Professional Documents
Culture Documents
Rheumatoid Arthritis
Uploaded by
JayricDepalobosCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rheumatoid Arthritis
Uploaded by
JayricDepalobosCopyright:
Available Formats
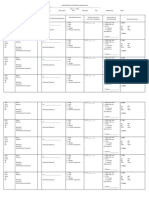
Joint Pain Module: Rheumatoid Arthritis
Definition and
Epidemiology
- It is a chronic
inflammatory
disease of unknown
etiology marked by
a symmetric,
peripheral
polyarthritis.
-
a chronic systemic
inflammatory
arthritis that may
affect many tissues
and organs but
principally attacks
the joints, producing
a nonsuppurative
proliferative and
inflammatory
synovitis that often
progresses to
destruction of the
articular cartilage
and ankylosis of the
joints.
Risk Factors
Increased incidence among:
- Females 3-5x > males
- Common in 40 to 70 years old
*NO AGE IS IMMUNE
- Age of onset usually 30 to 50
years old
Genetic Factors
- Specific HLA-DRB1 alleles
share a common sequence of
amino acids in the third
hypervariable region of the
chain shared epitope
- located in the antigen-binding
cleft of the DR molecule,
presumably the specific binding
site of the arthritogen(s) that
initiates the inflammatory
synovitis
- PTPN22 encodes a protein
tyrosine phosphatase, which
participates in activation and
control of inflammatory cells,
including T cells.
Environmental Factors
Smoking - higher citrullination of
proteins in bronchoalveolar fluid
*citrullinated proteins - enhance
the expression of a neoepitope
capable of inducing self-reactivity
Exposure to silicone dust and
mineral oil
Pathogenesis
The pathogenic
mechanisms of synovial
inflammation are likely to
result from a complex
interplay of genetic,
environmental, and
immunologic factors
produces dysregulation
of the immune system
and a breakdown in
self-tolerance.
1. initiation phase - A
variety of stimuli may
initiate the initial phase
of nonspecific
inflammation, which
may last for a
protracted period of
time with no or
moderate symptoms.
2. amplification phase When activation of
memory T cells in
response to a variety of
peptides presented by
antigen-presenting
cells occurs in
genetically susceptible
individuals
amplification of
inflammation occurs
with the promotion of
Clinical Symptoms
ARTICULAR
MANIFESTATIONS:
early morning joint
stiffness lasting more than
1 hour and easing with
physical activity
Common locations: Hands
(PIP,MCP),feet (MTP),
wrists, knees, elbows, ankles
Pattern of spread: may be
monoarticular, oligoarticular
(4 joints), or polyarticular
(>5 joints); symmetrically
additive
Usually insidious onset
Flexor tendon
tenosynovitis is a frequent
hallmark of RA and leads to
decreased range of motion,
reduced grip strength, and
trigger fingers
Ulnar deviationsubluxation of the MCP
joints, with subluxation of
the proximal phalanx to the
volar side of the hand
Swan-neck deformity
Hyperextension of the PIP
joint with flexion of the DIP
Joint Pain Module: Rheumatoid Arthritis
Bacterial antigens mycobacteria,
Borrelia, Proteus mirabilis, and
Mycoplasma
Viral antigens Epstein-Barr virus,
retroviruses, parvoviruses
local rheumatoid
factor and
other autoantibody
production and
enhanced capacity to
mediate tissue damage
3. chronic
inflammation with
tissue injury
Pathology:
Initially the synovium
becomes grossly
edematous, thickened,
and hyperplastic,
transforming its smooth
contour to one covered by
delicate and bulbous
fronds.
(1) infiltration of
synovial stroma by a
dense perivascular
inflammatory infiltrate
composed of lymphoid
aggregates (mostly
helper T cells), B cells,
plasma cells, dendritic
cells, and
macrophages
(2) increased
vascularity due to
vasodilation and
angiogenesis, with
joint
Bouttoniere deformity
flexion of the PIP joint with
hyperextension of the DIP
joint
Z-line deformitysubluxation of the first MCP
joint with hyperextension of
the first interphalangeal (IP)
joint
flat feet
metatarsophalangeal joint
(MTP) involvement
Atlantoaxial involvement:
cervical spine cervical
myelopathy
(-) thoracic and lumbar spine
affectation
EXTRA-ARTICULAR
MANIFESTATIONS:
- Constitutional - weight
loss, fever, fatigue,
malaise, depression, and
in the most severe cases,
cachexia
- Subcutaneous nodules
most common
cutaneous lesion; firm,
non-tender, and round to
oval, and in the skin arise
in the subcutaneous
tissue including the ulnar
aspect of the forearm,
Joint Pain Module: Rheumatoid Arthritis
superficial hemosiderin
deposits
(3) aggregation of
organizing fibrin
covering portions of
the synovium and
floating in the joint
space as rice bodies
(4) accumulation of
neutrophils in the
synovial fluid and
along the surface of
synovium
(5) osteoclastic activity
in underlying bone,
allowing the synovium
to penetrate into the
bone and cause juxtaarticular erosions,
subchondral cysts, and
osteoporosis
(6) pannus formation
fibrous ankylosis
bony ankyloses
The pannus is a mass of
synovium and synovial
stroma consisting of
inflammatory cells,
granulation tissue, and
synovial fibroblasts, which
grows over the articular
cartilage and causes its
erosion.
elbows, occiput, and
lumbosacral area. Less
commonly they form in
the lungs, spleen,
pericardium,
myocardium, heart
valves, aorta, and other
viscera.
Secondary Sjgren's
syndrome
Pleural disease, the most
common pulmonary
manifestation of RA
Pericarditis (most
common),
cardiomyopathy
Rheumatoid vasculitis
normochromic,
normocytic anemia
Feltys syndrome clinical triad of
neutropenia,
splenomegaly, and
nodular RA
Hypoandrogenism
Osteoporosis
Joint Pain Module: Rheumatoid Arthritis
Diagnosis
Rheumatoid arthritis is diagnosed if 4 or more of these
7 factors are present.
1) Morning stiffness: Morning stiffness in and
around the joints for at least one hour.
2) Arthritis of 3 or more joint areas: Swelling or
fluid around three or more joints simultaneously.
The 14 possible areas are right or left PIP, MCP,
wrist, elbow, knee, ankle, and MTP joints
3) Arthritis of hand joints: At least one swollen
area in the wrist, hand, or finger joints.
4) Symmetric arthritis: Arthritis involving the
same joint on both sides of the body.
5) Rheumatoid nodules: Are firm lumps in the
skin of people with rheumatoid arthritis. These
nodules are usually in pressure points of the
body, most commonly the elbows.
6) Serum rheumatoid factor: Abnormal amounts
of rheumatoid factor in the blood.
7) Radiographic changes: X-ray changes in the
hands and wrists typical of rheumatoid arthritis,
with destruction of bone around the involved
joints. However, these changes are typical of
later-stage disease.
* Criteria 1 through 4 must have been present for at
least 6 weeks. Patients with 2 clinical diagnoses are not
excluded.
The clinical diagnosis of RA is largely based on signs
and symptoms of a chronic inflammatory arthritis, with
laboratory and radiographic results providing important
Treatment
NSAIDS - both analgesic and anti-inflammatory
adjunctive therapy for management of symptoms;
minimize side effects of gastritis and peptic ulcer disease
with the use of selective COX-2 inhibitors
Glucocorticoids:
- Rapid disease control: low-to-moderate doses before
onset of fully effective DMARDS therapy
- Acute disease flares: 12 week burst of glucocorticoids
may be prescribed dose and duration guided by the
severity of the exacerbation
- patients with an inadequate response to DMARD
therapy: Chronic administration of low doses (510
mg/d) of prednisone (or its equivalent)
- minimize chronic use of low-dose prednisone therapy
owing to the risk of osteoporosis and other long-term
complications
- ACR recommends primary prevention of
glucocorticoid-induced osteoporosis with a
bisphosphonate in any patient receiving 5 mg/d or
more of prednisone for greater than 3 months
DMARDS RA progression
conventional DMARDs: hydroxychloroquine,
sulfasalazine, methotrexate, and leflunomide; delayed
onset of action of approximately 612 weeks
Methotrexate is the DMARD of choice for the treatment
of RA and is the anchor drug for most combination
therapies
leflunomide - inhibitor of pyrimidine synthesis, appears
similar to that of methotrexate
Joint Pain Module: Rheumatoid Arthritis
supplemental information.
2010 ACR-EULAR criteria yields a score of 010, with a
score of 6 fulfilling the requirements for definite RA
LABORATORY FEATURES:
-Serum RF: IgM, IgG, and IgA isotypes of RF occur in
sera from patients with RA, although the IgM isotype is
the one most frequently measured
-Serum anti-cyclic citrullinated peptide
antibodies: diagnostic specificity approaches 95%
Synovial fluid analysis: Most useful for confirming an
inflammatory arthritis, while at the same time excluding
infection or a crystal-induced arthritis such as gout or
pseudogout
- Reflects an inflammatory state.
Synovial fluid white blood cell (WBC) counts can range
between 5000 and 50,000 WBC/L3 ; neutrophil
predominance
Hydroxychloroquine has not been shown to delay
radiographic progression of disease and thus is not
considered to be a true DMARD
Joint Pain Module: Rheumatoid Arthritis
Joint imaging: plain Xray- juxtaarticular osteopenia,
soft tissue swelling, symmetric joint space loss, and
subchondral erosions, most frequently in the wrists and
hands (MCPs and PIPs) and the feet (MTPs)
MRI- greatest sensitivity for detecting synovitis and joint
effusions Ultrasound- ability to detect more erosions
than plain radiography, especially in easily accessible
joints
Remission
At any time point, patient must satisfy all of the following:
Tender joint count 1
Swollen joint count 1
C-reactive protein 1 mg/dL
Patient global assessment 1 (on a 010 scale)
OR
At any time point, patient must have a Simplified Disease
Activity Index score of 3.3
References:
Harrisons Principles of Internal Medicine , 16th and 18th ed
Cecil Medicine, 23rd Ed
Robbins and Cotran Pathologic Basis of Diseases 8th ed
Bates Guide to Physical Examination and History Taking 11th ed
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- TOGAF 9 Foundation Part 1 Exam Preparation GuideDocument114 pagesTOGAF 9 Foundation Part 1 Exam Preparation GuideRodrigo Maia100% (3)
- Honda Wave Parts Manual enDocument61 pagesHonda Wave Parts Manual enMurat Kaykun86% (94)
- Describing-Jobs-British-English StudentDocument3 pagesDescribing-Jobs-British-English Studentrenata pedroso100% (1)
- What's in A Birthday?: I. We Can Be Mixed Blessings To OthersDocument2 pagesWhat's in A Birthday?: I. We Can Be Mixed Blessings To OthersJayricDepalobosNo ratings yet
- Sample Child Dedication ProgramDocument1 pageSample Child Dedication ProgramJayricDepalobos100% (2)
- Oracle Learning ManagementDocument168 pagesOracle Learning ManagementAbhishek Singh TomarNo ratings yet
- Music Order for Northern Luzon Adventist CollegeDocument1 pageMusic Order for Northern Luzon Adventist CollegeJayricDepalobosNo ratings yet
- Insider Threat ManagementDocument48 pagesInsider Threat ManagementPatricia LehmanNo ratings yet
- "Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."Document3 pages"Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."JayricDepalobosNo ratings yet
- Clinical Pastoral OrientationDocument3 pagesClinical Pastoral OrientationJayricDepalobos100% (1)
- Computer ModuleDocument8 pagesComputer ModuleJayricDepalobosNo ratings yet
- The LightDocument2 pagesThe LightJayricDepalobosNo ratings yet
- The Church Must Stand TogetherDocument7 pagesThe Church Must Stand TogetherJayricDepalobosNo ratings yet
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- Medical Ward 1 Service 2 CensusDocument13 pagesMedical Ward 1 Service 2 CensusJayricDepalobosNo ratings yet
- FWD: Schedule Change AdvisoryDocument2 pagesFWD: Schedule Change AdvisoryJayricDepalobosNo ratings yet
- Shipping Confirmation 1264941Document1 pageShipping Confirmation 1264941JayricDepalobosNo ratings yet
- FWD: Schedule Change AdvisoryDocument2 pagesFWD: Schedule Change AdvisoryJayricDepalobosNo ratings yet
- Medical Ward 1 Service 2 CensusDocument13 pagesMedical Ward 1 Service 2 CensusJayricDepalobosNo ratings yet
- WWW SlidDocument1 pageWWW SlidJayricDepalobosNo ratings yet
- Chapter 01 ChoicesDocument9 pagesChapter 01 ChoicesJayricDepalobosNo ratings yet
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- YHH Strategic Plan 2016-2017Document5 pagesYHH Strategic Plan 2016-2017JayricDepalobosNo ratings yet
- Acquaintance Party ParticipantsDocument1 pageAcquaintance Party ParticipantsJayricDepalobosNo ratings yet
- CAA Concert ProgramDocument2 pagesCAA Concert ProgramJayricDepalobosNo ratings yet
- Census TemplateDocument3 pagesCensus TemplateJayricDepalobosNo ratings yet
- Psalm 23 SermonDocument5 pagesPsalm 23 SermonJayricDepalobosNo ratings yet
- Teen Parenting Brochure AssignmentDocument1 pageTeen Parenting Brochure AssignmentJayricDepalobosNo ratings yet
- General Anesthesia in Caesarean SectionDocument7 pagesGeneral Anesthesia in Caesarean SectionJayricDepalobosNo ratings yet
- Understanding Thalassemia: Causes, Symptoms and TreatmentDocument19 pagesUnderstanding Thalassemia: Causes, Symptoms and TreatmentJayricDepalobosNo ratings yet
- Tally Sheeth Per 10 HouseholdsDocument14 pagesTally Sheeth Per 10 HouseholdsJayricDepalobosNo ratings yet
- Peer Evaluation For Group 5Document1 pagePeer Evaluation For Group 5JayricDepalobosNo ratings yet
- Tally Sheeth Per 10 HouseholdsDocument14 pagesTally Sheeth Per 10 HouseholdsJayricDepalobosNo ratings yet
- Pneumonia Antibiotics PDFDocument1 pagePneumonia Antibiotics PDFRudy KurniawanNo ratings yet
- BIBLIO Eric SwyngedowDocument34 pagesBIBLIO Eric Swyngedowadriank1975291No ratings yet
- Yellowstone Food WebDocument4 pagesYellowstone Food WebAmsyidi AsmidaNo ratings yet
- Difference Between Mark Up and MarginDocument2 pagesDifference Between Mark Up and MarginIan VinoyaNo ratings yet
- Sarvali On DigbalaDocument14 pagesSarvali On DigbalapiyushNo ratings yet
- FSRH Ukmec Summary September 2019Document11 pagesFSRH Ukmec Summary September 2019Kiran JayaprakashNo ratings yet
- Guidelines On Occupational Safety and Health in Construction, Operation and Maintenance of Biogas Plant 2016Document76 pagesGuidelines On Occupational Safety and Health in Construction, Operation and Maintenance of Biogas Plant 2016kofafa100% (1)
- Do You Agree With Aguinaldo That The Assassination of Antonio Luna Is Beneficial For The Philippines' Struggle For Independence?Document1 pageDo You Agree With Aguinaldo That The Assassination of Antonio Luna Is Beneficial For The Philippines' Struggle For Independence?Mary Rose BaluranNo ratings yet
- Astera Data Integration BootcampDocument4 pagesAstera Data Integration BootcampTalha MehtabNo ratings yet
- Hindustan Motors Case StudyDocument50 pagesHindustan Motors Case Studyashitshekhar100% (4)
- 2023 Test Series-1Document2 pages2023 Test Series-1Touheed AhmadNo ratings yet
- India: Kerala Sustainable Urban Development Project (KSUDP)Document28 pagesIndia: Kerala Sustainable Urban Development Project (KSUDP)ADBGADNo ratings yet
- Passenger E-Ticket: Booking DetailsDocument1 pagePassenger E-Ticket: Booking Detailsvarun.agarwalNo ratings yet
- Numerical Methods Chapter 10 SummaryDocument8 pagesNumerical Methods Chapter 10 SummarynedumpillilNo ratings yet
- HCW22 PDFDocument4 pagesHCW22 PDFJerryPNo ratings yet
- Jfif 1.02Document9 pagesJfif 1.02Berry Hoekstra100% (1)
- Chem 102 Week 5Document65 pagesChem 102 Week 5CAILA CACHERONo ratings yet
- Energy AnalysisDocument30 pagesEnergy Analysisca275000No ratings yet
- Maj. Terry McBurney IndictedDocument8 pagesMaj. Terry McBurney IndictedUSA TODAY NetworkNo ratings yet
- AFNOR IPTDS BrochureDocument1 pageAFNOR IPTDS Brochurebdiaconu20048672No ratings yet
- ESA Knowlage Sharing - Update (Autosaved)Document20 pagesESA Knowlage Sharing - Update (Autosaved)yared BerhanuNo ratings yet
- Radio Frequency Transmitter Type 1: System OperationDocument2 pagesRadio Frequency Transmitter Type 1: System OperationAnonymous qjoKrp0oNo ratings yet
- Preventing and Mitigating COVID-19 at Work: Policy Brief 19 May 2021Document21 pagesPreventing and Mitigating COVID-19 at Work: Policy Brief 19 May 2021Desy Fitriani SarahNo ratings yet
- Surgery Lecture - 01 Asepsis, Antisepsis & OperationDocument60 pagesSurgery Lecture - 01 Asepsis, Antisepsis & OperationChris QueiklinNo ratings yet
- Movement and Position: Question Paper 4Document14 pagesMovement and Position: Question Paper 4SlaheddineNo ratings yet
- Planning A Real Estate ProjectDocument81 pagesPlanning A Real Estate ProjectHaile SilasieNo ratings yet