Professional Documents
Culture Documents
Epilepsia Volume 36 Issue 3 1995 [Doi 10.1111%2Fj.1528-1157.1995.Tb00993.x] Wolfgang Löscher; Dagmar Hönack; Angelika Richter; Hans-Ulrich -- New Injectable Aqueous Carbamazepine Solution Through Complexing With 2-H
Uploaded by
Franco CentCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Epilepsia Volume 36 Issue 3 1995 [Doi 10.1111%2Fj.1528-1157.1995.Tb00993.x] Wolfgang Löscher; Dagmar Hönack; Angelika Richter; Hans-Ulrich -- New Injectable Aqueous Carbamazepine Solution Through Complexing With 2-H
Uploaded by
Franco CentCopyright:
Available Formats
Epilepsia, 36(3):255-261, 1995
Raven Press, Ltd., New Yofk
0 International League Agamt Epilepsy
New Injectable Aqueous Carbamazepine Solution Through
Complexing with 2-Hydroxypropyl-~-Cyclodextrin:
Tolerability and Pharmacokinetics After Intravenous
Injection in Comparison to a
Glycofurol-Based Formulation
Wolfgang Loscher, Dagmar Honack, Angelika Richter, *Hans-Ulrich Schulz,
Michael Schurer, fRaija Dusing, and $Marcus E. Brewster
Department of Pharmacology, Toxicology and Pharmacy, School of Veterinary Medicine, Hannover; *LAFAA
Laboratory for Contract Research in Clinical Pharmacology and Biopharmaceutical Analytics GmbH, Bad
Schwartau; fDesitin Arzneimittel GmbH Hamburg, Germany; and SPharmos, Alachua, Florida, U . S . A .
Summary: The poor water solubility of the antiepileptic
drug (AED) carbamazepine (CBZ) is generally considered
an absolute contraindication to parenteral administration
in epileptic patients. However, the water solubility of
CBZ can be largely enhanced through formation of an
inclusion complex with an amorphous cyclodextrin derivative, 2-hydroxypropyl-~-cyclodextrin(HPPCD). We
studied tolerability and pharmacokinetics of an aqueous
CBZ:HPPCD solution after intravenous (i.v.) administration in dogs. For comparison, a conventional glycofurolbased solution of CBZ was used. We also administered a
commercial liquid formulation of CBZ orally (p.0.).
Infusion of CBZ:HPPCD solutions or HPPCD placebo formulations i.v. was well tolerated by the animals. In contrast, infusion of CBZ:glycofurol solutions and glycofurol
placebo solutions induced marked behavioral and cardiovascular adverse effects. Pharmacokinetic studies indicated that glycofurol inhibited CBZ metabolism by decreasing formation of the major CBZ metabolite CBZ10,ll-epoxide (CBZ-E). With infusion of CBZ:HPPCD 10
ml/min for 12-15 min, resulting in a CBZ dose of CBZ 5
mg/kg body weight, peak CBZ plasma levels of -3.6 pgl
ml were obtained. This relatively low peak concentration
is primarily due to the rapid elimination of CBZ in dogs
[half-life (t%) < 1 h]. Comparison of peak plasma levels
determined after p.0. administration of CBZ to dogs with
peak CBZ levels previously determined after p.0. administration in humans indicated that about four times higher
doses are needed in dogs to attain the same peak plasma
levels as in humans. In view of previous experimental
data showing rapid penetration of CBZ into brain, our
results indicate that aqueous CBZ:HPPCD solutions
might be ideally suited for parenteral use in acute clinical
conditions such as status epilepticus (SE), particularly
because CBZ is a drug with only minor respiratory or
cardiovascular effects. Key Words: Epilepsy-Cyclodextrins-Status epilepticus-Antiepileptic drugs-2H ydroxypropyl- P-c yclodextrin-PharmacokineticsDogs.
Carbamazepine (CBZ) is a major antiepileptic
drug (AED) with clinical efficacy against partial and
generalized convulsive seizures (Fromm, 1992).
One drawback to the drug is its insolubility in aqueous vehicles. Thus, no parenteral formulations of
CBZ are available for clinical use, although intravenous (i.v.) use of this drug would be desirable,
particularly for treatment of convulsive status epilepticus (SE). In several experimental studies of anticonvulsant potency and pharmacokinetics of CBZ
in animals, the drug was dissolved in polyethylene
glycol (PEG) (Levy et al., 1975; Ronfeld and Benet,
1975; Farghali-Hassan et al., 1976; Lockard et al.,
1979; Pate1 and Levy, 1980; Loscher and Honack,
1991), which, however, is not usable for i.v. administration in humans. More recently, Tauboll et al.
(1990) described the anticonvulsant activity of a solution of CBZ in glycofurol (PEG monotetrahydrofurfuryl ether; trade name Tetraglycol) in cats
Received November 1993; revision accepted January 1994.
Address correspondence and reprint requests to Dr. W.
Loscher at Department of Pharmacology, Toxicology and Pharmacy, School of Veterinary Medicine, Biinteweg 17, D-30559
Hannover, Germany.
255
W . LOSCHER ET AL.
256
and proposed that it might be possible to prepare a
glycofurol-based CBZ solution acceptable for human use. The anticonvulsant activity of CBZ solutions in glycofurol was also demonstrated by Loscher et al. (1990a,1991). However, we noted that
this solvent exerted effects of its own and markedly
potentiated the anticonvulsant and neurotoxic activity of AEDs (Loscher et al., 1990a). Similarly,
Yasaka et al. (1978) demonstrated that glycofurol
increased the pharmacologic actions of barbiturates
by altering drug distribution and elimination.
In the search for more inert solvents, cyclodextrins might be valuable candidates. Cyclodextrins
have been used extensively to increase the solubility, dissolution rate, and bioavailability of poorly
water-soluble drugs. The ability of cyclodextrins to
modify these characteristics has been attributed to
formation of an inclusion complex between cyclodextrins and guest drug molecules. Whereas the
unsubstituted crystalline cyclodextrins had limitations such as renal toxicity, more recently developed modified p-cyclodextrins have acceptable tolerability (Pitha et al., 1988; Brewster et al., 1990).
One of these modified cyclodextrins, 2-hydroxypropyl-P-cyclodextrin (HPPCD) was recently been
used to develop aqueous parenteral formulations of
CBZ (Brewster et al., 1991) and to improve oral
bioavailability of CBZ in rats (Choudhury and Nelson, 1992). In the present study, CBZ was solubilized for i.v. use by complexing with HPPCD, and
tolerability and pharmacokinetics of this newly developed aqueous parenteral solution of CBZ were
determined in dogs. Data obtained after i.v. administration of the cyclodextrin solution of CBZ were
compared with respective data of a glycofurol solution of the drug. Furthermore, a conventional commercial oral (p.0.) formulation of CBZ was used to
compare tolerability and pharmacokinetics of CBZ
after both i.v. and p.0. administration.
MATERIALS AND METHODS
Drugs
Three formulations of CBZ were used for the experiments in dogs: (a) A 20% aqueous solution of a
CBZ:HPPCD complex containing CBZ 10 mg/ml
solution, (b) a solution of 1% CBZ in 65% glycofurol, and (c) a commercial liquid oral formulation
(suspension) of CBZ containing 2% CBZ (Timonil).
The two parenteral formulations were diluted 1:20
by a 5% aqueous glucose solution immediately before i.v. administration; the p.0. formulation was
administered without dilution. Vehicle experiments
were performed with the parenteral formulations
(without CBZ) containing either 20% HPPCD or
Epilepsia, Vol. 36, No. 3 , 1995
65% glycofurol in the same way as those with the
CBZ-containing solutions. The undiluted CBZ or
placebo solutions were stable at room temperature
for at least 15 months when protected from light
(stability experiments were performed only in the
dark).
Animal experiments
Five male Beagle dogs aged 3-4.5 years and
weighing 10-13.5 kg were used. Each drug formulation and each vehicle (placebo formulation)
was tested in the same dogs, allowing direct comparison of tolerability and pharmacokinetics. Each
dog received the diverse drug and vehicle applications in a different succession. The time interval
between two experiments in the same dog was at
least 3 days. The parenteral formulations were administered i.v. into a vein of the foreleg by an infusion pump with an infusion rate of 10 ml/min for
~ 1 min,
5 depending on body weight of the individual dog. Because syringe with the solution for infusion had to be exchanged once or twice during infusion, the total time for infusion varied between 12
and 15 min in individual dogs. The total injected
volume was 10 ml CBZ or placebo formulations per
kg body weight, resulting in a total dose of 5 mg/kg
CBZ. This dosage was based on experiments in single dogs in which different i.v. doses (2.5, 3.75, or 5
mg/kg) of CBZ had been infused i.v. in 10-15 min.
At 5 mg/kg, peak plasma levels of -4 pg/ml were
achieved. Because our aim was to achieve CBZ
plasma levels of at least 4 pg/ml, i.e., the lower limit
for effectiveness against generalized tonic-clonic
seizures (GTC) in patients (Hvidberg, 1985), all subsequent i.v. experiments described in the present
study were performed with this dosage. For p.0.
administration of CBZ, the liquid p.0. formulation
was administered by gastric intubation at a volume
of 1 ml/kg body weight, corresponding to a dosage
of 20 mg/kg CBZ. This dosage was based on previous experiments using p.0. administration of CBZ
in dogs (Frey and Loscher, 1980).
During and after administration of the different
CBZ or placebo formulations, the dogs were closely
observed for behavioral and other observable adverse effects for at least 3 h. Furthermore, cardiovascular parameters [heart rate (HR), pulse, circulation in mucosa, ears] were evaluated.
For drug analysis in plasma, venous blood samples (2-3 ml) were taken before (blank), 5 min after
onset, and at the end of the i.v. infusion period as
well as 5 , 15, and 30 min and 1, 2, 3, 4, 5 , 6, and 8
h after discontinuation of infusion. In p.0. administration experiments, blood samples were taken at
the same times as in the i.v. experiments, except
25 7
PARENTERAL FORMULATIONS FOR CBZ
1). Concomitantly, all dogs showed hyperemization
of superficial blood vessels, indicating a decrease in
vascular tone. These cardiovascular effects were
observed for hours after discontinuation of infusion. Some dogs had edema of facial skin. Salivation and lacrimation also were observed. Behaviorally, all dogs appeared excited during infusion and
exhibited head and "wet dog" shakes; some dogs
also showed other stereotyped behavior, increased
locomotion, and ataxia for S 1 h after discontinuation of infusion. Based on the 1:20 dilution of the
glycofurol placebo formulation, the dose of glycofurol administered i.v. in these experiments was 325
mg/kg .
When the cyclodextrin CBZ solution was administered i.v. at a CBZ dose of 5 mg/kg body weight,
no cardiovascular or behavioral adverse effects
were observed (Table 1). In contrast, i.v. infusion
of the glycofurol-based CBZ solution induced pronounced cardiovascular and behavioral adverse effects that were almost identical to those observed
after infusion of the glycofurol placebo formulation.
Thus, HR and pulse frequency increased considerably (Table l), pulse was feeble and at times even
imperceptible, and hyperemization, increased salivation, and lacrimation were observed. Furthermore, the dogs showed excitation during infusion,
restlessness, head and wet dog shakes, and ataxia
for ~ 3 0 - 6 0min. In contrast to placebo, 4 of the 5
dogs showed reduced activity after the infusion of
CBZ:glycofurol solution. Furthermore, in contrast
to placebo, the effect of the CBZ:glycofurol solution on HR appeared to be biphasic, with a first
significant increase during infusion and a second
increase after 1 h (Table 1). After oral administration of CBZ at a dosage of 20 mg/kg, no cardiovascular or behavioral adverse effects were noted (Table 1).
that no samples were taken during administration
since CBZ was administered as p.0. bolus. In these
p.0. administration experiments, one additional
blood sample was taken after 10 h. All blood samples were collected in tubes with EDTA and immediately centrifuged, and plasma was stored deepfrozen until analysis.
Drug analysis
Determinations of CBZ and its major metabolite
CBZ-l0,ll-epoxide were made by a validated, sensitive, and specific high-performance liquid chromatography (HPLC) technique similar to the
method of Chelberg et al. (1988). Plasma levels are
mean values of duplicate determinations.
Pharmacokinetic analysis
Data after i.v. infusion and p.0. administration of
CBZ were analyzed kinetically by the PHARM/PCS
(version 4.2) program according to the methods of
Tallarida and Murray (1987).
Statistics
Significance of differences between experiments
was calculated by Student's t test for paired data.
RESULTS
Tolerability studies in dogs
No behavioral or cardiovascular adverse effects
were observed during or after i.v. infusion of the
HPPCD placebo formulation (Table 1). Based on
the 1:20 dilution of the HPpCD formulation before
use, the dose of HPPCD administered in these experiments was 100 mg/kg. In contrast to the experiments with the cyclodextrin, infusion of the glycofurol placebo formulation resulted in marked adverse effects. Thus, during the infusion, HR and
pulse rate increased significantly by -40% (Table
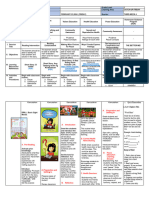
TABLE 1. Effect of different CBZ formulations and respective placebo solutions on heart rate in dogs
HR (beatshin)
Time after application
Formulation
F'redrug
control
HPpCD i.v.
CBZ:HPpCD i.v.
Glycofurol i.v.
CBZ:glycofuroli.v.
CBZ p.0.
117 f 26
126 f 21
116 f 20
1 1 1 f 18
114 f 15
During
infusion
(5 min)
118 f 27
126 f 12
167 ? 36"
176 33"
After infusion (or p.0. administration)
0 min
5 min
117 f 26
123 f 25
150 f 22"
118 f 12
-
122 f 17
115 f 14
156 f 35
115 f 33
110 9
15 min
113
113
f7
2 10
f 32
f 27
159
125
120 f 13
30 min
Ih
2h
3h
115 f 8
108 f 14
149 f 24
136 f 19
115 f 13
118 f 8
110 f 10
141 f 23
145 f 13"
120 f 14
123 f 7
121 f 22
136 f 9
145 f 46
115 ? 9
121 f 7
113 f 15
121 f 18
124 ? 18
116 f 9
CBZ, carbamazepine; HR, heart rate; i.v., intravenously; P.o., orally; HPpCD, 2-hydroxypropyl-p-cyclodextrin.
Glycofurol vehicle (3.25% glycofurol in 5% aqueous glucose solution) was infused i.v. for -12-15 min; total glycofurol dose was 325 m a g body weight.
CBZ:glycofurol solution was administered in the same way, yielding a total CBZ dose of 5 mg/kg body weight. HPpCD vehicle (diluted 1:20by 5% glucose
in water) was infused i.v. for -12-15 min; HPpCD total dose was 100 m a g body weight. CBZ:HPPCD solution was administered in the same way, yielding
a total CBZ dose of 5 m a g body weight. The p.0. formulation of CBZ was administered as a bolus at a CBZ dose of 20 mg/kg body weight. Data are means
SD of 5 dogs.
a Significance of differences from predrug control: p < 0.05.
Epilepsia, Vol. 36, No. 3, 1995
W . LOSCHER ET AL.
258
Pharmacokinetics of CBZ after i.v. and
p.0. administration
After i.v. administration of the CBZ:HPPCD formulation, peak CBZ levels of 3.34.0 pg/ml (mean
3.6 pg/ml) were determined at the end of the infusion period (Fig. 1 and Table 2). Thereafter, CBZ
levels decreased rapidly, with an average half-life
(tV2) of 0.6 h (Table 2). With the CBZ:glycofurol
solution, peak CBZ levels of 3.6-6.0 pg/ml (mean
4.4 pg/ml) were determined at the end (4 dogs) or 5
min after the infusion period (Fig. 2 and Table 2).
These peak levels were significantly higher than
peak CBZ levels obtained with the CBZ:HPPCD
solution. After peak levels were attained, CBZ decreased, with an average tY2 of 1 h, significantly
less rapid as compared with the CBZ:HPPCD solution.
After p.0. administration of 20 mg/kg CBZ, peak
CBZ levels of 4.1-8.7 pg/ml (mean 6.6 pg/ml) were
determined between 30 and 60 min after application
(Fig. 3 and Table 2). The average tY2 of CBZ after
p.0. administration was 0.93 h (Table 2).
The areas under the plasma concentration:time
curves (AUCs) shown in Table 2 demonstrate that
AUCs after infusion of the CBZ:HPPCD solution
were only -50% of those calculated after infusion
of the CBZ:glycofurol solution, although both solutions were administered at the same dosage of CBZ
(5 mg/kg). The AUC determined after p.0. administration of 20 mg/kg CBZ was about four times
0.01
higher than the average AUC after administration of
5 mg/kg CBZ as CBZ:HPPCD solution, indicating
-100% bioavailability of CBZ after p.0. administration of the liquid formulation.
Levels of CBZ-10,ll-epoxide (CBZ-E), the major
metabolite of CBZ, reached peak values of 1.7-2.6
pg/ml (mean 2.0) 0.5-2 h after discontinuation of
infusion of the CBZ:HPPCD solution (Fig. 1 and
Table 2). In the experiments using i.v. infusion of
the glycofurol-based CBZ solution, peak levels of
CBZ-E were significantly lower (mean 1.4 pg/ml,
range 1.2-1.6 pg/ml) and were reached not before
3-4 h after administration, indicating that glycofurol
markedly inhibited metabolism of CBZ (Fig. 2 and
Table 2), as was also indicated by the AUCs of the
metabolite, which were significantly smaller after
infusion of CBZ:glycofurol solution as compared
with the CBZ:HPPCD solution (Table 2). After oral
administration, peak metabolite levels of 5.5-7.3
pg/ml (mean 6.5 pg/ml) were determined after 2 4 h
(Fig. 3 and Table 2).
DISCUSSION
Our results demonstrate that development of an
aqueous parenteral formulation of CBZ through use
of a modified cyclodextrin resulted in a well-tolerated injectable CBZ solution. The CBZ:HPPCD solution used is stable for >1 year and can be easily
diluted with aqueous glucose, saline, or other infusion media before being administered i.v. HPPCD is
an amorphous mixture of modified P-cyclodextrins
with an aqueous solubility far greater than that of
the parent P-cyclodextrins (Brewster et al., 1990).
Studies in rats and monkeys have shown that this
novel solvent is well tolerated after i.v. administration (Brewster et al., 1990), as was substantiated by
the present experiments in dogs. The high aqueous
solubility of HPpCD results in vastly improved solubility of numerous compounds, including CBZ
(Brewster et al., 1990, 1991).
Because CBZ is nonionized at pH 7.4 and is
highly lipid soluble, the drug rapidly penetrates
the CNS at a rate similar to that of phenytoin
(PHT) (Loscher and Frey, 1984). The present
CBZ:HPPCD solution thus should be ideally suited
for parenteral administration to control severe epileptic attacks or SE. Although peak plasma levels
achieved with i.v. infusion of the CBZ:HPPCD solution were relatively low, i.e., near the lower limit
for effectiveness against GTC (Hvidberg, 1985),
dogs eliminate CBZ much more rapidly than humans (Frey and Loscher, 1980) (present study).
Therefore, peak levels obtained with the same dosage in patients would be considerably higher, as is
1
I.?
7
0
I0
time (h)
FIG. 1. Plasma concentrations of CBZ and its major metabolite, CBZ-l0,l 1-epoxide (CBZ-E), after intravenous (i.v.) administration of a CBZ:2-hydroxypropyl-p-cyclodextrin
(HPPCD) solution in dogs. CBZ was solubilized for i.v. use
through complexing with a p-cyclodextrin (HPPCD).
CBZHPpCD solution was diluted 1:20 with 5% glucose in
water before administration. This solution of CBZ was infused for -12-15 min with an infusion rate of 10 ml/min (corresponding to a CBZ dose of 5 mg/min) until a total CBZ dose
of 5 mg/kg body weight was reached. Data are means f SD
of 5 dogs. CBZ levels (solid circles); CBZ-E levels (open circles).
Epilepsia, Vol. 36, No. 3, 1995
PARENTERAL FORMULATIONS FOR CBZ
259
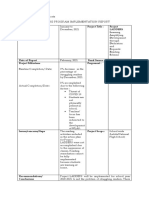
TABLE 2. Pharmacokinetic parameters of CBZ obtained after i.v. and p . 0 . administration
CBZ:HPpCD
CBZ:glycofurol
Parameters
CBZ
CBZ-E
Dose (mg/kg)
C,
(Kg/ml plasma)
L a x (h)
k, 0 - 9
hi, (h)
AUC (pg/ml . h)
5 i.v.
3.59 f 0.13
0.25
1.18 f 0.89
0.603 & 0.043
3.70 2 0.27
2.01 2 0.15
1.35 f 0.24
9.23
0.44
CBZ
5 i.v.
4.42 f 0.45"
0.27 f 0.02
0.691 f 0.0091"
1.0 2 0.014"
7.37 f 0.72"
CBZ p.0. formulation
CBZ-E
CBZ
20 p.0.
6.63 f 0.87
0.80 f 0.12
0.756 f 0.055
0.934 & 0.06
15.47 2 2.41
1.38 2 0.10*
3.85 & 0.24*
7.46 f 0.44"
CBZ-E
6.48
3.60
f 0.33
& 0.40
41.87 2 2.89
CBZ-E, CBZ-l0,ll-epoxide; AUC, area under the curve; other abbreviations as in Table 1 .
Data are means 2 SEM of 5 dogs; absence of SE indicates that all five values were identical. For AUC for CBZ, data were calculated
from zero to infinity; for CBZ-E data, AUC was calculated for observed plasma levels only. Absorption rate constant (kd for p.0. CBZ
was 1.922 f 0.35 h-', t,,, is the elimination half-life of CBZ in plasma.
a Significance of differences between the two i.v. formulations: p < 0.01.
also suggested by the data on p.0. administration in
dogs, since peak levels obtained with a liquid formulation of CBZ 20 mg/kg in dogs were comparable
to peak levels determined after oral administration
of a solution of CBZ 6 mg/kg in healthy volunteers
(Levy et al., 1976). After single-dose administration
to humans, the t% of CBZ is 20-65 h (Perucca and
Richens, 1985), whereas t% in dogs was -1 h after
p.0. administration and even lower after i.v. infusion of CBZ:HPPCD solution, which would explain
the relatively low peak plasma levels obtained with
i.v. or p.0. administration in this species. Short t%
similar to those in dogs have been determined in
various other species, including rats, gerbils, rabbits, rhesus monkeys, and baboons (Schmutz,
1985). In all species yet studied, including humans,
CBZ is almost entirely eliminated by hepatic metabolism; therefore, the large difference in elimina-
o.l
tion rate between other animal species and humans
is entirely due to differences in the overall rate of
biotransformation (Schmutz, 1985). Indeed, the
metabolic clearance of CBZ in animal species is
more than one power of 10 higher than that in humans. As demonstrated by our present data, the
major metabolite of CBZ, CBZ-10,ll-epoxide
(CBZ-E), is rapidly formed after i.v. administration
of CBZ in dogs, and AUCs of CBZ-E exceed those
of the parent drug. In contrast, in humans CBZ-E
levels in plasma are only -1&20% of that of CBZ
(Hvidberg, 1985). Based on these marked differences in metabolic rates, one may assume that i.v.
administration of CBZ:HPPCD solutions in patients
would yield about four times higher peak plasma
CBZ levels than in dogs.
For comparison with the CBZ:HPPCD solution,
a glycofurol solution of CBZ was used. Experimental data in cats indicated that solutions of CBZ in
glycofurol may be acceptable for human use
(Tauboll et al., 1990). However, the glycofurol CBZ
0.01I
10
time (k)
FIG. 2. Plasma concentrations of CBZ and its major metabolite, CBZ-l0,ll-epoxide (CBZ-E), after intravenous (i.v.) administration of a CBZ:glycofurol solution in dogs. CBZ was
solubilized for i.v. use in glycofurol and diluted 1 :20 with 5%
glucose in water before administration. This solution of CBZ
was infused for -12-15 min with an infusion rate of 10 ml/
min (corresponding to a CBZ dose of 5 mg/min) until a total
CBZ dose of 5 mg/kg body weight was reached. Data are
means +- SD of 5 dogs. CBZ levels (solid circles); CBZ-E
levels (open circles).
0.01
10
time (k)
FIG. 3. Plasma concentrations of CBZ and its major metabolite, CBZ-l0,l 1 -epoxide (CBZ-E), after oral administration of
a liquid formulation of CBZ in dogs. CBZ was administered
as a bolus at a dose of 20 mg/kg by gastric intubation. Data
are means f SD of 5 dogs. CBZ levels (solid circles); CBZ-E
levels (open circles).
Epilepsia, Vol. 36, No. 3, 1995
260
W . LOSCHER ET AL.
formulation used by Tauboll et al. could not be diluted with water, necessitating i.v. injection of undiluted glycofurol, which may cause strong local
tissue irritations. The CBZ glycofurol solution developed for the present studies is stable for >1 year
and allows dilution with aqueous media before its
injection. However, in contrast to the CBZ:HPPCD
solution, the glycofurol-based solution of CBZ was
poorly tolerated in dogs. Thus, marked cardiovascular and behavioral adverse effects were observed
after both placebo and CBZ-containing glycofurol
solutions in this species. Furthermore, glycofurol
appeared to inhibit CBZ metabolism, substantiating
and extending previous experimental data on glycofurol in rats; in those experiments glycofurol decreased elimination of hexobarbital and zoxazolamine by inhibiting hepatic microsomal metabolism,
resulting in increased drug plasma and brain concentrations (Yasaka et al., 1978). Although glycofurol is generally considered to have low toxicity
(Spiegelberg et al., 1956; Budden et al., 1979), it
increased central drug effects, including anticonvulsant and neurotoxic effects, in rodents (Crankshaw
and Raper, 1971; Yasaka et al., 1978; Loscher et al.,
1990~).By direct comparison with drug solutions in
other vehicles, the effects of glycofurol were shown
to be due not only to inhibitory effects on drug metabolism but also to pharmacodynamic effects of
glycofurol (Loscher et al., 1990a), as was also demonstrated by our present experiments, in which glycofurol doses below those previously reported to be
inert in mice (Budden et al., 1979) produced marked
cardiovascular and behavioral adverse effects in
dogs. Furthermore, glycofurol appeared to potentiate pharmacodynamic effects of CBZ, since decreased locomotor activity was observed in dogs
after infusion of the CBZ:glycofurol solution but
not after administration of the CBZ:HPPCD solution. At lower doses than those used in the present
study, glycofurol is well tolerated in dogs; e.g., we
previously used glycofurol to dissolve waterinsoluble P-carbolines and noted no vehicleassociated adverse effects after i.v. injection in
dogs at glycofurol doses ~ 2 0 0mg/kg body weight
(Loscher et al., 1990b). Formulations containing
glycofurol are used clinically as vehicles for parenteral preparations of drugs such as diazepam (DZP)
and PHT. However, our results indicate that at the
glycofurol concentrations necessary for preparation
of stable CBZ solutions that can be diluted with
aqueous media before use this vehicle is clearly inferior to inert cyclodextrins such as HPPCD.
Using a solution of CBZ in glycofurol, Tauboll et
al. (1990) recently reported that i.v. administration
of CBZ, 5-20 mg/kg, in undiluted glycofurol led to
Epilepsia, Vol. 36, No. 3 , 1995
immediate anticonvulsant effects in cats. Because
the animals were paralyzed, behavioral adverse effects could not be recorded, but the glycofurol solution did not alter mean arterial blood pressure
(Tauboll et al., 1990). Using a CBZ:HPPCD formulation for i.v. administration, Yan et al. (1990) reported that CBZ produced rapid (Le., 6 2 min) anticonvulsant effects in genetically seizure-susceptible rats. In the maximal electroshock seizure
(MES) test in rats, antiseizure effects were manifested as rapidly as 20 s after i.v. administration of
a CBZ:HPPCD solution, substantiating rapid in
vivo complex dissociation and near-instantaneous
bioavailability of the sequestered drug (Brewster et
al., 1991). The anticonvulsant ED5, of CBZ in the
MES test was 2.3 mg/kg i.v. (Brewster et al., 1991),
demonstrating that i.v. administration allowed
lower dosing as compared with other methods of
CBZ administration in this model (Loscher et al.,
1991). Experiments are in progress to compare the
time course of anticonvulsant activity of i.v.administered CBZ:HPPCD solutions with standard
drugs for i.v. treatment of SE in a mouse model of
repetitive seizures (Honack and Loscher, 1992).
Currently, DZP, PHT, or barbiturates are most
commonly used for i.v. administration to control
SE. In comparison to these drugs, CBZ has the advantage of being almost free of respiratory or cardiovascular adverse effects (Schmutz, 1985)
(present data).
Our data substantiate that preparation of aqueous
injectable formulations of CBZ through complexing
with the modified cyclodextrin HPpCD is a useful
way to obtain an aqueous solution of CBZ for i.v.
use that is well tolerated, at least in large experimental animals such as dogs. Until recently, the
low water solubility of CBZ was considered an absolute contraindication to parenteral administration. However, our present results with aqueous
CBZ:HPPCD solutions are encouraging and suggest
that pilot human studies should be undertaken. In
addition to parenteral use, CBZ:HPPCD solutions
might also be usable for p.0. administration, since
p.0. bioavailability of CBZ is markedly improved
by inclusion in HPPCD (Choudhury and Nelson,
1992).
Acknowledgment: We thank K. Naumann for excellent
technical assistance.
REFERENCES
Brewster ME, Estes K, Bodor N. An intravenous toxicity study
of 2-hydroxypropyl-~-cyclodextrin,a useful drug solubilizer,
in rats and monkeys. Int J Pharm 1990;59:231-4.
Brewster ME, Anderson WR, Estes KS, Bodor N. Development
PARENTERAL FORMULATIONS FOR CBZ
of aqueous parenteral formulations for carbamazepine
through the use of modified cyclodextrins. J Pharm Sci 1991;
80:380-3.
Budden R, Kiihl UG, Bahlsen J. Experiments on the toxic, sedative and muscle relaxant potency of various drug solvents in
mice. Pharmacol Ther 1979;5:467-74.
Chelberg RD, Gunawan S, Treiman DM. Simultaneous highperformance liquid chromatographic determination of carbamazepine and its principle metabolites in human plasma
and urine. Ther Drug Monit 1988;10:188-93.
Choudhury S , Nelson KF. Improvement of oral bioavailability of
carbamazepine by inclusion in 2-hydroxypropyl-Pcyclodextrin. Znt J Pharm 1992;85:175-80.
Crankshaw DP, Raper C. The effect of solvents on the potency
of chlordiazepoxide, diazepam, medazepam and nitrazepam.
J Pharm Pharmacol 1971;23:313-21.
Farghali-Hassan, Assael BM, Bossi L, et al. Carbamazepine
pharmacokinetics in young, adult and pregnant rats. Relation
to pharmacological effects. Arch Znt Pharmacodyn 1976;220:
125-39.
Frey H-H, Loscher W. Pharmacokinetics of carbamazepine in
the dog. Arch Znt Pharmacodyn 1980;243:180-91.
Fromm GH. Antiepileptic actions of carbamazepine. In: Faingold CL, Fromm GH, eds. Drugs for control of epilepsy.
Actions on neuronal networks involved in seizure disorders.
Boca Raton: CRC Press, 1992:425-36.
Honack D, Loscher W. Intravenous valproate: onset and duration of anticonvulsant activity against a series of electroconvulsions in comparison with diazepam and phenytoin. Epilepsy Res 1992;13:215-21.
Hvidberg EF. Monitoring antiepileptic drug levels. In: Frey
H-H, Janz D, eds. Antiepileptic drugs. Handbook of experimental pharmacology, vol. 74. Berlin: Springer, 1985:72544.
Levy RH, Lockard JS, Green JR, Friel P, Martis L. Pharmacokinetics of carbamazepine in monkeys following intravenous
and oral administration. J Pharm Sci 1975;64:302-7.
Levy RH, Pitlick WH, Troupin AS, Green JR, Neal JM. Pharmacokinetics of carbamazepine in normal man. Clin Pharmacol Ther 1976;17:657-68.
Lockard JS, Levy RH, DuCharme LL, Congdon WC, Patel IH.
Carbamazepine revisited in a monkey model. Epilepsia 1979;
20:169-73.
Loscher W, Frey H-H. Kinetics of penetration of common antiepileptic drugs into cerebrospinal fluid. Epilepsia 1984;25:
346-52.
Loscher W, Honack D. Anticonvulsant and behavioural effects
of two novel competitive N-methyl-D-aspartic acid receptor
antagonists, CGP 37849 and CGP 39551, in the kindling model
261
of epilepsy. Comparison with MK-801 and carbamazepine. J
Pharmacol Exp Ther 1991;256:432-40.
Loscher W, Nolting B, Fassbender CP. The role of technical,
biological and pharmacological factors in the laboratory evaluation of anticonvulsant drugs. I. The influence of administration vehicles. Epilepsy Res 1990a;7:173-81.
Loscher W, Honack D, Scherkl R, Hashem A, Frey H-H. Pharmacokinetics, anticonvulsant efficacy and adverse effects of
the P-carboline abecarnil, a novel ligand for benzodiazepine
receptors, after acute and chronic administration in dogs. J
Pharmacol Exp Ther 19906;255:541-8.
Loscher W, Fassbender CP, Nolting B. The role of technical,
biological and pharmacological factors in the laboratory evaluation of anticonvulsant drugs. 11. Maximal electroshock seizure models. Epilepsy Res 1991;8:79-94.
Patel IH, Levy RH. Intramuscular absorption of carbamazepine
in rhesus monkeys. Epilepsia 1980;21:103-9.
Perucca E, Richens A. Clinical pharmacokinetics of antiepileptic
drugs. In: Frey H-H, Janz D, eds. Antiepileptic drugs. Handbook of experimental pharmacology, vol. 74. Berlin:
Springer, 1985:661-24.
Pitha J, Irie T, Sklar P, Nye J. Drug solubilizers to aid pharmacologists: amorphous cyclodextrin derivatives. Life Sci 1988;
43:493-5.
Ronfeld RA, Benet LZ. Dose dependent kinetics of carbamazepine in the monkey. Res Commun Chem Pathol PharmaC O ~
1975;10:303-14.
Schmutz M. Carbamazepine. In: Frey H-H, Janz D, eds. Antiepileptic drugs. Handbook of experimental pharmacology,
vol. 74. Berlin: Springer, 1985:479-506.
Spiegelberg H, Schlapfer R, Zbinden G , Studer A. Ein neues
injizierbares Losungsmittel (Glycofurol). Arzneimittel Forschung Drug Res 1956;6:75-7.
Tallarida RJ, Murray RB. Manual of Pharmacologic Calculations with Computer Programs, 2nd ed. Berlin: Springer,
1987.
Tauboll E, Lindstrom S, Klem W, Gjerstad L. A new injectable
carbamazepine solution-antiepileptic effects and pharmaceutical properties. Epilepsy Res 1990;7:5944.
Yan 0-S, Jobe PC, Dailey JW. Parenteral carbamazepine: effect
on convulsions and on dialyzable hippocampal serotonin (5HT) in genetically epilepsy-prone rats (GEPRs). SOCNeurosci Abstr 1990;16:784.
Yasaka WJ, Sasame HA, Saul W, Maling HM, Gillette JR.
Mechanisms in the potentiation and inhibition of pharmacological actions of hexobarbital and zoxazolamine by glycofurol. Biochem Pharmacol 1978;27:2851-8.
Epilepsia, Vol. 36, No. 3, 1995
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Beatriz Colomina X Ray Architecture Lars Muller (001 045)Document45 pagesBeatriz Colomina X Ray Architecture Lars Muller (001 045)SABUESO FINANCIERONo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Inclusive Teaching Reflection PaperDocument2 pagesInclusive Teaching Reflection Paperapi-35177809179% (19)
- DLL Catch Up Friday Week 4Document16 pagesDLL Catch Up Friday Week 4Maryanne Labaso93% (27)
- Mock LET QuestionDocument24 pagesMock LET Questionarlenegomito100% (18)
- Earning Than Non-GraduatedDocument2 pagesEarning Than Non-GraduatedFranco CentNo ratings yet
- User Manual PDFDocument8 pagesUser Manual PDFcooljay2708No ratings yet
- Raoult's Law & Henry's Law: Unit: Mass. Frameworks Section(s) : Knowledge/UnderstandingDocument7 pagesRaoult's Law & Henry's Law: Unit: Mass. Frameworks Section(s) : Knowledge/UnderstandingFranco CentNo ratings yet
- Novel Method For Preparation of B-Cyclodextrin/grafted Chitosan and It's ApplicationDocument8 pagesNovel Method For Preparation of B-Cyclodextrin/grafted Chitosan and It's ApplicationFranco CentNo ratings yet
- Pte Accepted UniversitiesDocument28 pagesPte Accepted UniversitiesRaj KumarNo ratings yet
- AsdsadDocument1 pageAsdsadFranco CentNo ratings yet
- 01 Prepositions PDFDocument2 pages01 Prepositions PDFFranco CentNo ratings yet
- C Make ListsDocument17 pagesC Make ListsFranco CentNo ratings yet
- C Make ListsDocument2 pagesC Make ListsFranco CentNo ratings yet
- CMake ListsDocument1 pageCMake ListsFranco CentNo ratings yet
- Journal of Chromatography A: Guillaume Chalumot, Cong Yao, Verónica PinoDocument7 pagesJournal of Chromatography A: Guillaume Chalumot, Cong Yao, Verónica PinoFranco CentNo ratings yet
- Information For AuthorsDocument24 pagesInformation For AuthorsFranco CentNo ratings yet
- C Make ListsDocument17 pagesC Make ListsFranco CentNo ratings yet
- Optical Properties 2Document26 pagesOptical Properties 2Franco CentNo ratings yet
- 11 Reading Fill Blanks PTEA Strategies PDFDocument6 pages11 Reading Fill Blanks PTEA Strategies PDFJen ConstanteNo ratings yet
- Tutorial Postproc PDFDocument30 pagesTutorial Postproc PDFarnoldNo ratings yet
- Pte Accepted UniversitiesDocument28 pagesPte Accepted UniversitiesRaj KumarNo ratings yet
- Raoult's Law & Henry's Law: Unit: Mass. Frameworks Section(s) : Knowledge/UnderstandingDocument7 pagesRaoult's Law & Henry's Law: Unit: Mass. Frameworks Section(s) : Knowledge/UnderstandingFranco CentNo ratings yet
- PW TutorialDocument65 pagesPW TutorialGilberto LlorenteNo ratings yet
- NaCl Halite - CifDocument5 pagesNaCl Halite - CifPhương ĐôngNo ratings yet
- Highly Water-Soluble Prodrugs of Anthelmintic Benzimidazole Carbamates: Synthesis, Pharmacodynamics, and PharmacokineticsDocument4 pagesHighly Water-Soluble Prodrugs of Anthelmintic Benzimidazole Carbamates: Synthesis, Pharmacodynamics, and PharmacokineticsFranco CentNo ratings yet
- 01 Grammar PDFDocument8 pages01 Grammar PDFFranco CentNo ratings yet
- MM Notes 10Document12 pagesMM Notes 10Franco CentNo ratings yet
- NaCl Halite - CifDocument5 pagesNaCl Halite - CifPhương ĐôngNo ratings yet
- Adam and Rob: Elementary Podcast Transcript - Series 3 Episode 15Document4 pagesAdam and Rob: Elementary Podcast Transcript - Series 3 Episode 15duyhoangfuongNo ratings yet
- Van Hoorn e 2016Document42 pagesVan Hoorn e 2016Franco CentNo ratings yet
- Liquid Vapor e QuilDocument12 pagesLiquid Vapor e QuilFrancisco MartinezNo ratings yet
- Glab 1Document11 pagesGlab 1Franco CentNo ratings yet
- Pulse Diagnosis - CONCISE WORKBOOKDocument21 pagesPulse Diagnosis - CONCISE WORKBOOKVishnu Prabhu SivasubramaniamNo ratings yet
- Epidemiology and Pathogenesis of Benign Prostatic Hyperplasia - UpToDateDocument9 pagesEpidemiology and Pathogenesis of Benign Prostatic Hyperplasia - UpToDateFeer VillarrealNo ratings yet
- Case Study On Pemphigus Vulgaris (PharmD)Document18 pagesCase Study On Pemphigus Vulgaris (PharmD)kezia15rebeccaNo ratings yet
- Activity 2 - Quiñones Mary Angela Felicia T - CPE 1 - Nov 3 - Prof Andy GutierrezDocument7 pagesActivity 2 - Quiñones Mary Angela Felicia T - CPE 1 - Nov 3 - Prof Andy GutierrezMary Angela Felicia QuiñonesNo ratings yet
- Glow Worm 30-40-50f Boiler InstructionsDocument40 pagesGlow Worm 30-40-50f Boiler InstructionsBandit195850% (2)
- 13 KayachikitsaDocument2 pages13 KayachikitsaShreeNo ratings yet
- Welding Visual ReportDocument6 pagesWelding Visual ReportFerdie OSNo ratings yet
- GUIDELINES FOR INPATIENT DIABETES MANAGEMENT هااامDocument1 pageGUIDELINES FOR INPATIENT DIABETES MANAGEMENT هااامAbu HuzaifaNo ratings yet
- Mosquito Borne DiseasesDocument24 pagesMosquito Borne DiseasesSidney BowenNo ratings yet
- 266-Article Text-1446-1-10-20210421Document14 pages266-Article Text-1446-1-10-20210421syeda hajraNo ratings yet
- Company ProfileDocument102 pagesCompany ProfileOsama HammamNo ratings yet
- Faktor - Faktor Risiko Terjadinya Infertilitas Pada Wanita Pasangan Usia Subur Di Dusun V Desa Kolam Kecamatan Percut Sei Tuan Tahun 2020Document6 pagesFaktor - Faktor Risiko Terjadinya Infertilitas Pada Wanita Pasangan Usia Subur Di Dusun V Desa Kolam Kecamatan Percut Sei Tuan Tahun 2020Anastasia AbrahamNo ratings yet
- SRS Bulletin 2020 Vol 55 No 1Document9 pagesSRS Bulletin 2020 Vol 55 No 1Prasanna ShanNo ratings yet
- Reading Program Terminal Report-2020Document2 pagesReading Program Terminal Report-2020roselyn galinatoNo ratings yet
- Argumentative Essay About EuthanasiaDocument8 pagesArgumentative Essay About Euthanasiappggihnbf100% (2)
- De Thi Hoc Ki 1 Lop 9 Mon Tieng Anh Thi Diem Phong GD DT Hoa An Cao Bang Co Dap AnDocument16 pagesDe Thi Hoc Ki 1 Lop 9 Mon Tieng Anh Thi Diem Phong GD DT Hoa An Cao Bang Co Dap AnViệt KhôiNo ratings yet
- Secondary - Report Card Comment CodesDocument2 pagesSecondary - Report Card Comment CodesRICHARD SARDON LEONNo ratings yet
- Physiotherapy Management For Patient With Primary Spontaneous Pneumothorax Dextra: A Case StudyDocument5 pagesPhysiotherapy Management For Patient With Primary Spontaneous Pneumothorax Dextra: A Case Studyjavier garzonNo ratings yet
- PDF DocumentDocument1 pagePDF DocumentEuna DawkinsNo ratings yet
- A Systematic Review of The Effects of Residency Training On Patients OutcomesDocument11 pagesA Systematic Review of The Effects of Residency Training On Patients OutcomesMaik MouraNo ratings yet
- Principles of Fitness Training and 3-Week Exercise Training ProgramDocument10 pagesPrinciples of Fitness Training and 3-Week Exercise Training ProgramSunny EggheadNo ratings yet
- Chapter - Ii Inclusive Education-Philosophy, Principles, Policy and ProgrammesDocument22 pagesChapter - Ii Inclusive Education-Philosophy, Principles, Policy and ProgrammesAngelica AlejandroNo ratings yet
- Pharmacology Connections To Nursing Practice 3rd Edition Adams Solutions ManualDocument26 pagesPharmacology Connections To Nursing Practice 3rd Edition Adams Solutions ManualToniPerryptfo100% (36)
- Reliability in Medical Device IndustryDocument14 pagesReliability in Medical Device IndustrySubramani KarurNo ratings yet
- Catch Up Friday DLL March 1Document4 pagesCatch Up Friday DLL March 1Raymart MagsumbolNo ratings yet
- Position Paper. TEAM 14Document3 pagesPosition Paper. TEAM 14Carmina BesarioNo ratings yet