Professional Documents
Culture Documents
2automated Confrontation Test
Uploaded by
lady1605Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2automated Confrontation Test
Uploaded by
lady1605Copyright:
Available Formats
Optometry (2007) 78, 390-395
Comparison of an automated confrontation testing device
versus finger counting in the detection of field loss
Sherry J. Bass, O.D., Jeffrey Cooper, O.D., M.S., Jerry Feldman, Ph.D.,
and David Horn, O.D.
State University of New York State College of Optometry, New York, New York.
KEYWORDS
Confrontation visual
field testing;
Visual field screening;
Perimetry;
Glaucoma;
Automated
confrontation test;
Visual field defects
Abstract
PURPOSE: The aim of this study was to compare an automated confrontation visual field testing (ACV)
device with traditional finger-counting confrontation visual field testing (FCV).
METHODS: Forty-five eyes of 45 subjects with glaucoma, 5 eyes of 5 subjects with neurologic disease
and 15 eyes of 15 normal subjects (age matched to the subjects with glaucoma by frequency) were
tested on both ACV and FCV. All subjects with glaucoma and neurologic disease had visual field loss
on white-on-white Humphrey perimetry (HVF). The FCV was performed in 8 meridians in a normally
lighted room, whereas ACV was performed in a darkened room. The ACV device consisted of a black
rectangular box with 4 1.0-mm red light-emitting diodes at each corner and a fixation hole at the center.
Four automated randomized presentations were presented, and the subject was asked to identify the
number of red lights seen (from 1 to 4). Any point missed on any of the presentations on either test was
recorded as a failure.
RESULTS: All normal subjects passed both tests. FCV detected field loss in 33.0% of glaucomatous
eyes, whereas ACV detected field loss in 58% of glaucomatous eyes (P ! 0.001). Subjects with
glaucoma who passed FCV but failed ACV had an average mean deviation of "7.77 dB on HVF,
compared with subjects who failed both FCV and ACV, who had an average mean deviation of "19.74
dB on HVF (P ! 0.001). All subjects with absolute visual field loss because of advanced glaucoma or
neurologic disease failed both tests. No subject who passed ACV failed FCV.
CONCLUSIONS: Gross confrontation visual field testing using an automated testing device has a greater
sensitivity in the detection of moderate visual field loss than finger counting confrontation visual fields.
Optometry 2007;78:390-395
Determination of visual field loss is an important part of
a comprehensive eye examination. Routine threshold or
screening visual fields, which are time consuming, have not
been shown to be cost effective because of their relatively
low detection rates. On the other hand, gross confrontation
visual field testing is rapid and inexpensive to perform and
Corresponding author: Sherry J. Bass, O.D., SUNY College of Optometry, 33 West 42nd Street, New York, New York 10036.
E-mail: sbass@sunyopt.edu
has thus been designated as an essential part of a comprehensive eye examination.1
Gross confrontation visual field testing has not been
standardized, because clinicians tend to vary targets or
testing techniques.2 Targets have included fingers (either
stationary or oscillating), the palms of the hand, the examiners face, and illuminated white or colored stimuli. Presentation of stimuli may be kinetic or static, involve 1
quadrant at a time, or have simultaneous presentation in 2
quadrants. Some clinicians present 1 target in 1 quadrant,
whereas others use a multitude of targets; some test close to
1529-1839/07/$ -see front matter 2007 American Optometric Association. All rights reserved.
doi:10.1016/j.optm.2006.06.019
Bass et al
Issue Highlight
the visual axis, whereas others test the whole central field.
The testing distance may also vary from clinician to clinician and from subject to subject.
Johnson and Baloh3 compared the sensitivity and specificity of confrontation visual fields using wiggling or oscillating fingers presented simultaneously in opposing visual
hemifields with automated static perimetry. They found that
the sensitivity of confrontation visual field testing depended
on the type of visual field defect present. For example,
sensitivity was high for altitudinal field loss, central scotoma, and homonymous hemianopias but was poorer in
detecting arcuate scotomas (typically found in glaucomatous field loss) and bitemporal hemianopsia.
Shahinfar et al.4 performed confrontation visual field
testing using oscillating fingers in opposing quadrants,
which they also compared with automated perimetry. They
reported that confrontation visual field testing was relatively
insensitive to mild to moderate visual field defects (!26 dB
defect on automated perimetry). Sensitivity was high for
altitudinal and hemianopic defects but not as good for
arcuate scotoma.
In both of the previous studies, the specificity was high;
thus, when a field defect was identified, it was a true defect.
However, confrontation visual field testing using fingers
failed to detect the visual field defect in the majority of
patients who did not have dense visual field defects, or who
had arcuate field loss, as would be found in glaucoma.
Visual field defects caused by chiasmal and postchiasmal
lesions, which typically are dense, were easy to detect.
Confrontation visual field testing is not standardized, is
subject to examiner variability and choice of testing stimulus, and has been shown to be insensitive to shallow field
loss.
With this in mind, one of the authors of this study (J.C.)
designed the Automated Confrontation Visual Field Tester
(ACV). The ACV is cost effective and simple to use,
requiring very little training or experience. Because it is
automated, examiner variability is not as much of an issue
as it is with finger-counting or finger-oscillation confrontation visual field testing. The ACV also makes use of red
diodes as stimuli. The basis for the use of red targets lies in
the work of others.
Pandit et al.5 compared 7 methods of confrontation
visual field testing against the results achieved with static
automated perimetry in patients with small or shallow field
loss. These methods included the use of the examiners face,
quadrant finger counting, kinetic finger moving, red color
comparison, and kinetic red and white targets. They found
the most sensitive confrontation method was examination of
the central 20 degrees using a small (5 mm) red target.
Trobe et al.6 investigated the use of saturation differences in
red squares presented simultaneously in 2 separate quadrants and compared this method with finger counting in
chiasmal hemianopic and nerve fiber layer defects. Although the sensitivity of the red targets was double that of
finger counting for the chiasmal defects, color targets were
only slightly more accurate than finger counting in the
391
detection of nerve fiber bundle defects. Other studies have
found that small red objects are more sensitive in the
detection of both neurologic and glaucomatous field loss.7-9
The purpose of the current study was to determine
whether the ACV, with its automated program and small red
stimuli, would improve the detection rate of visual field loss
in subjects with glaucoma with established, reproducible
visual field loss on automated perimetry, using Humphrey
Visual Field (HVF) testing compared with gross confrontation visual field testing using finger-counting field testing
(FCV). It was also compared with FCV in patients with
absolute field loss (neurologic disease) and in normal subjects with no visual field loss.
Methods
After the approval of this study by the Institutional Review
Board (IRB) of the State University of New York (SUNY)
State College of Optometry for the protection of human
subjects, patients with glaucoma and patients with neurologic field loss were identified by screening records from the
Glaucoma and Neurology Clinics, respectively. Normal
subjects were recruited from the college community. All
subjects read and signed consent forms.
Forty-five eyes of 45 subjects with a diagnosis of glaucoma and visual field loss on HVF standard automated
perimetry (SAP), 5 eyes of 5 subjects with neurologic field
loss on HVF, and 15 eyes of 15 normal subjects (25 to 55
years of age) with no visual field loss on HVF were tested
and were age matched to the subjects with glaucoma by
frequency. The neurologic conditions of the subjects in the
group with neurologic field loss included anterior ischemic
optic neuropathy, cerebrovascular accident, and head
trauma secondary to motor vehicle accidents. These subjects were free of dense media opacities, retinal disease, and
glaucoma. Subjects in the glaucoma group with glaucomatous field loss who had dense media opacities, retinal
disease, or optic nerve disease (other than glaucoma) were
excluded from the study. Any children younger than 18
years were also excluded from the study. All normal subjects were examined and were free of any ocular disease.
Any subject deemed normal (free of ocular disease) who
had an unreliable or abnormal HVF result was also excluded
from the study.
The 3 visual field tests that were used in this study are
detailed below.
HVF (Humphrey SITA 24-2)
Swedish Interactive Threshold Algorith (SITA) Standard
HVF 24-2, white-on-white, HVF tests were performed previously on both the subjects with glaucoma and subjects
with neurologic disease who participated in this study. All
HVF tests had been performed within a 3-month period
before the subject was tested with FCV and the ACV.
392
Optometry, Vol 78, No 8, August 2007
Normal subjects were tested using the HVF 24-2 SITA Fast
program after FCV and ACV. We chose the fast strategy to
confirm that the normal subjects did not have any field
defects. Subjects with disease had already had SITA Standard visual fields performed as a part of their clinical care.
FCV (finger-counting field testing)
Traditional finger-counting gross confrontations was performed with the examiner seated 60 cm from the subject at
the subjects eye level in a well-lit room. Subjects were
instructed to occlude the left eye and look at the examiners
left eye with the right eye. The examiner held up 1 or 2
fingers using 1 or both hands in 4 quadrants (inferotemporal,
inferonasal, superotemporal, and superonasal) midway between the examiner and the subject. This was originally
performed with fingers presented in 1 quadrant only and
then 2 quadrants simultaneously. The subjects were asked to
count the number of fingers seen. The same procedure was
also performed on the left eye (if both eyes were being
tested) by having the subject look at the examiners right
eye with the left eye. A failure was recorded when the
subject missed 1 or more fingers on any of the presentations.
Only a pass or fail was recorded, not the location of the
defect. There were 3 different examiners, but all performed
the testing as directed by a set of detailed written instructions.
ACV (automated confrontation field testing)
The ACV device consisted of a black box that measured 12
cm by 17 cm. Four 1.0-mm red light-emitting diodes
(LEDs) were positioned 11.25 cm apart, which resulted in
an angular separation of 15 at 60 cm. A peephole located
in the center served as a fixation point for the subject and a
fixation monitor for the examiner (see Figure 1). The stimulus
size and color red were chosen because small red objects
have been shown to be most sensitive in the detection of
both neurologic and glaucomatous field loss.6-8 The place-
Figure 1
The automated confrontation field tester.
Figure 2
Examination of a subject using the ACV field tester.
ment of the LEDs was positioned so they could be easily
seen by a normal subject in all of the 4 quadrants.
The subject was seated in a darkened room with the left
eye occluded and instructed to look at the central peephole
with the right eye. The examiner sat at a distance of 60 cm
and viewed the subject through the central peephole to
ascertain fixation (see Figure 2). At this testing distance, the
stimuli, which were 11.25 cm apart, tested the central 15.
The examiner then pressed a button to randomly present
from 1 to 4 of the LEDs. Because the device was automated,
the examiner had no control over the number and position of
the lights that were presented during each trial. The subject
then reported the number of lights seen. The examiner then
recorded the subjects responses based on the red diodes
that lit up on the rear panel of the device (see Figure 3). If
the subjects response was correct, another presentation was
performed until 4 presentations were completed. If the
subject missed 1 or more of the stimuli, the subject was then
asked to state the location of the lights seen, to ascertain
which stimuli were missed for purposes of recording the
responses on a recording sheet (see Figure 4). However, in
all, only 4 presentations were performed in total per eye.
After the right eye was tested, the subject then occluded the
right eye, and the left eye was tested. Missing any light
Figure 3
Examiners view of the LED pattern seen by the patient.
Bass et al
Issue Highlight
393
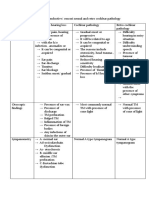
Table 2 Ability (percent failed) of automated
confrontation testing (AC) to identify visual field
abnormalities in a glaucomatous population
HVF
Figure 4
The recording form for the ACV tester. Seen stimuli were
circled; missed stimuli had an x drawn through the spot.
presented during any of the 4 trials per eye constituted a
failure.
All subjects who participated were tested initially with
FCV followed immediately by the ACV. This order of
testing was maintained because the study subjects with
glaucoma or neurologic disease had already had FCV and
HVF performed during the treatment of their glaucoma, or
to identify a neurologic disease, and within 3 months of
their participation in this study. To maintain consistency of
testing order, the normal subjects were also tested first with
FCV and then with the ACV.
For the subjects with glaucoma and for the normal
subjects, an unbiased examiner blind to each subjects
identity and disease status reviewed all visual field results
separate from any other testing results and classified the
HVF as glaucomatous or normal. This was done to ascertain
the accuracy of the HVF in identifying a pattern of field loss
associated with ocular disease and to remove bias from
knowing which subjects had disease and which subjects
were normal.
Results
Ability (percent failed) of FCV to identify visual
field abnormalities in eyes of a glaucomatous
population
FCV detected visual field loss in 33% of glaucoma eyes
with glaucomatous field loss on Humphrey visual fields (see
Table 1). The other 67% of glaucoma eyes passed FCV
testing. All normal eyes did not have visual field loss on
Humphrey visual fields and also passed FCV (i.e., no
failures). These findings were statistically significantly different from chance (Chi-square corrected, df # 1, P !
0.001, Phi-square # 0.11the phi coefficient is a measure
of the extent of association or relation between 2 sets of
Table 1 Ability (percent failed) of finger-counting (FC)
visual field testing to identify visual field abnormalities in a
glaucomatous population
Failed
Passed
Glaucoma
Normal
58
42
0
100
attributes measured on a nominal scale and is similar in
meaning to Pearsons correlation coefficient r).
Ability (percent failed) of ACV to identify visual
field abnormalities in eyes of a glaucomatous
population
ACV detected visual field loss in 58% of glaucomatous eyes
in subjects with glaucomatous field loss as determined by
HVF (see Table 2). The other 42% of glaucomatous eyes
passed ACV. All normal eyes did not have a visual field loss
on Humphrey visual fields and also passed ACV (i.e., no
failures). These findings were statistically significantly different from chance (Chi-square corrected, df # 1, P !
0.001, Phi-square # 0.26).
Percentage of agreement between FCV and ACV
for glaucomatous eyes
Of all the glaucoma eyes tested, 55% failed both FCV
and ACV; the remaining 45% of eyes failed only ACV.
No eyes that passed ACV failed FCV (0%), whereas all
eyes (100%) that passed ACV also passed FCV (see
Table 3). These findings were statistically significantly different from chance (Chi-square corrected, df # 1, P ! 0.001,
Phi-square # 0.43).
Percentage of agreement between an independent
observer and HVF results for glaucomatous and
normal eyes
An independent observer, blind to the disease status of the
subjects, categorized each visual field as glaucomatous or
normal. Glaucomatous visual field loss was identified cor-
Table 3
Percentage of agreement between AC and FC
AC
HVF
Failed
Passed
Glaucoma
Normal
33
67
0
100
FC
Failed
Passed
Failed
Passed
55
45
0
100
394
Optometry, Vol 78, No 8, August 2007
Table 4 Percentage of agreement: independent observer
and HVF assessment
Independent observer
HVF
Glaucoma
Normal
Glaucoma
Normal
95
5
8
92
rectly for 95% of eyes. Five percent of fields of the glaucomatous eyes were deemed to be normal. Ninety-two
percent of normal visual fields from the 15 eyes of the
normal patients were identified correctly, whereas 8% of
these visual fields were categorized as being glaucomatous
(see Table 4). These findings were not statistically significantly different from chance (McNemar, P ! 0.579), meaning there was no difference between assessment of disease
state by HVF and by the independent observer.
The overall difference in HVF mean deviation (MD)
among all subjects with glaucoma classified by the independent observer as either having a significant glaucomatous
HVF defect (MD # "11.73, SD # 7.60) or not (MD #
"1.43, SD # 1.63) was statistically significant. (Wilcoxin
matched Pairs, t # 27, P ! 0.001.)
Average of the mean deviation on HVF of
glaucomatous eyes detected with FCV versus ACV
The average of the mean deviation on HVF was determined
and compared among 3 groups of subjects with glaucoma.
For those subjects passing both FCV and ACV, the average
of the mean deviation on HVF was "7.03 dB, SD # 5.37,
N # 21 eyes. For those subjects failing both FCV and ACV,
the average of the mean deviation on HVF was "19.74 dB,
SD # 6.35, N # 14 eyes. For the group of subjects who
passed FCV and failed ACV, the average of the mean
deviation on HVF was "7.77 dB, SD # 4.01, N # 10 eyes
(see Figure 5). There were no subjects who passed ACV and
failed FCV; hence, there was no fourth group. An analysis
of variance (ANOVA) between these 3 independent groups
was statistically significant (F [2,42] # 25.38, P ! .001).
Tukey HSD paired comparison post hoc tests found statistically significant differences between 2 paired comparisons: (1) subjects who passed both tests versus those who
failed both tests (P ! 0.001) and (2) subjects that failed the
ACV but passed the FCV versus those that failed both tests
(P ! 0.001).
Percentage of agreement between HVF, ACV, and
FCV in eyes with neurologic field loss
Both FCV and ACV detected field loss in 100% of eyes
with neurologic field loss on HVF. There was, therefore,
100% agreement (1) between HVF loss and FCV testing, (2)
Figure 5
Graph comparing the average mean deviation on HVF with 3
groups of subjects: those who passed ACV and FCV (PASS/PASS), those who
failed ACV and failed FCV (FAIL/FAIL), and those who failed ACV but passed
FCV (FAIL/PASS).
between HVF loss and ACV testing, and (3) between FCV
and ACV.
Discussion
Gross confrontation visual field testing using large targets,
such as finger counting, will identify only large dense visual
field defects. To detect smaller relative scotomas, a confrontation visual field test has to have greater sensitivity. The
ACV in this study (which was comprised of small, red
targets separated by 15, a technique similar to the best
confrontation visual test suggested by Pandit et al.5) was
able to detect visual field defects more often than traditional
gross confrontation visual field testing with fingers. Our
results are similar to those of Pandit et al.5 who found that
the most sensitive method of visual field screening in
patients with shallow field loss was examination of the
central 20 using a small red target.
Lee et al.10 used a red laser pointer target projected onto
a tangent screen as a stimulus for gross confrontation visual
fields in patients with defects on automated perimetry.
Kinetic presentation of stimuli was followed by a static,
randomized presentation that straddled both vertical and
horizontal meridians, areas around the blind spot, in each
quadrant, and near central fixation. The average test time
was 1.5 minutes per eye. They reported a sensitivity of 73%
for the laser pointer versus 31% for finger-counting visual
fields. The ACV in the current study showed a sensitivity of
58% versus 33% for finger-counting visual fields. Although
the sensitivity of using the laser pointer visual field screening was 15% higher than using our ACV (73% for the laser
pointer versus 58% for the ACV), the ACV does not require
a tangent screen.
All normal subjects passed both FCV and ACV. When a
visual field defect was identified with either test, it was a
Bass et al
Issue Highlight
real defect, i.e., both tests had a specificity of 100%.
These results are similar to those of other previously described studies3,4 that reported a high specificity in patients
having various ophthalmologic and neurologic disorders
using finger-counting confrontation with simultaneous presentation in opposing quadrants.
The ACV had a greater rate of detection of visual field
loss in subjects with glaucoma compared with FCV. This is
likely because of the use of small red diodes that have been
shown in previously mentioned studies to increase sensitivity.5,10 The ACV was also more sensitive for glaucomatous
loss with a lower average mean deviation on Humphrey
visual field testing compared with FCV. Therefore, the
ACV detected moderate glaucomatous damage earlier in the
disease than with FCV. FCV only detected visual field loss
in advanced glaucomatous eyes and in patients with neurologic disease with high average mean deviation and deeper,
absolute field loss. It should be noted that subjects with very
early glaucomatous visual field loss (low average mean
deviation) passed both FCV and ACV testing. However, as
seen in Figure 5, the average MD on HVF of the group of
subjects who passed FCV but failed ACV was only slightly
greater than those glaucomatous subjects who passed both
ACV and FCV ("7.77 dB vs. "7.03 dB, respectively).
This study did not address the ability of the ACV to
correctly identify the location of a field defect. The purpose
of this study was to evaluate the ability of the ACV to
screen both neurologic and glaucoma defects. In clinical
application, missing any presentation (regardless of the
location) would alert the clinician to perform a more sensitive threshold visual field test.
The light weight and portability of the ACV make it ideal
for use in underdeveloped countries where the cost of
automated testing devices precludes visual field testing. Its
main advantage is the standardized way stimuli are presented. It runs on a 9-volt battery and does not require
access to electricity. It is smallabout the size of a calculatorand takes up little space. It is simple to manufacture,
costs little, is easy to use, and requires minimal training. The
ACV, therefore, may offer an advantage in disease detection
in countries that have little or no resources for the implementation of sophisticated visual field testing. To determine
whether the ACV would be useful in such settings, it would
be appropriate to test it on a mission like those done by
VOSH (Volunteer Optometric Services to Humanity).
In developed countries, where the standard of care is
confrontation visual field testing, this device may better
395
detect more relative visual field loss. We recognize that a
full visual field screening would likely be more effective in
the detection of relative visual field loss. However, full
visual field screenings are not the standard of care on every
patient, take several minutes to perform, and are not cost
effective.
Conclusions
The ACV is a fast method for performing gross confrontation visual fields and shows greater sensitivity in a small
group of subjects with glaucomatous field loss compared
with gross confrontation testing using finger counting.
The ACV, like FCV, will detect dense or absolute visual
field loss in patients with neurologic disease and advanced
glaucoma, but ACV has the additional advantage over FCV
in the ability to better detect relative visual field loss, as may
be found in moderate glaucoma. The design, portability, and
ease of use of the ACV make it a useful and sensitive
confrontation visual field testing device serving clinical
settings in both underdeveloped and developed countries.
References
1. American Optometric Association Consensus Panel. Comprehensive
Adult Eye and Vision Examination. Optometric Clinical Practice
Guideline 1994; p. 7.
2. Elliott DB, North I, Flanagan J. Confrontation visual field tests.
Ophthal Physiol Opt 1997;17(suppl 2):S17-S24.
3. Johnson LN, Baloh FG. The accuracy of confrontation visual field test
in comparison with automated perimetry. J Natl Med Assoc 1991;
83(10):895-8.
4. Shahinfar S, Johnson LN, Madsen RW. Confrontation visual field loss
as a function of decibel sensitivity loss on automated static perimetry.
Ophthalmol 1995;102:872-7.
5. Pandit RJ, Gales K, Griffiths PG. Effectiveness of testing visual fields
by confrontation. Lancet 2001;358(9290):1339-40. Erratum in: Lancet
2001;358(9295):1820.
6. Trobe JD, Acosta PC, Krischer JP. Confrontation visual field techniques in the detection of anterior visual pathway lesions. Ann Neurol
1981;10:28-34.
7. Mandahl A. Red square test for visual field screening. A sensitive and
simple bedside test. Acta Ophthalmol (Copenh) 1994;72(6):683-7.
8. Reader AL, Harper DG. Confrontation visual-field testing. JAMA
1976;236(3):250.
9. Vandeveer MR, Norden L. Visual fields: simplified screening and
recording procedures. J Am Optom Assoc 1983;54(5):457-64.
10. Lee MS, Balcer LJ, Volpe NJ, et al. Laser pointer visual screening.
J Neuroophthalmol 2003;23(24):260-3.
You might also like
- Dsadsgfdsgfjhhgkjh LK JfgtdsDocument1 pageDsadsgfdsgfjhhgkjh LK Jfgtdslady1605No ratings yet
- Bipolar DisorderDocument63 pagesBipolar DisorderRichard Martin100% (2)
- Gambar Spinal CordDocument1 pageGambar Spinal Cordlady1605No ratings yet
- Van HerickDocument4 pagesVan HerickcmirceaNo ratings yet
- Produksi Aquos HumorDocument31 pagesProduksi Aquos Humorlady1605No ratings yet
- Eye Movements Are Controlled by Muscles Innervated by Cranial Nerves IIIDocument3 pagesEye Movements Are Controlled by Muscles Innervated by Cranial Nerves IIIlady1605No ratings yet
- file:///C:/Users/user/Downloads/C123 - 1781-1794.pdf Overview#a2Document2 pagesfile:///C:/Users/user/Downloads/C123 - 1781-1794.pdf Overview#a2lady1605No ratings yet
- Blood Retina BarrierDocument4 pagesBlood Retina Barrierlady1605No ratings yet
- Retinopatia DiabéticaDocument5 pagesRetinopatia Diabéticalady1605No ratings yet
- 3 Stroke-2006-Singer-2726-32Document8 pages3 Stroke-2006-Singer-2726-32lady1605No ratings yet
- J Neurol Neurosurg Psychiatry 2008 Jankovic 368 76Document10 pagesJ Neurol Neurosurg Psychiatry 2008 Jankovic 368 76Wijaya BudiNo ratings yet
- Parkinson's Disease ReferencesDocument2 pagesParkinson's Disease Referenceslady1605No ratings yet
- Community Nutrition Assignment by Fransisca Stephanie, 030 10 109, Medical TrisaktiDocument5 pagesCommunity Nutrition Assignment by Fransisca Stephanie, 030 10 109, Medical Trisaktilady1605No ratings yet
- Fruits and Vegetables Consumption Pattern in School Children Ni Made Dewantari Dan Ari Widiani Abstract. Food Consumption in School Children Is Determined by Their FoodDocument7 pagesFruits and Vegetables Consumption Pattern in School Children Ni Made Dewantari Dan Ari Widiani Abstract. Food Consumption in School Children Is Determined by Their Foodlady1605No ratings yet
- ASTMA and AlergicDocument11 pagesASTMA and Alergiclady1605No ratings yet
- ObeseDocument29 pagesObeselady1605No ratings yet
- 905 FullDocument8 pages905 FullJupiter CarlNo ratings yet
- LalaDocument2 pagesLalalady1605No ratings yet
- Preeclampsia JOCC PDFDocument52 pagesPreeclampsia JOCC PDFindahsaviNo ratings yet
- RM 10015Document6 pagesRM 10015lady1605No ratings yet
- Buat NenengDocument2 pagesBuat Nenenglady1605No ratings yet
- Water BirthDocument5 pagesWater Birthlady1605No ratings yet
- Dafpus ManuskripDocument1 pageDafpus Manuskriplady1605No ratings yet
- Waterbirth ReviewDocument6 pagesWaterbirth Reviewlady1605No ratings yet
- Abs TrakDocument2 pagesAbs Traklady1605No ratings yet
- Jessie Liu ThesisDocument104 pagesJessie Liu Thesislady1605No ratings yet
- Daftar Pustaka Lupus NefritisDocument1 pageDaftar Pustaka Lupus Nefritislady1605No ratings yet
- Tabel ChiquareDocument8 pagesTabel Chiquarelady1605No ratings yet
- BMJ Open 2011 FinlayDocument26 pagesBMJ Open 2011 Finlaylady1605No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 2.1 Tutorial Task 6 & 7Document19 pages2.1 Tutorial Task 6 & 7ENOCH NAPARI ABRAMANNo ratings yet
- The Importance of Diversity On Congitive NeuroscienceDocument11 pagesThe Importance of Diversity On Congitive NeuroscienceMarlon ChaconNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaMelly SaNo ratings yet
- Acute Intermittent Porphyria - Clinicopathologic Correlation - Report of A Case and Review of The Literature (1997)Document7 pagesAcute Intermittent Porphyria - Clinicopathologic Correlation - Report of A Case and Review of The Literature (1997)Triple ANo ratings yet
- Psychology 2 KeyDocument6 pagesPsychology 2 KeyvictorybNo ratings yet
- Attenuation of 3,4-Methylenedioxymethamphetamine (MDMA) Induced Neurotoxicity With The Serotonin Precursors Tryptophan and 5-HydroxytryptophanDocument6 pagesAttenuation of 3,4-Methylenedioxymethamphetamine (MDMA) Induced Neurotoxicity With The Serotonin Precursors Tryptophan and 5-HydroxytryptophanflaminglawyerNo ratings yet
- Autonomic Nervous System OverviewDocument35 pagesAutonomic Nervous System OverviewDr. R. PeriasamyNo ratings yet
- 2 Myasthenia Gravis and MS 2Document50 pages2 Myasthenia Gravis and MS 2Rawbeena RamtelNo ratings yet
- The Use of The Cambridge Neuropsychological Test ADocument12 pagesThe Use of The Cambridge Neuropsychological Test ARafael MartinsNo ratings yet
- James Carter US Olympic Team Track & Field: Amitabh Bachchan Indian ActorDocument22 pagesJames Carter US Olympic Team Track & Field: Amitabh Bachchan Indian ActorSri KombongNo ratings yet
- FRQ Vocabulary ReviewDocument1 pageFRQ Vocabulary ReviewDrew AbbottNo ratings yet
- Growth and Development Theories ExplainedDocument105 pagesGrowth and Development Theories ExplainedAjmal Najeeb50% (2)
- Sistemas Atencionales y NegligenciaDocument6 pagesSistemas Atencionales y NegligenciacamiajoNo ratings yet
- RRL For PrecisDocument4 pagesRRL For PrecisDea SantellaNo ratings yet
- Case Study - Brain Tumor FINALDocument41 pagesCase Study - Brain Tumor FINALJaneeh Miranda67% (6)
- Short Case Hydrocephalus: by Febrianto Haba Bunga, S.Ked Consultant DR .Donny Argie, SP - BSDocument29 pagesShort Case Hydrocephalus: by Febrianto Haba Bunga, S.Ked Consultant DR .Donny Argie, SP - BSErkoNo ratings yet
- Clinical Pathways in Stroke RehabilitationDocument284 pagesClinical Pathways in Stroke RehabilitationArturo Valverde AmpaiNo ratings yet
- 267 Impulses Serving Pain Sensation in The Left Foot Are RelayedDocument12 pages267 Impulses Serving Pain Sensation in The Left Foot Are RelayedNathanNo ratings yet
- German Neurologist On Face Masks Oxygen Deprivation Causes Permanent Neurological Damage PDFDocument4 pagesGerman Neurologist On Face Masks Oxygen Deprivation Causes Permanent Neurological Damage PDFOpieNo ratings yet
- Vision Screening Form DepedDocument3 pagesVision Screening Form DepedAbigael Abac RiveraNo ratings yet
- Selective mutism-DSM-5-233-235Document3 pagesSelective mutism-DSM-5-233-235Mella IntaniabellaNo ratings yet
- Cook and Plisky - Balance, Posture and MovementDocument57 pagesCook and Plisky - Balance, Posture and MovementFlávio Garrett100% (1)
- Projecting Sensations To External Objects: Evidence From Skin Conductance ResponseDocument8 pagesProjecting Sensations To External Objects: Evidence From Skin Conductance ResponseappanagNo ratings yet
- Hearing Losses and Assocated CorealtesDocument3 pagesHearing Losses and Assocated CorealtesAchu SachuNo ratings yet
- Filippi Assessment Lesions MRI in MSDocument18 pagesFilippi Assessment Lesions MRI in MSAlfonso LemaNo ratings yet
- CHCDIS007 STUDENT WORKBOOK (WORD) - C4A.v1.1Document86 pagesCHCDIS007 STUDENT WORKBOOK (WORD) - C4A.v1.1shrestha31dristi100% (2)
- The Healy Programs Full List-0001Document15 pagesThe Healy Programs Full List-0001Vikram SharmaNo ratings yet
- Gestalt TheoryDocument3 pagesGestalt TheoryDiane Marie Ibañez100% (1)
- Attention Deficit/ Hyperactivity Disorder: Changes To The DisorderDocument2 pagesAttention Deficit/ Hyperactivity Disorder: Changes To The DisorderGemanDuenasNo ratings yet
- Mirroring People The Science of Empathy and How We Connect With OthersDocument330 pagesMirroring People The Science of Empathy and How We Connect With Othersggg3141550% (2)