Professional Documents
Culture Documents
Csim2.71 - The Patient With Proteinuria and Haematuria
Uploaded by
AinahMahaniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Csim2.71 - The Patient With Proteinuria and Haematuria
Uploaded by
AinahMahaniCopyright:
Available Formats
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
CSIM2.71 THE PATIENT WITH PROTEINURIA AND
HAEMATURIA
Focal
Diffuse
only a portion of glomeruli affected
all glomeruli affected
TERMS
Global
whole glomerulus affected
segmental
only a part of the glomerulus is affected (most focal lesions are also segmental)
proliferative
^cell numbers due to hyperplasia of one or more of the resident glomerular cells
membrane
alterations
crescent formation
capillary wall thickening
epithelial cell proliferation with mononuclear cell infiltration in Bowmans space
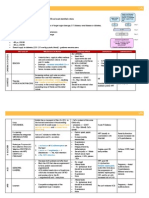
GLOMERULONEPHRITIS
Inflammatory condition of the glomeruli. Presented with Nephrotic or Nephritic
Syndrome
Common cause of ESRF in adults.
Presentation: Asymptomatic, haematuria (could be microscopic), proteinuria, renal failure or
HPT.
Abnormal Glomerulus
- Altered glomerular basement membrane (GBM) frequently result in significant renal
dysfunction.
- Crescent formation -> destruction of the affected glomerulus and is replaced by
fibrous scaring
Causes of PROTEINURIA
-
Glomerular dx
Tubulo-interstitial dx rarely
causes significant proteinuria
Physical exercise
Orthostatic proteinuria
Fever
Heart failure
Pregnancy
Inflammation of the glomeruli and nephrons which leads to;
- Damage to the glomerulus restricts blood flow, leading to compensatory ^BP
- Damage to the filtration mechanism allows protein and blood to enter urine.
- Loss of the usual filtration capacity leads to acute kidney injury
Looking for degree of damage and potential cause
- Imaging: CXR, renal ultrasound.
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
-
Blood: FBC, U&E, LFT,
ESR, CRP;
immunoglobulins,
electrophoresis,
complement (C3, C4);
autoantibodies (p555):
ANA, ANCA, anti-dsDNA,
anti-GBM; blood culture,
ASOT, HB A , anti-HCV
Urine: RBC casts, MC&S,
s
Bence Jones protein, ACR (see p286).
Presentation
Diagnosis
Treatm
ent
Prognos
is
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
IgA
Nephropathy
altered
regulation of IgA
^IgA possibly
due to infection,
which forms
immune
complexes and
deposits in
mesangial cells.
HenochSchonlein
Purpura (HSP)
Systemic IgA
nephropathy,
causing a small
vessel
vasculitis.
Systemic
lupus
erythematous
(SLE)
Common cause of
GN in adults
Young man (20-30
yo), Asians and
Caucasians with
episodic
macroscopic
haematuria,
recovery is often
rapid between
attacks
purpuric rash on
extensor surfaces
Arthralgias
Purpura
Abdominal pain,
GI bleeding
Hematuria
Mesangial
proliferation,
immunofluores
cence (IF)
shows deposits
of IgA and C3
+ IF for IgA
and C3 in skin
or renal biopsy.
Cough, chest pain, nasal congestion
Maculopapular rash over her chest
Haematuria, proteinuria,
Antiglomerular
basement
membrane
(GBM)
A.k.a.
Goodpastures
disease caused
by autoantibodies to
type IV collagen
an essential
component of
the GBM
Poststreptococcal
Strep. Ag is
deposited on
the glomerulus
causing a host
rxn and immune
complex form.
Pulmonary
haemorrhage
Haematuria/nephi
ritc syndrome
AKI may occur
within days of
onset of
symptoms
Malaise, fatigue,
anorexia, weight
loss, arthralgias,
myalgias
Occurs 1-12 wks
after a sore throat
or skin infection
Nephritic
syndrome
A/b develop
against 3
chain type IV
collagen in
GBM. Linear
deposition of
IgG along GBM
A/b detected
by ELISA
ANCA
capillary loop
staining with
IgG and C3
and extensive
crescent
formation
Urinalysis
Inflammation
rxn affecting
mesangial and
endothelial
cells
IF: IgG and C3
deposits
^ASOT ^C3
Control
BP with
ACEi,
immuno
suppres
sion
may
slow
decline
of renal
function
.
~15% ->
ESRF. If
same as
both
IgA
nephritic
nephrop
and
athy
nephroti
c 50% ->
ESRF
~1/3 SLE have renal
disease with vascular,
glomerular and
tubulointerstitial
damage.
Relapse
are rare.
Prognosi
s is poor
if
dialysisdepende
nt
presenta
tion.
Complica
tion
Severe
HPT,
renal
failure,
primary
disease
(SLE)
Plasma
exchan
ge,
steroids
,
Cycloph
ospham
ide
~20% ->
ESRF.
POOR
prognosi
s: Male,
^BP,
proteinur
ia or
renal
failure at
presenta
tion.
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
Rapidly
progressive
Most aggressive
GN. Could cause
ESRF over days.
AKI +- systemic
features (fever,
myalgia, weight
loss,
haemoptysis)
Pulmonary
haemorrhage is
the commonest
cause of death
ANCA +ve
patients
-
Aggressive
immunosupresion with
high-dose IV steroids
and cyclophophamide
+- plasma exchange
5 year survival 80%
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
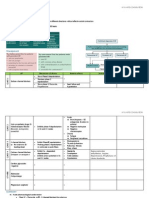
NEPHROTIC SYNDROME
1. Definition: the renal excretion of more than 3.5g of protein during a 24 hour period
2. Assessed by the collection of a cumulative 24h urine specimen.
3. As a result of abnormalities of the basement membrane, large amounts of plasma
proteins are filtered into the glomerular ultrafiltrate
4. Not associated with significant glomerular inflammation and red blood cell casts or other
signs of glomerular inflammation are present
5. The loss of nephrotic quantities of proteins for prolonged periods can result in
hypoproteinamia
6. Peripheral oedema because of loss of plasma oncotic pressure
Criteria
OEDEMA
PROTEINURIA (> 3.5 G/DAY/1.73
M2 )
Structural damage to the glomerular
basement membrane leads to an
increase in the size and number of
pores -> allow more and larger
molecules.
Fixed negatively charged components
are present in the glomerular capillary
wall, which repel negatively charged
protein molecules.
Reduction of this fixed charge occurs
in glomerular disease and appears to
be a key factor in the genesis of heavy
proteinuria.
HYPOALBUMINAEMIA (< 3.5G/DL)
-
Urinary protein loss of the order 3.5g
daily or more in adult required to
cause hypoalbuminaemia
Increased of catabolism of reabsorbed
albumin in the proximal tubules
though actual albumin synthesis is
increased.
Expansion of the interstitial
compartment is secondary to the
accumulation of sodium in the
extracellular compartment.
This is due to an imbalance between
oral (or parenteral) sodium intake and
urinary sodium output, as well as
alterations of fluid transfer across
capillary walls.
HYPERLIPIDAEMIA (C > 250 MG/DL)
-
Hyperlipidaemia is the consequence of
increased synthesis of lipoproteins in
the liver, abnormal transport of
circulating lipid particles, and
decreased catabolism.
HypoA stimulates protein synthesis in
the liver. Protein synthesis, lipid
synthesis.
Nephrotic syndrome is NOT a diagnosis. Therefore, the underlying cause should always be
sought.
Presentation
i.
ii.
iii.
Facial oedema
Peripheral oedema
Pleural effusion
iv.
v.
Ascites
Genital and sacral oedema
vi.
Histological patterns of NS; Minimal change, membranous nephropathy
1. Attributed to minimal change, membranous nephropathy. Consequence rather than
cause of nephrotic syndrome.
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
MEMBRANOUS NEPHROPATHY (COMMON CAUSE, 20-30% IN ADULT)
1. 75% are primary or idiopathic form but can be associated to 2 to;
- Malignancy (e.g. carcinoma of lung, colon, stomach, breast and lymphoma)
- drugs (penicillamine, gold, NSAIDs, probenecid, mercury, captopril),
- autoimmune disease (e.g. SLE, thyroiditis),
- Chronic infection (e.g. hepatitis B, hepatitis C, schistosomiasis, Plasmodium
malariae),
- SLE
2. At all stages, IF shows the presence of diffusely thickened
GBM of IgG and C3
3. COMMON: Adults, males
4. Asymptomatic proteinuria or frank nephrotic syndrome.
5. May present with macroscopic haematuria, hypertension
and/or renal impairment
6. POOR PROGNOSIS: HPT and higher degree of renal
impairment
7. 40% develop CKD
8. GOOD PROGNOSIS->
Younger, females, and
asymptomatic proteinuria of modest degree
9. 3 stages
Early: deposits are small can be missed on LM. EM
reveals small electron-dense deposits in the subepithelial aspects of the capillary walls
Intermediate: deposits are encircled by basement
membrane => appearance of spikes of basement membrane perpendicular to the
basement membrane on silver staining
Late: uniform thickening of the capillary basement membrane
MINIMAL CHANGE DISEASE
1. PAEDS: common cause, MALE good prognosis. X leads to CKD, facial oedema
2. ADULT: asso.
Idiopathic
With drugs (NSAIDs, lithium, antibiotics ( rifampicin, ampicillin, cephalosporins) ,
Hodgkins Lymphoma
3. Glomeruli appear normal on light microscopy but on EM, fusion of podocytes could be
seen
4. Tx: high dose corticosteroid therapy with prednisolone
60 mg/m2 daily (up to a maximum of 80 mg/day) for a
maximum of 46 weeks followed by 40 mg/m2 every
other day for a further 46 weeks corrects the urinary
protein leak in more than 95% of children
5. Two-thirds children have relapse and further courses of
corticosteroids are required.
6. One-third of these children regularly relapse on steroid
withdrawal, so that cyclophosphamide should be added
after repeat induction with steroids. A course of
cyclophosphamide 1.52.0 mg/kg daily is given for 8
12 weeks with concomitant prednisolone 7.515
mg/day.
MESANGIOCAPILLARY GN
1. Immune complex (IC)
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
Driven by circulating immune complexes, which deposit in the kidney and activate
complement via the classical pathway. An underlying cause can be found in most
cases, eg Hep C, SLE and monoclonal gammopathies.
2. Complement mediated
Less common and involves persistent activation of the alternative complement
pathway
3. BIOPSY: mesangial and endocapillary proliferation, a thickened capillary basement
membrane, double contouring (tramline) of the capillary walls. IF can show Ig
staining, complement staining or light chains depending on cause. EM shows electron
dense deposits.
FOCAL SEGMENTAL GLOMERULOSCLEROSIS (FSGS)
1. May be 1 or 2 (VUR, IgA nephropathy, Alports syndrome, vasculitis, sickle-cell disease)
2. Presentation: nephrotic syndrome or proteinuria. ~50% have impaired renal function.
3. BIOPSY: scarring of the glomeruli at certain segments (focal sclerosis). IF: IgM and C3
deposits at affected area.
4. Tx: corticosteroid. Resistant: cyclosphamide or ciclosporin
5. Untreated most progress ESRF
Complication
A. DVT
a. Hypercoagulable state due to urinary losses of anti-thrombin and thrombocytosis
b. Exacerbated by steroid therapy
c. Increased synthesis of clotting factors
d. Increased blood viscosity from the raised haematocrit
e. This is usually arterial and may affect the brain, limbs, and splanchnic circulation.
B. Pulmonary infection, Sepsis
a. Serum: IgG, complement, T cell function
b. Steroid: immunosuppressant toxicity
C. Accelerated atherosclerosis. Lipid abnormalities
D. Hypovolaemia
E. Acute renal failure (rare)
Investigation
DIAGNOSTIC
1.
2.
3.
4.
5.
Proteinuria +1> on 2/3 dipstick
P:C (> 200mg/mmol) (early morning)
Serum lipid
C3 level (sensitive n specific if other than MCD)
BP
FURTHER INVESTIGATION
1. Full blood count: HCT, WBC
2. Renal profile: normal in MCD
U+Es; Creatinine
3. Serum albumin: <25g/L
4. Urinalysis and quantification for
urinary protein excretion
abundant hyaline cast
Haematuria (other than MCD)
Na+ <10mmol/L in
hypovolaemia
Glucose
5. LFTs; ASOT
6. Urine culture
7. Varicella status should be known in
all children commencing steroids.
8. Other investigations
complement levels: suggest
other thn MCD
Antistreptolysin O titre and
throat swab
Hepatitis B antigen
9. Biopsy light microscopy/ EM/ IF
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
6. Management
Initial treatment
- Na restriction and THIAZIDE diuretics
- Unresponsive patients require
FUROSEMIDE 40-120mg daily +
amiloride
Normal protein intake
Albumin infusion
- only produce a transient effect
- Indication: diuretic-resistant, oliguria
and uraemia in the absence of severe
glomerular damage e.g. in minimal
change nephropathy.
Hypercoagulable states
- Predispose to venous thrombosis
This is due to loss of clotting factors
in the urine and increase in hepatic
production of fibrinogen.
Sepsis
- Susceptibility to infection due to
loss of immunoglobulin in the urine
Lipid abnormalities
- Increased CVS disease. Give HMGCoA
ACEi
- Reduce proteinuria by lowering
glomerular capillary filtration
pressure
NEPHRITIC SYNDROME
Variable amounts of proteinuria with the presence of RED BLOOD CELL CASTS (linear
aggregates of RBC formed in tubules as a consequence of glomerular haemorrhage)
And other inflammatory features (WBC and tubular cell casts) on urinalysis
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
Should get rapid evaluation of renal f(x)
Clinical features
i.
ii.
iii.
iv.
v.
Hypertension
Haematuria (usually micro, but can be macro)
Oliguria/acute renal failure
+/- odema
May be associated proteinurea
Crescenteric Glomerulonephritis
Proliferation of epithelial cells in
Bowmans space and signal the
dead of the glomeruli. Anti-GBM
Crescents on the renal biopsy
indicate acute severe glomerular
injury
Can occur in any type of
inflammatory glomerular injury
Start with a gap in the glomerular
capillary wall and GBM, plus gap in
Bowmans capsule
Circulating cells + inflammatory
mediators move into Bowmans
space
Fibrin, macrophages, T cells, fibroblasts start to proliferate
Crescents signify severe and aggressive immune damage and are a marker of severity of
renal damage
The percentage of glomeruli with crescents gives a guide to likely recovery
100% crescents is a poor outlook
10% crescents much better outlook
IgA Nephropathy
1.
2.
3.
4.
Young male patient, macroscopic haematuria after URTI
Deposition of IgA immunocomplexes in the glomeruli.
Less destructive
Routine tests
Haem FBC, Clotting factor
Biochemistry
i. U&E, LFT, calcium and albumin
ii. CRP/ESR
iii. Serum and urine Ig and electrophoresis
Immunology
i. Complement, dsDNA, ANA, ANCA, Rh factor, anti-GMB
Microbiology
i. Blood cultures
ii. MSU
Speed dealing with rapidly progressive GN
patients can rapidly become unwell with multisystem symptoms
all c ANCA positive patients are at risk of developing pulmonary involvement
rapid aggressive immunosuppression may salvage damaged nephrons and restore useful
renal function
THEMED WEEK 8: INVESTIGATION OF ABNORMAL RENAL FUNCTION
vasculitis will affect rest of body too
Untreated the kidneys will fail irreversibly
RECURRENT UTI
1. Same symptoms
2. No fixed definition of recurrent
a. 2 infections in 6 months
b. 3 infections in 12 months
3. After a single UTI there is a 30% risk of recurrence with 6 months
4. 60% will be the same organism (E coli)
5. After a first UTI 30-40% of patients will go onto have recurrent infections
Complicated or uncomplicated
a.
b.
c.
d.
Complicated: underlying anatomical or physiological abnormality
Uncomplicated: normal urinary tract
Complicated UTIs are more likely to recur but
Most recurrent infections occur in otherwise healthy women with a normal urinary tracts
Investigations
1.
2.
3.
4.
5.
Confirm infection dipstick and MSU
Other conditions can mimic infection
Confirm antibiotic sensitivities
History of previous antibiotic use
USS
Treatment
1. Be aware of the risk of resistance
2. Non-antibiotic treatments
Cranberry juice
Increase fluid intake
Probiotics
Regular and/or post coital complete voiding
Avoid spermicidal use/diaphragm
Topical oestrogens
3. Antibiotics
Long-term prophylaxis (1-2 yrs)
Low dose, at night
Single post-coital antibiotic dose
Self-treat
4.
5. Long term management
Low dose, once daily prophylactic antibiotics is an effective treatment for recurrent UTI.
Treatment significantly reduces the frequency of infection.
There is a risk on increasing antibiotic resistance and therefore treatment should be
reserved for patients with frequent, disabling infections.
Treatment should be for a limited period of time, usually 1-2 years, after which treatment
should be stopped and the patient re-assessed.
Single dose post-coital antibiotics can also be effective, particularly if infections follow
intercourse.
6.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Urinary IncontinenceDocument1 pageUrinary IncontinenceAinahMahaniNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- CSIM2.26 - Pituitary FunctionDocument3 pagesCSIM2.26 - Pituitary FunctionAinahMahaniNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Csim2.25 - Electrolyte Imbalance Calcium and BoneDocument7 pagesCsim2.25 - Electrolyte Imbalance Calcium and BoneAinahMahaniNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Csim2.92 - HypoventilationDocument1 pageCsim2.92 - HypoventilationAinahMahaniNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Csim2.26 - Pituitary F (X) Unusual DiabetesDocument2 pagesCsim2.26 - Pituitary F (X) Unusual DiabetesAinahMahaniNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- CSIM2.91 - COPD and Pulmonary HypertensionDocument2 pagesCSIM2.91 - COPD and Pulmonary HypertensionAinahMahaniNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Csim2.25 - Electrolyte ImbalanceDocument4 pagesCsim2.25 - Electrolyte ImbalanceAinahMahaniNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Csim2.26 - Pituitary F (X)Document1 pageCsim2.26 - Pituitary F (X)AinahMahaniNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Csim2.25 - Iron Metabolism & StorageDocument4 pagesCsim2.25 - Iron Metabolism & StorageAinahMahaniNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Csim2.25 - Electrolyte Imbalance Iron Metabolism & StorageDocument1 pageCsim2.25 - Electrolyte Imbalance Iron Metabolism & StorageAinahMahaniNo ratings yet
- Csim2.94 - Interstitial Lung DiseaseDocument3 pagesCsim2.94 - Interstitial Lung DiseaseAinahMahaniNo ratings yet
- CSIM2.24 - Signal TransductionDocument6 pagesCSIM2.24 - Signal TransductionAinahMahaniNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Penilaian Bahan TamhidiDocument3 pagesPenilaian Bahan TamhidiAinahMahaniNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- CSIM2.90 - Occupational AsthmaDocument1 pageCSIM2.90 - Occupational AsthmaAinahMahaniNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- CPTP - Pregnancy & LactatingDocument1 pageCPTP - Pregnancy & LactatingAinahMahaniNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- CPTP - Pud + Altered Bowel HabitDocument3 pagesCPTP - Pud + Altered Bowel HabitAinahMahaniNo ratings yet
- CPTP - Poisonig MH Misuse of DrugsDocument5 pagesCPTP - Poisonig MH Misuse of DrugsAinahMahaniNo ratings yet
- Penilaian Bahan MUAYYIDDocument3 pagesPenilaian Bahan MUAYYIDAinahMahaniNo ratings yet
- CPTP - Parkinson & MVMT DisordersDocument2 pagesCPTP - Parkinson & MVMT DisordersAinahMahaniNo ratings yet
- CPTP - PainDocument3 pagesCPTP - PainAinahMahaniNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CPTP - EpilepsyDocument4 pagesCPTP - EpilepsyAinahMahaniNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- CPTP - Infection and Antibiotics 2Document3 pagesCPTP - Infection and Antibiotics 2AinahMahaniNo ratings yet
- CPTP - Asthma & CopdDocument5 pagesCPTP - Asthma & CopdAinahMahaniNo ratings yet
- Infection and AntibioticsDocument4 pagesInfection and AntibioticsAinahMahaniNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- CPTP - Diabetes and Lipid Lowering DrugsDocument4 pagesCPTP - Diabetes and Lipid Lowering DrugsAinahMahaniNo ratings yet
- Infection and AntibioticsDocument4 pagesInfection and AntibioticsAinahMahaniNo ratings yet
- CPTP - HPT & HFDocument4 pagesCPTP - HPT & HFAinahMahaniNo ratings yet
- CPTP - Af & Anti CoagulationDocument4 pagesCPTP - Af & Anti CoagulationAinahMahaniNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Themed Week 7 - LIVERDocument24 pagesThemed Week 7 - LIVERAinahMahaniNo ratings yet
- Medical AbbreviationsDocument11 pagesMedical AbbreviationsbtraNo ratings yet
- Acute Renal FailureDocument4 pagesAcute Renal FailureKim GarciaNo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument3 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsNicole de Leon0% (1)
- Renal Haemodialysis: Adjudication RuleDocument3 pagesRenal Haemodialysis: Adjudication RuleMohammed ZubairNo ratings yet
- DNA Doubling Occurs During Cell Cycle InterphaseDocument26 pagesDNA Doubling Occurs During Cell Cycle InterphaseAbhani MøhitNo ratings yet
- Company Profile 2018Document18 pagesCompany Profile 2018Sarana Renal IndonesiaNo ratings yet
- A. Case Study Thesis-Front Page (Revised)Document10 pagesA. Case Study Thesis-Front Page (Revised)Lopirts NiganiNo ratings yet
- Mantak Chia - Five Elements Nutrition Alphabetic Food ListDocument74 pagesMantak Chia - Five Elements Nutrition Alphabetic Food ListLautaro Risso100% (1)
- Anemia and Chronic Kidney Disease: Stages 1-4Document16 pagesAnemia and Chronic Kidney Disease: Stages 1-4Pearl Raiza HadaniNo ratings yet
- Biology SrSecDocument12 pagesBiology SrSecdadan vishwakarmaNo ratings yet
- Biology Assignment Class-XDocument3 pagesBiology Assignment Class-XCoolCJ 1410No ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Group 10 Urine FormationDocument27 pagesGroup 10 Urine FormationgracechamdimbaNo ratings yet
- Biology: Revised Syllabus For Higher Secondary First Year CourseDocument4 pagesBiology: Revised Syllabus For Higher Secondary First Year CourseamitumikoibNo ratings yet
- The Kidney DissectionDocument4 pagesThe Kidney DissectionBeverly Carballo - MoguelNo ratings yet
- NCERT Solutions For Class 11 Biology Chapter 19: Excretory Products and Their Elimination Class 11Document6 pagesNCERT Solutions For Class 11 Biology Chapter 19: Excretory Products and Their Elimination Class 11AlfaazNo ratings yet
- Kidney Friendly Diet HandoutDocument3 pagesKidney Friendly Diet Handoutapi-474639492No ratings yet
- Oral Revalida ReviewerDocument10 pagesOral Revalida RevieweranneNo ratings yet
- What in The Cell Is Going OnDocument13 pagesWhat in The Cell Is Going Onsizzla7No ratings yet
- Cambridge International General Certificate of Secondary EducationDocument20 pagesCambridge International General Certificate of Secondary EducationMikaNo ratings yet
- Anesthetic Consideration in Hypertensive PatientDocument11 pagesAnesthetic Consideration in Hypertensive PatientYosiAsmaraNo ratings yet
- Congenital AnomaliesDocument69 pagesCongenital AnomaliesArnella HutagalungNo ratings yet
- Pharmacology-I Practical ManualDocument24 pagesPharmacology-I Practical ManualJunaed Ahmed50% (2)
- National NORCET-3 - FinalDocument90 pagesNational NORCET-3 - FinalSHIVANIINo ratings yet
- Krok 1 - 2020 (Feb) (General Medicine) - EneutronDocument41 pagesKrok 1 - 2020 (Feb) (General Medicine) - EneutronHarsh NimavatNo ratings yet
- Path Questions (USMLE)Document27 pagesPath Questions (USMLE)Goljan UsmleNo ratings yet
- Disorders of Water and Sodium BalanceDocument21 pagesDisorders of Water and Sodium BalanceStanNo ratings yet
- Pathology B - Midterm Ratio: Prelim TopicsDocument69 pagesPathology B - Midterm Ratio: Prelim TopicsHuey Manalang JavierNo ratings yet
- Nursing Care Plan for AML PatientDocument16 pagesNursing Care Plan for AML PatientAllan Macacapagal67% (9)
- Suggested Reading Materials: SectionDocument2 pagesSuggested Reading Materials: SectionAsh100% (1)
- NLUJ Course CurriculumDocument68 pagesNLUJ Course CurriculumChetan MitraNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)