Professional Documents
Culture Documents
Antihistamines in Asthma PDF
Uploaded by
dishoomdishoomOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antihistamines in Asthma PDF
Uploaded by
dishoomdishoomCopyright:
Available Formats
SELECTED PRESENTATION
ARE ANTIHISTAMINES USEFUL IN MANAGING ASTHMA?*
Based on a presentation by Andrew Wilson, MD
lthough it is generally considered that
many antihistamines have little or no
efficacy in managing asthma, they are
worth another look, because histamine
is a major mediator that can cause airway smooth muscle constriction and because it is a
major product of mast cells and basophils, the primary cells responsible for allergic reactions. In addition,
bronchial hyperresponsiveness to histamine is a key
feature in the diagnosis of asthma. The role of histamine, through its H1 receptors, in activating various
immune system cells, such as macrophages, dendritic
cells, or even lymphocytes, and contributing to airway
inflammation should not be underestimated.
The failure of antihistamines to produce meaningful
clinical effects in asthma can be attributed to drug potency, dose-limiting anticholinergic effects and central nervous system side effects, particularly with first-generation
agents, and redundancy in the immune system where
other mediators, such as leukotrienes and prostanoids,
are also potent causes of lower airway obstruction.
ANTIHISTAMINES HAVE ANTI-INFLAMMATORY EFFECTS
Studies have shown that antihistamines have a doseresponse effect on the release of various mediators in
human and animal allergic reaction models. Other antiinflammatory properties have also been recognized.1 For
example, one study using ovalbumin (OVA) stimulated
T-cells from mice treated with desloratadine and challenged with OVA found that desloratadine reduced
*Based on a presentation given by Andrew Wilson,
MD, at a luncheon seminar held in conjunction with the
2003 World Allergy Congress.
Department of Clinical Pharmacology, Ninewells
Hospital, Dundee, Scotland.
Advanced Studies in Medicine
proinflammatory Th2 cytokines but had no significant
effect on anti-inflammatory Th1 cytokines.2
Several studies evaluating the role of antihistamines
in blood-cell trafficking in asthma and seasonal allergic
rhinitis suggest that antihistamines reduce the movement of inflammatory cells from the circulation into the
tissues.3-5 In one study, antihistamines produced a significant dose-related reduction in soluble intracellular adhesion molecule-1 from nasal epithelial cells cultured in the
presence of eosinophils treated with latex beads, and this
was associated with a dose-related attenuation of
eosinophil adherence to endothelial cells.3
Similarly, a study of 20 children with seasonal allergic rhinitis in which nasal lavage was performed before
and after seasonal treatment with cetirizine found that
the antihistamine reduced the number of eosinophils in
the nasal lavage, suggesting decreased trafficking into the
nasal mucosa.4 A similar finding was noted in a study of
12 asthmatic patients who were treated with cetirizine 15
mg twice daily or placebo for 4 weeks in the beginning
of the pollen season and then challenged with allergen.
Bronchial alveolar lavage 24 hours after allergen challenge revealed significantly fewer eosinophils in the cetirizine group compared with the placebo group.5
SEASONAL ALLERGIC RHINITIS WITH ASTHMA
Several studies evaluating the effects of antihistamines on asthma in the context of seasonal allergic
rhinitis have found that these agents exert beneficial
effects on asthma symptoms. In a 6-week parallelgroup study comparing cetirizine with placebo in 90
patients with asthma and seasonal allergic rhinitis during pollen season, cetirizine significantly reduced asthma symptoms, such as chest tightness, wheezing,
breathlessness, and cough.6 Patients taking cetirizine
also reported improvement in quality of life measures and
S517
SELECTED PRESENTATION
were more likely to continue with the study compared
with those taking placebo. These results are a far cry
from a recommendation made in 1983 that antihistamines be contraindicated in asthma. A more recent 4week study of desloratadine 5 mg once daily versus
montelukast 10 mg once daily versus placebo, which
included patients with severe asthma, found that both
active treatments improved symptom severity scores
and reduced bronchodilator requirements.7 It is not
known whether these beneficial effects result from the
reduction in the magnitude of the nasal airway disease
or whether they reflect direct effects of antihistamines
on the lower airways.
Another important study, the Early Treatment of
the Atopic Child (ETAC) study evaluated the development of asthma in children aged 1 to 2 years with
atopic dermatitis and a positive family history of atopy
but no history of wheezing after 6 months of age after
18 months of treatment with cetirizine 0.25 mg/kg
twice daily or placebo.12 Although there was no significant effect with cetirizine therapy, when the entire
subject population was considered, cetirizine showed
significant protective effects against developing asthma
in children with high IgE levels to grass pollen and
house dust mites. These effects were maintained after
discontinuation of treatment.
BRONCHIAL HYPERRESPONSIVENESS
ADDITIVE THERAPY
Antihistamines have been shown in several studies to
exert beneficial effects on bronchial hyperresponsiveness.
In one study, 16 patients who were shown to have a dual
response to allergen challenge were treated with twicedaily cetirizine 15 mg or placebo.8 Although there was no
change in early allergic response, there was a significant
reduction in the late allergic response in the cetirizinetreated group versus placebo, as measured by maximum
fall in forced expiratory volume in 1 second (FEV1) and
area under the curve at 3 and 8 hours.
Exercise-challenge testing in 11 children taking
loratadine or placebo demonstrated improved airway
function during exercise with loratadine versus placebo.9 Mannitol-challenge testing in 20 subjects with
mild asthma who had received either fexofenadine 180
mg or montelukast 10 mg 2 days prior to challenge
revealed that fexofenadine significantly increased the
provocation dose (PD 15) compared with placebo and
delayed recovery from baseline, whereas the
leukotriene antagonist montelukast showed no change
in PD 15 compared with placebo but significantly
improved return to baseline.10
Histamine and the leukotrienes are released in concert during the early phase of allergic reactions.
Similarly, increased levels of histamine and
leukotrienes are found in the airways during the late
phase. A study by Roquet and colleagues showed that
the combination of loratadine (antihistamine) and
zafirlukast (leukotriene receptor antagonist) had
impressive, additive inhibitory effects on both the
early and the late bronchoconstrictive reaction
induced by allergen inhalation challenge in subjects
with asthma.13 In a placebo-controlled study evaluating combined therapy with montelukast (also a
leukotriene receptor antagonist) and loratadine in 117
patients with moderate persistent asthma and high
rates of allergic rhinitis (95%), the investigators found
that the addition of the antihistamine to the
leukotriene antagonist had a statistically significant
beneficial effect on FEV1, morning and evening peak
expiratory flow, and beta-agonist use.14
In a single-blind, double-dummy, randomized
crossover study comparing cetirizine plus montelukast
with inhaled and intranasal corticosteroids in 14
patients with moderately severe asthma and seasonal
allergic rhinitis during grass pollen season, Wilson and
his colleagues found that the combination of cetirizine
and montelukast had a significantly greater effect on
adenosine monophosphate challenge compared with
inhaled and intranasal budesonide, but the corticosteroids were significantly better in terms of exhaled
nitric oxide measurements. There was no significant
difference between the cetirizine/montelukast combination and the corticosteroids in terms of symptom
scores and bronchodilator use.15
ATOPIC MARCH
Asthma often coexists with allergic conditions,
such as eczema, dermatitis, and rhinitis. In a study of
children at high risk for developing asthma because of
allergy, high immunoglobulin E levels, and a strong
positive family history of allergy, only 3 of 45 children
taking ketotifen for 3 years developed asthma, compared with 14 of 40 children taking placebo, a statistically significant difference.11
S518
Vol. 4 (7A)
July 2004
SELECTED PRESENTATION
CONCLUSION
Antihistamines protect the lower airways from the
bronchoconstrictive effects of allergic reactions, have
anti-inflammatory effects, and seem to influence
bronchial hyperresponsiveness and the atopic march.
There is evidence that antihistamines are beneficial in
asthma, especially when it coexists with seasonal
allergic rhinitis or when antihistamines are combined
with leukotriene antagonists. More studies are
required to examine whetherand most importantly, in what instancesantihistamines should be used
alone or in combination with other agents for the
treatment of asthma.
REFERENCES
1. Togias A. H1-receptors: localization and role in airway
physiology and in immune functions. J Allergy Clin Immunol.
2003;112(4 suppl):S60-S68.
2. Bryce PJ, Geha R, Oettgen HC. Desloratadine inhibits allergen-induced airway inflammation and bronchial hyperresponsiveness and alters T-cell responses in murine models of
asthma. J Allergy Clin Immunol. 2003;112(1):149-158.
3. Abdelaziz MM, Devalia JL, Khair OA, Bayram H, Prior AJ,
Davies RJ. Effect of fexofenadine on eosinophil-induced
changes in epithelial permeability and cytokine release from
nasal epithelial cells of patients with seasonal allergic rhinitis. J Allergy Clin Immunol. 1998;101(3):410-420.
4. Ciprandi G, Tosca M, Ricca V, et al. Cetirizine treatment of
rhinitis in children with pollen allergy: evidence of antiallergic activity. Clin Exp Allergy. 1997;27(10):1160-1166.
5. Redier H, Chanez P, De Vos C, et al. Inhibitory effect of
cetirizine on the bronchial eosinophil recruitment induced by
allergen inhalation challenge in allergic patients with asthma. J Allergy Clin Immunol. 1992;90(2):215-224.
Advanced Studies in Medicine
6. Grant JA, Nicodemus CF, Findlay SR, et al. Cetirizine in
patients with seasonal rhinitis and concomitant asthma:
prospective, randomized, placebo-controlled trial. J Allergy
Clin Immunol. 1995;95(5, pt 1):923-932.
7. Baena-Cagnani CE, Berger WE, DuBuske LM, et al.
Comparative effects of desloratadine versus montelukast on
asthma symptoms and use of beta 2-agonists in patients
with seasonal allergic rhinitis and asthma. Int Arch Allergy
Immunol. 2003;130(4):307-313.
8. Wasserfallen JB, Leuenberger P, Pecoud A. Effect of certirizine, a new H1 antihistamine, on the early and late allergic reactions in a bronchial provocation test with allergen.
J Allergy Clin Immunol. 1993;91(6):1189-1197.
9. Baki A, Orhan F. The effect of loratadine in exerciseinduced asthma. Arch Dis Child. 2002;86(1):38-39.
10. Brannan JD, Anderson SD, Gomes K, King GG, Chan HK,
Seale JP. Fexofenadine decreases sensitivity to and montelukast improves recovery from inhaled mannitol. Am J
Respir Crit Care Med. 2001;163(6):1420-1425.
11. Bustos GJ, Bustos D, Bustos GJ, Romero O. Prevention of
asthma with ketotifen in preasthmatic children: a three-year
follow-up study. Clin Exp Allergy. 1995;25(6):568-573.
12. Allergic factors associated with the development of asthma
and the influence of certirizine in a double-blind, randomised, placebo-controlled trial: first results of ETAC. Early
Treatment of the Atopic Child. Pediatr Allergy Immunol.
1998;9(3):116-124.
13. Roquet A, Dahlen B, Kumlin M, et al. Combined antagonism of leukotrienes and histamine produces predominant
inhibition of allergen-induced early and late phase airway
obstruction in asthmatics. Am J Respir Crit Care Med.
1997;155(6):1856-1863.
14. Reicin A, White R, Weinstein SF, et al. Montelukast, a
leukotriene receptor antagonist, in combination with loratadine, a histamine receptor antagonist, in the treatment of
chronic asthma. Arch Intern Med. 2000;160(16):24812488.
15. Wilson AM, Orr LC, Sims EJ, Dempsey OJ, Lipworth BJ.
Antihistaminic effects of mediator blockade versus topical
corticosteroids in allergic rhinitis and asthma. Am J Respir
Crit Care Med. 2000;162(4, pt 1):1297-1301.
S519
SELECTED PRESENTATION
THE IDEAL INHALED CORTICOSTEROID*
Based on a presentation by Michael A. Kaliner, MD
nhaled corticosteroids are first-line therapy for
asthma in the United States and many other
countries; however, particularly at high doses,
they can produce unwanted local and systemic
side effects. Physicians should therefore consider the potential side effects of these agents in every
patient receiving them and at every visit.
Corticosteroids exert their beneficial effects on
asthma symptoms and lung function by interacting
with a corticosteroid receptor. Because the corticosteroid receptor in the lung is the same as the corticosteroid receptors elsewhere in the body, the amount of
inhaled drug that actually gets into the systemic circulation is the major determinant of systemic risk. The
lower the percentage of drug that gets into the lung,
the higher the percentage of drug that is lost to deposition in the oropharynx, where it is swallowed and
ultimately becomes available to circulate throughout
the body. Absorption of corticosteroids by the lung
and subsequent distribution into the systemic circulation is another source of systemic exposure. The quest
for the ideal inhaled corticosteroid thus begins with
the requirement that the agent be highly potent in the
lung and inactive elsewhere. The pharmacologic properties needed for an agent to produce such effects clinically are summarized in the Sidebar.
Is there such an agent? Recent and accumulating
data show that ciclesonide, a novel inhaled corticosteroid that is currently under investigation, possesses
some of these properties, is the safest inhaled cortico-
*Based on a presentation given by Michael A. Kaliner,
MD, at a dinner symposium held in conjunction with the
2003 World Allergy Congress.
Medical Director, Institute for Asthma and Allergy, and
Clinical Professor of Medicine, George Washington
University School of Medicine, Washington, DC.
S520
steroid studied to date, and may be the ideal corticosteroid for the treatment of asthma. The efficacy and
safety of ciclesonide were evaluated in a double-blind,
randomized, placebo-controlled clinical trial including
360 asthma patients with a forced expiratory volume
in 1 second of 60% to 90% and evidence of reversibility.1 Patients were pretreated with beclomethasone
dipropionate and, after 2 weeks, were randomized to
inhaled ciclesonide (80 g and 320 g) or placebo
once daily in the morning for 12 weeks. The efficacy
of the study regimens was estimated as follows: 62%
for ciclesonide 80 g, 77% for ciclesonide 320 g, and
45% for placebo. Compared with baseline, morning
peak expiratory flow increased by 129 mL and 192 mL
in patients taking the 80 g and 320-g doses of
ciclesonide, respectively, and decreased by 28 mL in
patients taking placebo. No significant differences
between treatments were found in the incidence of
adverse events.
The Ideal Inhaled Corticosteroid
NEGLIGIBLE LOCAL SIDE EFFECTS
Inactive parent compound
Low oropharyngeal deposition
Limited exposure of oropharynx to active molecule
HIGH POTENCY
High affinity for glucocorticoid receptor
Prolonged residence time in lung
Lipid conjugation in airways
NEGLIGIBLE SYSTEMIC SIDE EFFECTS
Low oral bioavailability/first-pass metabolism
Rapid systemic clearance
Complete plasma protein binding
Adapted from Derendorf H. Pharmacokinetic and pharmacodynamic
properties of inhaled corticosteroids in relation to efficacy and safety.
Respir Med. 1997;91(suppl A):22-28.
Vol. 4 (7A)
July 2004
SELECTED PRESENTATION
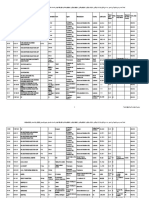
Table. Pharmacologic Properties of Ciclesonide and
Fluticasone Propionate
Ciclesonide/
Desciclesonide
Fluticasone
Propionate
Formulation
Solution
Suspension
Inhaled form
Inactive parent
compound
Active compound
Particle size
1.1 m to 2.1 m
65% >5 m
Oropharyngeal
38% (total)
72% to 78% deposition
Oral bioavailability
<1%
<1%
Pulmonary deposition
52%
12% to 13%
Residence time in lung
Prolonged (lipid
conjugation)
Prolonged (low solubility)
Receptor binding affinity 12/1200
1800
Protein binding
90%
98% to 99%
Clearance
396 L/hr
69 L/hr
Volume of distribution
1190 L
318 L
Elimination half-life
3.5 hr
7.8 hr
Similar efficacy was observed in a group of 283
patients with persistent asthma who had received
ciclesonide (160 g and 640 g once daily) or placebo
for 12 weeks.2 These patients were included in an
open-label extension study to determine the long-term
safety of ciclesonide. Patients first received a dose of
640 g of ciclesonide once daily or twice daily for 4
weeks, followed by an individualized dose ranging
from 160 g to 1280 g daily for another 36 weeks.
The incidence of oropharyngeal adverse events during
the extension study was low and consisted mainly of
pharyngitis (4%), voice alteration (2%) and oral candidiasis (1%). No relevant systemic or oral adverse
events were reported, and most respiratory adverse
events were considered unlikely or unrelated to
ciclesonide. Long-term administration of ciclesonide
was associated with a 28% increase in 24-hour urine
cortisol excretion.
Fluticasone propionate, the most frequently prescribed inhaled corticosteroid for asthma in the United
States, possesses several of the properties listed in the
Sidebar. Both fluticasone and ciclesonide are potent;
have high receptor-binding affinities; have prolonged
residence time in the lung, albeit by different mecha-
Advanced Studies in Medicine
nisms; and are rapidly cleared from the systemic
circulation by the liver. However, considerably
more oropharyngeal deposition and considerably
less pulmonary deposition occur with fluticasone
than with ciclesonide (Table). The high percentage
of oropharyngeal deposition with fluticasone is
associated with several local side effects, including
dysphonia, pharyngitis, and oral candidiasis. By
comparison, ciclesonide is inhaled as an inactive
parent compound that converts to desciclesonide,
or activated ciclesonide, in the lung, leaving very
little activated compound to be deposited in the
oropharynx.3
With fluticasone and several other inhaled corticosteroids, the dose response in terms of improvement in lung function is rather flat. A higher dose
will not necessarily produce additional clinical
improvement but will increase suppression of cortisol and will produce other unwanted effects.
Increased cortisol suppression with fluticasone is
most commonly seen in patients taking a daily dose
of 880 g or more.4 The daily dose should therefore
be lowered to 660 g or less. In contrast, studies
have shown that ciclesonide has no effect on the
adrenals and very little cortisol suppression.
REFERENCES
1. Langdon CG, Adler M, Mehra S, Drollmann A.
Ciclesonide is effective in the treatment of asthma: a 12week, placebo-controlled study. Presented at: the 4th World
Asthma Meeting; February 16-19, 2004; Bangkok,
Thailand. Abstract P-234.
2. Chapman KR, Boulet LP, DUrzo AD, Oedekoven C,
Engelstaetter R. Long-term administration of ciclesonide is
safe and well tolerated in patients with persistent asthma.
Presented at: the 4th World Asthma Meeting; February 1619, 2004; Bangkok, Thailand. Abstract P-232.
3. Richter K, Nave R, Biberger C, Bethke TD, Magnussen H.
Low oropharyngeal deposition of inhaled ciclesonide in
healthy subjects and asthma patients. Presented at: the 4th
World Asthma Meeting; February 16-19, 2004; Bangkok,
Thailand. Abstract P-235.
4. Brus R. Effects of high-dose inhaled corticosteroids on plasma cortisol concentrations in healthy adults. Arch Intern
Med. 1999;159(16):2549-2550.
S521
DEBATE
IMMUNOTHERAPY FOR ASTHMA: YES OR NO?
Based on presentations by Anthony Frew, MD* (the case for),
and N. Franklin Adkinson, Jr, MD (the case against).
THE CASE FOR
Immunotherapy is a viable treatment option for asthma, particularly allergic and established asthma. Current
therapies for asthma, such as inhaled corticosteroids,
improve lung function but do not cure the disease; however, they may also mask symptoms of allergy, an important cause of asthma that warrants treatment itself.
Immunotherapy is an important alternative because it
treats allergy rather than masking it.
As demonstrated in a meta-analysis of clinical studies evaluating the efficacy of immunotherapy against a
wide range of allergens, immunotherapy was associated with reductions in symptom scores, exacerbations,
and both specific and nonspecific airway responses,
the most important endpoints in clinical trials.1
The scale of improvement can be substantial. For
example, a 1-year, randomized, placebo-controlled, double-blind trial in 31 adults with asthma and allergy to
house dust mites found that specific immunotherapy significantly reduced inhaled steroid use by 38%, beta-agonist use by 46%, and symptom score by 57% and
significantly increased forced expiratory volume in 1 second (FEV1) from 85% to 89% of predicted values.2
Another important observation comes from a 3year prospective nonrandomized study in 22 children
younger than 6 years of age with asthma and allergy to
house dust mites and with or without rhinitis. The
study included 22 age-matched controls and demonstrated that specific immunotherapy prevents the
onset of new sensitizations.3
*Head, Department of Medical Specialties, University of
Southampton, Southampton, United Kingdom; Professor of
Medicine, Johns Hopkins University School of Medicine,
Baltimore, Maryland.
S522
With regard to disease prevention, a randomized,
but not double-blind, study of pollen immunotherapy
in 205 children between 6 and 14 years of age with
moderate-to-severe hay fever symptoms and with and
without mild asthma symptoms demonstrated that
immunotherapy reduced the risk of developing asthma.4 Although no children in the study had asthma
requiring daily treatment at study entry, 20% were
found to have mild asthma, as evaluated clinically and
by peak flow, during the pollen season. In the study
population as a whole, 26% developed asthma after 3
years of pollen immunotherapy, compared with 44%
in the control group.
Immunotherapy also has beneficial effects on disease progression. In a 4-year study of hyposensitization
therapy for mild and moderate bronchial asthma in
children, 70% of the subjects who received therapy
outgrew their asthma by 16 years of age, compared
with only 21% of those in the untreated control
group. Any symptoms in the treated group were classified mostly as mild, whereas asthma in 70% of the
untreated group (at age 16 years) was graded as moderate or severe.5
Although immunotherapy takes time to exert its
beneficial effects, which may prompt physicians to
avoid using it or discontinue it too soon, these effects
are more sustained than those of inhaled steroids. This
was demonstrated in a head-to-head comparison of
immunotherapy and inhaled budesonide in 51 young
patients with bronchial asthma who were given one
treatment or the other for 1 year and assessed for global symptom scores and FEV1 values.6 When both treatments were discontinued abruptly at 1 year and the
effects of cessation were analyzed, it was clear that
budesonide produced faster and more striking
improvement during the first few months of treatment
than immunotherapy, but its benefits declined rapidly
Vol. 4 (7A)
July 2004
DEBATE
once therapy was discontinued. Immunotherapy, by
comparison, produced slow but steady improvement
during the treatment period and a more gradual
decline in beneficial effect after therapy was stopped.
The effects of combining immunotherapy with
inhaled steroids have not been formally studied.
Another reason to consider immunotherapy in asthma management is cost. Asthma is an expensive disease,
with drugs accounting for most of the costs associated
with mild asthma and a considerable portion of costs
associated with moderate and more severe disease.
A 2-year study comparing immunotherapy with
placebo in adults with asthma exacerbated by seasonal
ragweed exposure found that the reduced medication
costs in patients receiving immunotherapy were counterbalanced by the costs of immunotherapy.7 The
important point, however, is that specific
immunotherapy may be cost effective if it reduces the
need for medication in future years or stops progression of disease.
Several surveys assessing the safety of immunotherapy have found that a high proportion of deaths attributed to this treatment occurred in patients with
asthma. Most of these deaths, however, were from precipitation of asthma rather than anaphylaxis, suggesting that safety can be considerably improved with
careful patient selection and appropriate management
of treatment-induced asthma. Other strategies to
improve safety include adequate staff training and the
use of antihistamine premedication.
THE CASE AGAINST
The use of immunotherapy for asthma does not
hinge on whether it is effective but on whether it is clinically indicated. Although immunotherapy may be effective in treating asthma, it is not clinically indicated if
better therapies can accomplish the same clinical endpointstherapies that are more efficacious, produce less
morbidity and mortality, and are more cost effective. In
addition, immunotherapy is not clinically indicated if its
unique benefits (ie, an additive effect, the ability to promote earlier or more frequent remissions, or the ability
to alter long-term outcome) are not significant.
The proposal to consider, then, is that allergen
immunotherapy is not clinically indicated for most
cases of allergic asthma, especially those involving
moderate or severe persistent asthma, because
immunotherapy is no better than currently available
Advanced Studies in Medicine
therapies and because there is little or no evidence that
its unique benefits are significant. For example, in a 2year study comparing immunotherapy with placebo in
adults with asthma exacerbated by ragweed allergy, the
positive clinical effects of immunotherapy on objective
measures of asthma and allergy were limited, and
many were not sustained over the course of the study.7
A meta-analysis of 24 studies of prophylactic
inhaled corticosteroid use in children with asthma
found that the average relative improvement in morning peak flow with inhaled steroids was 11%, twice
that of immunotherapy.8
In the only study comparing inhaled corticosteroids with immunotherapy in patients with asthma,
there was no significant difference between the early
response to budesonide in moderate doses and the
delayed response to immunotherapy.6 Although a
valiant study, it excluded patients with rhinitis and did
not evaluate higher doses of immunotherapy. A randomized, controlled, parallel-group study is needed.
In contrast, a randomized, double-blind, controlled study done at Johns Hopkins University
assessed the effects of immunotherapy in 121 children
with asthma and 4 to 7 major allergic sensitivities who
were already practicing allergy avoidance.9 The study
found no discernible effect of immunotherapy on
medication requirements, days of oral steroid use, use
of medical care for asthma, reported asthma symptoms, methacholine sensitivity, or the rate of partial or
complete remission from asthma.
Historical data indicate that there are 3 to 5 deaths
per year in the United States due to immunotherapy,
with 75% of the deaths occurring in patients with asthma. A French team has defined risk for systemic reactions to immunotherapy as a function of the depression
in FEV1 measurements taken at the time of injection,
indicating very clearly that uncontrolled asthma is a
major risk factor for all types of systemic reactions.10
As a result, practice standards now include guidelines that underscore the need to observe patients and
monitor pulmonary function. These guidelines, however, do not appear to have altered fatal outcomes of
immunotherapy in the United States. This reflects
the fact that immunotherapy is often administered by
general practitioners and specialists in areas other
than allergy and that treatment errors and patient
factors are not completely understood. In contrast,
inhaled steroids are not yet known to produce iatrogenic mortality.
S523
DEBATE
Several potential unique benefits of immunotherapy have been touted. One is immunologic specificity,
which differs from anti-inflammatory agents and antiimmunoglobulin E therapy. Specificity, however, is a
double-edged sword and may not be an advantage.
Another potential unique benefit is compliance, which
may be an advantage in patients with mild asthma and
in populations with limited access to medical care but
not in patients with moderate or severe asthma.
Cost is purported to be an advantage, but because
the costs of immunotherapy and inhaled corticosteroids vary so widely, it is difficult to determine cost
effectiveness. In the United States, however, estimates
suggest that the cost of 1 year of immunotherapy is the
same as or slightly higher than the cost of 1 year of
inhaled corticosteroids.
With regard to nonspecific bronchial hyperreactivity as assessed by methacholine challenge, most studies
show no consistent change, and all multiallergen
immunotherapy studies have been negative. Responses
seen with immunotherapy are comparable to those
seen with moderate doses of inhaled corticosteroids.
The effects of both therapies on bronchial hyperreactivity are very small relative to the gap between asthmatic and normal subjects. Furthermore, no evidence
has demonstrated that immunotherapy produces permanent changes in airway hyperreactivity. The potential unique benefit of immunotherapy regarding
remission rates requires further study.
Groups that appear to derive the most benefit from
immunotherapy include children, patients with mild
asthma, and individuals with restricted sensitivities (ie,
monosensitized). The most positive immunotherapy
studies reported over the past decade were conducted
in monosensitized subjects. Most immunotherapy in
the United States, however, is administered to patients
who are polysensitized.
Although immunotherapy is not appropriate for
patients with moderate or severe persistent asthma
S524
who are already taking inhaled corticosteroids, it
appears to hold promise in preventing disease progression in patients with early and mild asthma. Efforts to
reduce the risk of systemic reactions, including death,
are still needed.
REFERENCES
1. Abramson M, Puy R, Weiner J. Immunotherapy in asthma: an
updated systematic review. Allergy. 1999;54(10):1022-1041.
2. Olsen OT, Larsen KR, Jacobsan L, Svendsen UG. A 1-year,
placebo-controlled, double-blind house-dust-mite immunotherapy study in asthmatic adults. Allergy. 1997;52(8):853-859.
3. Des Roches A, Paradis L, Menardo JL, Bouges S, Daures JP,
Bousquet J. Immunotherapy with a standardized
Dermatophagoides pteronyssinus extract. VI. Specific
immunotherapy prevents the onset of new sensitizations in
children. J Allergy Clin Immunol. 1997;99(4):450-453.
4. Moller C, Dreborg S, Ferdousi HA, et al. Pollen
immunotherapy reduces the development of asthma in children with seasonal rhinoconjunctivitis (the PAT-study).
J Allergy Clin Immunol. 2002;109(2):251-256.
5. Johnstone DB, Dutton A. The value of hyposensitization therapy for bronchial asthma in children: a 14-year study.
Pediatrics. 1968;42(5):793-802.
6. Shaikh WA. Immunotherapy vs inhaled budesonide in
bronchial asthma: an open, parallel, comparative trial.
Clin Exp Allergy. 1997;27(11):1279-1284.
7. Creticos PS, Reed CE, Norman PS, et al. Ragweed
immunotherapy in adult asthma. N Engl J Med.
1996;334(8):501-506.
8. Calpin C, Macarthur C, Stephens D, Feldman W, Parkin
PC. Effectiveness of prophylactic inhaled steroids in childhood asthma: a systemic review of the literature. J Allergy
Clin Immunol. 1997;100(4):452-457.
9. Adkinson NF Jr, Eggleston PA, Eney D, et al. A controlled
trial of immunotherapy for asthma in allergic children.
N Engl J Med. 1997;336(5):324-331.
10. Bousquet J, Hejjaoui A, Dhivert H, Clauzel AM, Michel FB.
Immunotherapy with a standardized Dermatophagoides
pteronyssinus extract. Systemic reactions during the rush protocol in patients suffering from asthma. J Allergy Clin
Immunol. 1989;83(4):797-802.
Vol. 4 (7A)
July 2004
DEBATE
KILL THE CAT, OR BUY ONE?
Based on presentations by Adnan Custovic, MD,* and Thomas Platts-Mills, MD
he role of cats and other fur-bearing pets
on allergies and asthma is now a controversial topic. As such, it has engendered
numerous discussions, articles, and debates,
as well as a host of questions that go beyond
a recommendation to kill the cat or buy one.
For example, do pets exacerbate allergies and/or
increase the risk for asthma? Is the prevalence of pet ownership in a community related to the prevalence of allergy and asthma in that community? Does having a pet in
childhood promote or protect against the development
of asthma in adulthood? Is there a dose-response relationship between cat allergen exposure and sensitization
rates? Are avoidance measures effective?
between community prevalence of cat ownership and
community prevalence of respiratory symptoms and
asthma. It has also been shown that the chances of
being sensitized in adulthood increase with the duration of exposure to cats in the home during childhood.
Other studies have shown that cat ownership in
childhood is associated with more asthma in sensitized
adults who grew up in communities with a low frequency of cat ownership, but not in communities with
a high proportion of cat ownership. The relationship
between cat ownership and the development of allergic disease differs between different areas and age
groups, and is additionally influenced by the family
history of allergy.
KILL THE CAT
BUY A CAT
There is considerable evidence in support of eliminating cat exposure, in particular as a part of the management of cat-allergic patients. Studies have shown
that sensitization to cat allergen is an important risk
factor for asthma, and that commonly used avoidance
measures, such as high-efficiency particulate arrest air
cleaners, high-filtration vacuum cleaners, and washing
the cat, are ineffective in reducing the amount of
inhaled cat allergen (vacuum cleaners may actually
increase it). Thus, for cat-allergic cat owners who experience symptoms upon exposure, the only solution is
to remove the cat from the home.
The relationship between cat ownership and the
development of allergy and asthma is much more
complex. However, a number of studies have shown
that owning a cat is a significant risk for sensitization
to cat, and that there is a significant correlation
There is now evidence that increasing exposure to
cat allergens, ie, a cat in the home, does not increase
either the prevalence of sensitization or the risk of
asthma.1 The reason(s) for these observations are not
understood. Do cats in the environment promote
exposure to bacteria or to bacterial products that alter
the immune system towards a low allergy phenotype
(hygiene hypothesis), or do cat antigens promote a
specific form of immune tolerance? In most recent
studies, the presence of cats is not associated with
increased airborne endotoxin in a house; therefore, the
second possibility appears more plausible.
It is quite possible that some allergens are created
more equal than others and this may have extensive
biological and clinical implications. The early forms of
the hygiene hypothesis predicted that nonallergic individuals would have a Th1 immune response to allergens. However, both serological and T-cell results
suggest that the tolerant response to cat allergens has
the features of a modified Th2 response.2,3 This may
*University of Manchester, Manchester, United Kingdom;
of Virginia Medical Center, Charlottesville, Virginia
University
Advanced Studies in Medicine
S525
DEBATE
not be the case with other allergens. The problem with
these data is that they do not provide any information
on what will happen to a particular individual. Even if
buying 2 cats would be good advice for the average
allergic person, it could still be very bad advice for a
sizeable minority.
(including cat) may still need to be recommended in
highly atopic individuals. More data will be hopefully
available in the near future to clarify this matter.
RECOMMENDATIONS
1. Ownby D, Johnson C, Peterson E. Exposure to dogs and
cats in the first year of life and risk of allergic sensitization
at 6 to 7 years of age. JAMA. 2002;288(8):963-972.
2. Platts-Mills T, Vaughan J, Squillace S, Woodfolk J, Sporik R.
Sensitization, asthma, and a modified Th2 response in children exposed to cat allergen: a population-based cross-sectional study. Lancet. 2001;357(9258):752-756
3. Reefer AJ, Carneiro RM, Custis NJ, et al. A role for IL-10mediated HLA-DR7-restricted T cell-dependent events in
development of the modified Th2 response to cat allergen.
J Immunol. 2004;172(5):2763-2772
Before making a recommendation to kill the cat
or buy one, physicians should carefully assess all causes of all allergic/asthmatic symptoms, the level of allergen exposure, the presence of other allergic conditions
such as allergic dermatitis and the propensity for allergy (family history). At this point, allergen avoidance
S526
REFERENCES
Vol. 4 (7A)
July 2004
POSTER PRESENTATIONS
SELECTED ORAL AND POSTER PRESENTATIONS
The following are based on oral and poster presentations from the 2003 World Allergy Congress,
held September 7-12, 2003, in Vancouver, British Columbia.
BENEFIT OF MONTELUKAST FOR ASTHMA IN PATIENTS
WITH BOTH ASTHMA AND ALLERGIC RHINITIS: A POSTHOC ANALYSIS FROM THE COMPACT TRIAL
Based on an oral presentation by Price DB,* Swern AS,
Tozzi CA, Phillip G, Polos P, Yu Q
*General Practice and Primary Care, University of
Aberdeen, Aberdeen, Scotland; Merck & Co, Inc, Rahway,
New Jersey
A post-hoc analysis of the multicenter Clinical
Observation of Montelukast as a Partner Agent for
Complementary Therapy (COMPACT) trial has found
that adding montelukast to budesonide is superior to
doubling the budesonide dose in improving morning
peak flow in the subgroup of asthma patients with
concomitant allergic rhinitis. The initial COMPACT
study demonstrated that adding montelukast to budesonide was at least as effective as doubling the budesonide dose in improving morning peak flow in
patients with asthma.1
The COMPACT trial included 889 patients
between 15 and 70 years of age with chronic
asthma for 1 year or longer who were not optimally controlled (as judged by an investigator) despite
the use of inhaled corticosteroids (ie, 600 g to
1200 g daily of budesonide or equivalent) for at
least 12 weeks. All had a minimal level of daytime
symptoms and beta-agonist use prior to randomization. After a 4-week, single-blind, run-in phase
during which all patients received budesonide 400
g twice daily, patients were randomized in double-blind fashion to receive montelukast 10 mg
once daily plus budesonide 400 g twice daily
(n = 448) or budesonide 800 g twice daily
(n = 441) for 12 weeks.
Advanced Studies in Medicine
In this post-hoc analysis, the effect of montelukast
plus budesonide versus double-dose budesonide was
compared in the subgroup of patients with concomitant allergic rhinitis, defined by both a positive patient
history and a confirmed physician diagnosis.
Reasons for pursuing this line of investigation include
the following: rhinitis occurs in more than 75% of
patients with allergic asthma; the same triggers (ie,
allergens) can cause rhinitis and asthma; rhinitis can
be a risk factor for asthma exacerbations; and upper
and lower airways share a common and probably
interconnected inflammatory process, as evidenced
by common inflammatory cells and mediators and the
fact that nasal challenge leads to bronchial inflammation and vice versa.2 Moreover, optimal management of rhinitis may be beneficial in managing
coexistent asthma, and montelukast, which is
approved for the treatment of asthma, has recently
been approved for the treatment of allergic rhinitis in
several countries, including the United States.
Overall, 410 patients in the COMPACT trial with
asthma had concomitant allergic rhinitis (defined by
having both a positive patient history of rhinitis and a
confirmed physician diagnosis), whereas 479 had
asthma without both a patient history and physicianconfirmed allergic rhinitis. Of the 448 patients randomized to montelukast plus budesonide, 216 had
asthma and concomitant allergic rhinitis; 33 were
using rhinitis medications, such as intranasal steroids,
antihistamines, or other rhinitis treatments, prior to randomization. Of the 441 patients randomized to double-dose budesonide, 184 had asthma with
concomitant allergic rhinitis; 23 were using rhinitis
medications prior to randomization.
At the end of the 12-week, double-blind treatment
phase, there were increases in morning peak flow
S527
POSTERS
values in patients randomized to montelukast plus
budesonide of 8.6% in the total group and 9.2% in
those with asthma and allergic rhinitis; these values
were noted versus increases in patients randomized
to double-dose budesonide of 7.7% in the total group
and 6.0% in those with asthma and allergic rhinitis.
The addition of montelukast to budesonide significantly improved morning peak flow in patients with
concomitant asthma and allergic rhinitis (P < .03 vs
double-dose budesonide). Furthermore, this additional treatment effect of montelukast was greatest in
patients taking rhinitis medication prior to randomization (n = 33). The treatment effect of doubling the
dose of budesonide among patients taking rhinitis
medication prior to randomization (n = 23) was less
than adding montelukast (increases in peak flow values of 12.1% for patients taking montelukast plus
budesonide vs 1.9% for those taking double-dose
budesonide; P < .02).
Results of this post-hoc analysis suggest the potential for additional treatment benefit with montelukast in
the large population of asthmatics who have concomitant allergic rhinitis. Further study, including
prospectively designed clinical trials, should be
undertaken to evaluate this hypothesis.
REFERENCES
1. Price DB, Hernandez D, Magyar P, et al. Randomised controlled trial of montelukast plus inhaled budesonide versus
double dose inhaled budesonide in adult patients with asthma. Thorax. 2003;58(3):211-216.
2. Togias A. Rhinitis and asthma: evidence for respiratory system
integration. J Allergy Clin Immunol. 2003;111(6):1171-1183.
DEPOSITION OF EXTRA-FINE HYDROFLUOROALKANEBECLOMETHASONE DIPROPIONATE INHALED VIA
PRESSURIZED METERED-DOSE INHALERSPACER IN
ASTHMATIC CHILDREN
Based on an oral presentation by Roller CM,* Owen
JL,* Troedson RG, LeSouef PN,* Devadason SG*
*University of Western Australia, Perth; Princess
Margaret Hospital for Children, Perth, Western Australia.
S528
Using gamma scintigraphy, a team of Australian
investigators has demonstrated that inhalation of an
extra-fine aerosol reformulation of beclomethasone
dipropionate (smaller particles result by mixing
beclomethasone with the hydrofluoroalkane propellant), delivered via metered-dose inhaler with an
attached detergent-coated holding chamber, significantly decreases unnecessary oropharyngeal and gastrointestinal drug deposition while maintaining high
levels of lung deposition in children with mild asthma.
Because airway targeting largely determines the
efficacy of inhaled corticosteroids, maximizing the
amount of drug that gets into the lung is a major factor in optimizing inhalation therapy in asthmatic children. The smaller the particle size that is delivered
by an aerosol device, such as an inhaler, the better
the deposition into the airways. This issue is even
more important in children because of their smaller
airway diameters. Holding chambers are widely
recommended for children in order to minimize
unnecessary oropharyngeal and gastrointestinal
drug deposition, which can contribute to both local
and systemic side effects.
To assess the total body deposition and distribution
of extra-fine beclomethasone in children, the investigators had 12 boys inhale 99 m technetium-radiolabeled
drug via metered-dose inhaler and spacer. Eight boys,
5 to 10 years of age, took 5 tidal breaths through the
spacer after each actuation, while 4 boys older than
10 years of age used a slow maximal inhalation followed by a 10-second breath hold. Simultaneous anterior and posterior planar gamma scintigraphic scans of
the lungs were recorded.
Mean lung deposition, expressed as an attenuation-corrected percentage of the exactuated dose,
was 35.1% in 4 boys between 5 and 7 years of
age, 47.5% in 4 boys between 8 and 10 years of
age, and 58.4% in 4 boys between 11 and 15
years of age. Gastrointestinal deposition was 25%,
10.3%, and 20.8%, respectively, in these same age
groups. The percentage of the drug remaining in the
spacer was 39.5%, 41.5%, and 20.3%, respectively. Lung deposition of extra-fine beclomethasone
increased significantly with age (P < .04).
The extra-fine particle metered-dose inhalerspacer combination gave more efficient delivery of steroid
by minimizing unwanted oropharyngeal and gastrointestinal drug deposition while maintaining high
drug deposition to the airways.
Vol. 4 (7A)
July 2004
POSTERS
A DOUBLE-BLIND, PLACEBO-CONTROLLED, RANDOMIZED,
CROSSOVER TRIAL OF MONTELUKAST IN ADULTS WITH
NASAL POLYPOSIS
Based on a poster presented by Keith P, Ferrie P, Conway
M, Wasserman S, Schmuck M, Denburg J
Department of Medicine, McMaster University,
Hamilton, Ontario, Canada
In this study of 23 adults with bilateral nasal
polyps, once-daily therapy with montelukast 10 mg
for 4 weeks was significantly superior to placebo in
improving global assessment of symptoms and quality of life. Active treatment also showed a trend
toward reduction of blood eosinophil counts. These
findings demonstrate that montelukast, a cysteinyl
leukotriene receptor antagonist with clinical benefits
for both asthma and allergic rhinitis, has beneficial
effects for nasal polyposis, a chronic eosinophilic
inflammatory condition.
Study subjects were randomized in this doubleblind, placebo-controlled, crossover study to compare
4 weeks of montelukast therapy with placebo. There
was a 4-week washout period between treatment periods. All subjects remained off intranasal steroids for at
least 4 weeks prior to treatment and throughout the
study. Global assessment of nasal polyp symptoms,
quality of life assessment specific to patients with nasal
polyps, and blood eosinophil counts were performed
at the completion of each treatment period.
Nasal polyp symptoms were assessed on a +3 to
3 scale, with +3 being equivalent to very much better, 0 to no better, and 3 to very much worse.
There was a significant improvement in symptom
score for montelukast treatment compared with placebo, with scores of 1.8 for active treatment versus 0.4
for placebo after the first treatment period, and 1.3
for active treatment versus 0.8 for placebo after the
second treatment period (P = .001).
Similarly, quality of life, as assessed by a diseasespecific questionnaire that employed a 7-point scale,
was significantly better with montelukast compared
with placebo, with an improvement of 0.6 for active
treatment versus 0.21 for placebo after the first treatment period, and 0.6 for active treatment versus 0.0
for placebo after the second treatment period (P =
.01). The investigators conclude that montelukast
treatment globally improves the symptoms of nasal
polyposis and health-related quality of life.
Advanced Studies in Medicine
SINGLE-INHALER THERAPY WITH
BUDESONIDE/FORMOTEROL
Three of the posters presented at the World
Allergy Organization Congress in Vancouver
described studies evaluating fixed and
adjustable dosing with budesonide/formoterol,
an inhaled glucocorticosteroid and a long-acting fast-onset beta-adrenergic agonist, in a single inhaler device. Because all 3 studies
evaluated the same combination, and because 2
of the studies used the same design and patient
population, they are presented here as a unit. The
first, by FitzGerald et al, assesses the effects on
asthma exacerbations. The second, by Sears et
al, examines the effects on symptom severity in the
same patient population. The third, by Aalbers et
al, compares adjustable versus fixed dosing with
budesonide/formoterol and adjustable dosing
with budesonide/formoterol versus fixed dosing
with salmeterol/fluticasone.
BUDESONIDE/FORMOTEROL ADJUSTABLE MAINTENANCE
DOSING REDUCES ASTHMA EXACERBATIONS COMPARED
WITH FIXED DOSING: A 5-MONTH STUDY IN CANADA
Based on a poster presented by FitzGerald JM,* Boulet
LP, McIvor A, Becker A, Sears MR,|| Ernst P, Georgijev
NS,# Lee J#
*University of British Columbia, Vancouver; Laval
University, Quebec City, Quebec; Dalhousie University,
Halifax, Nova Scotia; University of Manitoba, Winnipeg;
||McMaster University, Hamilton, Ontario; McGill
University, Montreal, Quebec; #AstraZeneca Canada Inc,
Canada
In this 5-month, randomized, open-label, parallelgroup study involving 995 patients with asthma at 95
healthcare and hospital centers in Canada,
adjustable maintenance dosing with budesonide/formoterol in a single inhaler was significantly more
effective than fixed dosing with the same agents in
reducing asthma exacerbations.
Patients were 12 years of age or older (mean,
40.6 years in the adjustable-dosing group and 42.8
years in the fixed-dosing group), met American
Thoracic Society criteria for asthma, had postbron-
S529
POSTERS
chodilator forced expiratory volume in 1 second (FEV1)
values above 70% of predicted, and had been taking
constant-dose inhaled corticosteroids for 6 months, with
the dose constant (250 g to 1000 g daily) for at least
30 days prior to study entry. Patients were considered
symptomatic if they used a short-acting beta2-agonist on
at least 2 occasions in the previous 7 days, had asthma symptoms on at least 2 days in the previous 7 days,
or had at least 2 nighttime awakenings due to asthma
in the previous 30 days.
After a 1-month run-in period during which all
patients received fixed-dose budesonide/formoterol
(80/4.5 g or 160/4.5 g, 2 inhalations twice
daily) to gain control of their asthma, patients were
randomized to receive an additional 5 months of
treatment with either fixed dosing or adjustable dosing. In the adjustable-dosing protocol, patients could
step down from 2 inhalations twice daily to 1 inhalation twice daily if patients felt their asthma was well
controlled in the previous 7 days, used reliever medication no more than 2 times during this period, and
had no nighttime awakenings due to asthma during
this interval. Patients could step up from 1 inhalation
twice daily to 4 inhalations twice daily if they had 2
consecutive nights with awakenings due to asthma or
2 consecutive days with morning peak flow values
that were below 85% of their mean baseline value,
or with the need to use reliever medications 3 or more
times daily. Patients could again step down after 7 or
14 days of step-up treatment, from 4 inhalations
twice daily to 1 inhalation twice daily, if they met all
of the step-down criteria presented above.
Exacerbation was defined as the need for additional inhaled and/or oral corticosteroids for asthma,
emergency department treatment due to asthma worsening, an asthma-related serious adverse event,
and/or withdrawal from the study due to the need for
additional asthma maintenance therapy. Severe exacerbation was defined as the need for oral corticosteroids due to asthma worsening, emergency
department treatment or hospitalization due to asthma
worsening, and/or an asthma-related serious
adverse event.
Patients in both study groups were well matched
regarding age, sex, mean postbronchodilator FEV1,
peak expiratory flow during the run-in period, inhaled
corticosteroid and long-acting beta2-agonist use at
study entry, and stratification by budesonide/formoterol dose during the fixed-dose run-in phase. Of
S530
those receiving the 80/4.5-g fixed dose during the
run-in phase, 140 were randomized to adjustable dosing and 129 to fixed dosing. Of those receiving the
160/4.5-g fixed dose during run-in, 359 were randomized to adjustable dosing and 367 to fixed dosing.
At the end of the 5-month randomization phase, significantly fewer patients in the adjustable-dosing group
experienced exacerbations, with the mean number of
exacerbations reduced by 57% compared with the
fixed-dosing group (P = .001). This was accomplished
at an overall lower dose of the budesonide/formoterol
inhaler (mean, 2.5 vs 3.9 inhalations daily) and cost
(mean savings, $141 Canadian) compared with fixed
dosing. In addition, fewer patients in the adjustable
group had 1 or more severe exacerbations, with the
mean number of such exacerbations reduced by 47%
compared with the fixed-dosing group. Time to first
exacerbation was significantly prolonged in the
adjustable-dosing group (P = .001) compared with the
fixed-dosing group.
The study demonstrates that adjustable dosing
improves patient outcomes in asthma, a disease with
fluctuating symptoms and periodic exacerbations,
and reduces the potential for periods of undertreatment or overtreatment associated with fixed dosing.
BUDESONIDE/FORMOTEROL ADJUSTABLE MAINTENANCE
DOSING EFFECTIVELY IMPROVES ASTHMA SYMPTOM
SEVERITY: A MULTICENTER CANADIAN STUDY
Based on a poster presented by Sears MR,* McIvor A,
Becker A, FitzGerald JM, Boulet LP,|| Ernst P, Georgijev
NS,# Lee J#
*McMaster University, Hamilton, Ontario; Dalhousie
University, Halifax, Nova Scotia; University of Manitoba,
Winnipeg; University of British Columbia, Vancouver;
||Laval University, Quebec City, Quebec; McGill University,
Montreal, Quebec; #AstraZeneca Canada Inc, Canada
Using the same study design, dosing regimens,
step-up and step-down criteria, and patient population as the study described by FitzGerald et al (see
above), this report showed that adjustable maintenance dosing with budesonide/formoterol in a single
Vol. 4 (7A)
July 2004
POSTERS
inhaler lessened or maintained control of asthma
symptoms in the vast majority of patients despite a
lower overall dose than fixed dosing (2.5 vs 3.9
inhalations daily).
In addition to being well matched regarding the
demographics and baseline characteristics described
in the report above, study participants were well
matched for symptom severity, with similar numbers in
both the adjustable-dosing and fixed-dosing groups
having severe persistent asthma (n = 9 and n = 7,
respectively), moderate persistent asthma (n = 210
and n = 221, respectively), mild persistent asthma
(n = 280 and n = 267, respectively), and mild intermittent asthma (n = 0 and n = 1, respectively).
Patients recorded nighttime awakenings due to
asthma as well as study medication and reliever medication (short-acting beta2-agonist) use on a daily
diary card. Asthma symptom severity was assessed in
each patient at visits 1 (at the beginning of the 1month run-in phase) and 5 (at the end of the 5-month
randomization phase) by a modification of the
National Heart, Lung, and Blood Institute Expert
Panel Report asthma severity classification. Adverse
events, serious adverse events, and study discontinuation due to adverse events were also reported.
At the end of the randomization phase, asthma
symptom severity was reduced or constant in 64% of
patients in the adjustable-dosing group and 34% of
patients in the fixed-dosing group. There was no significant difference between the groups in nighttime
awakening or reliever medication use during the
study. In addition, the percentage of patients with
moderate or mild persistent asthma decreased by
20% to 30%, and more than 50% of patients in both
groups had mild intermittent asthma, the lowest level
of severity, at studys end.
Regimens were well tolerated in both groups, with no
deaths and a low incidence of serious adverse events
(n = 5 in the adjustable-dosing group and n = 7 in the
fixed-dosing group), discontinuations due to adverse
events (n = 9 and n = 13, respectively), and discontinuations due to asthma exacerbation (n = 2 and n = 6,
respectively). The study investigators note that guided selfmanagement coupled with adjustable maintenance dosing, as shown in this study, enables patients to achieve
and maintain asthma control with a lower dose.
Advanced Studies in Medicine
ADJUSTABLE DOSING WITH BUDESONIDE/ FORMOTEROL
REDUCES THE RATE OF ASTHMA EXACERBATIONS
COMPARED WITH FIXED-DOSING SALMETEROL/
FLUTICASONE
Based on a poster presented by Aalbers R,* Backer V,
Kava TTK, Welte T, Omenaas ER,|| Bergqvist PBF,
Sandstrm T#
*Department of Pulmonology, Martini Hospital,
Groningen, The Netherlands; Respiratory Unit,
Department of Internal Medicine, Bispebjerg Hospital,
Copenhagen, Denmark; Department of Respiratory
Medicine, Central Hospital of Northern Karelia, Joensuu,
Finland; Department of Pneumology and Intensive Care
Medicine, University of Magdeburg, Magdeburg, Germany;
||Centre for Clinical Research, Haukeland University
Hospital, Bergen, Norway; AstraZeneca R&D Lund,
Lund, Sweden; #Department of Respiratory Medicine and
Allergy, University Hospital, Umea, Sweden
This 7-month study is the first to compare
adjustable maintenance dosing with budesonide/formoterol in a single inhaler with fixed dosing with the
same agents, as well as with fixed dosing with salmeterol/fluticasone. The investigators concluded that
adjustable maintenance dosing with budesonide/formoterol is more effective in reducing exacerbations
than fixed dosing with the same agents and more
effective in controlling the variability of asthma than
fixed dosing with salmeterol/fluticasone.
The randomized, 2-phase, multicenter study,
which involved a total of 658 patients and included
a 1-month double-blind phase and a 6-month openextension phase, was preceded by a 2-week run-in
phase during which patients continued their usual
inhaled corticosteroids and were then randomized to
adjustable-dose (n = 219) or fixed-dose budesonide/formoterol (n = 215) or fixed-dose salmeterol/fluticasone (50/250 g, 1 inhalation twice
daily; n = 224). During the 1-month double-blind
phase, in which patients who were randomized to
either scheme of budesonide/formoterol therapy
received the fixed dose (160/4.5 g, 2 inhalations
twice daily), the fixed-dose combinations were compared with each other.
At the end of the double-blind phase, patients initially randomized to adjustable dosing who met the criteria for dose adjustment stepped down to 1 inhalation
S531
POSTERS
twice daily; those who did not remained on 2 inhalations twice daily. Patients were eligible for a step-down
adjustment if, during the last 7 days of the double-blind
period, they had no nighttime awakenings due to asthma and if they used reliever medication no more than
once per day for not longer than 2 days.
During the open-extension phase, patients randomized to adjustable dosing with budesonide/formoterol could increase their dose temporarily, up to 4
inhalations twice daily, if their symptoms worsened
(ie, if they required reliever medication on 2 consecutive days on 3 or more occasions, of if they had
nighttime awakenings due to asthma on 2 consecutive days). All patients were permitted to use short-acting beta2-agonists (terbutaline or salbutamol) as
needed for symptom relief throughout the study.
Study participants were at least 12 years of age
(mean age, 47 years in the adjustable-dosing group
and 46 years in both fixed-dosing groups), with symptomatic asthma despite current medications, prebronchodilatory forced expiratory volume in 1 second
(FEV1) value 50% or more of predicted, and mean
peak expiratory flow between 50% or higher and 85%
of postbronchodilatory peak expiratory flow. All were
taking inhaled corticosteroids for at least 3 months
before study entry and at a constant daily dose of 500
g to 1200 g during the month before the run-in
phase. All had total daily symptom scores that
S532
were above 0 on at least 4 of the last 7 days of the
run-in period. Patients in each of the 3 treatment
groups were well matched regarding age, sex, mean
asthma symptom score, mean dose of inhaled corticosteroids at study entry, beta2-agonist use at study
entry, and mean FEV1.
During the study, exacerbationsdefined as oral
steroid treatment for at least 3 days and/or emergency
department visits with or without hospitalizations
were recorded. Asthma symptoms and reliever medication use were recorded on patient diary cards.
At the end of the study, there was a 40% reduction
in the rate of exacerbations in the group receiving
adjustable-dose budesonide/formoterol compared with
the group receiving fixed-dose salmeterol/fluticasone. The difference was even more impressive in the
last 100 days of treatment (4-fold decrease in the
number of exacerbations). There were also fewer
exacerbations, fewer hospitalizations and/or emergency department visits, and less use of extra inhaled
steroids in the group receiving adjustable-dose budesonide/formoterol than in both groups receiving fixeddose treatment.
Study drug use was somewhat higher in the
adjustable-dose group (average daily budesonide,
550 g) compared with the fixed-dose group (average
daily fluticasone, 500 g).
Vol. 4 (7A)
July 2004
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Favipravir PresentationDocument35 pagesFavipravir PresentationSanjay Sharma100% (5)
- Integrated Cath Lab Safety ChecklistDocument2 pagesIntegrated Cath Lab Safety ChecklistwenhalNo ratings yet
- IVTDocument6 pagesIVTpatzieNo ratings yet
- Gender Affirming Hormone Therapy GuidelinesDocument9 pagesGender Affirming Hormone Therapy GuidelinesAji VillanuevaNo ratings yet
- Drug Information Bulletin 52 05Document8 pagesDrug Information Bulletin 52 05amritaryaaligarghNo ratings yet
- Assignment 3 Design Personal Training ProgramDocument3 pagesAssignment 3 Design Personal Training ProgramEjhay TenderoNo ratings yet
- Anticoagulant Drugs (HEPARIN)Document1 pageAnticoagulant Drugs (HEPARIN)KyrrielJimenoCeladaNo ratings yet
- Counseling Tool For PharmacistsDocument3 pagesCounseling Tool For Pharmaciststl drNo ratings yet
- Gambro Phoenix SystemDocument2 pagesGambro Phoenix SystemGraham Thomas GipsonNo ratings yet
- GTU B Pharm Sem 6 Full SyllabusDocument11 pagesGTU B Pharm Sem 6 Full Syllabusjadavjatin2003No ratings yet
- Assisting Clients With Medication Workbook PHM2006WBK.10Document30 pagesAssisting Clients With Medication Workbook PHM2006WBK.10Zulfa Ramadhani100% (2)
- Ivfluid Glines AdultDocument2 pagesIvfluid Glines AdultDilan Galary100% (1)
- Aurobindo Pharma Receives USFDA Approval For Linezolid Injection (Company Update)Document2 pagesAurobindo Pharma Receives USFDA Approval For Linezolid Injection (Company Update)Shyam SunderNo ratings yet
- Pep 2021 - October QuestionsDocument4 pagesPep 2021 - October QuestionsCynthia ObiNo ratings yet
- Ect Consent FormDocument2 pagesEct Consent FormChalla Krishna VasanNo ratings yet
- Price List Last Update 4-10-2018Document2 pagesPrice List Last Update 4-10-2018mdgayas70No ratings yet
- Web Marketed 20220408Document494 pagesWeb Marketed 20220408Darwiche DarwicheNo ratings yet
- Check List First AidDocument6 pagesCheck List First AidNatasha VanyaNo ratings yet
- Pace University End of Life Simulation State 2 Pain ManagementDocument4 pagesPace University End of Life Simulation State 2 Pain Managementapi-414017065No ratings yet
- Chapter 1. Intro To DrugsDocument10 pagesChapter 1. Intro To DrugsLyka Milo AvilaNo ratings yet
- Drug-Induced Memory DisordersDocument1 pageDrug-Induced Memory DisordersNeeru KaulNo ratings yet
- Combination Drugs: Innovation in PharmacotherapyDocument6 pagesCombination Drugs: Innovation in PharmacotherapyNational Pharmaceutical CouncilNo ratings yet
- Homeopathy: An Introduction Key PointsDocument4 pagesHomeopathy: An Introduction Key PointsIrina DomentiNo ratings yet
- Lumbini Provincial Hospital: Department of PharmacyDocument2 pagesLumbini Provincial Hospital: Department of PharmacyImdadHussainOPositiveNo ratings yet
- Drug Utilization Pattern of Anti-Diabetic Drugs Among Diabetic Outpatients in A Tertiary Care HospitalDocument3 pagesDrug Utilization Pattern of Anti-Diabetic Drugs Among Diabetic Outpatients in A Tertiary Care HospitalTazkiyatan IsriaNo ratings yet
- Prescription Writing: Esha Ann FransonDocument9 pagesPrescription Writing: Esha Ann FransonAlosious JohnNo ratings yet
- Wound ShieldDocument2 pagesWound ShieldIsrael ExporterNo ratings yet
- Jufe 3 10.30Document38 pagesJufe 3 10.30LíaNo ratings yet
- Bali Spa Overseas Prices Update1Document5 pagesBali Spa Overseas Prices Update1Dian WijayantiNo ratings yet
- Schedule YDocument30 pagesSchedule Yapi-3810976100% (13)