Professional Documents
Culture Documents
BIPN102 - Worksheet 3 Key PDF
Uploaded by
tcd_usaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BIPN102 - Worksheet 3 Key PDF
Uploaded by
tcd_usaCopyright:
Available Formats
Course: BIPN 102
TA: Irfan Haider
Section: Tue 6PM at Center 207
Worksheet 3
Email: ihaider@ucsd.edu
OH: Tue & Thur 9:30-10:45 AM
at PC Theater Lobby
1. a. What is an obstructive disease? What is a restrictive disease?
Obstructive lung disease is a category of respiratory disease characterized
by airway obstruction. It is generally characterized by inflamed and easily
collapsible airways, obstruction to airflow and problems exhaling.
Restrictive lung disease is a category of extrapulmonary or pleural diseases that
restrict lung expansion (e.g.: increased diffusion barrier thickness or lack of
surfactant).
b. Give an example of an obstructive disease.
Asthma: Decreases bronchiole radius due to smooth muscle spasm.
Bronchitis: inflammation due to infection decreases radius in the bronchi, increasing
resistance to airflow. Mucus build-up contributes to decreased radius as well.
Emphysema: When patients try to expire forcefully, their airways get compressed
more than normal because of destroyed elastic fibers, greatly increasing resistance
to airflow.
c. Given an example of a restrictive disease and explain why.
Pulmonary Fibrosis: collagen build up makes the lungs stiffer and harder to inflate.
Infant Respiratory Distress Syndrome: lack of surfactant making it harder to inflate
lungs.
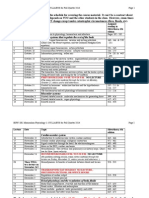
2. Compare and contrast obstructive and restrictive diseases by filling the table below
(increase; decrease; normal):
Obstructive disease Measured lung parameter Restrictive disease
Normal/
IRV (Inspiratory Reserve V.)
ERV (Expiratory Reserve V.)
Normal/
Normal/
RV (Residual V.)
VC (Vital Capacity)
Normal/
TLC (Total Lung Cap.)
Worksheet 3
Page 1 of 6
Course: BIPN 102
TA: Irfan Haider
Section: Tue 6PM at Center 207
Compliance
FEV1/FVC
Email: ihaider@ucsd.edu
OH: Tue & Thur 9:30-10:45 AM
at PC Theater Lobby
3. Explain what FEV1 and FVC stand for. Also, mention the ratios for normal lungs,
lungs with obstructive disease and lung with restrictive disease.
Expiratory Spirometer test will test the ratio of the volume expired during the first
second of expiration to the entire amount of air expired during the entire process of
expiration.
The first second of expiration is called the FEV1 (Functional Expiratory Volume in 1
second).
The entire volume that can be forcefully exhaled is called the FVC. The ratio between
the two can give us insight about the healthiness of the patient.
Normal FEV/FVC will equal to 80%.
Restrictive diseases will make the ratio >80%.
Obstructive diseases will make the ratio <80%.
4. For a person standing upright, indicate whether each property of the lung is higher
at the top of the lung or the bottom.
Note: Top refers to the apex of the lung. Bottom refers to the base of the lung.
Worksheet 3
Page 2 of 6
Course: BIPN 102
TA: Irfan Haider
Section: Tue 6PM at Center 207
Email: ihaider@ucsd.edu
OH: Tue & Thur 9:30-10:45 AM
at PC Theater Lobby
Higher
Top Bottom
Ventilation
x
Perfusion
x
V/Q ratio
x
Alveolar Compliance
x
PO2
x
Worksheet 3
Page 3 of 6
Course: BIPN 102
TA: Irfan Haider
Section: Tue 6PM at Center 207
5. What is Henrys Law?
Email: ihaider@ucsd.edu
OH: Tue & Thur 9:30-10:45 AM
at PC Theater Lobby
conc. of gas in a liquid = partial pressure of gas (gas phase) x solubility of gas in
liquid
6. a. What is the normal partial pressure of oxygen in the arterioles/arteries and
venules/veins? What is the normal partial pressure of carbon dioxide in the
arterioles/arteries and venules/veins?
Oxygen: 100 mmHg in arterioles/arteries and 40 mmHg in venules/veins.
Carbon dioxide: 40 mmHg in arterioles/arteries and 46 mmHg in venules/veins.
Extra Info:
Oxygen: 150 mmHg in fresh inhaled air and 100 mmHg in the alveoli
Carbon dioxide: 0 mmHg in fresh inhaled air and 40 mmHg in the alveoli
b. Although it may seem that Oxygen has a higher driving force (pressure gradient of
60 mmHg), Carbon Dioxide actually diffuses a lot faster than Oxygen. How does this
work?
The pressure difference for oxygen is 60 mmHg, while it is 6 mmHg for carbon
dioxide. However, the solubility of carbon dioxide is 20 times that of oxygen. So, 6
mmHg x 20 = 120 mmHg for carbon dioxide, a greater driving force.
c. What are the values of PO2 and PCO2 at:
The first 150 mL of expiration:
PO2 = 150 mmHg, PCO2 = 0 mmHg.
(due to dead space)
Last part of expiration:
PO2= about 100 mmHg or less, PCO2= about 46 mmHg or less
d. In normal conditions, uptake of oxygen is not limited by ____________________ but is
limited by ____________________. In a person with a respiratory disease, uptake of
oxygen is not limited by ____________________ but is limited by ____________________.
Answers: diffusion, perfusion, perfusion, diffusion.
Worksheet 3
Page 4 of 6
Course: BIPN 102
TA: Irfan Haider
Section: Tue 6PM at Center 207
Email: ihaider@ucsd.edu
OH: Tue & Thur 9:30-10:45 AM
at PC Theater Lobby
7. a. Describe the pressure and resistance in the pulmonary circulation vs. systemic
circulation. What accounts for the differences?
Pulmonary circulation has a much lower pressure and resistance. The systemic
circulation has higher pressure and resistance because it has to pump against
gravity and through a greater length (throughout the extremities).
b. If the pulmonary circulation experiences vasodilation, what must have happened
to venous and arterial pressures?
Pulmonary circulation must have experienced increased pressure from blood. This
vasodilation results in decreased resistance to blood flow (decrease in pulmonary
vascular resistance).
c. What are the two mechanisms by which pulmonary vascular resistance is
changed?
1. Distension: Increasing radius of the vessels. Think of Poiseuilles Law.
2. Recruitment: Increased number of blood vessels are opened up to blood flow
(increased cross sectional area).
8. a. What causes vasodilation in the systemic arterioles? Why? Which of these causes
is the most important for vasodilation to occur?
Decrease in partial pressure of oxygen (most important), increase in partial
pressure of carbon dioxide, decrease in pH. This works as a negative feedback loop.
b. What causes vasoconstriction in the pulmonary arterioles? Why?
All the same things listed for part a). When there are low levels of oxygen available,
certain arterioles are closed off to allow blood to perfuse past alveoli with the most
oxygen. This is the bodys way of picking up oxygen efficiently.
9. a. Lets say V/Q (ventilation/perfusion) ratio is optimal at a value of 1 for a specific
person. If a person has an overall V/Q ratio greater than 1, what does this say about
Worksheet 3
Page 5 of 6
Course: BIPN 102
TA: Irfan Haider
Section: Tue 6PM at Center 207
Email: ihaider@ucsd.edu
OH: Tue & Thur 9:30-10:45 AM
at PC Theater Lobby
alveolar PO2 and how will the bronchioles, pulmonary arterioles, and systemic
arterioles react?
This means that alveolar PO2 is increased and bronchioles will vasoconstrict,
pulmonary arterioles will vasodilate, and systemic arterioles will vasoconstrict.
b. If a person has an overall V/Q ratio less than 1, what does this say about alveolar
PO2 and how will the bronchioles, pulmonary arterioles, and systemic arterioles
react?
This means that alveolar PO2 is decreased and bronchioles will vasodilate,
pulmonary arterioles will vasoconstrict, and systemic arterioles will vasodilate.
10. Describe two serious physiological issues that can arise when someone is at very
high altitudes.
1. Cerebral edema: Increased blood pressure in brain due to dilation from low PO2
in the atmosphere causes net fluid movement out of the capillaries and into the
brain tissues. Since the skull is a non-expandable container, an increase in the
volume (due to excess fluid) will cause increase in pressure inside the skill. This
can be treated by putting the afflicted person in a pressure chamber with high
levels of PO2.
2. Pulmonary edema: The vasoconstriction of pulmonary arterioles throughout the
lungs results from low PO2 in the atmosphere. This vasoconstriction causes an
increased pulmonary arterial pressure, which combined with capillary damage
due to hypoxia causes more fluid to move into lung tissues and cause edema.
This makes breathing more difficult due to the increased distance that the gas
has to diffuse between alveoli and capillaries.
Worksheet 3
Page 6 of 6
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- 041917Document4 pages041917tcd_usaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Antiemetic Prophylaxis For CINV NEJM 2016Document12 pagesAntiemetic Prophylaxis For CINV NEJM 2016tcd_usaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Journal Club Handout FinalDocument5 pagesJournal Club Handout Finaltcd_usaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- BIPN102 - Worksheet 4 Key PDFDocument4 pagesBIPN102 - Worksheet 4 Key PDFtcd_usaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- BIPN102 - Worksheet 2 Key PDFDocument6 pagesBIPN102 - Worksheet 2 Key PDFtcd_usaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- BIPN102 - Worksheet 1 Key PDFDocument5 pagesBIPN102 - Worksheet 1 Key PDFtcd_usaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A2-3 Team 11 Fuel Cell X PDFDocument14 pagesA2-3 Team 11 Fuel Cell X PDFtcd_usaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- BILD 2 BiologyDocument6 pagesBILD 2 Biologytcd_usaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- CENG 122 Fall 2014 Syllabus Zhang CurriculumDocument3 pagesCENG 122 Fall 2014 Syllabus Zhang Curriculumtcd_usaNo ratings yet
- Weekly Check ListDocument1 pageWeekly Check Listtcd_usaNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Reverse OsmosisDocument2 pagesReverse Osmosistcd_usaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Job Search Handbook BookmarkedDocument52 pagesJob Search Handbook BookmarkedFlorence LeungNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- BIPN 100 Syllabus Fa14Document2 pagesBIPN 100 Syllabus Fa14tcd_usaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- CENG 122 Fall 2014 Syllabus Zhang CurriculumDocument3 pagesCENG 122 Fall 2014 Syllabus Zhang Curriculumtcd_usaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- AD ConversionDocument5 pagesAD Conversiontcd_usaNo ratings yet
- Molecular Biology R - F - Weaver 5th EdDocument1 pageMolecular Biology R - F - Weaver 5th EdAlapan NandaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Copd Action Plan PDFDocument2 pagesCopd Action Plan PDFdtech2No ratings yet
- Unit 2 - Innovations in Health and Medicine (Paragraphs)Document1 pageUnit 2 - Innovations in Health and Medicine (Paragraphs)April ThunNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- HIDROKELDocument22 pagesHIDROKELfairuz hanifahNo ratings yet
- Export Act 1963Document27 pagesExport Act 1963Anonymous OPix6Tyk5INo ratings yet
- Peritoneal DialysisDocument3 pagesPeritoneal DialysisSumit YadavNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Anatomy of BreathingDocument6 pagesThe Anatomy of BreathingmihaiylaNo ratings yet
- Case Study Discussion (A)Document3 pagesCase Study Discussion (A)Bq dwi EvaNo ratings yet
- Myofascial Trigger PointsDocument17 pagesMyofascial Trigger PointsVera Belchior100% (3)
- Rhinitis MedicamentosaDocument22 pagesRhinitis MedicamentosaDanti NurdindayantiNo ratings yet
- SAMPLE ELC151 - Final - TEST - PDFDocument11 pagesSAMPLE ELC151 - Final - TEST - PDFNara SakuraNo ratings yet
- Nursing Care of HydronephrosisDocument19 pagesNursing Care of Hydronephrosisvictor zhefaNo ratings yet
- Inles 4Document2 pagesInles 4Astrid CruzNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- 1116005I Rev. 02Document2 pages1116005I Rev. 02kirubel demelashNo ratings yet
- BIO 1 Course Syllabus UPDDocument3 pagesBIO 1 Course Syllabus UPDDanielle Marie100% (1)
- Common Metabolic DisordersDocument7 pagesCommon Metabolic DisordersDevika RajNo ratings yet
- Anti Malarial Drugs by Salaria AnamikaDocument10 pagesAnti Malarial Drugs by Salaria AnamikaSalaria Anamika100% (1)
- Personal Trainer Magazine ISSUE 13Document45 pagesPersonal Trainer Magazine ISSUE 13Jesmin AraNo ratings yet
- Request For Cashless Hospitalisation For Health Insurance Policy PART C (Revised)Document4 pagesRequest For Cashless Hospitalisation For Health Insurance Policy PART C (Revised)Abhishek MkNo ratings yet
- 2018 - ICRU 83 - BaliDocument86 pages2018 - ICRU 83 - BalisanggamNo ratings yet
- PDFDocument732 pagesPDFMahmud Eljaarani90% (10)
- Arthritis E-Book DF PDFDocument14 pagesArthritis E-Book DF PDFManuel Anthony Lopez0% (1)
- Chapter 22 Exile in DapitanDocument5 pagesChapter 22 Exile in DapitanJohn Terrence M. Romero83% (6)
- A Review of Fluid and Hydration in Competitive TennisDocument11 pagesA Review of Fluid and Hydration in Competitive TennisSilvio DantasNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Mental Health, Mental Illness, and Psychological Distress: Same Continuum or Distinct Phenomena?Document16 pagesMental Health, Mental Illness, and Psychological Distress: Same Continuum or Distinct Phenomena?ThiagoSoaresNo ratings yet
- Eating Disorder WebQuestDocument2 pagesEating Disorder WebQuestFiona Wang100% (1)
- 17-10 eJDD FinalDocument116 pages17-10 eJDD FinalMohamed GamalNo ratings yet
- Papaya Farming Land Preparation and Planting: Establishment of WindbreaksDocument9 pagesPapaya Farming Land Preparation and Planting: Establishment of WindbreaksmarcamilleNo ratings yet
- Corn FertilizationDocument8 pagesCorn FertilizationRaymond KatabaziNo ratings yet
- Acute MI DMII Medical ManagementDocument52 pagesAcute MI DMII Medical ManagementsherwincruzNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)