Professional Documents
Culture Documents
Clinical Survey On Malaria A Study in Anantapuramu District of Andhra Pradesh
Uploaded by
IOSRjournalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Survey On Malaria A Study in Anantapuramu District of Andhra Pradesh
Uploaded by
IOSRjournalCopyright:
Available Formats
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 4 Ver. VIII (Apr. 2015), PP 15-18
www.iosrjournals.org
Clinical Survey on Malaria a Study in Anantapuramu District Of
Andhra Pradesh
Dr.Veerabhadraiah M.D1, Dr.V.Sreenivas M.D2,
1,2,
Associate Professor, Govt Medical college, Anantapuramu
Abstract: Malaria is a public health problem in several parts of the country. About 95% population in the
country resides in Malaria endemic areas and 80% of malaria reported in the country is confined to areas
consisting 20% of population residing in tribal, hilly, difficult and inaccessible areas. India contributes about
70% of malaria in South East region of W.H.O. Although annually India reports about 2 million cases and 1000
deaths attributable to malaria, there is increasing trend in the proportion of Plasmodium Falciparum as the
agent. This study aimed to note the presentations and complications of Plasmodium Falciparum in Government
General Hospital, ,Anantapuramu district of Andhra Pradesh.
Methodology: The descriptive study was conducted at IPD (inpatient department) of Government General
Hospital Anantapuramu. In this study simple random technique was used for selection of sample. All adult
patients with positive malaria peripheral film admitted through the department was studied during 2014.Data
was entered and analyzed.
Results: A total of 97 patients were included in this study. Fever was the most common presentation. A
significant number of patients had non- specific complaints but tachycardia, altered mental status and adult
respiratory distress syndrome was important findings. Common reasons for admission were thrombocytopenia
and dehydration. Some patients were admitted for more than 48 hours. Complications included Pneumonia and
bleeding requiring platelet transfusion.
I.
Introduction
Malaria and six other diseases viz: Diarrhoea,HIV/AIDS,Tuberculosis,Measles,Hepatitis.B and
Pneumonia account for 85% of global infectious disease burden (Murray & Lopez 1996,1997).Malaria afflicts
36% of the world population i.e 2020 million in 107 countries and territories situated in the tropical and sub
topical regions. In the South east Asian region of W.H.O,out of about 1.4 billion people living in 11
countries,1.2 billion (85.7%)are exposed to the risk of Malaria and most of whom live in India. Plasmodium
Vivax malaria is a public health problem that puts billions of the worlds population at risk of infection as
highlighted in the world Malaria report2010.Despite Malaria control strategies, an estimated 100.300 million
cases are reported each year (1,2).
The global Malaria eradication programme of W.H.O launched in the 1950s was a huge success in
India as the incidence declined from estimated 75 million cases and 8 lakhs deaths in 1947 to just 49151 cases
(annual parasite incidence per 1000(API), 0.13; Slide positivity rate (SPR).0.38 percent and Plasmodium
falciparum (PF); 34.9 percent) no deaths in 1961 and Malaria was thought to be on the average of eradication. It
was then ,that a series of setbacks were witnessed leading to Malarial resurgence in multiple foci in the country
and reported cases increased to 13,22,398 by 1971(API:2.4,SPR:3.27% and PF:11.2%)and then to 64.67,215 in
1976(API:11.25:SPR;11.6 and PF;11.2%)(http;//www.searo.who.in//).The failure was attributed to the
complacency, administrative, operational and technical problems like resistance in vectors to commonly used
insecticide DDT and in parasites to chloroquine and overall low priority malarial enjoyed in the post control
period. Thereafter with the implementation of modified plan of operation (mpo) in 1997, Malaria cases declined
and ranged between 2-3 million per annum in the subsequent years. However in 1996, due to outbreaks and
epidemics 3035588 cases and 2803 deaths reported. In 2006,the reported number of cases was
16,69,333(API;1.57:SPR;1.635 and PF;45.3%).But country has witnessed different phases of malaria situations
in the country and from high prevalence of malaria to near eradication to resurgence in post DDT era to the use
of arteminisinin combination therapies(ACTS).
The current incidence of Malaria reported by National vector borne disease control programme,i.e the
case load though the steady around 2 million cases annually in the late 90s,as shown a declining trend since
2002.When interpreting API, it is important to evaluate the level of surveillance activity indicated by the annual
blood examination rate. At low levels of surveillance, the slide positive rate (spr) may be a better indicator. The
SPF has also shown gradual decline from 3.90 in 1995 to 0.98 in 2001.The report PF cases from 1.14 million in
1995 to 0.53 million cases in 2012.However, the PF percentage has gradually increased from 39 percent in 1995
to 50.05 percent in 2012.
DOI: 10.9790/0853-14481518
www.iosrjournals.org
15 | Page
Clinical Survey On Malaria A Study In Anantapuramu District Of Andhra Pradesh
The rapid progression of a febrile illness in to a systematic infection requires advances care with the
need of aggressive resuscitation and in hospital care. Frequent observation of Malaria patients presenting to out
patients department led us to conduct this study to note the presentations and complications and subsequent to
identify the determinants of hospital care of Malaria patients presenting to a tertiary care hospital in
Anantapuramu, Andhra Pradesh.
II.
Methodology
The descriptive study was conducted in IPD (In patient department) of Government General
Hospital,Anantapuramu ,Andhra Pradesh.Our department has annual patient turnover of 35,000 with 5-10 % of
admission rate. All adult patients with a positive plasmodium falciparum and plasmodium vivax peripheral film
were enrolled. Patients who were managed as out -patients were not included in the study. The size of the
sample is 97 and the simple random technique was used for selection of sample in the study.
A Data collection tool was designed with variables including the patients demographic details as well
as clinical presentation. Presenting complaints co-morbities, hemodynamic parameters at arrical, and physical
examination findings were noted. Laboratory test including hemoglobin, hamatocrit platelet count total
leukocyte count and serum creatinine were checked for malarial parasite and impact was also recorded. Further
inpatient complaints, length of the stay and outcome of the patients were noted as well as specific reasons for
admissions, clinical Varity of diseases were noted.
Data was extracted from patients files by the research team and double checked for accuracy before
analyses. Data was entered and analyzed using a SPSS version16.Frequencies and percentages of categorical
data were calculated. Keeping the length of stay and a cutoff of 2-5 days after admission. Level of significance
was taken at 95 percent CI with alpha of 0.05.
III.
Results
A total 97 patients were included in the study. Fever was the most common presentation involving 93
(97%) patients. Time duration of fever varied with a median span of 5days before presentation. A significant
number of patients more specific complaint along with fever including headache, poor oral intake, generalized
weakness but 50 percent of clients complaining of abdominal pain. These symptoms included nausea, vomiting,
and abdominal pain. About 12 percent of clients had shortness of breath and cough. Out of 97 patients seven
patients had neurological symptoms including confusion, disorientation and drowsiness were present. Decreased
urinary output was the main complaint in two patients.
Mean temperature on arrival was 38 1 degree centigrade. Although mean systolic blood pressure
(sbp) was normal (114 21mmhg), initial evaluation in the inpatient department demonstrated that most of the
patients were tachycardia (mean pulse rate 110 22 beats per minute).Also, 28(27%) patients had SBP of less
than 100 mmhg at the time of arrival, requiring aggressive fluid replacement. This hemodynamic compromise
leading to shock is better reflected through the shock index (SI).The mean value of SI was 1 (SD=0.26); Median
SI was 0.9 9iqr0.5).Minimal value calculated was 0.5 and the maximum was 1.6.Hepatomegaly was noted in
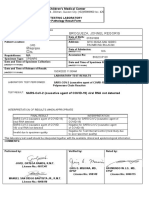
two patients.fig 1 describes the common abnormal physical findings with dehydration, abdominal tenderness
and jaundice the most frequently observed signs.
Table1. Demographic presenting symptoms co-morbities of study participant
DOI: 10.9790/0853-14481518
www.iosrjournals.org
16 | Page
Clinical Survey On Malaria A Study In Anantapuramu District Of Andhra Pradesh
Table2.Comparison of the factors affecting participants length of stay in hospital
Factors
Age
Days of fever
Systolic BP**
Diastolic BP
Heart Rate
Temperature
Oxygen Saturation
Hemoglobin
Hematocrit
Leucocytes
Platelets
Serum Creatinine
Up to 48 hours
Mean (SD)
30.5(16.2)
3.2(2)
100(15.3)
65.1(12.3)
111.3(22.8)
38.2(1.0)
96.8(1.3)
11.6(1.2)
37.1(5.1)
6.5(3.0)
68.6(52.1)
1.1(0.4)
More than 48 hours
p-value
46.3(21.8)
8.1(2.2)
117.5(22.0)
68.9(12.4)
106.2(19.7)
38.2(1.1)
97.2(2.4)
13.3(3.9)
37.0(6.0)
106(14.6)
59.5(39.0)
1.7(2.7)
0.21
0.10
0.10
0.69
0.30
0.99
0.22
0.22
0.89
0.16
0.35
0.26
More than 56 patients (58%) were treated with chloroquine and 37(38%) with artemether, another 17
(18%) received antibiotics at the time of presentation, which were discontinued after establishment of diagnosis.
In one patient antimalarial treatment was not documented. While only one patient required packed red blood
cells transfusion, five patients received multiple platelet transfusion due to persistently low platelets and
bleeding complications. The majority of the patients (67%) required initial intravenous fluid resuscitation, which
was continued as in-patient in 43(44%) patients due to dehydration and/or persistent vomiting.
Reasons for admission were mentioned for 84 patients out of whom 45(53%) had low platelets with or
without 42(50%) bleeding complications,13(15%) presented with signs and symptoms of septic shock requiring
continuous monitoring;4(5%) had electrolyte imbalance including hyponatremia,acute renal failure;2(2%) had
altered mental status at the time of presentation;2(2%) had concomitant cardiac problems; and 2(2%) had
ARDS.The remaining 20(23%) were admitted for other reasons including dehydration and vomiting/nausea with
poor oral intake. We also divided the patients according to their length of stay in two groups (table 2).However,
the analyses failed to demonstrate any statistically significant association of the clinical or laboratory features
such as age, blood pressure, Hb or Platelet levels with the duration of hospital stay.
The majority (80; 82%) of the patients were admitted in the general ward; 12(12%) were treated in the
high dependency or special care units and 2(2%) in the intensive care unit. The mean length of stay was 21
day. The majority, 67(; 70%) were managed within 48 hours of admission but 29(30%) had to be admitted for
more than 48hours.
.
Figure1. Physical examination findings of study participants.
General Physical Examination
DOI: 10.9790/0853-14481518
www.iosrjournals.org
17 | Page
Clinical Survey On Malaria A Study In Anantapuramu District Of Andhra Pradesh
IV.
Discussion
In this paper we present a cross sectional study describing the characteristics of Malaria patients who
were managed in a tertiary hospital. Despite a small number of subjects over a one-year period, we observed
that all these patients had signs and/or symptoms and laboratory parameters warranting in-patient management.
Respect to presenting complaints, high grade fever with generalized body aches and gastrointestinal
complaints were the commonest presentation. The classic description of tertian fever with, swinging temperature
was found only in a minority of patients, while many patients presented with non-specific symptoms, abdominal
pain, altered mental status, vomiting and dehydration which not only required laboratory workup but also
intravenous fluid resuscitation. Muddaiah and Prakash have reported that, among those Malaria patients who
were managed in-hospital, 47% had Vivax Malaria. Also nausea/vomiting, abdominal pain and headaches were
observed commonly in those who were managed as in-patients. Less frequently reported but important signs and
symptoms that were pertinent to the central nervous system included drowsiness and seizures and respiratory
complications including ARDS and respiratory distress.
Organ dysfunction was noted in a considerable proportion of patients who presented with signs of
systemic sepsis manifested by low blood pressure, depressed consciousness, and respiratory and renal
dysfunction. Andrade and Kaur also reported severe Plasmodium Vivax Malaria manifesting as acute renal
failure insufficiency and respiratory failure (17-18).In our data set 9% of patients had CNS related symptoms
including drowsiness and seizures. It is important to note that some researchers have identified cerebral Malaria
caused by Plasmodium Vivax, However, no specific diagnostic tests so far can confirm this diagnosis in
suspected patients (1, 8, 9).
Anemia is a common clinical feature that is caused by increased fragility and destruction of infected
non-infected RBCS (4, 5,6) which was not found in our study subjects; The Mean Hb level was 13
mg/dl.However,we found a significant number of patients at risk of bleeding complications due to low platelet
counts. Severe thrombocytopenia has been reported by other researchers (18,23,24).Altered
thrombostasis,thrombocytopenia and micro vascular thrombosis contribute to bleeding complications and micro
vascular obstructions(13).Thrombocytopenia at the time of admission was one of the major reasons for
admission in 30% of cases as well as prolonged length of stay. Regardless of the platelet levels ,only 5% of the
patients developed major bleeding complications requiring multiple blood and platelet transfusions and most of
the patients exhibited a rising platelet trend after initiation of anti malarial therapy. This finding is supported by
other investigators in Pakistan. In 2010, Rasheed et al, reported such thrombocytopenia (25), and also found that
despite low platelets, bleeding complications were rare and platelets responded well to anti-Malarial therapy.
Most of the patients were discharged within 2-5 days of admission and the discharge was guided by
improvement in symptoms coupled with hemodynamic stability in the majority of patients after confirmation of
negative parasitemia and improving platelet count. The main limitation of our study was its retrospective
descriptive design. This study was neither designed nor powered to predict the risk factors associated with
severe disease or poor prognosis. We included only those patients who were treated as in-patients in a single
tertiary care centers to identify determinants of disease severity warranting in-patient care.
V.
Conclusion
This study highlights the fact that debilitating impact o fplasmodoum falciparum, is remains high.
Water lagging areas and open drainages are the leading causes of plasmodium falciparum endemic in our area.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
[11].
Andrade BB,Reis-Filho A,Souza-Neto SM,Clarencio J,Camargo LM,Barral-Netto M (2010) Severe Plasmodium Vivax Malaria
exhibits marked inflammatory imbalance.Malar J9:13.
Anstey NM,Russll B,Yeo TW,Price RN (2009) The pathophysiology of vivax malaria.Trends parasitol 25:220-227.
Beg MA,Khan R,Baig SM,Gulzar Z,Hussain R,Smego RA,Jr (2002) Cerebral involvement in benign tertian malaria AmJ Trop Med
Hyg 67:230-232
Kaur D,Wsir V,Gulati S,Bagga A (2007) Unusual presentation of plasmodium vivax malaria with severe thrombocytopenia and
acute renal failure.J Trop Pediatr 53:210-212
Kochar DK,Das A, Kochar SK,Saxena V,Sirohi P,Garg S,Kochar A,Khatri MP,Gupta V(2009) Severe Plasmodium Vivax Malaria:
a report on serial cases from Bikaner in northwestern India.Am J Trop Med Hyg 80:194.
Makkar RP,Mukhopadhyay S,Monga A,Gupta AK(2002) Plasmodium Vivax malaria presenting with severe thrombocytopenia
Braz J Infect Dis 6:263-265.
Mendis K,Sina BJ,Marchesini P,Carter R (2001) The neglected burden of Plasmodium Vivax malaria,Am J Trop Med Hyg 64
Suppl 1-2 Suppl:97-106.
Muddaiah M and Prakash PS (2006) a Study of clinical profile of malaria in a tertiary referral centre in south Canara.J Vector Borne
Dis 43:29-33.
Ozen M,Gungor S,Atambay M,Daldal N (2006) Cerebral malaria owing to plasmodium vivax: Case report.Ann Trop Paediatr
26:141-144.
Rodriguez-Morales AJ,Sanchez E,Vargas M,Piccolo C,Colina R,Arria M( 2006) Anemia and thrombocytopenia in children with
Plasmodium Vivax Malaria J Trop Pediatr 52:49-51.
World Health Organization (2010) World Malaria report 2010.
DOI: 10.9790/0853-14481518
www.iosrjournals.org
18 | Page
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- "I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweDocument5 pages"I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweInternational Organization of Scientific Research (IOSR)No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Socio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanDocument7 pagesSocio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanInternational Organization of Scientific Research (IOSR)No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Attitude and Perceptions of University Students in Zimbabwe Towards HomosexualityDocument5 pagesAttitude and Perceptions of University Students in Zimbabwe Towards HomosexualityInternational Organization of Scientific Research (IOSR)No ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Review of Rural Local Government System in Zimbabwe From 1980 To 2014Document15 pagesA Review of Rural Local Government System in Zimbabwe From 1980 To 2014International Organization of Scientific Research (IOSR)No ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Role of Extrovert and Introvert Personality in Second Language AcquisitionDocument6 pagesThe Role of Extrovert and Introvert Personality in Second Language AcquisitionInternational Organization of Scientific Research (IOSR)No ratings yet
- Assessment of The Implementation of Federal Character in Nigeria.Document5 pagesAssessment of The Implementation of Federal Character in Nigeria.International Organization of Scientific Research (IOSR)No ratings yet
- A Proposed Framework On Working With Parents of Children With Special Needs in SingaporeDocument7 pagesA Proposed Framework On Working With Parents of Children With Special Needs in SingaporeInternational Organization of Scientific Research (IOSR)No ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Comparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesDocument7 pagesComparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesInternational Organization of Scientific Research (IOSR)No ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Investigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehDocument4 pagesInvestigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehInternational Organization of Scientific Research (IOSR)No ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Impact of Technologies On Society: A ReviewDocument5 pagesThe Impact of Technologies On Society: A ReviewInternational Organization of Scientific Research (IOSR)100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Edward Albee and His Mother Characters: An Analysis of Selected PlaysDocument5 pagesEdward Albee and His Mother Characters: An Analysis of Selected PlaysInternational Organization of Scientific Research (IOSR)No ratings yet
- An Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyDocument14 pagesAn Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyInternational Organization of Scientific Research (IOSR)No ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Designing of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesDocument5 pagesDesigning of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesIOSRjournalNo ratings yet
- Topic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshDocument7 pagesTopic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshInternational Organization of Scientific Research (IOSR)No ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Relationship Between Social Support and Self-Esteem of Adolescent GirlsDocument5 pagesRelationship Between Social Support and Self-Esteem of Adolescent GirlsInternational Organization of Scientific Research (IOSR)No ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Importance of Mass Media in Communicating Health Messages: An AnalysisDocument6 pagesImportance of Mass Media in Communicating Health Messages: An AnalysisInternational Organization of Scientific Research (IOSR)No ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Role of Madarsa Education in Empowerment of Muslims in IndiaDocument6 pagesRole of Madarsa Education in Empowerment of Muslims in IndiaInternational Organization of Scientific Research (IOSR)No ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Key To Eye Diagnosis by Tashfeen NasiraDocument8 pagesKey To Eye Diagnosis by Tashfeen Nasiralakshay sharmaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Use of Pycnogenol in The Treatment of Melasma: Original ArticlesDocument5 pagesThe Use of Pycnogenol in The Treatment of Melasma: Original ArticlesfreitasjonashenriqueNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Letter Explanation To DoctorDocument1 pageLetter Explanation To DoctorDonnaNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Îeéuwûéaéié Uréékéï: (Diseases of Tongue)Document87 pagesÎeéuwûéaéié Uréékéï: (Diseases of Tongue)Pranit Patil100% (1)
- Chapter 5neonatal Seizures and Neonatal SyndromesDocument10 pagesChapter 5neonatal Seizures and Neonatal SyndromesArista RiskaNo ratings yet
- Multi Organ Dysfunction SyndromeDocument40 pagesMulti Organ Dysfunction SyndromeDr. Jayesh PatidarNo ratings yet
- Myasthenia GravisDocument11 pagesMyasthenia GravisParvathy RNo ratings yet
- Anti InflamasiDocument27 pagesAnti InflamasiAuLia DamayantiNo ratings yet
- Trichuris TrichiuraDocument16 pagesTrichuris TrichiuraPaul Avila SorianoNo ratings yet
- Laparoscopic Course: General Principles of Laparoscopy: Specific Aspects of Transperitoneal Access (R.Bollens)Document4 pagesLaparoscopic Course: General Principles of Laparoscopy: Specific Aspects of Transperitoneal Access (R.Bollens)Anuj MisraNo ratings yet
- Uterine Leiomyomas (Fibroids) - Epidemiology, Clinical Features, Diagnosis, and Natural History - UpToDateDocument48 pagesUterine Leiomyomas (Fibroids) - Epidemiology, Clinical Features, Diagnosis, and Natural History - UpToDateRuben Orduño RizoNo ratings yet
- Errors 2Document5 pagesErrors 2Anggun rahmi PutriNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Principle:: Sample Considerations and Special ProceduresDocument97 pagesPrinciple:: Sample Considerations and Special Proceduresjustine anchetaNo ratings yet
- A Study On Level of Mental Health Problems of AdolescentDocument3 pagesA Study On Level of Mental Health Problems of AdolescentEditor IJTSRDNo ratings yet
- Test Bank For Medical Surgical Nursing 7th Edition Donna D IgnataviciusDocument24 pagesTest Bank For Medical Surgical Nursing 7th Edition Donna D Ignataviciusrobertblackmwjkpnyfrq100% (37)
- Nursing Care Plan Diabetes Mellitus Type 2Document2 pagesNursing Care Plan Diabetes Mellitus Type 2deric89% (75)
- NMSRC Sample Research PaperDocument4 pagesNMSRC Sample Research Paperjemma chayocasNo ratings yet
- 4D CT With Respiratory GatingDocument2 pages4D CT With Respiratory GatingLaura Karina Sanchez ColinNo ratings yet
- 30613167: Management of Osteitis Pubis in Athletes Rehabilitation and Return To Training - A Review of The Most Recent Literature PDFDocument10 pages30613167: Management of Osteitis Pubis in Athletes Rehabilitation and Return To Training - A Review of The Most Recent Literature PDFRicovially DavyaNo ratings yet
- Coma-Dr. AM IyagbaDocument53 pagesComa-Dr. AM IyagbaDr. Amb. Monday ZaccheausNo ratings yet
- Cholelithiasis Case 1Document21 pagesCholelithiasis Case 1Arvin F. LansangNo ratings yet
- Anesthesia Management For Pulmonary Hypertension PatientsDocument18 pagesAnesthesia Management For Pulmonary Hypertension PatientsAliNasrallahNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Conducting A Nurse Consultation: ClinicalDocument6 pagesConducting A Nurse Consultation: ClinicalAlif Akbar HasyimiNo ratings yet
- Chronic PeriodontitisDocument3 pagesChronic Periodontitisapi-537687828No ratings yet
- Broqueza, Jonnel Regoris: Philippine Children's Medical CenterDocument1 pageBroqueza, Jonnel Regoris: Philippine Children's Medical CenterRica RegorisNo ratings yet
- Med Surg (Oncology)Document169 pagesMed Surg (Oncology)DardarConstantinoNo ratings yet
- Four-Month Rifapentine Regimens With or Without Moxifloxacin For TuberculosisDocument14 pagesFour-Month Rifapentine Regimens With or Without Moxifloxacin For TuberculosisyanaNo ratings yet
- Hope 1 - FitnessDocument13 pagesHope 1 - FitnessMark Clemence R. ParcasioNo ratings yet
- Hypertency Emergency Acute PDFDocument12 pagesHypertency Emergency Acute PDFmasdika09No ratings yet
- GRP2Document87 pagesGRP2Veronica ChanNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)