Professional Documents
Culture Documents
Cholecystitis: (Alterations in Metabolic and Endocrine Functions)
Uploaded by
Jorie RocoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cholecystitis: (Alterations in Metabolic and Endocrine Functions)
Uploaded by
Jorie RocoCopyright:
Available Formats
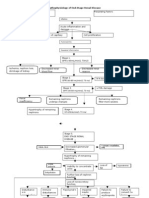
[Alterations in Metabolic and Endocrine Functions]
CHOLECYSTITIS
Precipitating factors:
Predisposing factor:
- Pregnancy
- Diabetes
- Tumor surrounding the Gallbladder
- Hyperlipidemia
- Losing weight rapidly and diet
- Obesity
- Gallstones
- Oral contraceptives
- Female (estrogen levels)
- Pregnancy
- Hormone therapy
- Family History
- Ethnicity
Decreased contractility of Bile Flow
Bile stasis
Contraction of substances present in bile
Precipitation of bile substances
Bile substances will increase in size
Stones migrate to gallbladder
Kinking/compression of common bile duct/pancreatic duct
Obstruction to gallbladder
Obstruction of flow of bile
Increase intraluminal pressure
Gallbladder distention
Stimulates smooth
muscle contraction
RUQ abdominal
pain
Increase tension
to duodenum
Pain radiates to
lower back
Presence of bile in the
circulation
Wall edema
Impaired Hepatic
uptake of bilirubin
Collection of soluble
bilirubin in the urine
No bile reaches the
GIT
Vascular compromise
Ischemia to Gallbladder
Cholesterol salts in
the skin
Jaundice
No bile in small intestine
for fat digestion
Escape of
bilirubin to GUT
Decreased
sterobilin
Presence of bile in
the urine
Emulsification
of fats
Dark yellow
urine
Nausea and
Vomiting
SOURCES:
Decrease bile in
the duodenum
Necrosis to Gallbladder
Invasion of bacteria
Realease of toxic metabolites into
Clay-colored
stool
Shock
Pulmonary Insufficiency
Acute renal failure
Dissemenated Intravascular
Coagulation
Intuit and Docstoc. (2014). Cholecystitis Pathophysiology. Retrieved March 2015, from
http://img.docstoccdn.com/thumb/orig/113462569.png.
Mayo Foundation for Medical Educationand Research. (2015). Cholecystitis. Retrieved March 2015, from
http://www.mayoclinic.org/diseases-conditions/cholecystitis/basics/symptoms/con-20034277.
Nursing Crib. (2015). Pathophysiology of Cholelithiasis/Cholecystitis. Retrieved March 2015, from http://nursing
crib.com/pathophysiology/pathophysiology-of-cholelithiasischoleccsytitis/.
1
[Alterations in Metabolic and Endocrine Functions]
CHOLECYSTITIS
Cholecystitis is inflammation of the gallbladder, a small organ near the liver that plays a
part in digesting food. It is usually associated with cholelithiasis. Normally, fluid called bile
passes out of the gallbladder on its way to the small intestine. If the flow of bile is blocked, it
builds up inside the gallbladder, causing swelling, pain, and possible infection. Cholecystitis
may be acute or chronic. These conditions usually occur together.[1]
ETIOLOGY
Cholecystitis occurs when gallbladder becomes inflamed. Gallbladder inflammation can
be caused by gallstones, the result of hard particles that develop in gallbladder from imbalances
in the substances in bile such as cholesterol and bile salts. Gallstones can block the cystic duct,
the tube through which bile flows when it leaves the gallbladder, causing the bile to build up and
resulting in inflammation. Also, it is caused by tumor that may prevent bile from draining out of
the gallbladder properly, causing the buildup that can lead to cholecystitis. Kinking or scarring of
the bile ducts can cause also blockages that lead to cholecystitis.[2]
Risk factors in developing cholecystitis include increasing age, female gender, obesity
and rapid weight loss, using hormonal therapies, pregnancy, having diabetes and being Native
American or Hispanic.[3]
Sometimes the bile duct becomes blocked temporarily. When this occurs repeatedly, it
can lead to chronic cholecystitis. This is swelling and irritation that continues over time.
Eventually, the gallbladder becomes thick and hard. It also does not store and release bile as
well.[4]
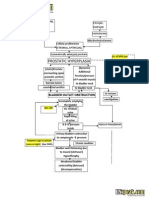
PATHOPHYSIOLOGY
The initial event in acute cholecystitis (ACC) is believed to be obstruction to
gallbladder drainage. This causes an increase in intraluminal pressure, gallbladder distention, and
wall edema that may progress to venous and lymphatic obstruction, ischemia, and necrosis. A
number of potential mediators have been identified including cholesterol-supersaturated bile,
lysolecithin,phospholipase A, and prostaglandins. Enhanced production of prostaglandins is
____________________________________________________________________________________________________________________
_
1
Mayo Clinic Health Letter-Online Edition. (2014, August 28). Disease and Conditions: Cholecsytitis. Retrieved March 2015,
from http://www.mayoclinic.org/diseases-conditions/cholecystitis/basics/symptoms/con-20034277.
Mayo Foundation for Medical Educationand Research. (2015). Cholecystitis. Retrieved March 2015, from
http://www.mayoclinic.org/diseases-conditions/cholecystitis/basics/symptoms/con-20034277.
Udan, J. Medical Surgical: Concepts and Clinical Application (First Edition). Philippines: Guiani Prints House. (2002).
Black, J.M., & Hawks, J.H. Medical-Surgical Nursing Clinical Management for Positive Outcomes. Philippines: Elsevier.
2
[Alterations in Metabolic and Endocrine Functions]
(2005).
believed to play a key role in mediating inflammation, and agents that reduce prostaglandin
production have been shown to block the inflammatory response and reduce the pain of
cholecystitis. Bile is sterile in the early stages of acute cholecystitis and infection is believed to
be a secondary event. Indeed, although ACC is often considered an infection. The organisms
most commonly cultured are enteric bacteria including Escherichia coli, Klebsiella, and
Enterococcus.[1]
Cholelithiasis develops when the balance that keeps cholesterol, bile salts, and calcium
in solution is altered so that precipitation of these substances occurs. Conditions that upset this
balance include infection and disturbances in the metabolism of cholesterol. It is known that in
patients with cholethiasis, the bile secreted by the liver is supersaturated with cholesterol. The
bile in the gallbladder also becomes supersaturated with cholesterol. When bile is supersaturated
with cholesterol, precipitation of cholesterol will occur.
CLINICAL MANIFESTATIONS
The main symptom is pain in the upper right side or upper middle of your belly that
usually lasts at least 30 minutes. You may feel:
Sharp, cramping, or dull pain
Steady pain
Pain that spreads to your back or below your right shoulder blade
Other symptoms that may occur include:
Clay-colored stools, steatorrhea
Fever
Nausea and vomiting
Yellowing of skin and whites of the eyes (jaundice)
Chronic diarrhea (4 - 10 bowel movements every day for at least 3 months) may be a
common symptom of gallbladder dysfunction.[3]
Jaclyn Mae T. Alviola, RN
____________________________________________________________________________________________________________________
_
1
Mayo Clinic Health Letter-Online Edition. (2014, August 28). Disease and Conditions: Cholecsytitis. Retrieved March 2015,
from http://www.mayoclinic.org/diseases-conditions/cholecystitis/basics/symptoms/con-20034277.
Black, J.M., & Hawks, J.H. Medical-Surgical Nursing Clinical Management for Positive Outcomes. Philippines: Elsevier.
(2005).
3
[Alterations in Metabolic and Endocrine Functions]
3
Lewis, S. and et.al. Medical Surgical Nursing: Assessment and Management of Clinical Problems. Singapore: Mosby Elsevier
Inc. . (2008).
You might also like
- Case Study CholecystitisDocument27 pagesCase Study CholecystitisBandana RajpootNo ratings yet
- Cholecystitis IntroductionDocument4 pagesCholecystitis IntroductionJechelle Ann Pabustan Martin-BoniquitNo ratings yet
- CholelithiasisDocument3 pagesCholelithiasisMIlanSagittarius0% (1)
- CHOLELITHIASISSDocument29 pagesCHOLELITHIASISSAngelica Mercado SirotNo ratings yet
- Pathophysiology OsteosarcomaDocument2 pagesPathophysiology OsteosarcomaVernadeth Dumagat50% (2)
- PAtho CholecystitisDocument2 pagesPAtho CholecystitisJanry-Mae Escobar TumanengNo ratings yet
- Cholecystitis Case StudyDocument7 pagesCholecystitis Case StudyElle MongeNo ratings yet
- Pathophysiology of Adenocarcinoma, Moderately DifferentiatedDocument5 pagesPathophysiology of Adenocarcinoma, Moderately Differentiatedmacel sibayan33% (3)
- NCP OsteosarcomaDocument6 pagesNCP OsteosarcomaNiksNo ratings yet
- Pathophysiology: Cholecystitis Non Modifiable Factors Modifiable FactorsDocument4 pagesPathophysiology: Cholecystitis Non Modifiable Factors Modifiable FactorsYuyu Tulawie100% (1)
- Case Presentation of Cellulitis & Urinary Tract Infection (Suspect)Document24 pagesCase Presentation of Cellulitis & Urinary Tract Infection (Suspect)tiban_0750% (2)
- A Case Study 0n Ascending CholangitisDocument41 pagesA Case Study 0n Ascending Cholangitisneil garcia100% (4)
- CHOLECYSTITISDocument13 pagesCHOLECYSTITISdolly joy100% (1)
- CholelithiasisDocument6 pagesCholelithiasismarkzamNo ratings yet
- Diverticular DiseaseDocument8 pagesDiverticular Diseasenurse_enzo100% (1)
- 2 Goso ReviseDocument1 page2 Goso ReviseAngelika Mae MiraNo ratings yet
- Gordon'S Functional Health Pattern Prior To Admission During Hospitalization Health Perception and Health ManagementDocument3 pagesGordon'S Functional Health Pattern Prior To Admission During Hospitalization Health Perception and Health ManagementJordz PlaciNo ratings yet
- Pernicious AnemiaDocument7 pagesPernicious AnemiaTracy PearlNo ratings yet
- Myoma PathoDocument3 pagesMyoma PathoJan Michael Artiaga100% (1)
- DiverticulitisDocument2 pagesDiverticulitisyapyapvinx50% (2)
- Pathophysiology (Client Base) :: Predisposing Factors: Precipitating FactorsDocument1 pagePathophysiology (Client Base) :: Predisposing Factors: Precipitating Factorsleslie_macasaetNo ratings yet
- Pathophysiology of Alzheimers DiseaseDocument2 pagesPathophysiology of Alzheimers DiseaseJaysellePuguonTabijeNo ratings yet
- Pathophysiology of GastritisDocument2 pagesPathophysiology of GastritisFlorsean Mae Sala80% (5)
- Osteomyelitis HandoutDocument4 pagesOsteomyelitis HandoutJazzmin Angel ComalingNo ratings yet
- Patho DiagramDocument4 pagesPatho DiagramNielArmstrongNo ratings yet
- Pathophysiology of Osteomyelitis DiagramDocument1 pagePathophysiology of Osteomyelitis DiagramKim Enrico JumarangNo ratings yet
- Pathophysiology of OsteomyelitisDocument3 pagesPathophysiology of OsteomyelitisJhon Jerric Pante Aguinaldo100% (1)
- CiprobayDocument2 pagesCiprobayianecunar100% (1)
- Chronic PyelonephritisDocument5 pagesChronic PyelonephritisIsak ShatikaNo ratings yet
- BUERGER's DiseaseDocument2 pagesBUERGER's DiseasechemnikoNo ratings yet
- Paget Disease of BoneDocument17 pagesPaget Disease of Boneraghunandhakumar100% (1)
- PYOMYOSITISDocument6 pagesPYOMYOSITISChristine CoridoNo ratings yet
- Predisposing Factors Age Diet Dehydration Precipitating Factors Family or Personal History Digestive Diseases and SurgeryDocument2 pagesPredisposing Factors Age Diet Dehydration Precipitating Factors Family or Personal History Digestive Diseases and SurgeryChloé Jane HilarioNo ratings yet
- Draft Case Study CholedocholithiasisDocument15 pagesDraft Case Study Choledocholithiasisapi-3828211100% (5)
- Pathophysiology of Gastric Cancer Precipitating Factors: - Predisposing FactorsDocument3 pagesPathophysiology of Gastric Cancer Precipitating Factors: - Predisposing FactorsJu Lie AnnNo ratings yet
- EsrdDocument3 pagesEsrdRonald Lavada RN100% (1)
- CellulitisDocument16 pagesCellulitisMhOt AmAd100% (1)
- Leukemias: Care SettingDocument11 pagesLeukemias: Care SettingTinNo ratings yet
- Benign Prostatic Hyperplasia - BPH - Pathophysiology - Schematic DiagramDocument2 pagesBenign Prostatic Hyperplasia - BPH - Pathophysiology - Schematic DiagramTrixie Arabit100% (3)
- Schematic Diagram of Alcoholic CirrhosisDocument2 pagesSchematic Diagram of Alcoholic CirrhosisCyrus De Asis0% (1)
- Gastrectomy Post OpDocument5 pagesGastrectomy Post Opfeirri100% (4)
- Mae LNMDocument9 pagesMae LNMCristina L. Jayson33% (3)
- DB13 - Pathophysiology of AtherosclerosisDocument2 pagesDB13 - Pathophysiology of Atherosclerosisi_vhie03No ratings yet
- TahbsoDocument4 pagesTahbsomichZ_13No ratings yet
- Acute and Chronic GastritisDocument17 pagesAcute and Chronic GastritisIndah Nur PratiwiNo ratings yet
- TahbsoDocument77 pagesTahbsoCzarina Charmaine DiwaNo ratings yet
- Case Study CholelithiasisDocument14 pagesCase Study Cholelithiasisb_faye20No ratings yet
- Anatomy and Physiology of The GallbladderDocument1 pageAnatomy and Physiology of The GallbladderRojanisa Baculi RomathoNo ratings yet
- Buergers Power PointDocument16 pagesBuergers Power PointYan VencerNo ratings yet
- A Case Study On CholedocholithiasisDocument81 pagesA Case Study On Choledocholithiasischristelle6cadiente67% (9)
- Path o PhysiologyDocument9 pagesPath o PhysiologyKyle Ü D. CunanersNo ratings yet
- The Pathophysiology of LabyrinthitisDocument2 pagesThe Pathophysiology of LabyrinthitisSurya Michael ChanceNo ratings yet
- Pathophysiology of PudDocument3 pagesPathophysiology of PudIrene InsoNo ratings yet
- AppendicitisDocument8 pagesAppendicitisAndini YusniaNo ratings yet
- Case Study of AmoebiasisDocument7 pagesCase Study of Amoebiasisbuzz Q75% (4)
- Cholecystitis Full With EditDocument43 pagesCholecystitis Full With Editmustafalotfy01No ratings yet
- Cholelithiasis Brief DiscussionDocument8 pagesCholelithiasis Brief Discussionriel100% (6)
- Cholelithiasis RLDocument29 pagesCholelithiasis RLPrincess Joanna Marie B DelfinoNo ratings yet
- Chole Cyst IsDocument8 pagesChole Cyst IsJose Adrian Mendoza OrejuelaNo ratings yet
- CholecystitisDocument20 pagesCholecystitisMYKRISTIE JHO MENDEZNo ratings yet
- Nursing TheoriesDocument51 pagesNursing TheoriesJorie RocoNo ratings yet
- Hypos TestingDocument192 pagesHypos TestingJorie RocoNo ratings yet
- Transpersonal CaringDocument46 pagesTranspersonal CaringJorie Roco100% (1)
- Critical Thinking PointersDocument40 pagesCritical Thinking PointersJorie RocoNo ratings yet
- Theoretical Foundation in NursingDocument24 pagesTheoretical Foundation in NursingJorie RocoNo ratings yet
- Measures of SkewnessDocument15 pagesMeasures of SkewnessJorie Roco100% (1)
- Measures of LocationDocument9 pagesMeasures of LocationJorie RocoNo ratings yet
- Advanced Statistics ReviewDocument21 pagesAdvanced Statistics ReviewJorie RocoNo ratings yet
- Kinds of Data PresentationDocument18 pagesKinds of Data PresentationJorie RocoNo ratings yet
- StaffingDocument50 pagesStaffingPradeep PandaNo ratings yet
- Liver Cirrhosis: (Alterations in Metabolic and Endocrine Functions)Document8 pagesLiver Cirrhosis: (Alterations in Metabolic and Endocrine Functions)Jorie RocoNo ratings yet
- Liver Cirrhosis: Precipitating Factors: Predisposing FactorDocument22 pagesLiver Cirrhosis: Precipitating Factors: Predisposing FactorJorie RocoNo ratings yet
- Saint Paul University Dumaguete Graduate School: Master of Science in NursingDocument5 pagesSaint Paul University Dumaguete Graduate School: Master of Science in NursingJorie RocoNo ratings yet
- Objectives For Hospital ExperienceDocument5 pagesObjectives For Hospital ExperienceJorie RocoNo ratings yet
- The Teacher and His Profession Written ReportDocument7 pagesThe Teacher and His Profession Written ReportJorie RocoNo ratings yet
- Pancreatitis: (Alterations in Metabolic and Endocrine Functions)Document7 pagesPancreatitis: (Alterations in Metabolic and Endocrine Functions)Jorie Roco0% (1)
- Medical Surgical NursingDocument3 pagesMedical Surgical NursingJorie RocoNo ratings yet
- Transcultural NSG HX Theory Cultural AssstDocument73 pagesTranscultural NSG HX Theory Cultural AssstJorie RocoNo ratings yet
- Respiratory System and AnemiaDocument112 pagesRespiratory System and AnemiaJorie RocoNo ratings yet
- Transcultural NursingDocument32 pagesTranscultural NursingJorie RocoNo ratings yet
- Communication and CultureDocument14 pagesCommunication and CultureJorie RocoNo ratings yet
- Transcultural Nursing: Prepared By: Maria Angelica T. Fernandez, BSN-RNDocument28 pagesTranscultural Nursing: Prepared By: Maria Angelica T. Fernandez, BSN-RNJorie RocoNo ratings yet
- Food Poisoning OutlineDocument3 pagesFood Poisoning OutlinemshaschixoNo ratings yet
- IFA Sports Nutrition Certification Test Answer Form: Tester: Date: NameDocument8 pagesIFA Sports Nutrition Certification Test Answer Form: Tester: Date: NameSimbarashe MabambeNo ratings yet
- CoughDocument11 pagesCoughVenkatesan VidhyaNo ratings yet
- Case Presentation On Chronic Kidney Disease1Document18 pagesCase Presentation On Chronic Kidney Disease1d100% (1)
- Childhood Obesity 1 PPT PresentationDocument37 pagesChildhood Obesity 1 PPT Presentationapi-218840558No ratings yet
- Parasitic ArthropodsDocument3 pagesParasitic ArthropodsVicky V. HerpworldNo ratings yet
- Sample MCQ'SDocument4 pagesSample MCQ'SHerman SehmbiNo ratings yet
- SSC - CHSL (10+2) Model Paper 2 by EenaduDocument19 pagesSSC - CHSL (10+2) Model Paper 2 by EenaduMahendraKumarNo ratings yet
- SIP 2016 Abstract & Background Booklet V.6 PDFDocument187 pagesSIP 2016 Abstract & Background Booklet V.6 PDFJimboreanu György PaulaNo ratings yet
- Daftar Kunjungan Peserta SakitDocument11 pagesDaftar Kunjungan Peserta SakitMaya rahmayanaNo ratings yet
- Renal Diseases PathophysiologyDocument6 pagesRenal Diseases PathophysiologyBilly Gayados100% (1)
- N V Adj AdvDocument5 pagesN V Adj AdvAlaa BabikerNo ratings yet
- Hepatitis in ChildrenDocument2 pagesHepatitis in ChildrenShilpi SinghNo ratings yet
- Alpine Sandthorn Berry BookDocument61 pagesAlpine Sandthorn Berry BookVitoc DanNo ratings yet
- Unit 2 Biology and Geology 3rd ESODocument64 pagesUnit 2 Biology and Geology 3rd ESOPaulaNo ratings yet
- Uia 16 MCQ QUESTIONSDocument7 pagesUia 16 MCQ QUESTIONSsofian ashourNo ratings yet
- Ichthyosis Vulgaris Cured With HomoeopathyDocument8 pagesIchthyosis Vulgaris Cured With HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (2)
- Cefazolin (Drug Study)Document1 pageCefazolin (Drug Study)Valerie Villanueva0% (2)
- Dr. Raghu Prasada M S MBBS, MD Assistant Professor Dept. of Pharmacology Ssims & RCDocument27 pagesDr. Raghu Prasada M S MBBS, MD Assistant Professor Dept. of Pharmacology Ssims & RCNastase Daniela EcaterinaNo ratings yet
- Doh Updated Prog M-RDocument49 pagesDoh Updated Prog M-Rdeeday echavezNo ratings yet
- The 7 Biggest Diabetes LiesDocument31 pagesThe 7 Biggest Diabetes Liesramon_portillo_nd_64100% (1)
- Nursing Care Plan For Nausea and VomitingDocument3 pagesNursing Care Plan For Nausea and Vomitingsp0ngelual100% (5)
- The Pathogenesis and Pathophysiology of Type 1 and PDFDocument12 pagesThe Pathogenesis and Pathophysiology of Type 1 and PDFasmawatiNo ratings yet
- The Frontal Assessment Battery (FAB) Normative Value PDFDocument9 pagesThe Frontal Assessment Battery (FAB) Normative Value PDFIcaroNo ratings yet
- Sexually Transmitted DiseasesDocument5 pagesSexually Transmitted Diseasesgodiee77No ratings yet
- Ethnomedicinal Uses, Phytochemistry and Pharmacological Aspects of The Genus Premna: A ReviewDocument26 pagesEthnomedicinal Uses, Phytochemistry and Pharmacological Aspects of The Genus Premna: A ReviewDavids MarinNo ratings yet
- 12 Biology Notes Ch08 Human Health and DiseaseDocument11 pages12 Biology Notes Ch08 Human Health and Diseaserohit403No ratings yet
- Kotak Proposal Form (KPF) : For Office Use OnlyDocument8 pagesKotak Proposal Form (KPF) : For Office Use OnlyMoolam RaoNo ratings yet
- Global Development DelayDocument35 pagesGlobal Development DelayJOHN ALEC FORTONo ratings yet
- Diphtheria 1Document24 pagesDiphtheria 1Anam AbidNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainFrom EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainRating: 4 out of 5 stars4/5 (95)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (6)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)