Professional Documents
Culture Documents
Dysgerminoma - Arare Ovarian Tumour - Case Report
Uploaded by
IOSRjournalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dysgerminoma - Arare Ovarian Tumour - Case Report
Uploaded by
IOSRjournalCopyright:
Available Formats
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 8 Ver. VI (Aug. 2015), PP 34-37
www.iosrjournals.org
Dysgerminoma Arare Ovarian Tumour - Case Report
Dr.Nidhi Dahiya; Dr.VeenaAseeja; Dr. JayatiNath
Abstract: Dysgerminoma, germ cell tumors (GCTs) are rare, comprising approximately 20% of all ovarian
tumors, both benign and malignant occurring at extremes of age groups. Approximately 3-5% of ovarian GCTs
are malignant.[1] In fact, dysgerminomas make up two thirds of all malignant ovarian neoplasms in women
younger than 20 years. Moreover, once diagnosed, dysgerminomas respond highly to the prescribed treatments,
rescuing patients from infertility and early mortality[1].Extraovarian tumor spread of dysgerminomas often
involves the retroperitoneal and pelvic lymph nodes; these tumors are highly susceptible to radiotherapy[2]. In
addition, hematogenous spread may occur; common sites of involvement are the lungs, liver, and
bone[3].Details of the case:-A 17 yrs old, unmarried girl , came to our institute on 21/4/15 with chief
complaints of pain abdomen, left side, since 1 year, associatiatedwith history of feeling of lump in abdomen
which was increasing in size since then.Not associated with nausea, vomiting, or menstrual complaints ,or
urinary or bowel complaints. After thoroughly investigating the patient, primary cytoreductivesurgery i.estaging
laparotomy with left salpingoophorectomy with infracolicomentectomywith peritoneal biopsy was done on
29/4/2015. The patient was discharged on 9/5/2015 and was asked to come for follow up for chemotherapy. She
received 3 cycles of chemotherapy and is clinically fine.
I.
Introduction
The 3 major types of ovarian tumors being epithelial, sex cord, and germ cell. Epithelial cell tumors
represent the majority of all ovarian neoplasms (82%). Conversely, germ cell tumors (GCTs) are rare,
comprising approximately 20% of all ovarian tumors. Approximately 3-5% of ovarian GCTs are malignant. The
most common GCT is the dysgerminoma, which accounts for approximately 2% of all ovarian cancers. All
dysgerminomas are considered malignant, but only one third of dysgerminomas behave aggressively.[4]
Although rare, dysgerminomas are important irrespective of incidence because they most commonly affect
women of reproductive age (ie, < 30 y). In fact, dysgerminomas make up two thirds of all malignant ovarian
neoplasms in women younger than 20 years of age. Moreover, once they are diagnosed, dysgerminomas respond
well to treatment, potentially avoiding complications like infertility and early mortality.[1]
II.
The Case Under Discussion
A 17 yrs old, moderately built and moderately nourished, unmarried young girl, came to our institute
on 21/4/15 and was admitted under gynaecology department of MMIMSR, Mullana, Ambala, with chief
complaints of pain abdomen, left side, since 1 year,mild in intensitywith no aggreviating or relieving factor,
associated with history of feeling of lump in abdomen which was increasing in size since then, with early
satiety, with vague abdominal complaints (eg, dyspepsia, digestive disturbances.Not associated with nausea,
vomiting, or menstrual complaints ,or urinary complaints.
On admission, patients general condition was fair, BP-114/76mm of Hg, PR- 114/min, RR- 22/min.
Patient was calm, conscious and cooperative and well oriented to time, place and person .On clinical
examination:-abdomen was soft, bowel sounds were present, no organomegaly. A firm irregularly contoured
mass arising from pelvis approximately 24 weeks size of uterus, non-tender, mobile from side to side,
superficial structures like skin not adherent to the mass, with irregularities more on left margin , right border
feels smoother. Right iliac fossa felt a little free, left iliac fossa was full. Tumour seems to arise from the left
adnexa. No superficial veins visible. No scar , no sinus, normal hernia sites. She had her menarche at 13 yrs of
age, her LMP was on 13/4/15, cycles were of 3-4 days/28+-2 days, regular, average flow. She had history of
?malaria?typhoid approx. 8 months back for which she took treatment (no medical papers were available with
the patient). Rest she had no significant medical or surgical history. No family history of any type of
malignancy.
Patient was investigated.ABO Rh- O positive, Hb-11.5 gm%, BT-2.10 CT-6.15, PCV- 32.9%, Platelet
count- 2lakh, TLC- 2500/cumm, DLC-P64L30E06M00B00, ESR-20mm/1st hour, MCH- 21pg, MCV-65um3
MCHC-21G/dl. RFT- urea- 19mg/dl, creatinine-0.80mg/dl, sodium-141mEq/l,
potassium -4.5mEq/L,
chloride106 mmol/L. LFT- bilirubin (total)-0.44mg/dl, bilirubin (direct)- 0.10mg/dl, SGOT 95IU/L , SGPT32 IU/L,
DOI: 10.9790/0853-14863437
www.iosrjournals.org
34 | Page
Dysgerminoma Arare ovarian tumour - case report
ALP-315 IU/L. LDH-238.3IU/L betaHCG-33.7mIU/ml, alpha feto protein- 50.9ng/ml, CA-125- 46.7U/ml,
HIV, VDRL, HCV, HBsAg-all were non reactive.USG showed- a large mass seen in pelvis measuring 15X19
cms ?arisingfrom left adnexa and reaching upto epigastrium .Uterus and left ovary were normal. ? malignant
ovarian mass.X-Ray chest PAview-was normal.
Patient was taken up for primary cytoreductivesurgery and exploratory laparotomy with left
salpingoophorectomywith partial(infra colic)omentectomy with peritoneal biopsy was done on 29/4/2015. Intra
op findings were-(1)Left ovarian tumour mass approximately20x20 cms ?malignant / dysgerminoma taken out.
(2) Surgical spill of cyst approximately 1x1 cmsoccured.(3) liver surface and under surface of diaphragm was
found normal. No Lymph node enlargement seen.(4) peritoneal washings and sample sent for histopathology.
Figure 1 posterior surface of tumour mass with multiloculatedappearence with part of left fallopian tube.
Figure 2 anterior surface of the tumour mass.
Figure 3omentectomy specimen.
DOI: 10.9790/0853-14863437
www.iosrjournals.org
35 | Page
Dysgerminoma Arare ovarian tumour - case report
Figure 4 cut section of the tumour mass
Figure 5 Ovarian dysgerminoma histology showing syncytiotrophoblast like giant cells.(A) and (B):
Hematoxylin-eosin, x200. (C) Hematoxylin-eosin, x400. (D) Hematoxylin-eosin, x600.
The patient recovered well post operatively with triple antibiotics cover, catheter was removed onpost
operative day-2. On post operative day-9,sutures were removed and the patient was discharged under
satisfactory condition and asked to come for follow-up as advised.
Histopathology report showed-1.Dysgerminoma of left ovary. 2. Omentum shows well defined epitheloid cell
granulomas with giant cells.ZN stain using 20% H2SO4 did not reveal any acid fast bacilli. 3. Peritoneal
washings free from tumour. 4.fallopian tube free from tumour.HPE diagnosis- Pt1nXmX.
After HPE confirmation of dysgerminoma, patient was given adjuvant chemotherapy BEP regime(3 cycles) in
follow-up.
III.
Discussion
A dysgerminoma is a tumor of the ovary that is composed of primitive, undifferentiated germ cells .
Germ cell tumors arise from primordial germ cells of the ovary and the testis. Of these ovarian lesions, 97% are
benign proliferations (i.e. mature teratomas); the remaining 3% are malignant .Germ cell tumors arise from
primordial germ cells of the ovary and the testis; Though , pathogenesis of the ovarian germ cell tumors is
unknown. Of the ovarian lesions, 97% are benign proliferations (ie, mature teratomas; the remaining 3% are
malignant.[2]. The most commonly occurring GCT is the dysgerminoma, which accounts for approximately 2%
of all ovarian cancers. Dysgerminomas are the most common malignant germ cell tumor occurring in theovary ,
and these lesions are most commonly found in adolescents and young adults; in fact, approximately 60% of
cases are diagnosed in patients younger than 20 years.[3]These tumors usually present as a unilateral mass and
can occur during pregnancy.
DOI: 10.9790/0853-14863437
www.iosrjournals.org
36 | Page
Dysgerminoma Arare ovarian tumour - case report
These tumors can have rapid growth and predispose to rupture and torsion with associated acute change
in symptoms in approximately 5-10% of patients. One should always get a pregnancy test done. This test should
be mandatory in all woman of reproductive age, even at the extremes of reproductive age, who presents with
abdomino-pelvic symptoms. LAB EVALUATION elevation in LDH, although it is not elevated in all the
cases. Occasionally, dysgerminomas may become infiltrated with syncytiotrophoblastic giant cells, which
produce beta-hCG. Elevations in AFP are even less common. However, preoperative evaluation of all of these
markers is suggested in patients with suspected ovarian GCTs/dysgerminomas. In addition, serum inhibin levels
can be done in this age group. Though inhibin B seems to be more sensitive and has a greater elevation in
GCTs, inhibin A can also be elevated with inhibin B or, more rarely, without elevation of inhibin B, as sex cord
stromal tumors are also in the differential for women with pelvic masses in this age group who present. [1]
Traditionally, patients undergoing surgery for ovarian cancer often undergo a mechanical and/or
antibiotic bowel preparation before surgery.
According to current American College of Obstetricians and Gynecologists (ACOG) recommendations,
second-look laparotomies are not considered the standard of care for dysgerminomas. However, second-look
surgery should be considered for patients with persistent elevation in tumor markers, especially if abnormal
findings on posttreatment imaging are associated with.[5]
Adjuvant chemotherapy regimens:The 4 regimens for chemotherapy are as follows: (1) BEP, which is the preferred regimen; (2) methotrexate,
actinomycin D, and chlorambucil (MAC); (3) cisplatin, vincristine, and bleomycin (PVB); and (4) vincristine,
actinomycin D, and cyclophosphamide (VAC). Although the efficiency of each protocol has been analyzed, the
BEP protocol has been favored in recent years owing to high cure rates with a favorable toxicity profile.[1]
BEP protocol (generally preferred)
The protocol is as follows[6] :
Bleomycin - Maximum 30 U IV per week for 9 weeks; dose at 20 U/m 2 Etoposide (ie, VP-16) - 100 mg/m 2 on
days 1-5 q3wk for 3 courses; reduced 20% for granulocytic fever or previous radiotherapy Cisplatin - 20 mg/m
2 on days 1-5 q3wk for 3 courses.
Follow-up with a medical oncologist and/or radiation oncologist is dictated by the stage and extent of disease.
References
[1].
[2].
[3].
[4].
[5].
[6].
Michener, C.M. and Huh, W.K. (2012) Ovarian dysgerminomas. Medscape Drugs, Diseases & Procedures.
Prat J. Prat J, ed. Pathology of the Ovary. Germ cell tumors. Philadelphia, Pa: Saunders; 2004. 251-82.
Talerman A. Blaustein's Pathology of the Female Genital Tract. Kurman RJ. Germ cell tumors of the ovary. 5th ed. New York, NY:
: Springer-Verlag; 2002. 967-1034.
Gimelli S, Beri S, Drabkin HA, Gambini C, Gregorio A, Fiorio P, et al. The tumor suppressor gene TRC8/RNF139 is disrupted by a
constitutional balanced translocation t(8;22)(q24.13;q11.21) in a young girl with dysgerminoma. Molecular Cancer. 2009. 8:52-.
[Medline].
Gershenson DM, Copeland LJ, del Junco G. Second-look laparotomy in the management of malignant germ cell tumors of the
ovary. Obstet Gynecol. 1986 Jun. 67(6):789-93. [Medline].
Gershenson DM, Morris M, Cangir A, Kavanagh JJ, Stringer CA, Edwards CL. Treatment of malignant germ cell tumors of the
ovary with bleomycin, etoposide, and cisplatin. J ClinOncol. 1990 Apr. 8(4):715-20. [Medline].
DOI: 10.9790/0853-14863437
www.iosrjournals.org
37 | Page
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Role of Extrovert and Introvert Personality in Second Language AcquisitionDocument6 pagesThe Role of Extrovert and Introvert Personality in Second Language AcquisitionInternational Organization of Scientific Research (IOSR)No ratings yet
- "I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweDocument5 pages"I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweInternational Organization of Scientific Research (IOSR)No ratings yet
- Socio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanDocument7 pagesSocio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanInternational Organization of Scientific Research (IOSR)No ratings yet
- Attitude and Perceptions of University Students in Zimbabwe Towards HomosexualityDocument5 pagesAttitude and Perceptions of University Students in Zimbabwe Towards HomosexualityInternational Organization of Scientific Research (IOSR)No ratings yet
- A Proposed Framework On Working With Parents of Children With Special Needs in SingaporeDocument7 pagesA Proposed Framework On Working With Parents of Children With Special Needs in SingaporeInternational Organization of Scientific Research (IOSR)No ratings yet
- The Impact of Technologies On Society: A ReviewDocument5 pagesThe Impact of Technologies On Society: A ReviewInternational Organization of Scientific Research (IOSR)100% (1)
- A Review of Rural Local Government System in Zimbabwe From 1980 To 2014Document15 pagesA Review of Rural Local Government System in Zimbabwe From 1980 To 2014International Organization of Scientific Research (IOSR)No ratings yet
- Importance of Mass Media in Communicating Health Messages: An AnalysisDocument6 pagesImportance of Mass Media in Communicating Health Messages: An AnalysisInternational Organization of Scientific Research (IOSR)No ratings yet
- Transforming People's Livelihoods Through Land Reform in A1 Resettlement Areas in Goromonzi District in ZimbabweDocument9 pagesTransforming People's Livelihoods Through Land Reform in A1 Resettlement Areas in Goromonzi District in ZimbabweInternational Organization of Scientific Research (IOSR)No ratings yet
- Investigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehDocument4 pagesInvestigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehInternational Organization of Scientific Research (IOSR)No ratings yet
- An Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyDocument14 pagesAn Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyInternational Organization of Scientific Research (IOSR)No ratings yet
- Comparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesDocument7 pagesComparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesInternational Organization of Scientific Research (IOSR)No ratings yet
- Assessment of The Implementation of Federal Character in Nigeria.Document5 pagesAssessment of The Implementation of Federal Character in Nigeria.International Organization of Scientific Research (IOSR)No ratings yet
- Relationship Between Social Support and Self-Esteem of Adolescent GirlsDocument5 pagesRelationship Between Social Support and Self-Esteem of Adolescent GirlsInternational Organization of Scientific Research (IOSR)No ratings yet
- Edward Albee and His Mother Characters: An Analysis of Selected PlaysDocument5 pagesEdward Albee and His Mother Characters: An Analysis of Selected PlaysInternational Organization of Scientific Research (IOSR)No ratings yet
- The Lute Against Doping in SportDocument5 pagesThe Lute Against Doping in SportInternational Organization of Scientific Research (IOSR)No ratings yet
- Topic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshDocument7 pagesTopic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshInternational Organization of Scientific Research (IOSR)No ratings yet
- Role of Madarsa Education in Empowerment of Muslims in IndiaDocument6 pagesRole of Madarsa Education in Empowerment of Muslims in IndiaInternational Organization of Scientific Research (IOSR)No ratings yet
- Human Rights and Dalits: Different Strands in The DiscourseDocument5 pagesHuman Rights and Dalits: Different Strands in The DiscourseInternational Organization of Scientific Research (IOSR)No ratings yet
- Substance Use and Abuse Among Offenders Under Probation Supervision in Limuru Probation Station, KenyaDocument11 pagesSubstance Use and Abuse Among Offenders Under Probation Supervision in Limuru Probation Station, KenyaInternational Organization of Scientific Research (IOSR)No ratings yet
- Classical Malay's Anthropomorphemic Metaphors in Essay of Hikajat AbdullahDocument9 pagesClassical Malay's Anthropomorphemic Metaphors in Essay of Hikajat AbdullahInternational Organization of Scientific Research (IOSR)No ratings yet
- Beowulf: A Folktale and History of Anglo-Saxon Life and CivilizationDocument3 pagesBeowulf: A Folktale and History of Anglo-Saxon Life and CivilizationInternational Organization of Scientific Research (IOSR)No ratings yet
- Women Empowerment Through Open and Distance Learning in ZimbabweDocument8 pagesWomen Empowerment Through Open and Distance Learning in ZimbabweInternational Organization of Scientific Research (IOSR)No ratings yet
- Micro Finance and Women - A Case Study of Villages Around Alibaug, District-Raigad, Maharashtra, IndiaDocument3 pagesMicro Finance and Women - A Case Study of Villages Around Alibaug, District-Raigad, Maharashtra, IndiaInternational Organization of Scientific Research (IOSR)No ratings yet
- A Study On The Television Programmes Popularity Among Chennai Urban WomenDocument7 pagesA Study On The Television Programmes Popularity Among Chennai Urban WomenInternational Organization of Scientific Research (IOSR)No ratings yet
- Motivational Factors Influencing Littering in Harare's Central Business District (CBD), ZimbabweDocument8 pagesMotivational Factors Influencing Littering in Harare's Central Business District (CBD), ZimbabweInternational Organization of Scientific Research (IOSR)No ratings yet
- An Exploration On The Relationship Among Learners' Autonomy, Language Learning Strategies and Big-Five Personality TraitsDocument6 pagesAn Exploration On The Relationship Among Learners' Autonomy, Language Learning Strategies and Big-Five Personality TraitsInternational Organization of Scientific Research (IOSR)No ratings yet
- Designing of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesDocument5 pagesDesigning of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesIOSRjournalNo ratings yet
- Kinesics, Haptics and Proxemics: Aspects of Non - Verbal CommunicationDocument6 pagesKinesics, Haptics and Proxemics: Aspects of Non - Verbal CommunicationInternational Organization of Scientific Research (IOSR)No ratings yet
- Design Management, A Business Tools' Package of Corporate Organizations: Bangladesh ContextDocument6 pagesDesign Management, A Business Tools' Package of Corporate Organizations: Bangladesh ContextInternational Organization of Scientific Research (IOSR)No ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Castration in The Horse: by Christina Cable, DVM, Dipl. ACVSDocument5 pagesCastration in The Horse: by Christina Cable, DVM, Dipl. ACVSRavi KangNo ratings yet
- Management of Vacuum Assisted Closure TherapyDocument14 pagesManagement of Vacuum Assisted Closure TherapyVoiculescu MihaelaNo ratings yet
- Psychiatric NursingDocument2 pagesPsychiatric NursingRn nadeenNo ratings yet
- BP 2017Document6 pagesBP 2017Rafael MeloNo ratings yet
- Preparation Support Pack 180515Document69 pagesPreparation Support Pack 180515sinbad200No ratings yet
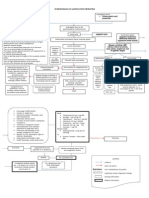
- Pathophysiology of GooDocument2 pagesPathophysiology of GooTania Noviza100% (1)
- Circulating SerotoninDocument17 pagesCirculating Serotoninnihilx27374No ratings yet
- En H PsyDocument9 pagesEn H PsyMohd IzwanNo ratings yet
- Att Reintroduction Nhs FlowchartDocument6 pagesAtt Reintroduction Nhs FlowchartNitesh Gupta100% (1)
- Respiratory System BOFDocument27 pagesRespiratory System BOFBenjamin NelsonNo ratings yet
- Fluid and ElectrolytesDocument14 pagesFluid and Electrolytesstring44100% (2)
- Faller RationaleDocument2 pagesFaller RationaleFaller TrixieNo ratings yet
- Government Gazette - 14 AugustDocument72 pagesGovernment Gazette - 14 AugustistructeNo ratings yet
- Nursing Manegmen of EQUIPMENTS in NICUDocument16 pagesNursing Manegmen of EQUIPMENTS in NICUPriyaNo ratings yet
- Clonidine HydrochlorideDocument1 pageClonidine HydrochlorideLovelyn Joy Abubo CortezNo ratings yet
- NSO Monthly Report FormDocument5 pagesNSO Monthly Report Formrose_almonteNo ratings yet
- Rachelle Manuel PobleteDocument4 pagesRachelle Manuel PobleteRachelle MondidoNo ratings yet
- Endodontic Diagnostic Terminology UpdateDocument3 pagesEndodontic Diagnostic Terminology UpdateAlyaefkageNo ratings yet
- NCM 105 Notes 5 StudentsDocument11 pagesNCM 105 Notes 5 StudentsRI NANo ratings yet
- Discharge PlanDocument5 pagesDischarge PlanDenise Louise PoNo ratings yet
- Reliability and Validity of The Turkish Version of The Job Performance Scale InstrumentDocument9 pagesReliability and Validity of The Turkish Version of The Job Performance Scale InstrumentsatmayaniNo ratings yet
- Nursing Diagnosis Rationale Interventions Rationale EvaluationDocument2 pagesNursing Diagnosis Rationale Interventions Rationale EvaluationJobie CasipongNo ratings yet
- Master of Dental Surgery in Prosthodontics Study PlanDocument2 pagesMaster of Dental Surgery in Prosthodontics Study PlanHANINo ratings yet
- Competency Based EducationDocument33 pagesCompetency Based EducationAncy Varkey100% (1)
- Chap 118Document5 pagesChap 118theodoruskevinNo ratings yet
- MDS3 Ch30 Dispensing Mar2012 PDFDocument0 pagesMDS3 Ch30 Dispensing Mar2012 PDFyiemetieNo ratings yet
- 3 - Modalities of NursingDocument6 pages3 - Modalities of NursingMark Zedrix MediarioNo ratings yet
- Ethics in Abnormal PregnanciesDocument123 pagesEthics in Abnormal PregnanciesspicylaingNo ratings yet
- Medication Therapy ManagementDocument4 pagesMedication Therapy ManagementAlexandru TibaNo ratings yet
- The Lumbar Spine: Understanding The Science Behind Both Movement and Dysfunction by Chris Gellert, PT, MMusc & Sportsphysio, MPT, CSCS, AMSDocument9 pagesThe Lumbar Spine: Understanding The Science Behind Both Movement and Dysfunction by Chris Gellert, PT, MMusc & Sportsphysio, MPT, CSCS, AMSChrisGellertNo ratings yet