or cataract extraction and the application
of lenses [1,11].Intervention programs may be needed
if significant developmental delays are identified
[26,50]. Appropriate coping strategies for the patient
and his family should be considered in the treatment
plan as well [25,28].
6.1. Genetic counseling
Appropriate genetic counseling is essential for the
management for Alport syndrome [3]. Carrier identification is important for the probands family especially if the urinalysis findings are inconsistent [21].
Molecular genetics can be used to determine the
amino acid sequence of the genetic lesion. This is
important since greater than 80% of X-linked disease
is due to a point mutation [21,30].Linkage studies will
frequently confirm the genetic etiology [ll]. Further
renal examinations, including ultrasound and biopsy,
should be conducted 1301.
148
P.A. McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000)139-150
6.2. Renal system treatment
6.2.1. CyclosporinA
The use of cyclosporin A is being studied for management of the kidney disease in these patients. This
drug appears to reduce the proteinuria and may influence systemic regulation of renal function. However, progression to renal failure can still occur. Unfortunately, cyclosporin A has toxic side effects in
renal tissues. Therefore, it is currently not recommended for the treatment of AS until further studies
have been completed [52].
6.2.2. Renal transplantation
Careful screening of potential renal donors must be
implemented both for the health of the donor and the
recipient. Monoclonal antibody studies are used to
screen for genetic patency of the donor [16]. Identified male carriers should be denied as a renal donor
because of possible renal disease progression and the
reduced life-span of these organs. Fortunately, female
carriers may donate a kidney to the patients because
severe renal disease usually will not occur [30,53].
Glomerular basement membrane nephritis, a posttransplant complication, occurs in 3 ~ 4 %of AS individuals. The typical composite of these patients is a
male with sensorineural deafness and ESRD before
30 years of age. Approximately 75% of these cases
occur during the first year and 3/4 of the grafts are
lost. Recurrence of this problem with another transplant is a possibility 1301.
6.3. Auditory management
Significant renal disease accompanied by hearing
loss may be prematurely assessed as Alport syndrome.
Anatomic anomalies, congenital etiologies and middle
ear disease must be ruled out. Therefore, appropriate
referral for audiology testing is indicated. If an AS
diagnosis can be made, the results of the audiology
consult will not only be of prognostic value but will
aid in identification of carriers within the other family
members [1,2,391.
Treatment of the sensorineural hearing loss should
be implemented as warranted [2]. Unfortunately, previous attempts with hearing aids in these patients
have been unsatisfactory. Improved audition after renal transplantation have been cited in the literature
but this does not appear to be the norm. Vision
deficits should be addressed as soon as possible to
enhance communication skills for those with hearing
deficiencies [l].
6.4. Ocular management
The AS patient presenting with posterior polymor-
phous dystrophy may be at risk for glaucoma (GLC)
due to iridocorneal adhesions. GLC medications that
reduce aqueous production are typically used. Filtering surgery is also an option for these patients. Laser
trabeculoplasty, however, is contraindicated due to
the growing membranes in the anterior chamber.
Penetrating keratoplasty (PKP) can be considered a
treatment option in severe cases of reduced vision
due to corneal edema. Unfortunately, preexisting
glaucoma and/or iridocorneal adhesions are poor
prognostic factors for PKP 1541.
The lenticonus and other lens changes need to be
addressed as well. Topical phenylephrine can be
administered if the patient has axial opacities. Care
must be taken if the patient has systemic hypertension by using a dilute concentration. Although the
efficacy of extracapsular cataract extraction (ECCE)
has been questioned, three cases of ECCE were noted
in this review without evidence of a fragile capsule. If
the patient also has posterior lenticonus, the capsular
bag may be stretched during the ECCE procedure to
reduce its magnitude. Steroids used after the transplant can cause a posterior subcapsular cataract (PSC).
Cataract extraction for the lenticonus and PSC is the
treatment of choice [11,55,56].
6.5. Management of psychosocial issues
An optometrist should recommend a developmental evaluation for the patient when decreased vision
and/or hearing is suspect as an etiology for developmental delay. Formal social assessments, such as the
Meadow-Kendall Social-Emotional Assessment Inventory for Deaf and Hearing Impaired Students
should also be administered. This particular inventory
has preschool- and school-aged items to determine
social and emotional adjustment for a child with hearing loss 1271. Placement in an intervention program is
recommended if developmental or social deficiencies
are present. Federal mandates require care for children beginning at 3 years of age when high-risk factors are present. These educational and rehabilitative
programs can assist in the development of intellectual, social and language skills needed in school.
Good communication between optometrists and the
EIP staff can facilitate the incorporation of visual,
perceptual and developmental therapy into daily activities [26,50].
The health management team should work within a
holistic approach to enhance the patients quality of
life. Treatment regimens must be considered for their
effect on the patients life along with their ability to
control symptoms or disease progression. The patients
perception of the disease process can affect his selfesteem and the emotional adjustment to AS [25].
Additional factors affecting the patients coping abili-
P A . McCavthy, D.M. Maino /Clinical Eye and Vuion Cave 12 (2000)139-150
ties include parental coping, family cohesiveness and
intrafamilial communication [28]. Psychological intervention may be needed to assist the patient with
coping strategies for AS. Frequent emotional adjustments by the patient (and the family) to the stages of
the illness and treatment regimens are necessary to
maintain as normal a lifestyle as possible 1251.
7. Conclusion
Alport syndrome offers many challenges to the
optometrist. Patients will present with the characteristic triad of hereditary nephritis, hearing loss and
ocular manifestations. A thorough investigation of the
hereditary nature of this syndrome within a family is
essential for appropriate classification [ 1-31. In addition, a careful investigation of the full cause of the
flecked retinopathy must not be neglected [1,7-151
Conscientious management of the ocular anomalies
should be emphasized to avoid dual sensory disability
[l]. A multi-disciplinary approach in the management
of these patients, including assistance for developmental and social deficiencies, as well as coping
mechanisms, is necessary to minimize detrimental effects on their quality of life and to improve management outcomes.
References
Gregory MC, Atkin CL. Aport syndrome. In: Schrier RW,
Gottschalk CW, editors. Diseases of the kidney. 5th rev. ed.
Boston: Little, Brown and Company, 1993:571-591.
Ancreoli SP, Deaton M. Aports syndrome. Ear Nose Throat
J 1992;71(10):508-511.
Bodzik KA, Hammond WS, Molitoris BA. Inherited diseases
of the glomerular basement membrane. Am J Kidney Dis
1994;23(4):605-618.
Guthrie LG. Idiopathic or congenital, hereditary and family
hematuria. Lancet 1902;1:123-126.
Aport AC. Hereditary familial congenital haemorrhagic
nephritis. Br Med J 1927;1:504-506.
Sohar E. Renal disease, inner ear deafness, and ocular
changes. Arch Intern Med 1956;97:627-630.
Grondalski SJ, Bennett GR. Alports syndrome: review and
case report. Optm Vis Sci 1989;66(6):396-398.
Gelisken 0, Hendrikse F, Schroder CH, Berden JHM. Retinal abnormalities in Aports syndrome. Acta Ophthalmol
(Copenh) 1988;66:713-717.
Polak BCP, Hogewind BL. Macular lesions in Aports disease. Am J Ophthalmol 1977;84(4):532-535.
Bhatnager R, Kumar A, Pakrasi S. Alports syndrome
ocular manifestations and unusual features. Acta Ophthalmol
(Copenh) 1990;68:347-349.
Govan JAA. Ocular manifestations of Aports syndrome: a
hereditary disorder of basement membranes? Br J Ophthalmol 1993;67:493-503.
McCartney PJ, McGuinness R. Alports syndrome and the
eye. Aust New Zealand J Ophthalmol 1989;17(2):165-168.
Sabates R, Krachmer JH, Weingeist TA. Ocular finding in
Aports syndrome. Ophthalmologica 1983;186:204-210.
~
149
Jeffrey BG, Jacobs M, Sa G, Barratt TM, Taylor D, Driss A.
An electrophysiological study on children and young adults
with Alports syndrome. Br J Ophthalmol 1994;78(1):44-48.
Gehrs KM, Pollock SC, Zilkha G. Clinical features and
pathogenesis of Aport retinopathy. Retina 1995;15(4):
305-311.
Yoshioka K, Satoshi H, Takemura T et al. Type IV collagen
a5 chain: Normal distribution and abnormalities in X-linked
Aport syndrome revealed by monoclonal antibody. Am J
Pathol 1994;144(5):986-996.
Hostikka SL, Eddy RL, Byers MG et al. Identification of a
distinct type IV collagen a chain with restricted kidney distribution and assignment of its gene to the locus of X
chromosome-linked Alport syndrome. Proc Natl Acad Sci
USA 1990;87:1606-1610.
Myers JC, Jones TA, Pohjolainen E-R et al. Molecular cloning
of a5(IV) collagen and assignment of the gene to the region
of the X chromosome containing the Alport syndrome locus.
Am J Hum Genet 1990;46:102-1033.
Hudson BG, Reeders ST, Tryggvason K. Type IV collagen:
structure, gene organization, and role in human diseases. J
Biol Chem 1993;268(35):26033-26036.
Zhou J, Leinonen A, Tryggvason K. Structure of the human
type IV collagen COL4A5 gene. J Biol Chem 1994;269 (9):
6608-6614.
Knebelmann B, Antignac C, Gubler MC, Griinfeld JP.
Molecular genetics of Alport syndrome: the clinical consequences. Nephrol Dial Transplant 1993;8:677-679.
Flinter F. Molecular genetics of Aports syndrome. Q J Med
1993;86:289-292.
Amari F, Segawa K, Ando F. Lens coloboma and Aport-like
glomerulonephritis. Dur J Ophthalmol 1994;4(3):181-183.
Flinter FA, Bobrow M, Chantler C. Alports syndrome or
hereditary nephritis? Pediatr Nephrol 1987;1:438-440.
Strauss AL. Chronic illness and the quality of life. St. Louis:
The C.V. Mosby Company, 1975.
Hatch SW. The role of optometry in early intervention. In:
Maino DM, editor. Diagnosis and management of special
populations. St. Louis: Mosby-Year Book, Inc, 1995:283-295.
Luetke-Stahlman B. Social integration: assessment and intervention with regard to students who are deaf. Am Ann Deaf
1995;140(3):295-303.
Boman K, Bodegkd G. Psychological long-term coping with
experience of disease and treatment in childhood cancer
survivors. Acta Paediatr 1995;84(12):1395-1402.
Streeten BW, Robinson MR, Wallace R, Jones DB. Lens
capsule abnormalities in Aports syndrome. Arch Ophthalmol 1987;105:1693-1697.
Kashtan CE, Michael AF. Alport syndrome: from bedside to
genome to bedside. Am J Kidney Dis 1993;22(5):627-640.
Rumpelt H-J. Alports syndrome: specificity and pathogenesis
of glomerular basement membrane alterations. Pediatr
Nephrol 1987;1:422-427.
Churg J, Sherman RL. Pathologic characteristics of hereditary nephritis. Arch Pathol 1973;95(6):374-379.
Cheong HI, Kashtan CE, Kim T, Kleppel MM, Michael AF.
Immunohistologic studies of type IV collagen in anterior lens
capsules of patients with Alport syndrome. Lab Invest 1994;
70(4):553-557.
Barker DF, Hostikka SL, Zhou J et al. Identification of
mutations in the COL4A5 collagen gene in Alport syndrome.
Science 1990;248:1224-1227.
Sirimanna KS, France E, Stephens SDG. Alports syndrome:
can carriers be identified by audiometry? Clin Otolaryngol
1995;20:158-163.
Turco AE, Rossetti S, Bresin E, Corr5 S. Erroneous genetic
150
P.A. McCavthy, D.M. Main0 /Clinical Eye and Vuion Cave 12 (2000)139-150
risk assessment of Alport syndrome [letter]. Lancet 1995;
346:1237.
Lonsdale RN, Robers PF, Vaughan R, Thiru S. Familial
oesophgeal leiomyomatosis and nephropathy. Hisopathology
1992;20:127-133.
Garcia-Torres R, Orozco L. Aport-leiomyomatosis syndrome: an update. Am J Kidney Dis 1993;22(5):641-648.
Thompson SM, Deady JP, Willshaw HE, White RHR. Ocular
signs in Alports syndrome. Eye 1987;1:146-153.
Burke JP, Clearkin LG, Talbot JF. Recurrent corneal epithelial erosions in Aports syndrome. Acta Ophthalmol (Copenh)
1991;69:555-557.
Yeo SMW, Ruben ST, Willshaw HE. Beharioural disturbance
as a manifestation of ocular disease in children [letter]. Br J
Ophthalmol 1995;79:502.
Brownell RD, Wolter JR. Anterior lenticonus in familial
hemorrhagic nephritis. Arch Ophthalmol 1964;71:481-483.
Davies PD. Pigment dispersion in a case of Aports syndrome. Br J Ophthalmol 1970;54:557-561.
Kondra L, Cangemi FE, Pitta CG. Aports syndrome and
retinal telangiectasia. Ann Ophthalmol 1983;15(6):550-551.
Mansour AM. Ocular manifestations of various systemic disorders. Curr Opin Ophthalmol 1994;5(VI):105-109.
Cavender JC, Ai E, Lee ST. Hereditary macular dystrophies.
In: Tasman W, Jaeger EA, editors. Duanes clinical ophthalmology, vol. 3, rev. ed. Philadelphia: Lippincott-Raven Publishers, 1995:l-33.
Carr RE, Heckenlively JR. Hereditary pigmentary degenerations of the retina. In: Tasman W, Jaeger EA, editors. Duanes
clinical ophthalmology, vol. 3, rev. ed. Philadelphia: Lippincott-Raven Publishers, 1995:l-28.
Grant S. Toxic retinopathies. In: Tasman W, Jaeger EA,
editors. Duanes clinical ophthalmology, vol. 3, rev. ed.
Philadelphia: Lippincott-Raven Publishers, 1995:l-15.
Peterson WS, Albert DM. Fundus changes in the hereditary
nephropathies. Trans Am Acad Ophthalmol Otol 1973;
28x762-771.
Britain LA, Golmes GE, Hassanein RS. High-risk children
referred to an early-intervention developmental program. Clin
Pediatr 1995;34(12):635-641.
Work HH. Psychologic reactions of children to physical illness. In: Pasnau RO, editor. Psychosocial aspects of medical
practice: children and adolescents. Menlo Park, California:
Addison-Wesley Publishing Company, 1982:ll-17.
Callis S, Vila A, Nieto J, Fortuny G. Effect of cyclosporin A
on proteinuria in patients with Aports syndrome. Pediatr
Nephrol 1992;6:140-144.
Sessa A, Pietrucci A, Carozzi S et al. Renal transplantation
from living donor parents in two brothers with Alport syndrome. Nephron 1995;70:106-109.
Mandelbaum S. Glaucoma associated with corneal disorders.
In: Tasman W, Jaeger EA, editors. Duaness clinical ophthalmology, vol. 3, rev. ed. Philadelphia: Lippincott-Raven Publishers, 1995:l-13.
John ME, Noblitt RL, Coots SD, Boleyn KL, Ballew C. Clear
lens extraction and intraocular lens implantation in a patient
with bilateral anterior lenticonus secondary to Alports syndrome. J Cataract Refract Surg 1994;20:652-655.
Basti S, Rathi V, Reddy MK, Gupta S. Clear lens extraction
for anterior lenticonus [letter]. J Cataract Refract Surg
1995;21:363-364.
You might also like
- Glaucoma A Symposium Presented at a Meeting of the Chicago Ophthalmological Society, November 17, 1913From EverandGlaucoma A Symposium Presented at a Meeting of the Chicago Ophthalmological Society, November 17, 1913No ratings yet
- Lowe Syndrome (Oculocerebrorenal syndrome) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandLowe Syndrome (Oculocerebrorenal syndrome) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Retina A Model for Cell Biology Studies Part_1From EverandThe Retina A Model for Cell Biology Studies Part_1Ruben AdlerNo ratings yet
- The Skeffington Perspective of the Behavioral Model of Optometric Data Analysis and Vision CareFrom EverandThe Skeffington Perspective of the Behavioral Model of Optometric Data Analysis and Vision CareNo ratings yet
- Glaucoma: Mohd Roslee Bin Abd GhaniDocument42 pagesGlaucoma: Mohd Roslee Bin Abd GhaniSaha DirllahNo ratings yet
- A Review of Anti-Vegf Agents For Proliferative Diabetic RetinopathyDocument7 pagesA Review of Anti-Vegf Agents For Proliferative Diabetic RetinopathyIJAR JOURNALNo ratings yet
- Extracapsular Cataract Extraction (ECCE) Is A Category of Eye Surgery in WhichDocument13 pagesExtracapsular Cataract Extraction (ECCE) Is A Category of Eye Surgery in WhichMa Christina RabayaNo ratings yet
- CorneaDocument18 pagesCorneaDrNarayan KRNo ratings yet
- Alport SyndromeDocument49 pagesAlport SyndromemuslimNo ratings yet
- School Eye Screening and The National Program For Control of Blindness - 2Document6 pagesSchool Eye Screening and The National Program For Control of Blindness - 2rendyjiwonoNo ratings yet
- 30secondary GlaucomasDocument19 pages30secondary GlaucomasShari' Si WahyuNo ratings yet
- Diabetic Retinopathy - Aetiopathogenesis, Clinical Presentation andDocument83 pagesDiabetic Retinopathy - Aetiopathogenesis, Clinical Presentation andOlayemi Olorundare0% (1)
- AION Anterior Ischemic Optic Neuropathy AIONDocument22 pagesAION Anterior Ischemic Optic Neuropathy AIONNyak Rahmat100% (1)
- Primary Angle Closure GlaucomaDocument39 pagesPrimary Angle Closure GlaucomaMaria ShafiqNo ratings yet
- Capsular Bag Distension Syndrome Following Cataract Surgery JournalDocument16 pagesCapsular Bag Distension Syndrome Following Cataract Surgery Journalnaveen ratna KumarNo ratings yet
- Diseases of Lens DR D.JLDocument113 pagesDiseases of Lens DR D.JLNithya GunasekaranNo ratings yet
- By: Noor Majeed RehaniDocument23 pagesBy: Noor Majeed RehaniMihaela Toma0% (1)
- Myopia by NamanDocument19 pagesMyopia by NamanAkshit ChitkaraNo ratings yet
- Early Detection of Hypoxia-Induced Cognitive Impairment Using The King-Devick TestDocument6 pagesEarly Detection of Hypoxia-Induced Cognitive Impairment Using The King-Devick TestDeni Tri HanantoNo ratings yet
- Short Case 1 PterygiumDocument15 pagesShort Case 1 PterygiumAnmol KhadkaNo ratings yet
- A Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaDocument17 pagesA Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaJosé Díaz OficialNo ratings yet
- StrabismusDocument27 pagesStrabismuspason1988No ratings yet
- Anterior Chamber Angle Assessment TechniquesDocument29 pagesAnterior Chamber Angle Assessment TechniquesSabyasachi100% (4)
- Glaucoma LectureDocument166 pagesGlaucoma LectureSonali Gupta100% (1)
- Eye Disorder in Childhood & Adolescent: Lia Meuthia Zaini FK Unsyiah / RSUZADocument54 pagesEye Disorder in Childhood & Adolescent: Lia Meuthia Zaini FK Unsyiah / RSUZACut MulianiNo ratings yet
- Hypertensive RetinopathyDocument46 pagesHypertensive RetinopathyAnadia RahmaNo ratings yet
- CATARACTDocument25 pagesCATARACTDea NabilaNo ratings yet
- Hyphema 2Document7 pagesHyphema 2heidyNo ratings yet
- Congenital Disorders of The CorneaDocument100 pagesCongenital Disorders of The Corneaeyemd_in_trainingNo ratings yet
- Lens and CataractDocument55 pagesLens and CataractRold Brio Sos100% (1)
- PUPILDocument31 pagesPUPILHamza FarooqNo ratings yet
- Medical Management of GlaucomaDocument43 pagesMedical Management of Glaucomahemnath rajendran100% (1)
- Non-Concomitant Strabismus 2Document60 pagesNon-Concomitant Strabismus 2Ijeoma Okpalla100% (2)
- Clinical Ophthalmology Dadapeer 23 28Document6 pagesClinical Ophthalmology Dadapeer 23 28AntaraaNo ratings yet
- Acute and Chronic Chorea in Childhood: Donald L. Gilbert, MD, MSDocument6 pagesAcute and Chronic Chorea in Childhood: Donald L. Gilbert, MD, MSKalindraParahitaNo ratings yet
- Glaucoma 1Document8 pagesGlaucoma 1xoxoNo ratings yet
- Approach To Epilepsy POWER POINT - EDITEDDocument41 pagesApproach To Epilepsy POWER POINT - EDITEDVipul NagnesiaNo ratings yet
- Neuro-Ophta EditedDocument97 pagesNeuro-Ophta EditedMarshet GeteNo ratings yet
- Colour Vision AnomaliesDocument27 pagesColour Vision AnomaliesGershon HayfordNo ratings yet
- Superior Oblik PalsyDocument13 pagesSuperior Oblik PalsyYunita ManurungNo ratings yet
- Pupiliary PathwayDocument91 pagesPupiliary Pathwaydrsrp8467% (3)
- College of Medicine and Health Science, Department of OptometryDocument47 pagesCollege of Medicine and Health Science, Department of Optometryhenok birukNo ratings yet
- Anophthalmia and MicrophthalmiaDocument8 pagesAnophthalmia and MicrophthalmiaLjubomirErdoglijaNo ratings yet
- Aqueous Humor Dynamics (DR Poonam)Document28 pagesAqueous Humor Dynamics (DR Poonam)Sampitroda DesaiNo ratings yet
- Red Eye: A Guide For Non-Specialists: MedicineDocument14 pagesRed Eye: A Guide For Non-Specialists: MedicineFapuw Parawansa100% (1)
- 7.1 Gradual Loss of VisionDocument19 pages7.1 Gradual Loss of VisionparugandooNo ratings yet
- Metabolic and Complicated Cataract: DR - Ajai Agrawal Additional Professor Department of Ophthalmology AIIMS, RishikeshDocument31 pagesMetabolic and Complicated Cataract: DR - Ajai Agrawal Additional Professor Department of Ophthalmology AIIMS, Rishikeshsai shantanu100% (1)
- Retinitis PigmentosaDocument35 pagesRetinitis Pigmentosawessam284No ratings yet
- RetinaDocument82 pagesRetinafebienaNo ratings yet
- 42fundus AngiographyDocument28 pages42fundus AngiographyHitesh SharmaNo ratings yet
- Drug Induced Optic NeuropathyDocument23 pagesDrug Induced Optic NeuropathyFaizi JaniNo ratings yet
- Papilledema Grading System (Frisen Scale)Document2 pagesPapilledema Grading System (Frisen Scale)tesarNo ratings yet
- ACHONDROPLASIADocument18 pagesACHONDROPLASIAJennie Mayaute AllcaNo ratings yet
- Motor Neuron Disease 1Document95 pagesMotor Neuron Disease 1La Ode Rinaldi100% (1)
- Cataract InformationDocument25 pagesCataract Informationvasanth_1515No ratings yet
- Diagnosis Approach of Optic Neuritis 2155 9562 1000345Document13 pagesDiagnosis Approach of Optic Neuritis 2155 9562 1000345Juaan AvilaNo ratings yet
- Diagram For Ophtal NoteDocument7 pagesDiagram For Ophtal NoteSiam Weng LoongNo ratings yet
- LEUKOKORIADocument3 pagesLEUKOKORIAFahlevie EpinNo ratings yet
- Physiology of Human EyeDocument6 pagesPhysiology of Human EyeJim Jose AntonyNo ratings yet
- Intraocular Pressure Variation During Femtosecond Cataract SurgeryDocument6 pagesIntraocular Pressure Variation During Femtosecond Cataract SurgeryRodrigoBarreraNo ratings yet
- Ocular Features Aid The Diagnosis of AsDocument5 pagesOcular Features Aid The Diagnosis of AsRodrigoBarreraNo ratings yet
- Alport Retinopathy Results From Severe COL4A5 Mutations and Predicts Renal FailureDocument5 pagesAlport Retinopathy Results From Severe COL4A5 Mutations and Predicts Renal FailureRodrigoBarreraNo ratings yet
- Risk Factors For Steroid Response Among Cataract PatientsDocument7 pagesRisk Factors For Steroid Response Among Cataract PatientsRodrigoBarreraNo ratings yet
- BostonSight PROPOSE Patients and Doctors CurrentDocument8 pagesBostonSight PROPOSE Patients and Doctors CurrentRodrigoBarreraNo ratings yet
- Risk Factor For Preoperative Ocular HypertensionDocument5 pagesRisk Factor For Preoperative Ocular HypertensionRodrigoBarreraNo ratings yet
- Gokhale Epidemiologia Queratocono Indian J Ophthalmol 2013Document2 pagesGokhale Epidemiologia Queratocono Indian J Ophthalmol 2013RodrigoBarreraNo ratings yet
- Akcay Queratocono y Prolapso Mitral J Ophth 2014Document7 pagesAkcay Queratocono y Prolapso Mitral J Ophth 2014RodrigoBarreraNo ratings yet
- Kosker Rapuano Queratocono y Diabetes Cornea 2014Document6 pagesKosker Rapuano Queratocono y Diabetes Cornea 2014RodrigoBarreraNo ratings yet
- Serdarogullari Prevalencia Queratocono Pentacam JOVR 2013Document7 pagesSerdarogullari Prevalencia Queratocono Pentacam JOVR 2013RodrigoBarreraNo ratings yet
- Keratoconus Tissue Engineering and BiomaterialsDocument24 pagesKeratoconus Tissue Engineering and BiomaterialsRodrigoBarreraNo ratings yet
- Advantages and Limitations of Small Gauge VitrectomyDocument11 pagesAdvantages and Limitations of Small Gauge VitrectomyRodrigoBarreraNo ratings yet
- Comm3 Speech PlanDocument2 pagesComm3 Speech PlanArra Faith Gacosta EsturNo ratings yet
- Pylera 140Mg-125Mg CapsulesDocument6 pagesPylera 140Mg-125Mg CapsulesarchurbaNo ratings yet
- Zandian (2007) Cause and Treatment of Anorexia NervosaDocument8 pagesZandian (2007) Cause and Treatment of Anorexia NervosaRenzo LanfrancoNo ratings yet
- Case 1-2022: A 67-Year-Old Man With Motor Neuron Disease and Odd Behaviors During SleepDocument8 pagesCase 1-2022: A 67-Year-Old Man With Motor Neuron Disease and Odd Behaviors During Sleeppogesil46No ratings yet
- Case Studies Therapy 1Document9 pagesCase Studies Therapy 1WONDWOSSEN ALEMUNo ratings yet
- Post-Traumatic Stress DisorderDocument12 pagesPost-Traumatic Stress Disorderecbt100% (2)
- Respiratory Tract InfectionDocument50 pagesRespiratory Tract InfectionAvi Verma100% (2)
- Diabetes and Hearing Loss (Pamela Parker MD)Document2 pagesDiabetes and Hearing Loss (Pamela Parker MD)Sartika Rizky HapsariNo ratings yet
- Patient Care Classification SystemDocument8 pagesPatient Care Classification SystemWin AndangNo ratings yet
- 10 Drug StudyDocument25 pages10 Drug StudyM AnnNo ratings yet
- Alternative Systems of MedicineDocument53 pagesAlternative Systems of MedicineShruti Baid BafnaNo ratings yet
- PBL 5.2 (Git 1)Document46 pagesPBL 5.2 (Git 1)aiman mazlanNo ratings yet
- Case StudyDocument7 pagesCase Studyapi-402806930No ratings yet
- Collateral History For Delirium/ DementiaDocument2 pagesCollateral History For Delirium/ DementiaPetros Akin-NibosunNo ratings yet
- Tachdjian's Pediatric Orthopaedics v.4Document660 pagesTachdjian's Pediatric Orthopaedics v.4Leonardo Garay QuinteroNo ratings yet
- Drug StudyDocument1 pageDrug StudyMaui LopezNo ratings yet
- Prophylactic Antibiotics in LaborDocument17 pagesProphylactic Antibiotics in LaborAlejandra BuNo ratings yet
- Acute Liver Failure Group 3Document16 pagesAcute Liver Failure Group 31S VILLEGAS GabrielNo ratings yet
- (Oxford Specialist Handbooks in Psychiatry) Jessica Yakeley Et Al. (Eds.) - Medical Psychotherapy-Oxford University Press (2016)Document641 pages(Oxford Specialist Handbooks in Psychiatry) Jessica Yakeley Et Al. (Eds.) - Medical Psychotherapy-Oxford University Press (2016)Cristina Lefter100% (1)
- Ok Sa Deped Form B - For SchoolsDocument5 pagesOk Sa Deped Form B - For SchoolsAna Cella Rico MarzoNo ratings yet
- Dermatology Made EasyDocument46 pagesDermatology Made EasyHeather Marie Mathis100% (1)
- Anti-Inflammatory Effect of Panyawan Stem For Toothache (1)Document10 pagesAnti-Inflammatory Effect of Panyawan Stem For Toothache (1)Nolemae NavalesNo ratings yet
- Diabetes in Childhood and Adolescence GuidelinesDocument132 pagesDiabetes in Childhood and Adolescence GuidelinesJust MahasiswaNo ratings yet
- Astigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedDocument12 pagesAstigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedLynden BulanNo ratings yet
- Lecture For Community Health CareDocument7 pagesLecture For Community Health CareagbrittainNo ratings yet
- ArteriosclerosisDocument3 pagesArteriosclerosisVirag PatilNo ratings yet
- Acute AbdomenDocument54 pagesAcute AbdomenMoses ChatipaNo ratings yet
- Hygiene and Health in IslamDocument37 pagesHygiene and Health in Islamالمدینہ اسلامک ریسرچ سینٹر کراچی100% (1)
- Endocrine System DiseasesDocument87 pagesEndocrine System DiseasesFahmiArifMuhammadNo ratings yet
- Pursed Lips Breathing and CHFDocument6 pagesPursed Lips Breathing and CHFErwan HermansyahNo ratings yet