Professional Documents
Culture Documents
907 Full
Uploaded by
isan15Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
907 Full
Uploaded by
isan15Copyright:
Available Formats
Journal of Medical Microbiology (2008), 57, 907908
Case Report
DOI 10.1099/jmm.0.2008/000471-0
Isolation of Helcococcus kunzii from plantar
phlegmon in a vascular patient
Nadine LemaItre,1 Dominique Huvent,2 Caroline Loez,1 Frederic Wallet1
and Rene J. Courcol1
Correspondence
Nadine LemaItre
n-lemaitre@chru-lille.fr
Received 16 January 2008
Accepted 18 March 2008
Laboratoire de Bacteriologie-Hygie`ne, Centre de Biologie-Pathologie, Centre Hospitalier Regional
Universitaire, Lille, France
Service de Soins de Suite et Readaptation, Centre Hospitalier Regional Universitaire, Lille, France
Helcococcus kunzii has previously been considered to belong to the normal skin flora of podiatry
patients. Here, H. kunzii was isolated in abundance from a pus specimen collected by incision and
drainage of plantar phlegmon. This fastidious Gram-positive species was unambiguously
identified with the colorimetric VITEK 2 GP card identification system. This suggests that this
phenotypic identification system is able to identify promptly H. kunzii, which should be considered
a potential pathogen.
Case report
A 79-year-old man was hospitalized in December 2006 due
to gangrenous ischaemia of the third right toe and a right
ankle ulcer. There was a history of hypertension associated
with severe intermittent claudication in both legs. Indeed, 3
months before the current admission, in September 2006,
the patient underwent a first amputation of the fourth left
toe associated with percutaneous transluminal angioplasty
(PTA) because of focal stenosis of the left and right
superficial femoral and left popliteal arteries. After PTA,
the distal blood flow was restored.
On admission in December 2006, the patient had no
systemic signs of infection and was metabolically stable. On
examination, the right popliteal, dorsalis pedis and
posterior tibial pulses were absent, as were the left dorsalis
pedis and posterior tibial pulses. The Doppler ultrasound
detected no flow in the right posterior and anterior tibial
arteries. Plain radiography showed osteitis of the third
right toe and amputation was done. One intraoperative
bone biopsy was positive by culture for Enterococcus
faecalis, Klebsiella oxytoca and meticillin-susceptible
Staphylococcus aureus. After completion of 3 weeks of
amoxicillin/clavulanate, the patient was discharged home.
Four months later, in April 2007, the patient was
hospitalized in a re-education centre for local care of a
right heel ulcer and non-healing surgical wound of the
third right toe amputation. In fact, at the time of
admission, the patient exhibited right plantar phlegmon,
the temperature was 37.8 uC and blood pressure was 157/
57 mmHg. Laboratory findings were a white blood cell
count of 24 000 mm23 with 90 % polymorphonuclear
leukocytes, a sedimentation rate of 111 min (normal value
310 min) and a C-reactive protein level of .200 mg l21
(normal value ,6 mg l21). The patient was referred to a
2008/000471 G 2008 SGM Printed in Great Britain
vascular surgeon to consider operative exploration. The
Doppler ultrasound revealed that the lower limb arteries
were occluded bilaterally. The surgeon performed curative
surgical debridement and the phlegmon was incised and
drained. Wound fluid as well as deep tissue biopsies were
collected intraoperatively for microbiological examination.
Microbiological investigation
The examination of a Gram-stained smear of the
intraoperative samples showed numerous polymorphonuclear leukocytes and a mixture of Gram-positive cocci
and Gram-negative bacilli. The specimens were inoculated
onto Columbia agar containing 5 % horse blood, bromocresol purple (BCP) agar and in Brain Heart Infusion
(BHI) broth and incubated aerobically for 24 h at 37 uC. A
Viande Levure (VL) agar plate was also incubated under
anaerobic conditions for 48 h at 37 uC. After 24 h of
incubation under aerobic conditions, a heavy growth of
pinpoint, slightly grey and a-haemolytic colonies appeared
on the Columbia agar associated with a few colonies of
coliforms subsequently identified as Klebsiella oxytoca,
which was also recovered on BCP agar. A Gram stain of the
pinpoint colonies showed Gram-positive cocci arranged in
pairs and clusters but not in chains. These colonies were
catalase- and oxidase-negative. A Gram smear and the
subculture of the BHI yielded a similar mixture of Grampositive cocci and Gram-negative bacilli. In addition to
pinpoint colonies and colonies of K. oxytoca, strictly
anaerobic bacilli, later identified as Bacteroides fragilis, grew
on the VL agar plate incubated anaerobically. The enzyme
profile and biochemical characteristics of the Grampositive cocci were determined by the colorimetric
VITEK 2 GP card identification system (bioMerieux).
The isolate gave positive reactions for leucine arylamidase,
907
N. LemaItre and others
alanine arylamidase, L-pyrolidonylarylamidase, b-galactosidase, D-mannose and b-galactopyranosidase and was
identified as Helcococcus kunzii with a probability of 99 %.
To confirm this identification, partial sequencing of the
16S rDNA was performed. Pair-wise alignments of the 16S
rRNA gene showed that the isolate was 99 % identical to H.
kunzii lodged in GenBank with the accession number
DQ082899.1 (Woo et al., 2005). Antimicrobial susceptibility testing as determined by the disc diffusion method
using MuellerHinton agar supplemented with 5 % sheep
blood showed that the isolate of H. kunzii was susceptible
to penicillin, ampicillin, aminoglycosides and vancomycin.
Discussion
H. kunzii was first described in 1993. This species grows
slowly and shares many phenotypic characteristics with
other fastidious Gram-positive cocci such as Aerococcus
viridans (Collins et al., 1993). H. kunzii is considered to be
part of the normal flora of the skin of the lower extremities
(Haas et al., 1997). However, underlying conditions such as
diabetes and/or vascular insufficiencies may be linked to
colonization with H. kunzii and this species might be a
component of the polymicrobial flora of lower extremity
ulcers (Caliendo et al., 1995; Haas et al., 1997). Thus
isolation in mixed superficial culture, particularly with
Staphylococcus aureus, makes it difficult to demonstrate a
clear-cut pathogenic role for this species (Caliendo et al.,
1995; Haas et al., 1997) in diabetic or vascular foot ulcers.
Here, H. kunzii was isolated along with enteric bacteria and
anaerobes from a foot infection in a non-diabetic vascular
patient, as previously described (Haas et al., 1997).
However, the presence of H. kunzii by Gram staining and
from two separate deep samples, in abundance, suggested
that H. kunzii may play a pathogenic role in the phlegmon.
In addition, some authors reported the isolation of H.
kunzii in pure culture from life-threatening invasive
infections such as primary bacteraemia and empyema
thoracis in two intravenous-drug users (Woo et al., 2005).
Moreover, H. kunzii has also been isolated from an infected
sebaceous cyst associated with cellulitis (Peel et al., 1997),
from a breast abscess (Chagla et al., 1998) and from a postsurgical foot abscess (Riegel & Lepargneur, 2003) in
immunocompetent patients. These reports demonstrated
that H. kunzii plays a potential pathogenic role. Therefore,
routine bacteriological laboratories should be able to
908
identify promptly this organism. Unfortunately, H. kunzii
resembles several members of various fastidious cocci and
some commercial systems such as API systems can fail to
identify this species. Usually, the API 20 STREP profile of
H. kunzii corresponds to a doubtful Aerococcus viridans
with a numerical profile of 4100413 (Chagla et al., 1998;
Haas et al., 1997; Woo et al., 2005). Similarly, the VITEK 2
system combined with fluorometric cards misidentified H.
kunzii (Wallet et al., 2005) and the ability of other
automated systems such as BD Phoenix to identify
correctly H. kunzii is unknown. In contrast, the VITEK 2
colorimetric system, which is known to better identify
members of the Streptococcaceae (Wallet et al., 2005), can
provide discriminating identification of H. kunzii by
analysis of 43 biochemical characters. This last automated
system is a good alternative to 16S rRNA sequencing,
which may not be routinely available in many laboratories.
References
Caliendo, A. M., Jordan, C. D. & Ruoff, K. L. (1995). Helcococcus, a new
genus of catalase-negative, gram-positive cocci isolated from clinical
specimens. J Clin Microbiol 33, 16381639.
Chagla, A. H., Borczyk, A. A., Facklam, R. R. & Lovgren, M. (1998).
Breast abscess associated with Helcococcus kunzii. J Clin Microbiol 36,
23772379.
Collins, M. D., Facklam, R. R., Rodrigues, U. M. & Ruoff, K. L. (1993).
Phylogenetic analysis of some Aerococcus-like organisms from clinical
sources: description of Helcococcus kunzii gen. nov., sp. nov. Int J Syst
Bacteriol 43, 425429.
Haas, J., Jernick, S. L., Scardina, R. J., Teruya, J., Caliendo, A. M. &
Ruoff, K. L. (1997). Colonization of skin by Helcococcus kunzii. J Clin
Microbiol 35, 27592761.
Peel, M. M., Davis, J. M., Griffin, K. J. & Freedman, D. L. (1997).
Helcococcus kunzii as sole isolate from an infected sebaceous cyst.
J Clin Microbiol 35, 328329.
Riegel, P. & Lepargneur, J. P. (2003). Isolation of Helcococcus kunzii
from a post-surgical foot abscess. Int J Med Microbiol 293, 437439.
Wallet, F., Loez, C., Renaux, E., Lemaitre, N. & Courcol, R. J. (2005).
Performances of VITEK 2 colorimetric cards for identification of
Gram-positive and Gram-negative bacteria. J Clin Microbiol 43,
44024406.
Woo, P. C., Tse, H., Wong, S. S., Tse, C. W., Fung, A. M., Tam, D. M.,
Lau, S. K. & Yuen, K. Y. (2005). Life-threatening invasive Helcococcus
kunzii infections in intravenous-drug users and ermA-mediated
erythromycin resistance. J Clin Microbiol 43, 62056208.
Journal of Medical Microbiology 57
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Dole Annual Medical Report Sample Amp GuideDocument5 pagesDole Annual Medical Report Sample Amp Guidehr.ionhotelNo ratings yet
- Journal Reading HIVDocument20 pagesJournal Reading HIVayuni fatriciaNo ratings yet
- Palpation and Percussion of The Abdomen: Physical Inspection, AuscultationDocument10 pagesPalpation and Percussion of The Abdomen: Physical Inspection, AuscultationbagasNo ratings yet
- Sífilis Ocular 2021 Super CompletoDocument69 pagesSífilis Ocular 2021 Super CompletoouranpisNo ratings yet
- Increases in COVID 19 Are Unrelated To Levels of Vaccination Across 68 Countries and 2947 Counties in The United StatesDocument4 pagesIncreases in COVID 19 Are Unrelated To Levels of Vaccination Across 68 Countries and 2947 Counties in The United StatesKyle Becker95% (19)
- Late Puerperal Sepsis, Case Report and Literature ReviewDocument10 pagesLate Puerperal Sepsis, Case Report and Literature ReviewMuskanNo ratings yet
- Compre paraDocument103 pagesCompre paraDeniebev'z OrillosNo ratings yet
- 22.0 Infection Control and Prevention QuizDocument3 pages22.0 Infection Control and Prevention QuizHassan Abdallah M. AliNo ratings yet
- Immunesera ProductionDocument22 pagesImmunesera Productionnilima nikaljeNo ratings yet
- Virology UG Class IV SemesterDocument109 pagesVirology UG Class IV Semestervallabhaneni rajesh100% (1)
- Tests From The Database Croc 2Document30 pagesTests From The Database Croc 2Андрій ВознякNo ratings yet
- Sasa MapDocument2 pagesSasa MapmaliksuneelNo ratings yet
- NCERT Exemplar Solutions For Class 8 Science Chapter 2 Microorganisms Friend and FoeDocument10 pagesNCERT Exemplar Solutions For Class 8 Science Chapter 2 Microorganisms Friend and FoePradipti VermaNo ratings yet
- Skin and Soft Tissue InfectionsDocument8 pagesSkin and Soft Tissue InfectionsMARTIN REY EDRICK SANTOSNo ratings yet
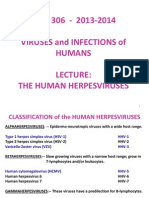
- 13-14 MBB306 Lecture 5 The Herpesviruses - RJDocument28 pages13-14 MBB306 Lecture 5 The Herpesviruses - RJAnonymous PyUR1NINo ratings yet
- Medical Microbiology at A Glance EbookDocument70 pagesMedical Microbiology at A Glance EbookAnkita ShuklaNo ratings yet
- Medmastery Antimicrobial - Stewardship - HandbookDocument65 pagesMedmastery Antimicrobial - Stewardship - HandbookHhaNo ratings yet
- Immunology and SerologyDocument15 pagesImmunology and SerologysherwinbuluranNo ratings yet
- Biological ClasifficationDocument6 pagesBiological Clasifficationchannel of dhyanaNo ratings yet
- Biological HazardDocument2 pagesBiological HazardBryan JamesNo ratings yet
- BibliographyDocument2 pagesBibliographyapi-197414643No ratings yet
- 11-Microbiology of Milk and Milk ProductDocument14 pages11-Microbiology of Milk and Milk Productguestiam29No ratings yet
- Week 9.IMCI Case Study - JennyDocument7 pagesWeek 9.IMCI Case Study - JennyGeorgia Shayne CubeloNo ratings yet
- Communicable DiseasesDocument17 pagesCommunicable DiseasesKriska NoelleNo ratings yet
- DRUG STUDY (Cephalexin)Document2 pagesDRUG STUDY (Cephalexin)Avianna CalliopeNo ratings yet
- Microbiology and Genetics Course Outline Spring 2014Document3 pagesMicrobiology and Genetics Course Outline Spring 2014api-244509569No ratings yet
- 101 Shocking Science Facts PDFDocument210 pages101 Shocking Science Facts PDFAjith Cristiano100% (1)
- Jurnal GlomerulonefritisDocument12 pagesJurnal GlomerulonefritiszoddickgNo ratings yet
- Veterinary Clinical Pathology Clerkship ProgramDocument46 pagesVeterinary Clinical Pathology Clerkship ProgramDrVijayata ChoudharyNo ratings yet
- ONE HEALTH Presentation of VPHDocument37 pagesONE HEALTH Presentation of VPHsufian abdo jilo100% (2)