Professional Documents
Culture Documents
A Cost Effect Analysis of Utilising Community Health Workers in The Management of Tuberculosis, Kenya
Uploaded by
IOSRjournalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Cost Effect Analysis of Utilising Community Health Workers in The Management of Tuberculosis, Kenya
Uploaded by
IOSRjournalCopyright:
Available Formats
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 6 Ver. III (Jun. 2015), PP 99-102
www.iosrjournals.org
A Cost Effect Analysis of Utilising Community Health Workers in
the Management of Tuberculosis, Kenya
Jane Rahedi Ongango1, Christina Mwachari1, Simon Karanja2
1
(Centre for Respiratory Disease Research, Kenya Medical Research Institute, Kenya)
(College of Health Sciences, Jomo Kenyatta University of Agriculture and Technology, Kenya)
Abstract
Introduction: Community Health Workers (CHWs) have been utilised for various primary health care
activities in different settings especially in developing countries. Usually when utilised in well defined terms,
they have a positive impact.
Objectives: The overall objective of this study was to undertake a cost effect analysis of utilising CHWs in
tuberculosis (TB) management.
Methods: A retrospective cohort study was conducted in selected health facilities using standard clinical
records for each TB patient registered for treatment between 2005 to 2011.
Results: The study assessed 2778 tuberculosis patients and among them 1499 (54%) utilized CHWs for their
TB treatment. The cost effect analysis revealed that the average cost per Disability Adjusted Life Year (DALY)
averted for treatment success was higher (184 US$) in the cohort that utilised CHWs compared to the nonutilising cohort (87 US$). Use of CHWs resulted in better treatment success rate (82.15%) compared to not
using at 72.25% (p-value <0.001). Utilising CHWs resulted in less DALYs (5688) from death compared to not
utilising CHWs (5725). Of the patients who died, a majority ( ) died within the first month of their treatment and
they were in the cohort that did not utilise CHWs.
Conclusion: The use of CHWs may be considered as a health and economic benefit because more life was
saved with a higher treatment success rate and there seemed to be death averted in the early months of TB
treatment.
Keywords - CHWs, Cost Effect Analysis, DALY, TB
I.
Introduction
Community Health Workers (CHWs) have been utilised for various primary health care activities in
different parts of the world [1,2,3]. It is generally felt that engagement of CHWs impacts positively on human
health via encouraging increased utilization of health care services and supporting preventive health
programmes [4,5]. In Kenya, the National TB Programme (NTP) provides free TB treatment that consists of a
standard 6 month regimen (2 months intensive phase of combined rifampicin, isoniazid, pyrazinamide, and
ethambutol (RHZE), followed by 4 months continuation phase of combined isoniazid and rifampicin (RH)) for
the new TB cases diagnosed that are sensitive to first line treatment. Retreatment TB cases are treated with a
standard 8-month regimen (2 months intensive phase of combined streptomycin, rifampicin, isoniazid,
pyrazinamide, and ethambutol (SRHZE), a continuation phase of 1 month (RHZE) followed by 5 months of
combined rifampicin, isoniazid and ethambutol (RHE).
A qualitative study has shown that TB patients on treatment, who receive the support and care of their
families were more likely to adhere to therapy and achieve cure [6]. More studies [7,8,9,10] have reported good
treatment outcomes when CHWs are involved in TB management. To measure the effectiveness of utilising the
CHWs in TB management, this study did a cost effect analysis.
II.
Methods
This was a retrospective cohort study that retrieved standard clinical records for each TB patient
registered for treatment between the years 2005 to 2011. The study was carried out in an urban and rural setting.
In each of these settings, two similar TB treatment health facilities were purposively selected: one engaged
CHWs for TB management and the other did not. One informal settlement in Nairobi, namely, Kawangare of
Dagoretti Division and Nyando District, Nyanza Province of Western Kenya represented the urban and rural setup respectively. The study was approved by the scientific and ethical review committees of KEMRI before
implementation. STATA version 12 was used for statistical analysis. The cost effectiveness of utilising the
CHWs was measured in terms of cost per DALY averted using the number of tuberculosis cases that were
successfully treated being considered as averted. To calculate the cost per DALY averted by successfully
treating these patients, the following assumptions were made; that the professional health care provided to these
DOI: 10.9790/0853-146399102
www.iosrjournals.org
99 | Page
A Cost Effect Analysis Of Utilising Community Health Workers In The Management Of
patients was equal in the 2 comparison groups, the only difference being the additional care provided by the
CHWs in the intervention group so that this would be an additional cost to be included in the calculation. The
additional cost of utilising the CHWs mainly considered the main expenditure that sustains the CHW work
which includes; incentive that CHWs receive on a monthly basis (US$25 per month for each CHW), 3 day
training received once per year at a cost of US$84 per training for each CHW and also the number of CHWs that
were utilised in the facilities yearly which was always about 5 for each facility throughout the year. The cost of
treating these patients with first line TB regimen for new and retreatment TB patients was also considered.
Based on the price list of the Global Drug Facility (GDF) a six-month course of treatment for a newly diagnosed
TB patient was approximately US$ 30, while an eight-month course of treatment for a retreatment patient was
estimated to be US$ 50 [11]. Infrastructure factors and other logistics were not considered in the calculations.
The calculation of DALY considered the disability weighting of TB (0.3) as provided by the Global burden
disease study 2010 [12] and time duration(in years) of treatment of TB which was 6 months for the new TB
patients and 8 months for the retreatment TB patients. The following formula was used with the assumption that
disability was only at that the time of TB treatment;
Disability Weighting of TB (0.3) X Time in years on TB treatment ( 6/12 or 8/12)
Each new TB patient had a DALY 0.15, while a retreatment patient had a DALY of 0.2.
In addition a comparison of mortality of TB patients in the 2 groups was also compared using DALY.
The total DALYs resulting from these deaths were calculated using the following recommended formula;
(Life expectancy years Age of person at death) X the weighting of Death.
Kenyas 2012 life expectancy at Birth of 63 years [13]was used with the disability weighting of death at 1.
III.
Results
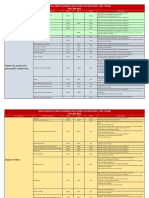
The study enrolled 2778 TB patients and among them 1499 (54%) utilized CHWs for their TB
treatment. The proportion of males and females was comparable in both the groups that utilized CHWs and that
which did not (Table 1). Age group distribution was similar in the 2 groups with mean age and standard
deviations falling within the same range. The urban setting in comparison with the rural setting contributed
significantly to a higher proportion (70%) of patients utilising the CHWs (p<0.001).
Of the enrolled 2,778 patients in the study, 2,669 (96%) had treatment outcomes documented. There
was a significant statistical difference in treatment success rate between the cohort that utilised CHWs and that
which did not utilise (82.15% vs 72.25% p-value <0.001), (Table 2).
Among the patients that were successfully treated there were 2 types of patients; the new TB patients
(n=1,749) who were having TB disease for the first time and retreatment TB patients (n=323) who previously
had TB (Table 3). Table 4 illustrates the cost of treating TB patients who had a treatment success outcome, the
total DALYs averted and the average cost per DALY averted in both the intervention and control group. The
average cost per DALY averted was higher (184 US$) in the cohort that utilised CHWs compared to the cohort
that did not utilise CHWs (87 US$). A total of 191 deaths were reported among the TB patients enrolled. Table
5 summarises the number of deaths and total DALYs resulting from them. Utilising CHWs resulted in less
DALYs (5688) from death compared to not utilising CHWs (5725).
A majority of patients died in the first 3 months of treatment in both the study cohorts (Fig 1). However
of concern was a majority (n=30) who died within the first month in the cohort that did not utilise CHWs.
p- value
<0.001
CHWs not utilized n=1279*
32.73 (mean) SD 14.24
0.563
660 (51.60)
619 (48.40)
<0.001
936 (73.18)
40 (3.13)
299 (23.38)
4 (0.31)
<0.001
1106 (86.47)
110 (8.60)
63 (4.93)
<0.001
287 (22.44)
992 (77.56)
<0.001
785 (61.38)
494 (38.62)
DOI: 10.9790/0853-146399102
Table 1: Characteristics of study participants
CHWs utilized n= 1499*
29.88 (mean) SD 13.39
Age
Gender
790 (52.70)
Male
709 (47.30)
Female
Disease Classification
287 (19.15)
Pulmonary Smear Positive (PSP)
839 (56.0)
Pulmonary Smear Negative (PSN)
371 (24.75)
Extra Pulmonary TB (EPTB)
2 (0.13)
Missing
Patient Classification
1128 (75.25)
New
329 (21.95)
Retreatment
42 (2.80)
Missing
Accepted HIV Screening
87 (5.80)
No
1412 (94.20)
Yes
Location
448 (29.89)
Rural
1051 (70.11)
Urban
Adherence to treatment
www.iosrjournals.org
100 | Page
A Cost Effect Analysis Of Utilising Community Health Workers In The Management Of
<0.001
343 (26.82)
875 (68.41)
61 (4.77)
215(14.34)
1237 (82.52)
47 (3.14)
No
Yes
Missing
*All data are n(%)
Table 2: Tuberculosis treatment outcomes and utilisation of CHWs
p-value
<0.001
CHWs not utilised n=1218*
880 (72.25)
104 (8.54)
7 (0.57)
156 (12.81)
71 (5.83)
CHWs utilised n=1451*
1192 (82.15)
87 (6)
2 (0.14)
86 (5.93)
84 (5.79)
TB Treatment Outcomes
Treatment Success
Died
Failure
Lost to Follow-up
Transfer Out
* All data are n(%)
Table 3: Tuberculosis Treatment Success by Type of Patient
Patients treated successfully
CHWs not utilised n=880*
803 (91)
77 (9)
CHWs utilised n=1192*
946 (79)
246 (21)
Type of Patient
New
Retreatment
* All data are n(%)
Table 4: Total number of patients treated successfully, total cost of treatment in US dollars, total DALYs
averted, and average cost per DALY averted for utilising CHWs and not utilising CHWs for tuberculosis
treatment
Average Cost per
DALY averted( US$)
184
87
weighted Total
DALYs averted
332
320
Total DALYs
averted
191
135
Total cost of
treatment
(US$)
61,211
27,940
Number of Patients
with a treatment
Success
1192
880
Intervention
Utilised CHWs
CHWs not utilised
Table 5: Number of deaths, total DALYs, by utilisation of CHWs and not utilising
CHWs for TB treatment
Weighted
DALYs
5688
5725
Total
Total DALYs
2588
3120
Number
Deaths
86
103
of
Intervention
Utilised CHWs
CHWs not utilised
Figure 1: Time of Death in months, of TB patients after initiating treatment
DOI: 10.9790/0853-146399102
www.iosrjournals.org
101 | Page
A Cost Effect Analysis Of Utilising Community Health Workers In The Management Of
IV.
Discussion
The average cost per DALY averted for treatment success was higher (184 US$) in the cohort that
utilised CHWs compared to the cohort that did not utilise CHWs (87 US$). Valuable resources were allocated
for the use of CHWs and this resulted in a better treatment success rate of 82.15% compared to 72.25% (p-value
<0.001). This may be considered as a health and economic benefit because life was saved by curing those who
had TB and a majority of them were in the productive age group of 25-34 years making up 38% of the cohort
that utilised CHWs. This finding is similar to other studies [14,15] that reported improved quality of life by
curing or controlling chronic disease.
Utilising CHWs resulted in less DALYs (5688) from death compared to not utilising CHWs (5725).
This finding re-emphasises the outcome of better treatment success rate that prevented the occurrence of death.
A majority of patients who died within the first month were in the cohort that did not utilise CHWs. The use of
CHWs seems to strongly avert death and this could greatly prevent death in the early months of TB treatment.
Using routine care data by this study strongly supports the intervention of utilising CHWs in the
management of TB treatment. The positive effect of utilising CHWs in a programmatic setting as found in this
study can be of value for areas outside the context of TB especially for chronic illnesses.
Cost effective analysis differs in various studies depending on the scope of cost put into the analysis
and also pricing differs in different set-ups. The analysis done in this study may have limited application to only
the local setting where the data was gathered from.
V.
Conclusion
Investment in the use of CHWs resulted in higher treatment success rate and more deaths were averted
an indication of health and economic gain.
Acknowledgements
We acknowledge the Director KEMRI, for authorising this study and permitting the publication of this
manuscript. We would like to thank the National TB Program (MOH) for facilitating the data collection process.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
[11].
[12].
[13].
[14].
[15].
Newell J, Baral S, Pande S, Bam D, Malla P, Family-member DOTS and community DOTS for tuberculosis control in Nepal:
cluster-randomised controlled trial. Lancet, 367, 2006, 903-909.
Brownstein J, Lee R, Dennison C, Hill M, Kim M, Levine D, Community Health Workers as Interventionists in the Prevention and
Control of Heart Disease and Stroke. Am J Prev Med, 29(5S1), 2005,128133.
Friedman I, In Community Based Health Worker (SAHR The SEED Trust, Health Programme, 2002).
Dick J, Murray E, Botha E, Operations Research Results; The Effectiveness of TB DOTS Supporters in South Africa. (Quality
Assurance Project. USAID, 2005).
Lehmann U, Friedman I, Sanders D, Review of the Utilisation and Effectiveness of Community health workers in Africa. A Joint
Learning Initiative. (Human Resources for Health and Development, Working Paper 4-1, 2004).
Macq J, Theobald S, Dick J, Dembele M, An exploration of the concept of directly observed treatment (DOT) for tuberculosis
patients: from a uniform to a customised approach. Int J Tuberc Lung Dis, 7,2003, 103-109.
Clarke M, Dick J, Zwarenstein M, Lombard C, Diwan V, Lay health worker with choice of DOT superior to standard TB care for
farm dwellers in South Africa: a cluster randomised control trial. Int J Tuberc Lung Dis., 9, 2005,673-679.
Menon A, Utilization of village health workers with in a primary health care programme in the Gambia. Journal of Tropical
Medicine and Hygiene, 94(4),1991, 268-271.
Nyonator F, Awoonor-Williams J, Phillips J, Jones T, Miller R, The Ghana Community Health Planning and Services Initiative:
Fostering Evidence-based Organizational Change and Development in a Resource-constrained Setting (Ghana: Population Council,
Policy Research Division, 2003).
Zvavamwe Z, Ehlers V, Experiences of a community-based tuberculosis treatment programme in Namibia: a comparative cohort
study. Int J Nurs Stud., Mar 46(3), 2009,302-9.
Stop TB Partnership, www.stoptb.org/gdf/drugsupply, 2014.
WHO, http://www.who.int/healthinfo/global_burden_disease/en/index.html. Retrieved April 15, 2010, from WebCite at
http://www.webcitation.org/5p118giwH.
CIA, World Fact Book as of February 21,2013.
Brown HS, Wilson KJ, Pagn JA, Arcari CM, Martinez M, Smith K, Reininger B, Cost-effectiveness analysis of a community
health worker intervention for low-income Hispanic adults with diabetes, Prev Chronic Dis. 2012;9:E140. doi:
10.5888/pcd9.120074.
Islam Md. A, Wakai S, Ishikawa NChowdhury AMR,Patrick Vaughan J, Cost-effectiveness of community health workers in
tuberculosis control in Bangladesh, Bulletin of the World Health Organization 2002;80:445-450
DOI: 10.9790/0853-146399102
www.iosrjournals.org
102 | Page
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Socio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanDocument7 pagesSocio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanInternational Organization of Scientific Research (IOSR)No ratings yet
- "I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweDocument5 pages"I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweInternational Organization of Scientific Research (IOSR)No ratings yet
- Assessment of The Implementation of Federal Character in Nigeria.Document5 pagesAssessment of The Implementation of Federal Character in Nigeria.International Organization of Scientific Research (IOSR)No ratings yet
- An Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyDocument14 pagesAn Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyInternational Organization of Scientific Research (IOSR)No ratings yet
- A Review of Rural Local Government System in Zimbabwe From 1980 To 2014Document15 pagesA Review of Rural Local Government System in Zimbabwe From 1980 To 2014International Organization of Scientific Research (IOSR)No ratings yet
- Relationship Between Social Support and Self-Esteem of Adolescent GirlsDocument5 pagesRelationship Between Social Support and Self-Esteem of Adolescent GirlsInternational Organization of Scientific Research (IOSR)No ratings yet
- A Proposed Framework On Working With Parents of Children With Special Needs in SingaporeDocument7 pagesA Proposed Framework On Working With Parents of Children With Special Needs in SingaporeInternational Organization of Scientific Research (IOSR)No ratings yet
- Attitude and Perceptions of University Students in Zimbabwe Towards HomosexualityDocument5 pagesAttitude and Perceptions of University Students in Zimbabwe Towards HomosexualityInternational Organization of Scientific Research (IOSR)No ratings yet
- The Role of Extrovert and Introvert Personality in Second Language AcquisitionDocument6 pagesThe Role of Extrovert and Introvert Personality in Second Language AcquisitionInternational Organization of Scientific Research (IOSR)No ratings yet
- The Impact of Technologies On Society: A ReviewDocument5 pagesThe Impact of Technologies On Society: A ReviewInternational Organization of Scientific Research (IOSR)100% (1)
- Comparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesDocument7 pagesComparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesInternational Organization of Scientific Research (IOSR)No ratings yet
- Investigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehDocument4 pagesInvestigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehInternational Organization of Scientific Research (IOSR)No ratings yet
- Importance of Mass Media in Communicating Health Messages: An AnalysisDocument6 pagesImportance of Mass Media in Communicating Health Messages: An AnalysisInternational Organization of Scientific Research (IOSR)No ratings yet
- Edward Albee and His Mother Characters: An Analysis of Selected PlaysDocument5 pagesEdward Albee and His Mother Characters: An Analysis of Selected PlaysInternational Organization of Scientific Research (IOSR)No ratings yet
- Human Rights and Dalits: Different Strands in The DiscourseDocument5 pagesHuman Rights and Dalits: Different Strands in The DiscourseInternational Organization of Scientific Research (IOSR)No ratings yet
- The Lute Against Doping in SportDocument5 pagesThe Lute Against Doping in SportInternational Organization of Scientific Research (IOSR)No ratings yet
- Beowulf: A Folktale and History of Anglo-Saxon Life and CivilizationDocument3 pagesBeowulf: A Folktale and History of Anglo-Saxon Life and CivilizationInternational Organization of Scientific Research (IOSR)No ratings yet
- Topic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshDocument7 pagesTopic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshInternational Organization of Scientific Research (IOSR)No ratings yet
- Role of Madarsa Education in Empowerment of Muslims in IndiaDocument6 pagesRole of Madarsa Education in Empowerment of Muslims in IndiaInternational Organization of Scientific Research (IOSR)No ratings yet
- Classical Malay's Anthropomorphemic Metaphors in Essay of Hikajat AbdullahDocument9 pagesClassical Malay's Anthropomorphemic Metaphors in Essay of Hikajat AbdullahInternational Organization of Scientific Research (IOSR)No ratings yet
- An Exploration On The Relationship Among Learners' Autonomy, Language Learning Strategies and Big-Five Personality TraitsDocument6 pagesAn Exploration On The Relationship Among Learners' Autonomy, Language Learning Strategies and Big-Five Personality TraitsInternational Organization of Scientific Research (IOSR)No ratings yet
- Transforming People's Livelihoods Through Land Reform in A1 Resettlement Areas in Goromonzi District in ZimbabweDocument9 pagesTransforming People's Livelihoods Through Land Reform in A1 Resettlement Areas in Goromonzi District in ZimbabweInternational Organization of Scientific Research (IOSR)No ratings yet
- Kinesics, Haptics and Proxemics: Aspects of Non - Verbal CommunicationDocument6 pagesKinesics, Haptics and Proxemics: Aspects of Non - Verbal CommunicationInternational Organization of Scientific Research (IOSR)No ratings yet
- Women Empowerment Through Open and Distance Learning in ZimbabweDocument8 pagesWomen Empowerment Through Open and Distance Learning in ZimbabweInternational Organization of Scientific Research (IOSR)No ratings yet
- Motivational Factors Influencing Littering in Harare's Central Business District (CBD), ZimbabweDocument8 pagesMotivational Factors Influencing Littering in Harare's Central Business District (CBD), ZimbabweInternational Organization of Scientific Research (IOSR)No ratings yet
- Design Management, A Business Tools' Package of Corporate Organizations: Bangladesh ContextDocument6 pagesDesign Management, A Business Tools' Package of Corporate Organizations: Bangladesh ContextInternational Organization of Scientific Research (IOSR)No ratings yet
- Substance Use and Abuse Among Offenders Under Probation Supervision in Limuru Probation Station, KenyaDocument11 pagesSubstance Use and Abuse Among Offenders Under Probation Supervision in Limuru Probation Station, KenyaInternational Organization of Scientific Research (IOSR)No ratings yet
- Designing of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesDocument5 pagesDesigning of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesIOSRjournalNo ratings yet
- Micro Finance and Women - A Case Study of Villages Around Alibaug, District-Raigad, Maharashtra, IndiaDocument3 pagesMicro Finance and Women - A Case Study of Villages Around Alibaug, District-Raigad, Maharashtra, IndiaInternational Organization of Scientific Research (IOSR)No ratings yet
- A Study On The Television Programmes Popularity Among Chennai Urban WomenDocument7 pagesA Study On The Television Programmes Popularity Among Chennai Urban WomenInternational Organization of Scientific Research (IOSR)No ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Generic Run Report: Prehospital Patient Care ChartDocument2 pagesGeneric Run Report: Prehospital Patient Care ChartBCF PRODUCTIONNo ratings yet
- Ipratropium Salbutamol (DUAVENT)Document2 pagesIpratropium Salbutamol (DUAVENT)Kristine Young100% (2)
- Blood - Transfusion Guidelines in Rwanda - 2018 - Version 3 - Final PDFDocument58 pagesBlood - Transfusion Guidelines in Rwanda - 2018 - Version 3 - Final PDFShandy B100% (6)
- 5th Yr Gynec ExamDocument151 pages5th Yr Gynec ExamHIMANSHU GUPTANo ratings yet
- Renal Glucose Carrier LabDocument4 pagesRenal Glucose Carrier LabJuvy Anne LozanoNo ratings yet
- 2020NSDUHFFR1PDFW102121Document156 pages2020NSDUHFFR1PDFW102121bachillerataNo ratings yet
- Safety Behaviours: Human Factors For Pilots 2nd Edition: Resource Booklet 3 Human PerformanceDocument32 pagesSafety Behaviours: Human Factors For Pilots 2nd Edition: Resource Booklet 3 Human PerformanceSonya McSharkNo ratings yet
- New Concepts in Transcatheter Mitral Valve ReplacementDocument210 pagesNew Concepts in Transcatheter Mitral Valve ReplacementhanNo ratings yet
- Eapp Q4 M4Document12 pagesEapp Q4 M4Allen Benedict NatoNo ratings yet
- Geriatric PsychiatryDocument91 pagesGeriatric PsychiatryVipindeep SandhuNo ratings yet
- ფოლიუმის დეფიციტური ანემიაDocument14 pagesფოლიუმის დეფიციტური ანემიაoliko maglakvelidzeNo ratings yet
- Mse SivaDocument8 pagesMse Sivasivagiri.pNo ratings yet
- Lista de Dispositivos Medicos PrioritariosDocument20 pagesLista de Dispositivos Medicos PrioritariosEimyNo ratings yet
- Tetanus Symptoms, Causes, Treatment and PreventionDocument4 pagesTetanus Symptoms, Causes, Treatment and PreventionSneha SnehaNo ratings yet
- Heartbeats: Learning About The HeartDocument6 pagesHeartbeats: Learning About The HeartKush ThumarNo ratings yet
- Molar PregnancyDocument13 pagesMolar PregnancyShalynurNo ratings yet
- Environmental Studies ProjectDocument8 pagesEnvironmental Studies ProjectROYAL GAMER YTNo ratings yet
- Biobank Doggo - Purpose - Partnership - and - Possibilities - The - ImplemenDocument11 pagesBiobank Doggo - Purpose - Partnership - and - Possibilities - The - ImplemenTri4alNo ratings yet
- Mental Health and Self-Care ReflectionDocument2 pagesMental Health and Self-Care Reflectionapi-472652222No ratings yet
- The Outer Limits - 7x02 - Patient Zero - en PDFDocument51 pagesThe Outer Limits - 7x02 - Patient Zero - en PDFoic-ad-agNo ratings yet
- Psa Assignment-FinalDocument3 pagesPsa Assignment-Finalapi-519381955No ratings yet
- Factors Influencing The Use of E-CigarettesDocument96 pagesFactors Influencing The Use of E-Cigarettes1G - Kyle Kenjie DahiliNo ratings yet
- (CPG) Philippine Guidelines On Periodic Health Examination: Screening For Neoplastic DiseasesDocument194 pages(CPG) Philippine Guidelines On Periodic Health Examination: Screening For Neoplastic DiseasesBianca Watanabe - RatillaNo ratings yet
- Cardiac Case Study Homework Week 5Document4 pagesCardiac Case Study Homework Week 5Study AssistantNo ratings yet
- Emergency Disaster Nursing QuestionsDocument3 pagesEmergency Disaster Nursing QuestionsYvory Diane100% (3)
- Drug Study: Generic NameDocument9 pagesDrug Study: Generic NameAlyanna Alcazar CapateNo ratings yet
- UTS g7Document15 pagesUTS g7John Emerson MerelosNo ratings yet
- LDL particle size and inflammation key to heart disease riskDocument2 pagesLDL particle size and inflammation key to heart disease risksimasNo ratings yet
- HP A 19 COMP Lung Volume CapacitiesDocument5 pagesHP A 19 COMP Lung Volume CapacitiesDewiIntanP100% (1)
- Understanding the pathogenesis and progression of peri-implantitisDocument11 pagesUnderstanding the pathogenesis and progression of peri-implantitisMuhammad GhifariNo ratings yet