Professional Documents
Culture Documents
Draft Antimania
Uploaded by
Wahyu Ahp0 ratings0% found this document useful (0 votes)
7 views5 pagesmania
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentmania
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views5 pagesDraft Antimania
Uploaded by
Wahyu Ahpmania
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
Other drug treatments for mania
The long-term toxic effects of lithium, such as nephrogenic diabetes
insipidus, which has been calculated to occur in up to 5% of patients, and
the rare possibility of lithium combined with neuroleptics being neurotoxic,
has stimulated the research for other drug treatments. However, apart from
the neuroleptics, these drugs have not been studied as extensively in the
treatment of acute mania, but are worthy of consideration because of their
reduced side effects.
Neuroleptics
Most psychotic and non-compliant patients are difficult to treat with lithium
alone and need to be treated with neuroleptics. Haloperidol has been widely
used alone to control the more florid symptoms of mania, but doubts have
arisen concerning its toxic interactions with lithium. Such considerations are
based on a report that such a combination caused neurotoxicity in a small
group of manic patients, but it should be emphasized that a variety of other
neuroleptics have also been rarely found to cause these effects. The symptoms
of neurotoxicity include ataxia, confusion, hyperactive reflexes, chorea,
slurred speech and even coma. It seems likely that some of these patients
suffered from the malignant neuroleptic syndrome rather than enhanced
lithium toxicity, but problems such as dehydration and over-sedation may
have enhanced the drug interaction. More recently, atypical antipsychotics
such as olanzapine and risperidone have been shown to be effective in the
treatment of acute mania. These drugs have advantages over haloperidol, and
the first-generation neuroleptics, due to the improved side-effect profiles and
better patient compliance.
Tardive dyskinesia can occur in manic patients on neuroleptics alone, the
frequency may be greater than in schizophrenics who are more likely to be on
continuous medication. One possible explanation for this lies in the fact that
neuroleptics are often administered to manic patients for short periods only,
sufficient to abort the active episode, and then abruptly stopped. Thus high
doses of neuroleptics are separated by drug-free periods, leading to a situation
most likely to precipitate tardive dyskinesia. The recent increase in prescribing
high potency neuroleptics such as haloperidol instead of low potency drugs
such as chlorpromazine or thioridazine has undoubtedly increased the
frequency of tardive dyskinesia. Clearly, use of the atypical antipsychotics
with the very low frequency of EPS makes them the treatments of choice.
Valproate
Valproic acid (dipropylacetic acid) is a single branched chain carboxylic
acid that is structurally unlike any of the other drugs used in the treatment
of bipolar disorder or epilepsy. The amide derivative, valproamide, is
available in Europe as a more potent form of valproate. Valproate was first
developed in France as an antiepileptic agent in 1963. As an antiepileptic
agent, it was shown to be active against a variety of epilepsies without
causing marked sedation.
The mechanism of action of valproate is complex and still the subject of
uncertainty. The drug appears to act by enhancing GABAergic function.
Thus it increases GABA release, inhibits catabolism and increases the
density of GABA-B receptors in the brain. There is also evidence that it
increases the sensitivity of GABA receptors to the action of the inhibitory
transmitter. Other actions that may contribute to its therapeutic effects
include a decrease in dopamine turnover, a decrease in the activity of the
NMDA-glutamate receptors and also a decrease in the concentration of
somatostatin in the CSF. Unlike carbamazepine, valproate does not bind to
peripheral benzodiazepine receptors (see p. 230).
Numerous open studies, and seven controlled studies, have shown that
valproate is effective in the treatment of acute mania. It has also been
claimed to have an antidepressant action. Recent studies have shown that
valproate is effective in the long-term treatment of bipolar disorder.
Valproate is generally well tolerated and less likely to cause cognitive
impairment than other antiepileptic drugs such as carbamazepine. It does
frequently cause gastrointestinal upset and a benign elevation of liver
transaminases however. Because valproate is highly plasma protein bound,
and is partially metabolized by the cytochrome P450 system, it can interact
with many other drugs. For example, aspirin can enhance the efficacy and
toxicity of valproate by displacing it from the plasma proteins while
microsomal enzyme-inducing drugs such as carbamazepine can decrease
its plasma and tissue concentrations. The general properties of valproate are
further discussed in Chapter 12.
Carbamazepine
This is a tricyclic compound somewhat similar to imipramine that is an
anticonvulsant widely used in the treatment of temporal lobe epilepsy.
Following its widespread use as an antiepileptic, it soon became evident
that it had psychotropic effects. These included an improvement in mood,
reduced aggressiveness and improved cognitive function. Kindling refers to
the development of seizures after repeated delivery of a series of
subthreshold stimuli to any region of the brain. This phenomenon can
most readily be induced in limbic structures and, whereas conventional
anticonvulsants such as phenytoin and phenobarbitone have little effect in
attenuating kindled seizures, carbamazepine and the benzodiazepine
anticonvulsants prevent such seizure development. It is now well
established that carbamazepine is relatively selective in attenuating seizure
activity in the hippocampus and amygdala, which suggests that it acts
preferentially at limbic sites in the brain.
The mechanism of action of carbamazepine is complex, and is complicated
by the fact that it has a long half-life metabolite, carbamazepine epoxide,
which also has pronounced psychotropic properties.
The anticonvulsant properties of the drug would appear to be due to its
ability to inhibit fast sodium channels, which may be unrelated to its
psychotropic effects. Like lithium, it has been shown to decrease the release
of noradrenaline and reduce noradrenaline-induced adenylate cyclase
activity; unlike lithium, it seems to have little effect on tryptophan or
5-HT levels in patients at therapeutically relevant concentrations. It also
reduces dopamine turnover in manic patients and increases acetylcholine
synthesis in the cortex, an effect also seen with lithium. The effect of
carbamazepine on GABAergic function appears to be related to its
interaction with GABA-B type receptors, which may be relevant to its
usefulness in the treatment of trigeminal neuralgia. There is no evidence
that it changes GABA levels in the CSF of patients. Furthermore, while it
would appear that the drug has no effect on central benzodiazepine
receptors, there is evidence that it has a high affinity for the peripheral type
of benzodiazepine receptor. These receptors are found in the mammalian
brain but differ from the central receptors in that they are not linked to
GABA receptors and therefore do not affect chloride ion flux. The main
function of the peripheral type of benzodiazepine receptor would seem to
be to control calcium channels. This may help to explain some of the
psychotropic effects of carbamazepine, particularly as calcium channel
antagonists such as verapamil have antimanic effects.
Changes in the activity of adenosine receptors have been implicated in
the stimulant effects of drugs like caffeine. Carbamazepine exhibits a partial
agonist effect on adenosine receptors, and experimental evidence suggests
that the reduced reuptake and release of noradrenaline caused by the drug
are due to its interaction with these receptors. The precise relevance of these
findings to its anticonvulsant and psychotropic effects is presently unclear.
Of the various peptides (e.g. the opioids, vasopressin, substance P and
somatostatin) thought to be involved in the actions of carbamazepine, there
is evidence that the reduction in the CSF concentration of somatostatin
might be important in explaining its effects on cognition and also on the
hypothalamopituitaryadrenal axis; somatostatin is a major inhibitory
modulator of this axis and hypercortisolism frequently occurs in patients
following carbamazepine administration.
There is still controversy regarding the general usefulness of carbamazepine
as an alternative to lithium. It is apparent that the nature of the
illness alters throughout the lifetime of the patient, so that pharmacological
interventions may differ according to the stage of the illness. Preliminary
clinical studies suggest that lithium may be particularly beneficial during
the early and intermediate stages of the illness, whereas carbamazepine and
related anticonvulsants may be more useful, either alone or in combination
with lithium, at later stages, particularly, when the patient shows rapid,
continuous cycling between mania and depression.
Other drugs
Other drugs that are reported to have beneficial effects but which have not
undergone such extensive evaluation as the neuroleptics or carbamazepine
include the calcium channel antagonists such as verapamil. A small open
study has suggested that the alpha2 adrenoceptor agonist clonidine may
have some activity. More substantial studies have been conducted on the
benzodiazepines lorazepam and clonazepam, and the anticonvulsant sodium
valproate. All these drugs facilitate GABAergic function in some way, the
first two by acting as agonists at benzodiazepine receptor sites and the latter
by desensitizing the GABA autoreceptor and thereby enhancing the release
of this inhibitory transmitter. Lastly, electroconvulsive shock treatment
(ECT) has been claimed to be effective in attenuating the symptoms of an
acute manic attack, but there is evidence that patients treated with ECT
should not receive lithium concomitantly to reduce the possibility of
neurotoxic side effects.
In addition to these drugs, many of the newer antiepileptic drugs such as
lamotrigine have found a place in the therapeutic management of mania.
These are extensively covered in Chapter 12.
Maintenance treatments for bipolar disorder
The pharmacological management of bipolar disorder involves treatment of
both the acute and the longer-term maintenance phase of the illness. Longterm
maintenance is necessary to reduce or prevent the recurrence of the
symptoms, and to minimize the risk of suicide.
For many years, lithium salts have been used for maintenance treatment.
However, naturalistic studies have reported a relatively high failure rate in
patients on lithium and therefore other therapeutic approaches have been
considered.
With regard to the use of lithium in maintenance therapy, the studies
which were published in the 1970s clearly demonstrated the efficacy of
lithium in preventing relapse into mania or depression in patients with
bipolar disorder. However, subsequent longer-term naturalistic studies
raised doubts over the validity of these findings. In particular, these studies
have shown that up to 50% of patients respond poorly to lithium. Some of
the reasons for the re-evaluation of the early reports on the efficacy of
lithium as a maintenance treatment are due to the methodological
limitations of the placebo-controlled studies which include a lack of
diagnostic criteria and a limited consideration of those patients withdrawing
from the clinical trial prematurely.
In contrast to the large number of studies that have investigated lithium
as a maintenance treatment for bipolar disorder, relatively few studies have
been made of divalproex sodium, despite its widespread use in the acute
treatment of mania. There is evidence from one placebo-controlled study in
which lithium was compared with divalproex sodium that the latter drug
was better tolerated but that the prevention of relapse did not differ
between the drugs. It would therefore appear that a switch to divalproex
sodium may be particularly useful in bipolar patients who are experiencing
cognitive deficits, loss of creativity and functional impairments consequent
on lithium use.
Again there are relatively few studies that have investigated the use of
carbamazepine in maintenance therapy. The results of the studies published
suggest that carbamazepine is not as effective as lithium or divalproex. In
the controlled studies of carbamazepine, the majority of patients required
adjunctive treatment to prevent a breakthrough for the manic or depressive
symptoms.
Despite the widespread use of neuroleptics in maintenance treatment of
bipolar disorder, there have not been any systematic studies of their
suitability for this role. Through clinical experience it has been widely
accepted that neuroleptics are useful adjunctive treatments to lithium and
related drugs. Treatment refractory patients frequently respond to atypical
antipsychotics such as clozapine or risperidone. Such adverse effects as
EPS, cognitive dysfunction and weight gain frequently limit the long-term
use of classical neuroleptics. For this reason, the atypical neuroleptics such
as olanzapine and risperidone should now be considered as alternatives for
maintenance treatment.
Treatment decisions for bipolar disorder
. Treatment of choice mood stabilizer with or without an antidepressant
(e.g. lithium, valproate, carbamazepine, lamotrigine). Antidepressants
include an SSRI, venlafaxine, mirtazepine as possibilities but few
controlled trials to substantiate choice.
. Switching alternative mood stabilizer plus alternative secondgeneration
antidepressant.
. Augmentation of the response combine two mood stabilizers; add
thyroid hormone to mood stabilizer.
. Other options ECT; possibly calcium channel blockers such as
verapamil or nimodipine.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
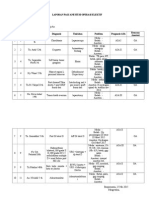
- Absen Rg. LilyDocument93 pagesAbsen Rg. LilyWahyu AhpNo ratings yet
- DapusDocument3 pagesDapusWahyu AhpNo ratings yet
- Dafrar Pustaka: Kedokteran Universitas Indonesia. Jakarta. 2008Document1 pageDafrar Pustaka: Kedokteran Universitas Indonesia. Jakarta. 2008Wahyu AhpNo ratings yet
- Laporan Pagi Anestesi Operasi ElektifDocument2 pagesLaporan Pagi Anestesi Operasi ElektifWahyu AhpNo ratings yet
- Awas !!! Bencana Pemurtadan !: Oleh DustakuDocument6 pagesAwas !!! Bencana Pemurtadan !: Oleh DustakuWahyu AhpNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- RubelinDocument7 pagesRubelinPeace Andong PerochoNo ratings yet
- Slide World Urethral StrictureDocument10 pagesSlide World Urethral Strictureاميرة عليNo ratings yet
- Fluid and Electrolyte Therapy, Calculation of Fluids and Its AdministrationDocument11 pagesFluid and Electrolyte Therapy, Calculation of Fluids and Its AdministrationAnusha Verghese100% (2)
- InTech-Management of Bone Loss in Primary and Revision Knee Replacement SurgeryDocument25 pagesInTech-Management of Bone Loss in Primary and Revision Knee Replacement SurgerySagaram ShashidarNo ratings yet
- Hospital Case StudyDocument3 pagesHospital Case StudyShashi88% (8)
- InfertilityDocument10 pagesInfertilityits_piks7256No ratings yet
- PsicologiaDocument24 pagesPsicologiaPablo UlisesNo ratings yet
- 1344938487binder2Document34 pages1344938487binder2CoolerAdsNo ratings yet
- Inservice PresentationDocument13 pagesInservice Presentationapi-467829418No ratings yet
- Patient Education: Alopecia Areata (Beyond The Basics) - UpToDateDocument9 pagesPatient Education: Alopecia Areata (Beyond The Basics) - UpToDateAngga Julyananda PradanaNo ratings yet
- IntussusceptionDocument2 pagesIntussusceptionkentkriziaNo ratings yet
- Polypharmacy in Elderly PatientsDocument7 pagesPolypharmacy in Elderly PatientsMariana RibeiroNo ratings yet
- Prison Architecture and DesignDocument46 pagesPrison Architecture and Designbryant neutron100% (1)
- Fatality Inquiry Report: Jeffrey & Jeremy BostickDocument54 pagesFatality Inquiry Report: Jeffrey & Jeremy BostickEmily MertzNo ratings yet
- The Unique Therapeutic Effect of Different Art Materials Onpsychological Aspects of 7 - To 9-Year-Old ChildrenDocument9 pagesThe Unique Therapeutic Effect of Different Art Materials Onpsychological Aspects of 7 - To 9-Year-Old ChildrenwilmaNo ratings yet
- Effectiveness of Robotic-Assisted Gait Training in Stroke Rehabilitation: Revolution in Patient OutcomeDocument9 pagesEffectiveness of Robotic-Assisted Gait Training in Stroke Rehabilitation: Revolution in Patient OutcomeIJAR JOURNALNo ratings yet
- EBPDocument32 pagesEBPKlinikbersalin BpsadyamyshaNo ratings yet
- Antibiotics in DentistryDocument25 pagesAntibiotics in Dentistryimmortalneo100% (1)
- Pseudo ExfoliationDocument6 pagesPseudo ExfoliationvannyanoyNo ratings yet
- Leptospirosis: A Case Study: Mathew SullivanDocument3 pagesLeptospirosis: A Case Study: Mathew SullivanSagara MaheshNo ratings yet
- 21st Century Cures ActDocument312 pages21st Century Cures ActStephen LoiaconiNo ratings yet
- Chinese Eye ExercisesDocument12 pagesChinese Eye ExercisesAnonymous ofwFwNtM100% (1)
- Obstetric Safety ProtocolsDocument10 pagesObstetric Safety ProtocolsApril LilianNo ratings yet
- Neuropsychiatry Final MCQDocument6 pagesNeuropsychiatry Final MCQRifqi MuhammadNo ratings yet
- Psoriasis PresentationDocument70 pagesPsoriasis PresentationnunuijoeNo ratings yet
- Neurologija SkripticaDocument26 pagesNeurologija SkripticaLazar VučetićNo ratings yet
- Poster Presentations: 2009 The Authors Journal Compilation 2009 Blackwell Verlag GMBH - Mycoses, 52 (Suppl. 1), 29-123Document95 pagesPoster Presentations: 2009 The Authors Journal Compilation 2009 Blackwell Verlag GMBH - Mycoses, 52 (Suppl. 1), 29-123Flávio VianiNo ratings yet
- 10-22-14 EditionDocument32 pages10-22-14 EditionSan Mateo Daily JournalNo ratings yet
- A Systematic and Integrative Model For Mental Health Assessment and Treatment PlanningDocument35 pagesA Systematic and Integrative Model For Mental Health Assessment and Treatment PlanningCharleneKronstedt100% (2)
- Irest Trauma Treatment Protocol ScriptDocument6 pagesIrest Trauma Treatment Protocol Scriptyogafireyogaflame100% (3)