Professional Documents
Culture Documents
Surface Epithelial-Stromal Tumor
Uploaded by
dger11Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Surface Epithelial-Stromal Tumor
Uploaded by
dger11Copyright:
Available Formats
Surface epithelial-stromal tumor
Surface epithelial-stromal tumor
Surface epithelial-stromal tumor
Classification and external resources
High magnification micrograph of a Brenner tumor, a type of surface epithelial-stromal tumor. H&E stain.
ICD-10
C56
ICD-9
183
[1]
, D27
[3]
, 220
[2]
[4]
Surface epithelial-stromal tumors are a class of ovarian neoplasms that may be benign or malignant. Neoplasms in
this group are thought to be derived from the ovarian surface epithelium (modified peritoneum) or from ectopic
endometrial or Fallopian tube (tubal) tissue. Tumors of this type are also called ovarian adenocarcinoma. This
group of tumors accounts for 90% to 95% of all cases of ovarian cancer. Serum CA-125 is often elevated but is only
50% accurate so it is not a useful tumor marker to assess the progress of treatment.
Surface epithelial-stromal tumor
Classification
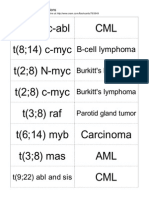
Epithelial-stromal tumors are classified on
the basis of the epithelial cell type, the
relative amounts of epithelium and stroma,
the presence of papillary processes, and the
location of the epithelial elements.
Microscopic pathological features determine
whether a surface epithelial-stromal tumor is
benign, borderline, or malignant (evidence
of malignancy and stromal invasion).
Borderline tumors are of uncertain
malignant potential.
This group consists of serous, mucinous,
endometrioid, clear cell, and brenner
(transitional cell) tumors, though there are a
few mixed, undifferentiated and unclassified
types.
Serous tumors
These tumors vary in size from small and
nearly imperceptible to large, filling the
abdominal cavity.
Benign, borderline, and malignant types
of serous tumors account for about 30%
of all ovarian tumors.
Ovarian cancers in women aged 20+, with area representing relative incidence and
color representing 5-year relative survival rate. Surface epithelial-stromal tumors
are labeled in center of the main diagram, and represent all types except the ones
separated at top.
75% are benign or of borderline
malignancy, and 25% are malignant
The malignant form of this tumor, serous cystadenocarcinoma, accounts for approximately 40% of all carcinomas
of the ovary and are the most common malignant ovarian tumors.
Benign and borderline tumors are most common between the ages of 20 and 50 years.
Malignant serous tumors occur later in life on average, although somewhat earlier in familial cases.
20% of benign, 30% of borderline, and 66% of malignant tumors are bilateral (affect both ovaries).
Components can include:
1. cystic areas
2. cystic and fibrous areas
3. predominantly fibrous areas
The chance of malignancy of the tumor increases with the amount of solid areas present, including both papillary
structures and any necrotic tissue present.
Surface epithelial-stromal tumor
Pathology
lined by tall, columnar, ciliated epithelial cells
filled with clear serous fluid
the term serous which originated as a description of the cyst fluid has come to be describe the particular type of
epithelial cell seen in these tumors
may involve the surface of the ovary
the division between benign, borderline, and malignant is ascertained by assessing:
cellular atypia (whether or not individual cells look abnormal)
invasion of surrounding ovarian stroma (whether or not cells are infiltrating surrounding tissue)
borderline tumors may have cellular atypia but do NOT have evidence of invasion
the presence of psammoma bodies are a characteristic microscopic finding of cystadenocarcinomas
Prognosis
The prognosis of a serous tumor, like most neoplasms, depends on
degree of differentiation
this is how closely the tumor cells resemble benign cells
a well-differentiated tumor closely resembles benign tumors
a poorly differentiated tumor may not resemble the cell type of origin at all
a moderately differentiated tumor usually resembles the cell type of origin, but appears frankly malignant
extension of tumor to other structures
in particular with serous malignancies, the presence of malignant spread to the peritoneum is important with
regard to prognosis.
The five year survival rate of borderline and malignant tumors confined to the ovaries are 100% and 70%
respectively. If the peritoneum is involved, these rates become 90% and 25%.
While the 5-year survival rates of borderline tumors are excellent, this should not be seen as evidence of cure, as
recurrences can occur many years later.
Mucinous tumors
Mucinous tumors:
Closely resemble their serous counterparts but unlikely to be bilateral
Somewhat less common, accounting for about 25% of all ovarian neoplasms
Occur principally in middle adult life and are rare before puberty and after menopause
80% are benign or borderline and about 15% are malignant
Mucinous cystadenocarcinomas (the malignant form of this tumor) are relatively uncommon and account for only
10% of all ovarian cancers
Mucinous tumors are characterized by more cysts of variable size and a rarity of surface involvement as
compared to serous tumors
Also in comparison to serous tumors, mucinous tumors are less frequently bilateral, approximately 5% of primary
mucinous tumors are bilateral.
May form very large cystic masses, with recorded weights exceeding 25kg
Appear as multiloculated tumors filled with sticky, gelatinous fluid
Surface epithelial-stromal tumor
Pathology
Benign mucinous tumors are characterized by a lining of tall columnar epithelial cells with apical mucin and the
absence of cilia, similar in appearance with benign cervical or intestinal epithelia. Cystadenocarcinomas (malignant
tumors) contain a more solid growth pattern with the hallmarks of malignancy: cellular atypia and stratification, loss
of the normal architecture of the tissue, and necrosis. The appearance can look similar to colonic cancer. Clear
stromal invasion is used to differentiate borderline tumors from malignant tumors.
Prognosis
10-year survival rates for borderline tumors contained within the ovary, malignant tumors without invasion, and
invasive malignant tumors are greater than 95%, 90%, and 66%, respectively. One rare but noteworthy condition
associated with mucinous ovarian neoplasms is pseudomyxoma peritonei. As primary ovarian mucinous tumors are
usually unilateral (in one ovary), the presentation of bilateral mucinous tumors requires exclusion of a non-ovarian
origin.
Endometrioid tumors
Endometrioid tumors account for approximately 20% of all ovarian cancers and are mostly malignant (endometroid
carcinomas). They are made of tubular glands bearing a close resemblance to benign or malignant endometrium.
15-30% of endometrioid carcinomas occur in individuals with carcinoma of the endometrium, and these patients
have a better prognosis. They appear similar to other surface epithelial-stromal tumors, with solid and cystic areas.
40% of these tumors are bilateral, when bilateral, metastases is often present.
Pathology
Glands bearing a strong resemblance to endometrial-type glands
Benign tumors have mature-appearing glands in a fibrous stroma
Borderline tumors have a complex branching pattern without stromal invasion
Carcinomas (malignant tumors) have invasive glands with crowded, atypical cells, frequent mitoses. With
poorer differentiation, the tumor becomes more solid.
Prognosis
Prognosis again is dependent on the spread of the tumor, as well as how differentiated the tumor appears. The overall
prognosis is somewhat worse than for serous or mucinous tumors, and the 5-year survival rate for patients with
tumors confined to the ovary is approximately 75%.
Clear cell tumors
Clear cell tumors are characterized by large epithelial cells with
abundant clear cytoplasm and may be seen in association with
endometriosis or endometrioid carcinoma of the ovary, bearing a
resemblance to clear cell carcinoma of the endometrium. They may be
predominantly solid or cystic. If solid, the clear cells tend to be
arranged in sheets or tubules. In the cystic variety, the neoplastic cells
make up the cyst lining.
Prognosis
Micrograph of an ovarian clear cell carcinoma.
H&E stain.
These tumors tend to be aggressive, the five year survival rate for
tumors confined to the ovaries is approximately 65%. If the tumor has spread beyond the ovary at diagnosis, the
prognosis is poor
Surface epithelial-stromal tumor
Brenner tumor
Brenner tumors are uncommon surface-epithelial stromal cell tumors
in which the epithelial cell (which defines these tumors) is a
transitional cell. These are similar in appearance to bladder epithelia.
The tumors may be very small to very large, and may be solid or
cystic. Histologically, the tumor consists of nests of the
aforementioned transitional cells within surrounding tissue that
resembles normal ovary. Brenner tumors may be benign or malignant,
depending on whether the tumor cells invade the surrounding tissue.
Treatment
Brenner tumour. H&E stain.
For more general information, see ovarian cancer.
For advanced cancer of this histology, the US National Cancer Institute recommends a method of chemotherapy that
combines intravenous (IV) and intraperitoneal (IP) administration.[5] Preferred chemotherapeutic agents include a
platinum drug with a taxane.
Metastases
For surface epithelial-stromal tumors, the most common sites of metastasis are the pleural cavity (33%), the liver
(26%), and the lungs (3%).[6]
Effect on fertility
Fertility subsequent to treatment of surface epithelial-stromal tumors depends mainly on histology and initial staging
to separate it into early borderline (or more benign) versus advanced stages of borderline (or more malignant).
Conservative management (without bilateral oophorectomy) of early stage borderline tumors have been estimated to
result in chance of over 50% of spontaneous pregnancy with a low risk of lethal recurrence of the tumor (0.5%). On
the other hand, in cases of conservative treatment in advanced stage borderline tumors, spontaneous pregnancy rates
have been estimated to be 35% and the risk of lethal recurrence 2%.
Surface epithelial-stromal tumor
Additional images
Brenner tumour. H&E stain.
Sources
Braunwald, Eugene (2001). Harrison's principles of internal medicine (15th ed.). New York: McGraw-Hill.
ISBN0-07-913686-9.
Haber, Meryl H. (2002). Differential diagnosis in surgical pathology. Philadelphia: W.B. Saunders.
ISBN0-7216-9053-X.
References
[1]
[2]
[3]
[4]
[5]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ C56
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ D27
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=183
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=220
NCI Issues Clinical Announcement for Preferred Method of Treatment for Advanced Ovarian Cancer (http:/ / www. cancer. gov/ newscenter/
pressreleases/ IPchemotherapyrelease), January 2006
[6] (http:/ / jco. ascopubs. org/ content/ 20/ 4/ 982. full. pdf) PMID 11844820 (http:/ / www. ncbi. nlm. nih. gov/ pubmed/ 11844820): Epithelial
Ovarian Cancer Metastasizing to the Brain: A Late Manifestation of the Disease With an Increasing Incidence
External links
Johns Hopkins: "Surface Epithelial Tumors" (http://ovariancancer.jhmi.edu/epithelial.cfm)
Diagram: "Epithelial Stromal Ovarian Tumors" (http://www.netterimages.com/image/3561.htm)
Article Sources and Contributors
Article Sources and Contributors
Surface epithelial-stromal tumor Source: http://en.wikipedia.org/w/index.php?oldid=560101173 Contributors: Alborz Fallah, Arcadian, Arnavchaudhary, Atp413, BigTenDoc, Casualdoc,
Cyrusa, DO11.10, Drmies, Galaxiaad, Grendelkhan, Hopping, Jay5r, Jibbajabba, Julesd, Laurienne Bell, Lisatwo, Mikael Hggstrm, Nephron, Niceguyedc, Optigan13, Pathologyresident,
Pekaje, Pigman, RDBrown, Rettetast, Some standardized rigour, StephP, Tarek, Una Smith, Wouterstomp, Yeokesh, Zigger, 11 anonymous edits
Image Sources, Licenses and Contributors
File:Brenner tumour high mag cropped.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Brenner_tumour_high_mag_cropped.jpg License: Creative Commons
Attribution-Sharealike 3.0 Contributors: Nephron
File:Incidence of ovarian cancers by histopathology.png Source: http://en.wikipedia.org/w/index.php?title=File:Incidence_of_ovarian_cancers_by_histopathology.png License: Creative
Commons Zero Contributors: Mikael Hggstrm
Image:Ovarian clear cell carcinoma -a- very high mag - cropped.jpg Source:
http://en.wikipedia.org/w/index.php?title=File:Ovarian_clear_cell_carcinoma_-a-_very_high_mag_-_cropped.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: Nephron
Image:Brenner tumour4.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Brenner_tumour4.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: Nephron
License
Creative Commons Attribution-Share Alike 3.0
//creativecommons.org/licenses/by-sa/3.0/
You might also like
- Translocations Small00center10 765849Document5 pagesTranslocations Small00center10 765849dger11No ratings yet
- Translocations Small00center10 765849Document5 pagesTranslocations Small00center10 765849dger11No ratings yet
- Klyosov 1Document31 pagesKlyosov 1dger11No ratings yet
- Squamous Cell Carcinoma of The LungDocument2 pagesSquamous Cell Carcinoma of The Lungdger11No ratings yet
- Luntz Wexner AnalysisDocument17 pagesLuntz Wexner Analysisdger11No ratings yet
- Congenital Cytomegalovirus InfectionDocument5 pagesCongenital Cytomegalovirus Infectiondger11No ratings yet
- Translocations Small00center10 765849Document5 pagesTranslocations Small00center10 765849dger11No ratings yet
- Vertically Transmitted InfectionDocument6 pagesVertically Transmitted Infectiondger11No ratings yet
- Medullary Thyroid CancerDocument5 pagesMedullary Thyroid Cancerdger11No ratings yet
- Allergic Bronchopulmonary AspergillosisDocument6 pagesAllergic Bronchopulmonary Aspergillosisdger11No ratings yet
- Deci Dual IzationDocument2 pagesDeci Dual Izationdger11No ratings yet
- Pneumocystis Pneumonia Diagnosis and TreatmentDocument5 pagesPneumocystis Pneumonia Diagnosis and Treatmentdger11No ratings yet
- Atrophic VaginitisDocument3 pagesAtrophic Vaginitisdger11No ratings yet
- The Flyting of Dunbar and KennedyDocument25 pagesThe Flyting of Dunbar and KennedyCholo MercadoNo ratings yet
- Renal Cell CarcinomaDocument15 pagesRenal Cell Carcinomadger11No ratings yet
- Cancer SyndromeDocument6 pagesCancer Syndromedger11No ratings yet
- Congenital Cytomegalovirus InfectionDocument5 pagesCongenital Cytomegalovirus Infectiondger11No ratings yet
- Nodular Fasciitis: Etiology and Clinical CourseDocument3 pagesNodular Fasciitis: Etiology and Clinical Coursedger11No ratings yet
- Vertically Transmitted InfectionDocument6 pagesVertically Transmitted Infectiondger11No ratings yet
- Squamous Cell Carcinoma of The LungDocument2 pagesSquamous Cell Carcinoma of The Lungdger11No ratings yet
- Medullary Thyroid CancerDocument5 pagesMedullary Thyroid Cancerdger11No ratings yet
- Anglo SaxonDocument4 pagesAnglo Saxondger11No ratings yet
- Viking00barr BWDocument154 pagesViking00barr BWdger11No ratings yet
- Allergic Bronchopulmonary AspergillosisDocument6 pagesAllergic Bronchopulmonary Aspergillosisdger11No ratings yet
- The Flyting of Dunbar and KennedyDocument25 pagesThe Flyting of Dunbar and KennedyCholo MercadoNo ratings yet
- Outlines in PathologyDocument200 pagesOutlines in PathologyLisztomaniaNo ratings yet
- Vuk Stefanovic Karadzic: Srpski Rjecnik (1898)Document935 pagesVuk Stefanovic Karadzic: Srpski Rjecnik (1898)krca100% (2)
- Calender of The Close RollsDocument938 pagesCalender of The Close Rollsdger11No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Its A Simple Test Cervical Cancer Screening UrduDocument1 pageIts A Simple Test Cervical Cancer Screening UrduIqbal BaryarNo ratings yet
- Terapi Lesi Pra-Kanker Leher Rahim (Krioterapi)Document31 pagesTerapi Lesi Pra-Kanker Leher Rahim (Krioterapi)yulia gustiNo ratings yet
- 1-General Table For Screening - LockedDocument34 pages1-General Table For Screening - LockedChristian Yzaguirre AbantoNo ratings yet
- Ovarian Cancer TypesDocument60 pagesOvarian Cancer TypesLeslie Ann Pablo MarantanNo ratings yet
- Survival Outcomes For Different Subtypes of Epithelial Ovarian CancerDocument7 pagesSurvival Outcomes For Different Subtypes of Epithelial Ovarian CancerasclepiuspdfsNo ratings yet
- Pathology of The Female Genital Tract Course OutlineDocument2 pagesPathology of The Female Genital Tract Course OutlineDanica BiteraNo ratings yet
- Lesi Prakanker & Tumor Ginekologi (Versi 2003)Document71 pagesLesi Prakanker & Tumor Ginekologi (Versi 2003)Satwika EkanandaNo ratings yet
- Artikel Trias Mei Purnama AnggrainiDocument10 pagesArtikel Trias Mei Purnama AnggrainiRenandaNo ratings yet
- 2014 AsccpDocument62 pages2014 AsccpGia DuyNo ratings yet
- CCSP GuidelinesDocument42 pagesCCSP GuidelinesAzhagendranNo ratings yet
- Management of Abnormal Pap Smears PresentationDocument17 pagesManagement of Abnormal Pap Smears Presentationapi-210786702100% (1)
- TAMIZACION CANCER DE CUELLO UTERINO EN COLOMBIADocument53 pagesTAMIZACION CANCER DE CUELLO UTERINO EN COLOMBIALUIS FERNANDO PLAZAS MUNOZNo ratings yet
- Mucinous Cystadenoma 0708Document12 pagesMucinous Cystadenoma 0708eosfieldNo ratings yet
- Gyne Long Exam 5 Premalignant and Malignant Lesions Vulva and VaginaDocument3 pagesGyne Long Exam 5 Premalignant and Malignant Lesions Vulva and VaginaRemelou Garchitorena AlfelorNo ratings yet
- SGH Cervical Screening Colposcopy PathwaysDocument13 pagesSGH Cervical Screening Colposcopy PathwaysAbraham ChiuNo ratings yet
- Distribuţia Genotipurilor Virusului Papiloma Uman La Paciente Din Zona MoldoveiDocument5 pagesDistribuţia Genotipurilor Virusului Papiloma Uman La Paciente Din Zona MoldoveiZama VitalieNo ratings yet
- Jurnal Vaksin HPVDocument9 pagesJurnal Vaksin HPVlitaayuningdyahNo ratings yet
- Pap TestDocument24 pagesPap TestAmirah MuhammadNo ratings yet
- Daftar Pustaka Kanker ServiksDocument3 pagesDaftar Pustaka Kanker ServiksRiri AmalinaNo ratings yet
- TNMC CreditDocument7 pagesTNMC CreditSathyaNo ratings yet
- CS-PUB-LAB-1 Cervical Cytology Management Recommendations Explanatory GuideDocument11 pagesCS-PUB-LAB-1 Cervical Cytology Management Recommendations Explanatory GuideMc Coral100% (1)
- Does Speculum Lubricant Affect Liquid Based Papanicolaou Test Adequacy?Document6 pagesDoes Speculum Lubricant Affect Liquid Based Papanicolaou Test Adequacy?Cristina CostaNo ratings yet
- Ovarian TumoursDocument41 pagesOvarian TumoursVlad RazvanNo ratings yet
- Cervical Pap Smear Study in a Tertiary HospitalDocument4 pagesCervical Pap Smear Study in a Tertiary HospitalkushalNo ratings yet
- 9 Endometrial Hyperplasia - Libre PathologyDocument5 pages9 Endometrial Hyperplasia - Libre PathologyfadoNo ratings yet
- Bethesda SystemDocument186 pagesBethesda SystemJoyce Pardo FernandezNo ratings yet
- HPV Vaksin 11 Maret 2023 - Dr. Cindy Rani SpOG KFER PDFDocument35 pagesHPV Vaksin 11 Maret 2023 - Dr. Cindy Rani SpOG KFER PDFYuliyanahNo ratings yet
- საშვ. ყელის ფონური დაავ-ბი IIDocument32 pagesსაშვ. ყელის ფონური დაავ-ბი IIAchi BeridzeNo ratings yet
- Hubungan Tingkat Pengetahuan Kanker Serviks Dengan Minat Untuk Vaksinasi HPV Pada Mahasiswi Fakultas Kedokteran Universitas HKBP Nommensen MedanDocument4 pagesHubungan Tingkat Pengetahuan Kanker Serviks Dengan Minat Untuk Vaksinasi HPV Pada Mahasiswi Fakultas Kedokteran Universitas HKBP Nommensen Medanintan fairuzNo ratings yet
- Bethesda system for reporting cervical cytologyDocument3 pagesBethesda system for reporting cervical cytologyNgotelo FunwiNo ratings yet