Professional Documents
Culture Documents
Antibioticos para Procedimientos 2013
Uploaded by
Renzo Cruz CaldasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antibioticos para Procedimientos 2013
Uploaded by
Renzo Cruz CaldasCopyright:
Available Formats
Australian and New Zealand Journal of Obstetrics and Gynaecology 2012; 52: 412419
DOI: 10.1111/j.1479-828X.2012.01460.x
Review Article
Antibiotic prophylaxis in obstetric and gynaecological procedures:
A review
Vanessa CLIFFORD and Andrew DALEY
Department of Microbiology, The Royal Childrens Hospital, Melbourne, Vic., Australia
Surgical site infections are a common complication of obstetric and gynaecological surgeries; up to 10% of
gynaecological patients undergoing an operative procedure will develop a surgical site infection. In surgeries with high
rates of post-operative infection, antibiotic prophylaxis (using an antibiotic with an appropriate microbiological
spectrum and administered in a timely manner) can play a major role in improving outcomes. This review examines
the medical literature to assess the indications and appropriate antibiotic choices for prophylaxis to prevent surgical
site infection in obstetric and gynaecological surgery. For some procedures, such as caesarean section, surgical
termination of pregnancy and hysterectomy, antibiotic prophylaxis is clearly indicated. For other procedures, such as
insertion of an intrauterine device, medical termination of pregnancy and laparoscopy, antibiotic prophylaxis is usually
not required. For several other procedures where the evidence for antibiotic prophylaxis is unclear or inadequate, we
discuss the current evidence for and against prophylaxis. Guidelines for infective endocarditic prophylaxis with
surgery are also discussed.
Key words: antibiotic prophylaxis, gynaecological surgery, obstetric surgery, surgical site infection.
Introduction
Surgical site infections (SSIs) are a common adverse
event in hospitalised patients;1 810% of gynaecological
surgery patients undergoing an operative procedure will
develop an SSI.2 SSIs have been shown to increase
mortality, readmission rate and length of hospital stay.3,4
Rates of infection vary according to the premorbid
condition of the patient, as well as surgical and
anaesthetic factors.2
Appropriate and timely antibiotic prophylaxis has
been shown to be highly effective in reducing the
incidence of SSI.5 Antibiotic prophylaxis is designed to
reduce the microbial contamination of a wound during
surgery to a level that will limit the opportunity for
post-operative infection. The need for antibiotic
prophylaxis depends primarily upon the likely risk of
wound contamination during surgery. In 1964, the US
National Research Council developed a Surgical
Wounds Classification scheme.6 This scheme classifies
wounds as clean, clean-contaminated, contaminated or
Correspondence: Dr Vanessa Clifford, Department of
Microbiology, Royal Childrens Hospital, Flemington Road
Parkville Victoria 3052, Australia.
Email: vanessa.clifford@rch.org.au
Received 11 February 2012; accepted 9 May 2012.
412
dirty-infected (SSI rates are 12%, 69%, 1320% and
>40% without antibiotic prophylaxis respectively for
each type of wound).7 Owing to the high rates of postoperative wound infection with all but clean surgical
procedures, administration of prophylactic antibiotics is
universally recommended.8 Procedures that open the
genito-urinary tract are usually considered cleancontaminated. In addition, antibiotic prophylaxis is often
recommended for clean surgical wounds where the
consequences of post-operative infection will be
devastating.8 A variety of refinements to this risk
assessment have been proposed, including the United
States National Healthcare Safety Network Risk Index
Scoring system, which takes into account additional
factors such as patient health (American Society of
Anesthesiologists score) and duration of the operation
(>75th percentile).
A number of studies across a range of surgical
procedures have shown that there is a narrow window of
opportunity for the administration of effective
antimicrobial prophylaxis.9 Antibiotics need to be present
in the tissue at the time of incision to be effective.10 In
general, antimicrobial prophylaxis after wound closure is
unnecessary as it does not provide additional benefit.11
and can lead to higher costs, morbidity and drive the
emergence of resistant bacteria.12
It is rare in obstetric or gynaecological practice to
require additional doses of antibiotics beyond the initial
2012 The Authors
ANZJOG 2012 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists
The Australian and
New Zealand Journal
of Obstetrics and
Gynaecology
Antibiotic prophylaxis in O &G procedures
dose administered at induction of anaesthesia. Most
studies comparing single with multiple dose strategies
do not show a benefit,11,13 although these are not
all restricted to obstetric and gynaecological procedures.
In general, doses only need to be repeated if the
operation lasts longer than the half life of the
antimicrobial agent.
Reviews of surgical prophylaxis suggest compliance
issues in 3090% of cases owing to problems with
antibiotic choice, dose and duration.14
Ideally, prophylactic antibiotics should cover the
narrowest spectrum or organisms possible to minimise
the development of bacterial resistance.15 For this
reason, it is important to consider the likely source of
pathogens in each type of surgery. For most infections that
occur after obstetric or gynaecological surgery, the source
of pathogens is the endogenous flora of the womans
vagina or skin. The endogenous flora of the genital tract is
polymicrobial, consisting of anaerobes, gram-negative
aerobes and gram positive cocci (such as Staphylococci
and Streptococci). In contrast, laparoscopic procedures
that do not breach any mucosal surfaces are more
commonly contaminated with skin organisms only (usually
gram positive organisms such as Staphylococci).
It should be noted that prophylactic antibiotics do not
need to cover every possible pathogen that may cause
infection. Decreasing the number of organisms present
(the bacterial load) will usually enable the patients
immunological
defences
to
function
adequately.
Prophylaxis is also understood as being distinct from early
treatment when clinical infection is present.
Other factors to consider when choosing an appropriate
antibiotic for prophylaxis include low toxicity, an
established safety record and the ability to reach an
effective concentration in the relevant tissue prior to the
procedure.1
Narrow-spectrum first-generation cephalosporins, such
as cephazolin, are used in preference to later generation
agents, such as ceftriaxone, because the latter are strong
drivers of resistance in gram-negative bacteria and have
less activity against Staphylococci, a common cause of
post-operative wound infection. Cephalosporins in general
have no activity against Enterococcus spp., which may be
of significance for intra-abdominal procedures where the
bowel is breached. Comparisons of first and third
generation cephalosporins in several trials have not shown
superiority in preventing wound infection.16
Whilst allergies to b-lactam antibiotics are frequently
reported by patients, the incidence of true IgE-mediated
allergy (urticaria, angioedema, bronchospasm) or serious
adverse reaction (such as drug fever and toxic epidermal
necrolysis) is rare. Rates are reported as between 1 and 4
per 10 000 doses.17
Alternative agents include lincomycin/clindamycin
and/or vancomycin. High rates of methicillin-resistant
Staphylococcus aureus at an institution would influence the
choice of prophylactic antibiotic in favour of a
glycopeptide such as vancomycin.
Obstetric Procedures
Caesarean section
Women who undergo caesarean section have a much
higher risk of developing an infection compared with
women who deliver vaginally.18 A 2010 Cochrane review
found conclusively that routine antibiotic prophylaxis for
caesarean section (in both elective and non-elective
settings) is effective in reducing SSI [relative risk (RR) for
wound infection 0.39; 95% confidence interval (CI) 0.32
0.48]; the analysis included 77 studies and 11 971
women.19 The timing of antibiotic prophylaxis was not
specifically addressed in the review.
A second recent Cochrane review assessed whether
different classes of antibiotic are more (or less) effective
for surgical prophylaxis. This review, whilst limited by
poor quality data, showed no overall difference in
outcome according to antibiotic class (e.g when
comparing penicillins and cephalosporins).20 None of the
studies looked at the outcome for the baby or maternal
infection after the initial post-operative stay. An exception
should be made for obese women, where there is
emerging evidence that they have a higher risk of SSI
post-Caesarean section and may benefit from extended
spectrum antibiotic prophylaxis (e.g cephalosporin plus
azithromycin).21
Studies have shown that single-dose antibiotic
prophylaxis is as effective as multiple doses of
antibiotic.13,22
Recent evidence suggests that antibiotics administered
prior to skin incision may further reduce the risk of postoperative infection.23 A meta-analysis in 2008 (that
included three randomised controlled trials; with a total of
749 women) found preoperative administration of
antibiotic (compared with administration of antibiotic after
cord clamping) was associated with a 53% reduction
in postpartum endometritis (RR 0.47; 95% CI 0.26
0.85).24 Other outcomes (wound infection and confirmed
sepsis) did not reach statistical significance. Other large
retrospective cohort studies published since this 2008
review have supported the finding of a reduction in
infectious
morbidity
with
antibiotic
prophylaxis
administered prior to skin incision.25,26 The meta-analysis
of these RCTs did not differentiate between labouring
and non-labouring women; it is therefore difficult to
be sure that these results apply equally to women
undergoing elective caesarean section. Interestingly, a
recent prospective controlled trial did not find a benefit
of pre-incision antibiotic prophylaxis compared with
administration after cord clamping in women undergoing
elective caesarean section.27 In addition, no benefit for
pre-incision antibiotic prophylaxis for elective caesareans
was found in a recent large study reporting on infection
rates using historical controls, after an institutional policy
change.25
The benefit of administration of antibiotic prophylaxis
prior to skin incision needs to be weighed against
potential risks. To date, studies have shown that exposure
2012 The Authors
ANZJOG 2012 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists
413
V. Clifford and A. Daley
of the infant to antibiotics (when administered prior to
cord clamping) is not associated with an increase in
neonatal sepsis, admission or length of stay in the
Neonatal Intensive Care Unit.25,27,28 Other infant
outcomes were infrequently reported;19 in particular, no
studies reported on the incidence of oral thrush in babies
exposed to antibiotics. The long-term outcomes of infant
exposure to antibiotics are not known.
There is a very small risk of maternal anaphylaxis with
antibiotic prophylaxis and, if administered pre-cord
clamping, may put the infant at risk. This minor risk is
likely outweighed by the benefits, especially given that
antibiotic prophylaxis for Group B streptococcus is
routinely administered to a significant proportion of
labouring women.
The currently available evidence suggests that all
women undergoing caesarean section should receive
antibiotic prophylaxis. A single dose administered in the
30 min prior to skin incision for emergency caesarean
sections is appropriate (see Table 1).
Termination of pregnancy
Reported infection rates for first trimester surgical
termination of pregnancy range from 0.01 to 2.44%;29
similar rates have been reported for second trimester
surgical termination of pregnancy.30 Cervicitis (caused by
Chlamydia trachomatis or Neisseria gonorrhoeae) is a risk
factor for postabortal infection.31 A Swedish cohort study
found that the presence of chlamydia prior to termination
of pregnancy (in the era before antibiotic prophylaxis)
conferred a 30-fold increased risk of salpingitis and a
4-fold increased risk of endometritis.32
A meta-analysis of various antibiotic regimes showed
that antibiotic prophylaxis for surgical termination of
pregnancy reduces the risk of upper genital tract infection
(RR 0.58; CI 0.470.71).33 Most of the studies included
in this meta-analysis had relatively high rates of sexually
transmitted infections (STI) infections; the benefit of
universal prophylaxis in populations at very low risk is
unclear.29
Both oral doxycycline31,34 and metronidazole31 have
been shown to be effective in reducing the risk of
postabortal infection. To maximise efficacy, antibiotic
prophylaxis should be administered before the
procedure.29
One study found that a screen and treat strategy for
detecting C. trachomatis was less cost-effective than
universal antibiotic treatment with doxycycline prior to
termination of pregnancy.35 There are no randomised
trials that compare single-dose antibiotic prophylaxis for
C. trachomatis with a screen and treat approach.29 The
relative cost-effectiveness of each approach will clearly
vary according to the incidence of STIs in the population.
The association between bacterial vaginosis (a complex
alteration of normal vaginal flora with overgrowth of
anaerobic organisms) and postabortal infection rates is
not clear. To date, there has been one trial of oral
414
metronidazole treatment of bacterial vaginosis (BV) prior
to termination of pregnancy that demonstrated a
reduction in postabortal infection rates,36 whilst three
other trials have not demonstrated a statistically significant
difference in infection rates.29
For medical abortion, there are no randomised
controlled trials of antibiotic prophylaxis. The best
estimate of first trimester medical termination of
pregnancy infection rates is approximately 0.3%,29,37 with
rates of serious infection estimated at approximately
0.09%.38 A retrospective cohort study from the Planned
Parenthood Federation of America suggests that the
number needed to treat (NNT) with doxycycline (for
1 week) would be 2500 to prevent one serious infection.38
Based on this estimate, antibiotic prophylaxis for medical
abortion is not warranted.
Manual removal of retained placenta
Manual removal of a retained placenta is required in
approximately 2% of deliveries39 and increases the risk of
bacterial contamination of the uterine cavity.40
Controversy exists over whether manual removal increases
the risk of postpartum endometritis above that which
would occur with vaginal delivery of the placenta. Ely
et al.41 reported a retrospective cohort study involving
1082 women which demonstrated that the incidence of
endometritis following manual removal of the placenta
was 6.7% compared with 1.8% of women with normal
placental delivery (OR 2.9; CI 1.74.9). A 2006
Cochrane review did not find any randomised trials that
evaluated whether antibiotic prophylaxis reduced the risk
of infection with this procedure;40 no further randomised
trials were identified in the published literature after 2006.
On the basis of reported rates of endometritis in the
study by Ely et al., and until controlled studies become
available, antibiotic prophylaxis for manual removal of a
retained placenta is justified.
Third- and Fourth-degree vaginal tears
Severe perineal trauma occurs in 18% of vaginal
deliveries; it is more common with operative vaginal
delivery (especially when forceps are used) and/or midline
episiotomy.42 Third- and fourth-degree tears involve the
anal sphincter and thus give rise to a contaminated or
clean-contaminated wound. Risks from perineal tears
include dyspareunia, incontinence and recto-vaginal
fistula.43 A recent Cochrane review42 found only one
randomised controlled trial assessing the outcome of
antibiotic prophylaxis for third- and fourth-degree vaginal
tears.44 This trial showed a reduction in post partum
infection rates (RR 0.34, 95% CI 0.120.96) with
antibiotic prophylaxis, but was limited by early
termination owing to difficulties in enrolment and some
loss to follow-up.42,44
In the absence of definitive evidence from well-designed
randomised controlled trials, a pragmatic approach is to
2012 The Authors
ANZJOG 2012 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists
Antibiotic prophylaxis in O &G procedures
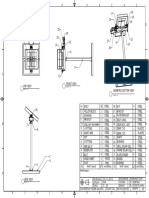
Table 1 Antibiotics for surgical prophylaxis
Surgery
Obstetric
Caesarean section
Termination of
pregnancy (surgical)
Medical Termination
of pregnancy
Manual removal of
placenta
3rd and 4th degree
vaginal tears
Gynaecological
Hysterectomy
IUD insertion
Hysterosalpingography
or hysterosocopy or
chromotubation for
patients with dilated
tubes or a history of
PID or tubal
damage
Hysterosalpingography
or hysterosocopy or
chromotubation with
no history of PID
and normal tubes on
visualisation
Endometrial biopsy
Laparoscopy
1st line
Level of
evidence64
Alternative
Cephazolin 1 g (adult
80 kg or more: 2 g) IV,
before skin incision.
Clindamycin
600 mg IV
Metronidazole 500 mg IV,
ending the infusion at the
time of induction AND
Doxycycline 400 mg PO
Not indicated-level
Clindamycin
600 mg
IV + Azithromycin
Metronidazole 500 mg IV,
ending the infusion at the
time of induction AND
Cephazolin 1 g (adult
80 kg or more: 2 g) IV, at
the time of induction
Metronidazole 500 mg IV,
AND
Cephazolin 1 g (adult
80 kg or more: 2 g) IV
III-3
Clindamycin
600 mg IV
II
Clindamycin
600 mg IV
Metronidazole 500 mg IV,
ending the infusion at the
time of induction AND
Cephazolin 1 g (adult
80 kg or more: 2 g) IV, at
the time of induction
Not indicated
Doxycycline 100 mg bd
for 5 days +
Metronidazole 500 mg IV
single dose
Clindamycin
600 mg IV
Gentamicin
OR
Cefoxitin 2 g IV at
time of induction
Comments
Antibiotics prior to skin incision reduce
maternal morbidity without affecting
neonatal morbidity or mortality. Surgical
prophylaxis should be administered even if
the patients has received Group B
Streptococcal antibiotic prophylaxis during
labour
An alternative approach is to screen for
C. trachomatis and bacterial vaginosis prior
to ToP
III-3
I
IV
Not indicated
IV
Not indicated
Not indicated
IV
II
Patients should be screened and treated for
bacterial vaginosis before hysterectomy
Azithromycin 1 g
orally
National Health and Medical Research Council Levels of Evidence.64
Level I: A systematic review of level II studies; Level II: A randomised controlled trial; Level III-1 A pseudo-randomised controlled trial;
Level III-2 A comparative study with concurrent controls; Level III-3 A comparative study without concurrent controls; Level IV A case
series with either post-test outcomes or pretest/post-test outcomes.
2012 The Authors
ANZJOG 2012 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists
415
V. Clifford and A. Daley
recommend antibiotic prophylaxis on the basis of the
wound type (contaminated) and the potential adverse
outcomes arising from an infection.
Gynaecological Procedures
Hysterectomy
The benefit of antibiotic prophylaxis in reducing postoperative infection is well established for both vaginal and
abdominal hysterectomy,45,46 although it should be noted
that randomised trials of antibiotic prophylaxis for
laparoscopic total hysterectomy and laparoscopically
assisted hysterectomy have not been performed.1
Multiple doses of antibiotic are not more effective than
a single antibiotic dose prior to incision.47 No particular
antibiotic has been shown to be superior.1 In the absence
of direct evidence on the appropriate choice of
prophylactic antibiotic, the practical approach is to choose
a combination of antibiotics that cover the expected
microbial flora of the region.
Bacterial vaginosis is a risk factor for infection after
hysterectomy. A randomised non-blinded controlled trial
found that treatment with rectal metronidazole for women
with bacterial vaginosis significantly reduced the rates of
vaginal cuff infection post hysterectomy.48
The available evidence suggests that all patients should
be screened and treated for bacterial vaginosis prior to
undergoing hysterectomy. Patients should receive
antibiotic prophylaxis for hysterectomy (including an
antibiotic with an anaerobic spectrum).
Hysteroscopy, hysterosalpingography or
chromotubation
Infection after hysterosalpingography (HSG) occurs in a
small number of women; reported rates are 1.43.4%.49,50
The risk appears to be far lower when the fallopian tubes
are not dilated, although this data is from a retrospective
review.49 Infections after hysteroscopic surgery are
reported in 0.181.5% of cases.5153 In a study of 200
women undergoing hysteroscopic surgery, three developed
severe pelvic infection; all three had a history of pelvic
inflammatory disease (PID). A recent Dutch study of
hysteroscopy conducted in an outpatient setting in
asymptomatic women with infertility found an infection
rate of 0.4% without antibiotic prophlaxis.54
Based on these studies, it is reasonable to recommend
antibiotic prophylaxis for women with a history of PID or
for those with tubal damage noted at the time of the
procedure. Doxycycline is the usual recommended agent
and is continued for 5 days to treat presumed PID.
Single-dose azithromycin is an acceptable alternative.
Intra-uterine device (IUD) Insertion
The risk of PID because of the introduction of genital
tract organisms is six times higher in the first 20 days
416
after insertion of an IUD. The risk of IUD-associated
infections is also significantly higher in women from
populations where there is a high prevalence of STIs (3
14%).55
Whilst significant concern exists about the risk of
PID after IUD insertion, a 2001 Cochrane metaanalysis of four randomised trials found that there was
no evidence that antibiotic prophylaxis reduced the risk
of PID.55 This included two trials conducted in areas
with a high prevalence of STIs, Kenya and Nigeria. In
the Kenyan trial, which had the highest rate of STIs, a
benefit was found with prophylactic antibiotics.56 It is
also important to note that all the women in the
United States trial had been screened for STIs prior to
IUD insertion.57
In addition, a well-defined complication associated with
IUD use is infection with Actinomyces spp. The incidence
of cervical colonisation with these organisms increases
with the duration of IUD use. Antimicrobial prophylaxis
at the time of IUD insertion does not impact on the risk
of future actinomycosis.55
Whilst at present, the cost-effectiveness of screening for
STIs prior to IUD insertion is unclear, it is reasonable
that women should be screened and treated for STIs prior
to IUD insertion, because the risk of IUD-associated
infection is higher in this group. Universal prophylaxis for
IUD insertion is not indicated.
Laparoscopy
Laparoscopic surgery is usually clean surgery, with a low
infection risk (no mucosal surfaces are breached). A
single placebo-controlled randomised trial of antibiotic
prophylaxis for laparoscopic gynaecological surgery failed
to find a benefit.1,58 At this stage, there is insufficient
evidence to be certain of the benefits of prophylaxis for
laparoscopic surgery.
Other procedures: large loop excision of the
transformation zone (LLETZ) and midurethral
sling procedures
For several other common gynaecological procedures,
there is insufficient research evidence to determine
whether antibiotic prophylaxis is indicated.
Large loop excision of the transformation zone
Many women report vaginal discharge and bleeding after
LLETZ, but there is very little trial evidence for
antimicrobial prophylaxis for LLETZ procedure.59 It is
also unclear whether discharge and bleeding is
necessarily attributed to infection. A single randomised
controlled trial did not find a difference in vaginal
discharge with routine administration of ofloxacin
following LLETZ.60 There are no trials of preoperative
antibiotic prophylaxis.
2012 The Authors
ANZJOG 2012 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists
Antibiotic prophylaxis in O &G procedures
Midurethral sling
References
Rates of infection (especially urinary tract infection) are
relatively high (~5.5%) after midurethral sling
procedures,61 suggesting that perioperative antibiotic
prophylaxis may be useful. There is, however, very little
high-quality research evidence to support this practice.
Further evaluation is needed.
1 ACOG Committee on Practice BulletinsGynecology. ACOG
practice bulletin No. 104: antibiotic prophylaxis for gynecologic
procedures. Obstet Gynecol 2009; 113: 11801189.
2 Kamat AA, Brancazio L, Gibson M. Wound infection in
gynecologic surgery. Infect Dis Obstet Gynecol 2000; 8: 230234.
3 Australian Council for Safety and Quality in Health Care.
Preventing Surgical Site Infection: Toolkit. In; 2011.
4 Kirkland KB, Briggs JP, Trivette SL et al. The impact of
surgical-site infections in the 1990s: attributable mortality,
excess length of hospitalization, and extra costs. Infect Control
Hosp Epidemiol 1999; 20: 725730.
5 Steinberg JP, Braun BI, Hellinger WC et al. Timing of
antimicrobial prophylaxis and the risk of surgical site
infections: results from the Trial to Reduce Antimicrobial
Prophylaxis Errors. Ann Surg 2009; 250: 1016.
6 Berard F, Gandon J. Postoperative wound infections: the
influence of ultraviolet irradiation of the operating room and
of various other factors. Ann Surg 1964; 160: 1192.
7 Cruse PJ, Foord R. The epidemiology of wound infection. A
10-year prospective study of 62,939 wounds. Surg Clin North
Am 1980; 60: 2740.
8 Dellinger EP, Gross PA, Barrett TL et al. Quality standard for
antimicrobial prophylaxis in surgical procedures. Infectious
Diseases Society of America. Clin Infect Dis 1994; 18: 422
427.
9 Classen DC, Evans RS, Pestotnik SL et al. The timing of
prophylactic administration of antibiotics and the risk of
surgical-wound infection. N Engl J Med 1992; 326: 281286.
10 Burke JF. The effective period of preventive antibiotic action
in experimental incisions and dermal lesions. Surgery 1961;
50: 161168.
11 McDonald M, Grabsch E, Marshall C, Forbes A. Single- versus
multiple-dose antimicrobial prophylaxis for major surgery:
a systematic review. Aust N Z J Surg 1998; 68: 388396.
12 Harbarth S, Samore MH, Lichtenberg D, Carmeli Y.
Prolonged antibiotic prophylaxis after cardiovascular surgery
and its effect on surgical site infections and antimicrobial
resistance. Circulation 2000; 101: 29162921.
13 McGregor JA, French JI, Makowski E. Single-dose cefotetan
versus multidose cefoxitin for prophylaxis in cesarean section
in high-risk patients. Am J Obstet Gynecol 1986; 154: 955
960.
14 Dettenkofer M, Forster DH, Ebner W et al. The practice of
perioperative antibiotic prophylaxis in eight German hospitals.
Infection 2002; 30: 164167.
15 Weinstein JW, Roe M, Towns M et al. Resistant enterococci: a
prospective study of prevalence, incidence, and factors
associated with colonization in a university hospital. Infect
Control Hosp Epidemiol 1996; 17: 3641.
16 Jones RN, Wojeski W, Bakke J et al. Antibiotic prophylaxis of
1,036 patients undergoing elective surgical procedures. A
prospective, randomized comparative trial of cefazolin,
cefoxitin, and cefotaxime in a prepaid medical practice. Am J
Surg 1987; 153: 341346.
17 International Rheumatic Fever Study Group. Allergic
reactions to long-term benzathine penicillin prophylaxis for
rheumatic fever. International Rheumatic Fever Study Group.
Lancet 1991; 337: 13081310.
Prevention of infective endocarditis
The 2007 American Heart Association guideline found no
evidence that administration of prophylactic antibiotics for
genitourinary procedures reduces the risk of infective
endocarditis.62 For this reason, prophylaxis is generally
not recommended except for persons with heart
conditions with the highest lifetime risk of endocarditis.
These conditions includes a prosthetic cardiac valve,
unrepaired cyanotic congenital heart disease (CHD),
completely repaired CHD with prosthetic material or
device in the first 6 months after the procedure,
repaired CHD with a prosthetic patch or device and
cardiac transplantation recipients who develop cardiac
valvulopathy.62
For these patients, prophylaxis with an antibiotic that is
active against enterococci (such as ampicillin or
vancomycin) should be considered in addition to any
antibiotic that would otherwise be administered as routine
surgical prophylaxis in a healthy person.63
Conclusions
Infection occurs when the balance between host defences
and organism virulence are disturbed. In addition to
prophylactic antibiotics, careful attention should be paid
to other aspects of surgical care including meticulous
skin antisepsis, aseptic surgical technique, avoidance of
shaving, management of chronic illness (e.g hypoalbuminemia, malnutrition) and maintenance of normoglycemia and normothermia perioperatively, to further
reduce the incidence of SSI.
Prophylactic antibiotics are a very effective adjunct
in preventing SSI when used appropriately (see
Table 1). Attention should be paid to ensure that a low
toxicity antibiotic with an appropriate spectrum of
activity is administered in a timely manner prior to
surgery.
It should be noted that prophylactic antibiotics may not
be necessary for some low-risk obstetric and gynaecological procedures such as laparoscopy, IUD insertion
or medical termination of pregnancy.
Conflicts of Interest and Financial
Disclosure
There are no conflicts of interest and no relevant sources
of funding.
2012 The Authors
ANZJOG 2012 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists
417
V. Clifford and A. Daley
18 Declercq E, Barger M, Cabral HJ et al. Maternal outcomes
associated with planned primary cesarean births compared with
planned vaginal births. Obstet Gynecol 2007; 109: 669677.
19 Smaill FM, Gyte GM. Antibiotic prophylaxis versus no
prophylaxis for preventing infection after cesarean section.
Cochrane Database Syst Rev 2010; 1: CD007482.
20 Alfirevic Z, Gyte GM, Dou L. Different classes of antibiotics
given to women routinely for preventing infection at caesarean
section. Cochrane Database Syst Rev 2010; 10: CD008726.
21 Tita AT, Owen J, Stamm AM et al. Impact of extendedspectrum
antibiotic
prophylaxis
on
incidence
of
postcesarean surgical wound infection. Am J Obstet Gynecol
2008; 199: 303.
22 Tita AT, Rouse DJ, Blackwell S et al. Emerging concepts in
antibiotic prophylaxis for cesarean delivery: a systematic
review. Obstet Gynecol 2009; 113: 675682.
23 Lamont RF, Sobel JD, Kusanovic JP et al. Current debate on
the use of antibiotic prophylaxis for caesarean section. BJOG
2011; 118: 193201.
24 Costantine MM, Rahman M, Ghulmiyah L et al. Timing of
perioperative antibiotics for cesarean delivery: a metaanalysis.
Am J Obstet Gynecol 2008; 199: 301.
25 Owens SM, Brozanski BS, Meyn LA, Wiesenfeld HC.
Antimicrobial prophylaxis for cesarean delivery before skin
incision. Obstet Gynecol 2009; 114: 573579.
26 Kaimal AJ, Zlatnik MG, Cheng YW et al. Effect of a change
in policy regarding the timing of prophylactic antibiotics on
the rate of postcesarean delivery surgical-site infections. Am J
Obstet Gynecol 2008; 199: 310.
27 Witt A, Doner M, Petricevic L et al. Antibiotic prophylaxis
before surgery vs after cord clamping in elective cesarean
delivery: a double-blind, prospective, randomized, placebocontrolled trial. Arch Surg 2011; 146: 14041409.
28 Yildirim G, Gungorduk K, Guven HZ et al. When should we
perform prophylactic antibiotics in elective cesarean cases?
Arch Gynecol Obstet 2009; 280: 1318.
29 Achilles SL, Reeves MF. Prevention of infection after induced
abortion: release date October 2010: SFP guideline 20102.
Contraception 2011; 83: 295309.
30 Jacot FR, Poulin C, Bilodeau AP et al. A five-year experience
with second-trimester induced abortions: no increase in
complication rate as compared to the first trimester. Am J
Obstet Gynecol 1993; 168: 633637.
31 Levallois P, Rioux JE. Prophylactic antibiotics for suction
curettage abortion: results of a clinical controlled trial. Am J
Obstet Gynecol 1988; 158: 100105.
32 Osser S, Persson K. Postabortal pelvic infection associated
with Chlamydia trachomatis and the influence of humoral
immunity. Am J Obstet Gynecol 1984; 150: 699703.
33 Sawaya GF, Grady D, Kerlikowske K, Grimes DA.
Antibiotics at the time of induced abortion: the case for
universal prophylaxis based on a meta-analysis. Obstet Gynecol
1996; 87: 884890.
34 Darj E, Stralin EB, Nilsson S. The prophylactic effect of
doxycycline on postoperative infection rate after first-trimester
abortion. Obstet Gynecol 1987; 70: 755758.
35 Cameron ST, Sutherland S. Universal prophylaxis
compared with screen-and-treat for Chlamydia trachomatis
prior to termination of pregnancy. BJOG 2002; 109: 606
609.
418
36 Larsson PG, Platz-Christensen JJ, Thejls H et al. Incidence of
pelvic inflammatory disease after first-trimester legal abortion
in women with bacterial vaginosis after treatment with
metronidazole: a double-blind, randomized study. Am J Obstet
Gynecol 1992; 166: 100103.
37 Spitz IM, Bardin CW, Benton L, Robbins A. Early pregnancy
termination with mifepristone and misoprostol in the United
States. N Engl J Med 1998; 338: 12411247.
38 Fjerstad M, Trussell J, Sivin I et al. Rates of serious infection
after changes in regimens for medical abortion. N Engl J Med
2009; 361: 145151.
39 Taylor LK, Simpson JM, Roberts CL et al. Risk of
complications in a second pregnancy following caesarean
section in the first pregnancy: a population-based study. Med
J Aust 2005; 183: 515519.
40 Chongsomchai C, Lumbiganon P, Laopaiboon M.
Prophylactic antibiotics for manual removal of retained
placenta in vaginal birth. Cochrane Database Syst Rev 2006; 2:
CD004904.
41 Ely JW, Rijhsinghani A, Bowdler NC, Dawson JD. The
association between manual removal of the placenta and
postpartum endometritis following vaginal delivery. Obstet
Gynecol 1995; 86: 10021006.
42 Buppasiri P, Lumbiganon P, Thinkhamrop J, Thinkhamrop B.
Antibiotic prophylaxis for third- and fourth-degree perineal
tear during vaginal birth. Cochrane Database Syst Rev 2010;
11: CD005125.
43 Homsi R, Daikoku NH, Littlejohn J, Wheeless CR, Jr.
Episiotomy: risks of dehiscence and rectovaginal fistula. Obstet
Gynecol Surv 1994; 49: 803808.
44 Duggal N, Mercado C, Daniels K et al. Antibiotic
prophylaxis for prevention of postpartum perineal wound
complications: a randomized controlled trial. Obstet Gynecol
2008; 111: 12681273.
45 Duff P, Park RC. Antibiotic prophylaxis in vaginal
hysterectomy: a review. Obstet Gynecol 1980; 55: 193S202S.
46 Tanos V, Rojansky N. Prophylactic antibiotics in abdominal
hysterectomy. J Am Coll Surg 1994; 179: 593600.
47 Chang WC, Lee MC, Yeh LS et al. Quality-initiated
prophylactic
antibiotic
use
in
laparoscopic-assisted
vaginal hysterectomy. Aust N Z J Obstet Gynaecol 2008; 48:
592595.
48 Larsson PG, Carlsson B. Does pre- and postoperative
metronidazole treatment lower vaginal cuff infection rate after
abdominal hysterectomy among women with bacterial
vaginosis? Infect Dis Obstet Gynecol 2002; 10: 133140.
49 Pittaway DE, Winfield AC, Maxson W et al. Prevention of
acute pelvic inflammatory disease after hysterosalpingography:
efficacy of doxycycline prophylaxis. Am J Obstet Gynecol
1983; 147: 623626.
50 Moller BR, Allen J, Toft B et al. Pelvic inflammatory disease
after hysterosalpingography associated with Chlamydia
trachomatis and Mycoplasma hominis. Br J Obstet Gynaecol
1984; 91: 11811187.
51 Baggish MS, Sze EH. Endometrial ablation: a series of 568
patients treated over an 11-year period. Am J Obstet Gynecol
1996; 174: 908913.
52 Garry R, Shelley-Jones D, Mooney P, Phillips G. Six
hundred endometrial laser ablations. Obstet Gynecol 1995; 85:
2429.
2012 The Authors
ANZJOG 2012 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists
Antibiotic prophylaxis in O &G procedures
53 McCausland VM, Fields GA, McCausland AM, Townsend
DE. Tuboovarian abscesses after operative hysteroscopy. J
Reprod Med 1993; 38: 198200.
54 Kasius JC, Broekmans FJ, Fauser BC et al. Antibiotic
prophylaxis for hysteroscopy evaluation of the uterine cavity.
Fertil Steril 2011; 95: 792794.
55 Grimes DA, Schulz KF. Prophylactic antibiotics for
intrauterine device insertion: a metaanalysis of the
randomized controlled trials. Contraception 1999; 60: 5763.
56 Sinei SK, Schulz KF, Lamptey PR et al. Preventing IUCDrelated pelvic infection: the efficacy of prophylactic doxycycline
at insertion. Br J Obstet Gynaecol 1990; 97: 412419.
57 Walsh TL, Bernstein GS, Grimes DA et al. Effect of
prophylactic antibiotics on morbidity associated with IUD
insertion: results of a pilot randomized controlled trial. IUD
Study Group. Contraception 1994; 50: 319327.
58 Kocak I, Ustun C, Emre B, Uzel A. Antibiotics prophylaxis in
laparoscopy. Ceska Gynekol 2005; 70: 269272.
59 Chan KKL, Tam KF, Tse KY, Ngan HYS. The use of vaginal
antimicrobial after large loop excision of transformation
zone: a prospective randomised trial. BJOG 2007; 114: 970
976.
60 Foden-Shroff J, Redman CW, Tucker H et al. Do routine
antibiotics after loop diathermy excision reduce morbidity? Br
J Obstet Gynaecol 1998; 105: 10221025.
61 Swartz M, Ching C, Gill B et al. Risk of infection after
midurethral synthetic sling surgery: are postoperative
antibiotics necessary? Urology 2010; 75: 13051308.
62 Wilson W, Taubert KA, Gewitz M et al. Prevention of
infective endocarditis: guidelines from the American Heart
Association: a guideline from the American Heart Association
Rheumatic Fever, Endocarditis, and Kawasaki Disease
Committee, Council on Cardiovascular Disease in the Young,
and the Council on Clinical Cardiology, Council on
Cardiovascular Surgery and Anesthesia, and the Quality of
Care and Outcomes Research Interdisciplinary Working
Group. Circulation 2007; 116: 17361754.
63 Antibiotic Expert Group ed. Therapeutic Guidelines:
Antibiotic. 14 ed. Melbourne: Therapeutic Guidelines
Limited; 2010.
64 National Health and Medical Research Council. (2009)
NHMRC levels of evidence and grades for recommendations
for developers of guidelines: National Health and Medical
Research Council.
2012 The Authors
ANZJOG 2012 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists
419
You might also like
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Kecamatan Sooko Dalam Angka 2022Document152 pagesKecamatan Sooko Dalam Angka 2022alexanNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Wa0041Document2 pagesWa0041Muthu KumarNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Tutorial Collection SimpleDocument11 pagesTutorial Collection SimplerallupymeyraldoNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hydro Corr TestDocument19 pagesHydro Corr TestPramoth NarashimmanNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Module II - Value Chain AnalysisDocument72 pagesModule II - Value Chain AnalysisloganathprasannaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Blockchain Unconfirmed Transaction Hack ScriptDocument10 pagesBlockchain Unconfirmed Transaction Hack ScriptPrecious Clement100% (4)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Commercial InvoiceDocument4 pagesCommercial InvoiceHenry SilvaNo ratings yet
- Ritter Insurance Broker PresentationDocument10 pagesRitter Insurance Broker Presentationritter.roNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- 5 Energy ManagementDocument1 page5 Energy ManagementDibyo SetiawanNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Workshop On Previewing - CECARDocument12 pagesWorkshop On Previewing - CECARestefaany tejada100% (2)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Gallipoli Diary, Volume 2 by Hamilton, Ian, 1853-1947Document191 pagesGallipoli Diary, Volume 2 by Hamilton, Ian, 1853-1947Gutenberg.orgNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Dissertation Fight ClubDocument5 pagesDissertation Fight ClubWriteMyPaperForMeCheapAlbuquerque100% (1)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- CH 9 Radical Reactions 1Document19 pagesCH 9 Radical Reactions 1Darth VADERNo ratings yet
- Paediatrica Indonesiana: Ari Kurniasih, Guslihan Dasa Tjipta, Muhammad Ali, Emil Azlin, Pertin SianturiDocument6 pagesPaediatrica Indonesiana: Ari Kurniasih, Guslihan Dasa Tjipta, Muhammad Ali, Emil Azlin, Pertin SianturiHarry FebryantoNo ratings yet
- International Financial Regulation Seminar QuestionsDocument2 pagesInternational Financial Regulation Seminar QuestionsNicu BotnariNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- My Beamer TalkDocument85 pagesMy Beamer TalkOtmane El ouardiNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Lecture 9Document26 pagesLecture 9Tesfaye ejetaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Noc20-Cs53 Week 04 Assignment 02Document4 pagesNoc20-Cs53 Week 04 Assignment 02Modicare QuiteNo ratings yet
- Part 1b - Selection and Literature Review of A CultureDocument3 pagesPart 1b - Selection and Literature Review of A Cultureapi-535208903No ratings yet
- Asgkit Coding STDDocument10 pagesAsgkit Coding STDDavid ZamudioNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Negative Effects of Social Media AddictionDocument2 pagesNegative Effects of Social Media AddictionTubagus Fikih AriansyahNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- 2014-05-13-VGT Press Release - Swiss SigningDocument1 page2014-05-13-VGT Press Release - Swiss SigningSwissmissionEUNo ratings yet
- Soalan Tugasan 2 HBEC4403 OUMDocument7 pagesSoalan Tugasan 2 HBEC4403 OUMTutor EvonNo ratings yet
- DX11 Effects in Metro 2033Document47 pagesDX11 Effects in Metro 2033test23No ratings yet
- Coverpage BLDG Projects F.Y. 2021Document4 pagesCoverpage BLDG Projects F.Y. 2021Adrian PachecoNo ratings yet
- Open CVDocument11 pagesOpen CVXavier Ibarra CorteNo ratings yet
- WJ 3 Inch Lift InstallDocument3 pagesWJ 3 Inch Lift InstallGuilleNo ratings yet
- Algorithm and FlowchartsDocument9 pagesAlgorithm and FlowchartsNambashisha RyngksaiNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Project Sr. AccountantDocument3 pagesProject Sr. Accountantraisiqbal11No ratings yet
- Gun TypesDocument125 pagesGun Typesdewaaaaa-76100% (2)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)