Professional Documents
Culture Documents
Mycoplasma Hominis Necrotizing Pleuropneumonia in A Previously Healthy Adolescent
Uploaded by
Satriyani AmirOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mycoplasma Hominis Necrotizing Pleuropneumonia in A Previously Healthy Adolescent
Uploaded by
Satriyani AmirCopyright:
Available Formats
Pascual et al.
BMC Infectious Diseases 2010, 10:335
http://www.biomedcentral.com/1471-2334/10/335
CASE REPORT
Open Access
Mycoplasma hominis necrotizing pleuropneumonia
in a previously healthy adolescent
Andres Pascual1,2*, Marie-Helene Perez2, Katia Jaton4, Gaudenz Hafen3, Stefano Di Bernardo3,
Jacques Cotting2, Gilbert Greub1,4, Bernard Vaudaux1,3
Abstract
Background: Mycoplasma hominis is a fastidious micro-organism causing systemic infections in the neonate and
genital infections in the adult. It can also be the cause of serious extra-genital infections, mainly in
immunosuppressed or predisposed subjects.
Case Presentation: We describe a case of severe pneumonia and pericarditis due to Mycoplasma hominis in a
previously healthy adolescent who did not respond to initial therapy.
Conclusions: Mycoplasma hominis could be an underestimated cause of severe pneumonia in immunocompetent
patients and should be particularly suspected in those not responding to standard therapy.
Background
Mycoplasma hominis (M. hominis) belongs to the order
of Mycoplasmatales, prokaryotes that lack a cell wall.
This characteristic has implications for antibiotic therapy as many commonly used antibiotics act by inhibiting
the bacterial cell wall synthesis. Mycoplasma organisms
have fastidious growth requirements and are often difficult to culture on a cell-free medium. A recent analysis
of the M. hominis genome sequence revealed that it is
the second smallest genome among self-replicating free
living organisms with a predicted genome of 537 coding
genes [1]. M. hominis is an opportunistic organism that
is uncommonly associated with infection in humans.
However, it is frequently isolated from the urogenital
and respiratory tract of asymptomatic healthy persons
[2]. Infants may be colonized following vaginal delivery
but M. hominis is rarely recovered from prepubertal
children. Colonization in postpubertal individuals results
mainly from sexual contact [3].
M. hominis exceptionally penetrates the submucosal
layer, unless the patient is immunosupressed or traumatized (through accident or instrumentation). In this case,
* Correspondence: Andres.Pascual@chuv.ch
Contributed equally
1
Infectious Diseases Service, Department of Medicine, Centre Hospitalier
Universitaire Vaudois and University of Lausanne, 1011, Lausanne,
Switzerland
Full list of author information is available at the end of the article
it can invade the bloodstream and disseminate to many
different organs and tissues throughout the body, causing extragenital infections [4]. However, extragenital
infections are uncommon in healthy patients and cases
of pneumonia are exceptional.
M. hominis is an organism recognized to be intrinsically resistant to macrolides. In addition, there is recent
evidence of increasing resistance to tetracycline and
emerging resistance to fluoroquinolones [5-7].
Case Presentation
A previously healthy 15-year-old sexually active female
came to the emergency room because of dyspnoea, fever
and right thoracic pain. The physical examination was
suggestive of right sided pneumonia and laboratory tests
revealed a marked leukocytosis (39800/mm3 WBC, 89%
neutrophils; 74% segmented and 15% bands) and an elevated C-reactive protein level (>250 mg/L). The chest
X-ray confirmed the clinical suspicion of right lobar
pneumonia and an outpatient treatment of oral clarithromycin (500 mg bid) was started. The absence of
clinical improvement and the onset of a pleural effusion
on the fourth day of antibiotic therapy lead to admission
to our hospital and the addition of i.v. ceftriaxone (2 g
bid) to the macrolide regimen.
As the high fever persisted, a chest CT scan was done
on the seventh day of antibiotic treatment, showing a
bilateral necrotizing pneumonia as well as a bilateral
2010 Pascual et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Pascual et al. BMC Infectious Diseases 2010, 10:335
http://www.biomedcentral.com/1471-2334/10/335
pleural effusion. At this time, on the basis of a presumed polymicrobial infection including anaerobes, a
treatment of i.v. amoxicillin/clavulanate (2.2 g tid) was
substituted to the previous clarithromycin-ceftriaxone
regimen.
Two days later the patient was transferred to the paediatric intensive care unit because of rapid worsening of her
symptoms with the risk of respiratory failure. Amoxicillin/
clavulanate therapy was switched to imipenem-cilastatin
(500 mg i.v. qid) and vancomycin (750 mg i.v. tid).
Cultures of pleural effusion for aerobic and anaerobic
pathogens obtained by needle aspiration were negative. M.
hominis was then detected by eubacterial PCR [DNA
extracts were amplified using PCR targeting the 16S rRNA
as follows: forward primer (Bak11wF): 5-AGTTTGATCMTGGCTCAG-3, reverse Primer (Pc3 mod): 5GGACTACHAGGGTATCTAAT-3, sequencing primer:
Bak11wf and Bak533 r: 5-TTACCGCGGCTGCTGGCAC] [3], and confirmed by a M. hominis specific Taqman PCR
(98,500,000 copies/mL). The primers of the TaqMan PCR
used
were:
Forward
primer:
5-TTTGGTC
AAGTCCTGCAACGA-3, Reverse Primer: 5-CCCCAC
CTTCCTCCCAGTTA-3 and probe: FAM-TTACTAACATTAAGTTGAGGACTCTA-MGB, targeting the M.
hominis 16 rRNA gene sequence [8], and further confirmed
by specific culture (Mycoplasma IST, bioMrieux, France).
The antibiotic susceptibility tests revealed resistance to
macrolides and susceptibility to tetracyclines and quinolones, leading to the addition of doxycycline (100 mg
bid) twelve days after the start of symptoms.
Page 2 of 4
A new CT scan showed a larger amount of pleural
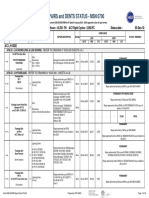
fluid as well as a pericardial effusion (Figure 1).
Because of worsening respiratory and haemodynamic
conditions, the pericardial and pleural effusions were
evacuated by pericadiectomy with window and pleural
drainage by chest tube insertion. Any respiratory support (other than oxygen supplementation) was needed
thereafter. M. hominis DNA was also amplified in the
pericardial fluid by specific PCR (85 copies/mL). Standard axenic cultures and specific PCR assays for Streptococcus pneumoniae and Staphylococcus aureus, as well
as Legionella pneumophila urinary antigen test were
negative in all specimens. Complement-fixing antibody
to Mycoplasma pneumoniae showed no increase in
titers.
Imipenem-cilastin and vancomycine were discontinued
while doxycycline was administered for a total of
2 weeks. This treatment was associated with clinical and
biological improvement and the patient could be discharged from the hospital on day 19. At this time, the
CRP level was down to 16 mg/L. Finally the patient
completely recovered without any sequel on the chest
X-ray.
Discussion
We described a case of severe pneumonia and pericarditis due to M. hominis in a previously healthy adolescent
who completely recovered under doxycycline therapy.
M. hominis was detected from the pleural and pericardial fluids by eubacterial PCR assay and subsequent
Figure 1 CT scan of the thorax showing bilateral necrotizing pneumonia (black circles) and pleural effusion (black squares) as well as
pericardial effusion (leftwards arrows). Note the presence of a chest tube inserted into the pleural cavity (in communication with the lung
abscess) and a drainage tube into the pericardial cavity (downwards arrows).
Pascual et al. BMC Infectious Diseases 2010, 10:335
http://www.biomedcentral.com/1471-2334/10/335
specific PCR assay and culture. No alternative pathogen
has been identified by culture, molecular or serological
diagnostic procedures.
M. hominis may cause genital infections in adults and
may be involved in neonatal infections. Serious extragenital infections, such as brain abscess, pneumonia,
mediastinitis, pericarditis, endocarditis, osteitis and
arthritis, wound infections, peritonitis, and pyelonephritis have been reported, mainly in immunosuppressed
patients [9-12]. However, such cases have also been
described in immunocompetent patients, particularly in
individuals with predisposing factors such as trauma,
altered cardiorespiratory function and complicated urogenital manipulations or surgery.
Our review of the literature identified 11 cases of
M. hominis pneumonia in immunocompetent patients
(Additional file 1) [13-17].
Six cases occurred in patients with pre-existing
co-morbidities (trauma or surgery, subarachnoid haemorrhage, and oesophageal carcinoma), one case in a
pregnant woman, and four cases in patients with no
known predisposing conditions.
Complete resolution has been described in the five
patients who received antibiotic therapy active against
M. hominis. In contrast, among those receiving an
inadequate antibiotic therapy, four died and two recovered suggesting that untreated M. hominis infection may
aggravates pre-existing conditions and lead to death.
Initially, our patient experienced a severe worsening of
her clinical condition while on antibiotics active against
common respiratory pathogens, but has fully recovered
after receiving an antimicrobial drug active against M.
hominis.
M. hominis may be an underestimated cause of severe
pneumonia in previously healthy patients, particularly
when other common etiological agents have been ruled
out in those not responding to standard therapy.
The M. hominis strain isolated in our patient was susceptible to both tetracyclines and quinolones. We used
a susceptibility assay based on breakpoint cut offs set
according to the recommendations of the Clinical and
Laboratory Standards Institute (CLSI) [18].
Unpublished data from our center on the antibiotic
susceptibility of M. hominis strains isolated from the
genital and respiratory tracts between 2000 and 2008
are in accordance with the data from the literature: 55%
are susceptible to ciprofloxacin (5/9), 100% are susceptible to doxycycline (11/11), and 100% are resistant to
clarithromycin (9/9).
M. hominis is intrinsically resistant to macrolides
[19-21], and tetracyclines have been considered the
drugs of choice. However, the therapeutic activity of tetracyclines may become unreliable due to resistance phenomena induced by previous antibiotic exposure.
Page 3 of 4
Moreover, they are no longer a valid therapeutic option
in some areas [5,7]. As no resistance to levofloxacin (or
other newer fluoroquinolones) and clindamycin is yet
identified, these drugs could be a suitable therapeutic
alternative [5,7,20,22,23]. The increasing resistance of
M. hominis strains to antibiotics makes guidance of
therapy by in vitro susceptibility tests of paramount
importance in invasive infections leading to lifethreatening situations.
Conclusions
This case report shows the role of M. hominis as a possible etiologic agent in a previous healthy adolescent
suffering a severe and complicated pneumonia not
responding to macrolide and b-lactam agents.
The eubacterial PCR is a useful tool to detect unusual
pathogens.
The efficacy of traditional drugs such as tetracyclines
on M. hominis is affected by increasing resistance, making susceptibility testing an important issue nowadays.
The newest fluoroquinolones are an attractive option to
treat invasive infections caused by M. hominis.
Consent
Written informed consent was obtained from the patient
and her mother for publication of this case report. A
copy of the written consent is available for review by
the Editor-in-Chief of this journal.
Additional material
Additional file 1: Table S1: Summary of previously reported
Mycoplasma hominis pneumonia in immunocompetent patients.
Acknowledgements
We are thankful to Aline Wenger for her assistance in the microbiology
identification and susceptibility testing, to Jean Daniel Krhenbhl, Andrs
Roby, Pascal Stucki and Frdric Lamoth for their careful review of the
manuscript.
Author details
Infectious Diseases Service, Department of Medicine, Centre Hospitalier
Universitaire Vaudois and University of Lausanne, 1011, Lausanne,
Switzerland. 2Pediatric Intensive Care Unit, Centre Hospitalier Universitaire
Vaudois and University of Lausanne, 1011, Lausanne, Switzerland. 3Pediatric
Service, Department of Pediatrics, Centre Hospitalier Universitaire Vaudois
and University of Lausanne, 1011, Lausanne, Switzerland. 4Institute of
Microbiology, Centre Hospitalier Universitaire Vaudois and University of
Lausanne, 1011, Lausanne, Switzerland.
1
Authors contributions
JC, MHP, GH, SDB, BV and AP: have been involved in patient clinical care,
and in acquisition and interpretation of data. MHP, AP and BV have been
involved in drafting the manuscript. GG and KJ carried out the standard and
specific microbiologic tests and the molecular genetic studies. GH, GG, MHP,
AP and BV: have reviewed the manuscript. All authors read and approved
the final manuscript.
Pascual et al. BMC Infectious Diseases 2010, 10:335
http://www.biomedcentral.com/1471-2334/10/335
Competing interests
The authors declare that they have no competing interests.
Received: 5 August 2009 Accepted: 24 November 2010
Published: 24 November 2010
References
1. Pereyre S, Sirand-Pugnet P, Beven L, Charron A, Renaudin H, Barre A, et al:
Life on arginine for Mycoplasma hominis: clues from its minimal
genome and comparison with other human urogenital mycoplasmas.
PLoS Genet 2009, 5:e1000677.
2. Mufson MA: Mycoplasma hominis: a review of its role as a respiratory
tract pathogen of humans. Sex Transm Dis 1983, 10:335-340.
3. Goldenberger D, Kunzli A, Vogt P, Zbinden R, Altwegg M: Molecular
diagnosis of bacterial endocarditis by broad-range PCR amplification
and direct sequencing. J Clin Microbiol 1997, 35:2733-2739.
4. Meyer RD, Clough W: Extragenital Mycoplasma hominis infections in
adults: emphasis on immunosuppression. Clin Infect Dis 1993, 17(Suppl 1):
S243-S249.
5. Duffy LB, Crabb D, Searcey K, Kempf MC: Comparative potency of
gemifloxacin, new quinolones, macrolides, tetracycline and clindamycin
against Mycoplasma spp. J Antimicrob Chemother 2000, 45(Suppl 1):29-33.
6. Krausse R, Schubert S: In-Vitro Activities of Tetracyclines, Macrolides,
Fluoroquinolones and Clindamycin against Mycoplasma hominis and
Ureaplasma ssp. isolated in Germany over 20 years. Clin Microbiol Infect
2010, 16(11):1649-55.
7. Ngan CC, Lim T, Choo CM, Toh GL, Lim YS: Susceptibility testing of
Singapore strains of Mycoplasma hominis to tetracycline, gatifloxacin,
moxifloxacin, ciprofloxacin, clindamycin, and azithromycin by the Etest
method. Diagn Microbiol Infect Dis 2004, 48:207-210.
8. Pascual A, Jaton-Ogay K, Ninet B, Bille J, Greub G: New Diagnostic RealTime PCR for Specific Detection of Mycoplasma hominis DNA. Int J
Microbiol 2010, 2010:317512.
9. Fenollar F, Gauduchon V, Casalta JP, Lepidi H, Vandenesch F, Raoult D:
Mycoplasma endocarditis: two case reports and a review. Clin Infect Dis
2004, 38:e21-e24.
10. Garcia-de-la-Fuente C, Minambres E, Ugalde E, Saez A, Martinez-Martinez L,
Farinas MC: Post-operative mediastinitis, pleuritis and pericarditis due to
Mycoplasma hominis and Ureaplasma urealyticum with a fatal outcome.
J Med Microbiol 2008, 57:656-657.
11. Kupila L, Rantakokko-Jalava K, Jalava J, Peltonen R, Marttila RJ, Kotilainen E,
et al: Brain abscess caused by Mycoplasma hominis: a clinically
recognizable entity? Eur J Neurol 2006, 13:550-551.
12. Rohner P, Schnyder I, Ninet B, Schrenzel J, Lew D, Ramla T, et al: Severe
Mycoplasma hominis infections in two renal transplant patients. Eur J
Clin Microbiol Infect Dis 2004, 23:203-204.
13. Fabbri J, Tamm M, Frei R, Zimmerli W: [Mycoplasma hominis empyema
following pleuropneumonia in late pregnancy]. Schweiz Med Wochenschr
1993, 123:2244-2246.
14. Garcia C, Ugalde E, Monteagudo I, Saez A, Aguero J, Martinez-Martinez L,
et al: Isolation of Mycoplasma hominis in critically ill patients with
pulmonary infections: clinical and microbiological analysis in an
intensive care unit. Intensive Care Med 2007, 33:143-147.
15. Madoff S, Hooper DC: Nongenitourinary infections caused by
Mycoplasma hominis in adults. Rev Infect Dis 1988, 10:602-613.
16. Norton R, Mollison L: Mycoplasma hominis pneumonia in aboriginal
adults. Pathology 1995, 27:58-60.
17. Ti TY, Dan M, Stemke GW, Robertson J, Goldsand G: Isolation of
Mycoplasma hominis from the blood of men with multiple trauma and
fever. JAMA 1982, 247:60-61.
18. Waites KB, Bbar CM, Roberston JA, Talkngton DF, Kenny GE, editors:
Cumitech 34: laboratory diagnosis of mycoplasmal infections. American
Society for Microbiology, Washington D.C 2001.
19. Kenny GE, Cartwright FD: Susceptibilities of Mycoplasma hominis,
M. pneumoniae, and Ureaplasma urealyticum to GAR-936, dalfopristin,
dirithromycin, evernimicin, gatifloxacin, linezolid, moxifloxacin,
quinupristin-dalfopristin, and telithromycin compared to their
susceptibilities to reference macrolides, tetracyclines, and quinolones.
Antimicrob Agents Chemother 2001, 45:2604-2608.
Page 4 of 4
20. Samra Z, Rosenberg S, Soffer Y: In vitro susceptibility of Mycoplasma
hominis clinical isolates to tetracyclines, quinolones and macrolides.
Diagn Microbiol Infect Dis 2002, 44:359-361.
21. Ullmann U, Schubert S, Krausse R: Comparative in-vitro activity of
levofloxacin, other fluoroquinolones, doxycycline and erythromycin
against Ureaplasma urealyticum and Mycoplasma hominis. J Antimicrob
Chemother 1999, 43(Suppl C):33-36.
22. Waites KB, Canupp KC, Kenny GE: In vitro susceptibilities of Mycoplasma
hominis to six fluoroquinolones as determined by E test. Antimicrob
Agents Chemother 1999, 43:2571-2573.
23. Waites KB, Crabb DM, Duffy LB: Comparative in vitro activities of the
investigational fluoroquinolone DC-159a and other antimicrobial agents
against human mycoplasmas and ureaplasmas. Antimicrob Agents
Chemother 2008, 52:3776-3778.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1471-2334/10/335/prepub
doi:10.1186/1471-2334-10-335
Cite this article as: Pascual et al.: Mycoplasma hominis necrotizing
pleuropneumonia in a previously healthy adolescent. BMC Infectious
Diseases 2010 10:335.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color figure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Pref - 2 - Grammar 1.2 - Revisión Del IntentoDocument2 pagesPref - 2 - Grammar 1.2 - Revisión Del IntentoJuan M. Suarez ArevaloNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- CAC Bubble DiagramsDocument12 pagesCAC Bubble Diagramsangst6250No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Ii 2015 1Document266 pagesIi 2015 1tuni santeNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- TranscriptDocument1 pageTranscriptapi-310448954No ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Latihan To: Nilai: 7.4 Benar: 37 Salah: 13Document17 pagesLatihan To: Nilai: 7.4 Benar: 37 Salah: 13glensNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Math 202 Syllabus-Spring18 PDFDocument2 pagesMath 202 Syllabus-Spring18 PDFvonacoc49No ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- DEEP ECOLOGY - An Intro - McLaughlinDocument5 pagesDEEP ECOLOGY - An Intro - McLaughlinCarlo MagcamitNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- 2 Contoh Narative TextDocument9 pages2 Contoh Narative TextRini RienzNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- IPC's 2 Edition of Guidance Manual For Herbs and Herbal Products Monographs ReleasedDocument1 pageIPC's 2 Edition of Guidance Manual For Herbs and Herbal Products Monographs ReleasedRakshaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Pythagorean Theorem WorksheetDocument11 pagesPythagorean Theorem WorksheetJames ChanNo ratings yet
- 412 X 7 Va CJ CSDocument1 page412 X 7 Va CJ CSRajesh KumarNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Upaam 1135891 202105060749199700Document18 pagesUpaam 1135891 202105060749199700Kartik KapoorNo ratings yet
- Tran-Effects of Assisted JumpingDocument5 pagesTran-Effects of Assisted JumpingyoungjessNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Academic Reading: All Answers Must Be Written On The Answer SheetDocument21 pagesAcademic Reading: All Answers Must Be Written On The Answer SheetLemon MahamudNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Disectie AnatomieDocument908 pagesDisectie AnatomieMircea SimionNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unofficial Aterlife GuideDocument33 pagesThe Unofficial Aterlife GuideIsrael Teixeira de AndradeNo ratings yet
- Bio (RocessDocument14 pagesBio (RocessVijay SansanwalNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- By This Axe I Rule!Document15 pagesBy This Axe I Rule!storm0% (1)
- ST 36Document4 pagesST 36ray72roNo ratings yet
- Motor CAT C13 AcertDocument3 pagesMotor CAT C13 AcertJosé Gonzalez100% (4)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Milviz F-15e Poh V 2Document499 pagesMilviz F-15e Poh V 2Jose Ramon Martinez GutierrezNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- 1ST SUMMATIVE TEST FOR G10finalDocument2 pages1ST SUMMATIVE TEST FOR G10finalcherish austriaNo ratings yet
- Binder 3 of 4 Dec-2018Document1,169 pagesBinder 3 of 4 Dec-2018Anonymous OEmUQuNo ratings yet
- Sw34 Religion, Secularism and The Environment by NasrDocument19 pagesSw34 Religion, Secularism and The Environment by Nasrbawah61455No ratings yet
- Updating - MTO I - Unit 2 ProblemsDocument3 pagesUpdating - MTO I - Unit 2 ProblemsmaheshNo ratings yet
- Energy Transfer in Cell During Exercise and Oxygen Metabolism and Transport - PalakDocument85 pagesEnergy Transfer in Cell During Exercise and Oxygen Metabolism and Transport - Palakpalooo4No ratings yet
- Earth Sciences Notes Csir-Ugc Net JRFDocument57 pagesEarth Sciences Notes Csir-Ugc Net JRFmanas773No ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Variable Resistor Has Been AdjustedDocument3 pagesThe Variable Resistor Has Been AdjustedPank O RamaNo ratings yet
- Tabel Gsi, RMR, RmiDocument4 pagesTabel Gsi, RMR, RmiPup BooNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)