Professional Documents
Culture Documents
Edukasi Jantung
Uploaded by
Suci Ika PratiwiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Edukasi Jantung
Uploaded by
Suci Ika PratiwiCopyright:
Available Formats
TAKING THE FAILURE
OUT OF HEART FAILURE
GET WITH THE GUIDELINES- HEART FAILURE
ENHANCED HEART FAILURE PATIENT EDUCATION
PRIOR TO HOSPITAL DISCHARGE
Why is enhanced patient education prior to
discharge so important? Patient education is key
early enough to allow the patient or a healthcare provider an
Why is Get With The Guidelines-Heart Failure
asking hospitals if the patient was provided
with 60 minutes of patient education prior
to discharge? At least 60 minutes of patient education
opportunity to institute treatments that can prevent clinical
is needed in order to ensure that the patient and/or their
deterioration in those patient with heart failure.1-2 However,
caregiver(s) understand what actions must be taken post
education of patients and their caregiver(s) can often
discharge. In one study a 60 minute teaching session delivered
be complex. It is critical for patients and their caregiver(s)
by an RN educator at the time of hospital discharge to patients
to understand how best to comply with physicians and
with heart failure using standardized instructions resulted
other healthcare providers instructions. Understanding
in improved clinical outcomes, increased self-care measure
care instructions has been associated with improved
adherence, and reduced cost of care.4
in order to detecting changes in body weight or clinical status
patient outcomes, such as reduced hospital readmissions.
There is data which supports the value of enhanced
Who Should Provide the Education to the
Patient and/or the Patients Caregiver(s)?
patient education in improving care and potentially reducing
Education and counseling should be delivered by providers
readmission. In a meta-analysis of 18 studies patients who
with the required knowledge base and using a team approach.
received appropriate patient education and proper discharge
RNs with expertise in heart failure management should provide
support showed a trend toward lower all-cause mortality,
the majority of education and counseling, supplemented by
length of stay, hospital costs, and an improvement in quality-
physician input and, when available and needed, input from
of life scores.
dietitians, pharmacists, and other health care providers.
What is the goal of patient education?
problem solving abilities, and motivation necessary for
Does the patient education need to occur
in a single 60 minute session or can the
education be broken into multiple sessions
so long as they total 60 minutes or more?
adherence to the treatment plan and effective participation in
The patient education does not need to occur in a single
self-care. Upon discharge, patient and caregiver(s) should be
60 minute session, but can be broken up by the educator into
aware and supportive of self-care follow-up plans, how to care
multiple sessions so long as they total 60 or more minutes.
The goals of heart failure patient education are to help patients
and their caregiver(s) acquire the knowledge, skills, strategies,
out self-care follow-up plans, and understand the importance
of adherence to a patients health-related quality of life.
JUNE 2011 | PAGE 01
2011 American Heart Association
TAKING THE FAILURE
OUT OF HEART FAILURE
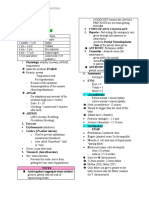
What domains should be covered during the
60 minute educational session? The 60 minute
The AHA/ACC Chronic Heart Failure guidelines state that:
patient education should include discussion on each of the
to improve clinical status in ambulatory patients with current
following domains:
or prior symptoms of HF and reduced LVEF (Class I, Level
Exercise training is beneficial as an adjunctive approach
of Evidence B).
01 Recognition of escalating symptoms and
concrete plan for response to particular symptoms.
03 Indications, use, and need for adherence with each
The patient/caregiver(s) should be able to identify specific
medication prescribed at discharge. Patients require
signs and symptoms of heart failure, and explain actions
guidance on how to institute an individualized system
to take when symptoms occur. Actions may include a flexible
for medication adherence. Nonadherence with heart failure
diuretic regimen or fluid restriction for volume overload.
medications can rapidly and profoundly adversely affect the
Example of signs and symptom include:
clinical status of patients. During the patient education period,
Shortness of breath (dyspnea)
it is important for the educator to reiterate medication name,
Persistent coughing or wheezing
dosing schedule, basic reason for specific medications,
Buildup of excess fluid in body tissues (edema)
expected side effects, and what to do if a dose is missed.
Tiredness, fatigue, decrease in exercise and activity
Asking patients to read and interpret the instructions from
Lack of appetite, nausea
a prescription medication bottle or procedure preparation
Increased heart rate
instructions provides a good literacy assessment. Patients
require guidance on how to institute an individualized system
A concrete plan for response for each particular symptom
for medication adherence, especially when the medication
should be discussed. Close monitoring, which includes
schedule requires doses to be taken when outside of the
surveillance by the patient and his or her family, can lead
home. During the patient education period, the educator
to the detection of changes in body weight or clinical status
should assess ability to read labels as needed and ensure
early enough to allow the patient or a healthcare provider
that the patient/caregiver have a plan for refilling medications
an opportunity to institute treatments that can prevent
on time to further promote medication adherence.
clinical deterioration.
04 Importance of daily weight monitoring.
02 Activity/exercise recommendations. In order to reduce
Sudden weight gain or weight loss can be a sign of heart
chances of readmissions, and to improve ambulatory status,
failure or worsening of condition. Therefore, the patient/
it is important for the patient to follow specific exercise
caregiver(s) should understand the importance of measuring
recommendations provided by the patient educator.
the patients weight on a daily basis, how todays weight
Instructions should include how to carry out the activity/
compares with dry weight, normal and exceptional limits
exercise, how long to carry out the activity/exercise, expected
of weight gain, and actions to take when weight increases
physiological changes with exercise (moderate increase in
above set limits, suggesting volume overload.
heart rate, breathing effort and diaphoresis), type and length
of time completing warm-up exercises and type and length
of time completing cool-down exercises.
JUNE 2011 | PAGE 02
2011 American Heart Association
TAKING THE FAILURE
OUT OF HEART FAILURE
05 Modify risks for heart failure progression. Below are
07 End of Life.Patients/Caregiver(s) should be educated on end of
some of the modifiable risk factors to discuss, as needed,
life, whenever appropriate. According to the AHA/ACC guidelines:
prior to patient discharge:
Options for end-of-life care should be discussed with the patient
Smoking cessation: If the patient is a smoker, then the
and family when severe symptoms in patients with refractory
educator should provide counseling on the importance of
end-stage HF persist despite application of all recommended
smoking cessation. A smoking cessation intervention may
therapies (Class I, Level of Evidence: C).1
include smoking cessation counseling (eg, verbal advice
to quit, referral to smoking cessation program or counselor)
08 Follow-up Appointments: Patients/Caregiver(s) should
and/or pharmacological therapy).
understand the rationale of the follow-up appointment in
Maintain specific body weight that promotes a normal body
improving the patients quality of life and reducing readmission
mass index: provide counseling on the effects of obesity on
even if the patient feels fine. The location, date, and time of the
insulin resistance, blood pressure and heart function. Provide
follow-up appointments should be provided in writing to the
practical information about eating a well balanced diet, high
patient prior to hospital discharge.
in fruits and vegetables and low in saturated fats and
non-whole grain carbohydrates.
Maintain blood pressure in target range: The blood pressure
goals should be reviewed with each patient.
09 Discharge Instructions: Failure of these patients to
understand how best to comply with physicians and other
healthcare providers instructions is often a cause of heart
failure exacerbation leading to subsequent hospital readmission.
06 Specific diet recommendations: individualized
A critical component of care coordination and transitions of care
low-sodium diet; recommendation for alcohol intake.
are that of written discharge instructions and educational materials
Sodium Restriction: Patient/caregiver(s) should be able to
given to patient and/or caregiver at discharge to home or during
understand and comply with sodium restriction. This includes
the hospital stay addressing all the above domains. Education
advising patients/caregiver(s) on how to read a food label to
of HF patients and their families is critical and often complex.
check sodium amount per serving and sort foods into highand low-sodium groups. Counseling also includes discussion
The patient/caregiver (s) should be provided with comprehensive
and possibly demonstration of how to achieve and maintain
written discharge instructions. This should include an emphasis
a low sodium diet when eating away from the home
on domains previously discussed but with special emphasis on:
(restaurant, when shopping or at another social gathering
The following 6 aspects of care: diet, discharge medications,
or at the homes of friends/relatives), when snacking, when
with a special focus on adherence, persistence, and uptitration
desiring ethnic foods, and when the budget is limited.
to recommended doses of ACE inhibitor/ARB and beta-blocker
Alcohol: Patients/Caregiver(s) should be able to understand
the limits for alcohol consumption or need for abstinence
if history of alcoholic cardiomyopathy.
medication, activity level, follow-up appointments, daily weight
monitoring, and what to do if [heart failure] symptoms worsen
(Class I, Level of Evidence: C).1
1 ACC/AHA 2009 Guideline Update for the Diagnosis and Management of Chronic Heart
3 Phillips CO, Wright SM, Kern DE, et al. Comprehensive discharge planning with post discharge
Failure in the Adult http://circ.ahajournals.org/cgi/reprint/CIRCULATIONAHA.109.192064.
support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291:135867.
2 HFSA 2010 Comprehensive Heart Failure Practice Guideline: Section 8: Disease
4 Koelling TM, Johnson ML, Cody RJ, et al. Discharge education improves clinical outcomes in
Management, Advance Directives, and End-of-Life Care in Heart Failure Education and
patients with chronic heart failure. Circulation. 2005;111:17985.
Counseling http://www.onlinejcf.com/article/S1071-9164(10)00223-X/fulltext .
JUNE 2011 | PAGE 03
2011 American Heart Association
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 50 Fungsi Keyboard Microsoft ExcelDocument10 pages50 Fungsi Keyboard Microsoft Exceltary_nuryanaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- NAEMT EMT Data ReportDocument20 pagesNAEMT EMT Data ReportepraetorianNo ratings yet
- What Is Good Practice in Autism EducationDocument51 pagesWhat Is Good Practice in Autism EducationAinisaNo ratings yet
- Sop 11Document2 pagesSop 11tary_nuryana100% (1)
- Narrative ChartingDocument2 pagesNarrative Chartingearl_llamas0% (2)
- HAS Manual Guidelines RiskDocument13 pagesHAS Manual Guidelines Risktary_nuryana100% (1)
- ThesisDocument44 pagesThesisApple T. ElarcosaNo ratings yet
- Clsi FungiDocument28 pagesClsi Fungimihai200775100% (2)
- Direct Compression - An Overview: - ReviewDocument4 pagesDirect Compression - An Overview: - ReviewJim ColinsNo ratings yet
- Basa Jawa HanacarakaDocument1 pageBasa Jawa HanacarakaSuci Ika PratiwiNo ratings yet
- Regresi LinierDocument2 pagesRegresi LinierSuci Ika PratiwiNo ratings yet
- A Meta-Analysis: Echinacea in The Prevention of Induced Rhinovirus ColdsDocument10 pagesA Meta-Analysis: Echinacea in The Prevention of Induced Rhinovirus ColdsSuci Ika PratiwiNo ratings yet
- Tests of NormalityDocument2 pagesTests of NormalitySuci Ika PratiwiNo ratings yet
- Kaffir Lime Peel MSDS SheetDocument3 pagesKaffir Lime Peel MSDS SheetSuci Ika PratiwiNo ratings yet
- Drug InteractionDocument5 pagesDrug InteractionSuci Ika PratiwiNo ratings yet
- Article1380709595 - Landy Et AlDocument7 pagesArticle1380709595 - Landy Et AlSuci Ika PratiwiNo ratings yet
- Interactions Between Sparfloxacin and Antacids - Dissolution and Adsorption StudiesDocument6 pagesInteractions Between Sparfloxacin and Antacids - Dissolution and Adsorption StudiesSuci Ika PratiwiNo ratings yet
- Crit Care Nurse 2005 Bergs 50 8Document10 pagesCrit Care Nurse 2005 Bergs 50 8Suci Ika PratiwiNo ratings yet
- Drug InteractionDocument5 pagesDrug InteractionSuci Ika PratiwiNo ratings yet
- Anti DepresaanDocument2 pagesAnti DepresaanSuci Ika PratiwiNo ratings yet
- Amlodipine and Simvastatin InteractionDocument5 pagesAmlodipine and Simvastatin InteractionSuci Ika PratiwiNo ratings yet
- Tenses AnggunDocument7 pagesTenses AnggunSuci Ika PratiwiNo ratings yet
- Protein Estrogen ReseptorDocument7 pagesProtein Estrogen ReseptorSuci Ika PratiwiNo ratings yet
- Cemaran MikrobaDocument1 pageCemaran MikrobaSuci Ika PratiwiNo ratings yet
- EmoDocument3 pagesEmoSuci Ika PratiwiNo ratings yet
- Ja200895a PDFDocument5 pagesJa200895a PDFSuci Ika PratiwiNo ratings yet
- 149 PDFDocument7 pages149 PDFSuci Ika PratiwiNo ratings yet
- Investigasi Uji Profisiensi 2010Document1 pageInvestigasi Uji Profisiensi 2010Suci Ika PratiwiNo ratings yet
- EmoDocument3 pagesEmoSuci Ika PratiwiNo ratings yet
- Stevi PDFDocument4 pagesStevi PDFSuci Ika PratiwiNo ratings yet
- 121 32 4 - Sigma Aldrich PDFDocument5 pages121 32 4 - Sigma Aldrich PDFSuci Ika PratiwiNo ratings yet
- 109995m Stability PDFDocument1 page109995m Stability PDFSuci Ika PratiwiNo ratings yet
- Alfa BetDocument1 pageAlfa Bettary_nuryanaNo ratings yet
- Micro-Needling Consultation & Consent FormDocument8 pagesMicro-Needling Consultation & Consent FormVivi AnaNo ratings yet
- Pharmacotherapy of HTNDocument57 pagesPharmacotherapy of HTNAbera JamboNo ratings yet
- Helping the Blind: Causes, Devices and PreventionDocument2 pagesHelping the Blind: Causes, Devices and PreventionZuzana Cverckova100% (1)
- Anthropometric Profile Evaluation of The Midface in Patients With Cleft Lip and PalateDocument10 pagesAnthropometric Profile Evaluation of The Midface in Patients With Cleft Lip and PalateAndy HongNo ratings yet
- Nursing Care Plan - Risk For BleedingDocument2 pagesNursing Care Plan - Risk For BleedingDaniel Andre S. SomorayNo ratings yet
- Pedia TranscriptDocument18 pagesPedia TranscriptUma CrespoNo ratings yet
- RCPA 225069 2018-Product-Catalogue PDFDocument91 pagesRCPA 225069 2018-Product-Catalogue PDFTanmay MehtaNo ratings yet
- Lung Dictionary Nov18 d070819Document60 pagesLung Dictionary Nov18 d070819KEZZIA MAE ABELLANo ratings yet
- U.S. v. James CurryDocument10 pagesU.S. v. James CurryLaw&CrimeNo ratings yet
- Exercises: Physical Fitness Test Individual FormDocument1 pageExercises: Physical Fitness Test Individual FormHazelle SagaoNo ratings yet
- Guideline For Connective Tissue DiseaseDocument6 pagesGuideline For Connective Tissue DiseaseLoudry Amsal EGNo ratings yet
- 12-Year-Old Female with RLQ Pain and Possible AppendicitisDocument4 pages12-Year-Old Female with RLQ Pain and Possible AppendicitiskymhanNo ratings yet
- ANIMAL PRODUCTION AND HEALTH GUIDEDocument78 pagesANIMAL PRODUCTION AND HEALTH GUIDEGaurav ModgilNo ratings yet
- Brainsci 10 00207 v2Document4 pagesBrainsci 10 00207 v2Isabel BelisaNo ratings yet
- Health 10 LAS Q4Document19 pagesHealth 10 LAS Q4JOSH ELORDENo ratings yet
- First FormativeDocument7 pagesFirst Formativeola nagarNo ratings yet
- WHO - Global Database On Body Mass IndexDocument1 pageWHO - Global Database On Body Mass IndexOwer AsvNo ratings yet
- NegOr Q4 MAPEH7 Module4b v2Document13 pagesNegOr Q4 MAPEH7 Module4b v2Jayvee PamintuanNo ratings yet
- Guide To FmgeDocument3 pagesGuide To FmgePraveen KumarNo ratings yet
- Otitis MediaDocument55 pagesOtitis MediaJollyann SedaNo ratings yet
- Forensic Medicine Thesis TopicsDocument7 pagesForensic Medicine Thesis Topicsafloziubadtypc100% (2)
- Department of Education: Republic of The PhilippinesDocument2 pagesDepartment of Education: Republic of The PhilippinesMeshiela MuñozNo ratings yet
- Personal Accident Takaful Claim FormDocument5 pagesPersonal Accident Takaful Claim FormALFRED CHEAM JIA JING -No ratings yet
- The PICOT Method - Why and How v4 - CADocument3 pagesThe PICOT Method - Why and How v4 - CAmelodia gandezaNo ratings yet
- Neurology Examination On Unconscious PatientDocument38 pagesNeurology Examination On Unconscious PatientAldo D'vatho MpNo ratings yet