Professional Documents
Culture Documents
Oxidative Stress
Uploaded by
fotea_nicoleta816Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oxidative Stress
Uploaded by
fotea_nicoleta816Copyright:
Available Formats
seminars in CELL & DEVELOPMENTAL BIOLOGY, Vol. 12, 2001: pp.
449457
doi:10.1006/scdb.2001.0282, available online at http://www.idealibrary.com on
Reactive oxygen species and mitochondrial diseases
Ilias G. Kirkinezosa and Carlos T. Moraesa,b,
produce ROS at a rate higher than their scavenging
capacity, resulting in the incomplete metabolism of
approximately 13% of the consumed oxygen. 4,5 The
byproducts of incomplete oxygen metabolism are
.
superoxide (O
2 ), hydrogen peroxide (H2 O2 ),
and hydroxyl radical (OH). The formation
of superoxide occurs via the transfer of a free
electron to molecular oxygen. This reaction occurs
at specific sites of the electron transport chain
(ETC), which resides in the inner mitochondrial
membrane [Figure 1(a)]. ETC complexes I (NADH
dehydrogenase) and III (ubisemiquinone) produce
most of the superoxide, 4,6,7 which is then scavenged
by the mitochondrial enzyme manganese superoxide
dismutase (MnSOD) to produce H2 O2 . Since
mitochondria do not contain catalase, their only
defense against the potentially toxic properties
of H2 O2 is the enzyme glutathione peroxidase
(GSPx). GSPx requires reduced glutathione (GSH)
as a coenzyme and converts H2 O2 to water, thus
completely detoxifying ROS. However, in the
presence of reduced transition metals, H2 O2 can
produce the highly reactive OH, which can cause
extensive damage to DNA, proteins, and lipids
[Figure 1(a)]. 8
Two other important radical species are nitric
oxide (NO) and peroxynitrite (ONOO ). Recent
evidence has demonstrated that mitochondria
possess their own nitric oxide synthase (mtNOS) 9
and can produce endogenous NO and ONOO . 10,11
Although the main source of ONOO is through
the reaction of NO with superoxide [Figure 1(a)],
there are also several other ways to produce ONOO
in a cell. 1216 Mitochondrial NO decays mainly
via ONOO formation, ubiquinol oxidation, and
reversible binding to cytochrome c oxidase. 17
A variety of diseases have been associated with excessive reactive oxygen species (ROS), which are produced mostly in the
mitochondria as byproducts of normal cell respiration. The
interrelationship between ROS and mitochondria suggests
shared pathogenic mechanisms in mitochondrial and ROSrelated diseases. Defects in oxidative phosphorylation can
increase ROS production, whereas ROS-mediated damage
to biomolecules can have direct effects on the components of
the electron transport system. Here, we review the molecular
mechanisms of ROS production and damage, as well as the
existing evidence of mitochondrial ROS involvement in human diseases.
Key words: mitochondria / reactive oxygen species /
mtDNA diseases / neurodegeneration / aging
c 2001 Academic Press
Molecular mechanisms of mitochondrial ROS
production
Mitochondria are unique organelles, as they are
the main site of oxygen metabolism, accounting for
approximately 8590% of the oxygen consumed
by the cell. 1,2 Incomplete processing of oxygen
and/or release of free electrons results in the
production of oxygen radicals. Mitochondria
constantly metabolize oxygen thereby producing
reactive oxygen species (ROS) as a byproduct.
These organelles have their own ROS scavenging
mechanisms that are required for cell survival. 3
It has been shown, however, that mitochondria
From the Departments of a Cell Biology and Anatomy and b Neurology,
University of Miami School of Medicine, Miami, Florida 33136.
*Corresponding author. University of Miami School of Medicine, 1095 NW
14th Terrace, Miami, Florida 33136.
E-mail: cmoraes@med.miami.edu
c
2001
Academic Press
10849521 / 01 / 060449+ 09 / $35.00 / 0
ROS-mediated damage
Under normal conditions, the effects of ROS are
counteracted by a variety of antioxidants, by both
enzymatic and nonenzymatic mechanisms. Oxidative
449
I. G. Kirkinezos and C. T. Moraes
(a)
(b)
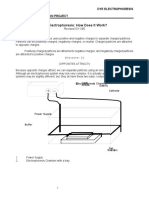
Figure 1. Generators and targets of reactive oxygen species (ROS) in mitochondria.
(a) A schematic diagram of the generation of the main mitochondrial reactive oxygen species and their targets. Solid
) indicate
arrows with solid arrowheads ( I) indicate generation of molecules. Solid arrows with pointed arrowheads (
diffusion of molecules. Hatched arrows indicate damaging effects.
(b) An illustration of the vicious cycle hypothesis. MtDNA damage leads to defective ETC complexes, which consequently
increase ROS production, potentially leading to further mtDNA damage.
450
Reactive oxygen species and mitochondrial diseases
NO are cytotoxic, although the exact mechanism
associated with this effect is still unclear. It may be
involved in inflammatory, neurodegenerative, and
cardiovascular pathological processes. 20 NO can
regulate aerobic respiration by reversible inhibition
of cytochrome c oxidase. Interestingly, because
of the short half-life and diffusibility of NO, any
cell that produces excess NO will inhibit its own
respiration and respiration of surrounding cells,
which may contribute to the cytotoxic effects of
NO. For example, in co-cultures of astrocytic and
neuronal cells, astrocytic-derived NO causes both
reversible and irreversible damage to the neuronal
electron transport chain. 22
Peroxynitrite is a highly damaging agent with a
vast repertoire of targets and detrimental cellular
effects. ONOO modifies proteins by nitrating
tyrosine residues, forming dityrosine, and oxidizing
tryptophan and cysteine. 23 The main mitochondrial
targets of peroxynitrite are complexes I, II, IV and V,
aconitase, creatine kinase, superoxide dismutase,
mitochondrial membranes, and mtDNA. Damage of
these molecules may induce mitochondrial swelling,
depolarization, calcium release, and permeability
transition. 24 Uptake of calcium by mitochondria
induces mtNOS which increases ONOO levels in
the organelle, leading to release of cytochrome c,
increase of lipid peroxidation 25 and to a subsequent
release of calcium in the cytosol, 26 a process
which has been suggested to be a feedback loop
preventing mitochondrial calcium overload. Another
important finding is that ONOO inhibits MnSOD
enzymatic activity by nitration and oxidation of
critical tyrosine residues. 27 Curiously, ONOO
seems to preferentially damage certain proteins in
a cell-type specific manner. The molecule affects
the electron transport chain of neurons, but not
astrocytes, 28 however, it preferentially depletes
glutathione (GSH) in astrocytes. 29
stress is considered to be the result of an imbalance
of two opposing and antagonistic forces, ROS
and antioxidants, in which the effects of ROS are
more potent than the compensatory capacity of
antioxidants. In the case of mitochondrial-derived
ROS, superoxide is the first radical produced. It
is a highly reactive species and does not diffuse
easily throughout the cell. Because the main site
.
of O
2 production is the inner mitochondrial
membrane, the mitochondrial DNA (mtDNA) has
been hypothesized to be a major target for ROS
damage [Figure 1(b)]. 18 A circumstantial correlation
between ROS and mtDNA damage was shown by
measuring the levels of mtDNA rearrangements in
heart and skeletal muscle tissue of mice. The level
of mtDNA rearrangements were higher in the heart,
which coincides with the fact that heart has lower
antioxidant defenses than skeletal muscle. 18 H2 O2 is
the next key player in mitochondrially derived ROS,
as it is the product of superoxide detoxification by
MnSOD. H2 O2 is not a free radical by definition
because it lacks free electrons. Nevertheless, its role
in ROS-mediated damage is extremely significant
by virtue of chemical versatility and diffusibility.
H2 O2 is a substrate in many physiological and
abnormal chemical reactions both intracellularly and
extracellularly. Due to its small size and relatively
benign reactivity, compared to the rest of the ROS,
H2 O2 can diffuse freely across several cell radii;
therefore, it is able to mediate toxic effects far from
the site of ROS production. Although by itself H2 O2
is not a major source of oxidative damage, it can react
with free transition metals via the Fenton reaction
(Fe2+ + H2 O2 Fe3+ + OH + OH), producing
the extremely reactive hydroxyl radical. OH has
a very short half-life and reacts with virtually any
molecules in close proximity [Figure 1(a)]. There is
no known scavenger for OH, but OH toxicity can
be avoided by minimizing the levels of H2 O2 and
most importantly the availability of free transition
metals (e.g. Fe2+ , Cu+ ).
Nitric oxide has also been implicated in ROSmediated damage. NO has a dual personality,
which is both beneficial, 19 and detrimental. 20
In some instances, different intracellular levels
of NO can mediate diverse effects. For example,
physiological levels of NO inhibit the opening of
the mitochondrial permeability transition pore
(PTP), whereas high NO concentrations promote
PTP opening. 21 In this review, however, we will only
discuss the harmful effects of NO. High levels of
Mitochondrial dysfunction and ROS in human
pathology
There has been a great deal of research on the
role of ROS in the pathogenesis of a number of
human diseases. A multitude of theories exist,
attempting to explain the mechanisms of ROSmediated damage and its effects in the progression
of diseases. In many diseases, primary mitochondrial
involvement is profound and evident. In others,
the mitochondrial participation is only suspected
451
I. G. Kirkinezos and C. T. Moraes
rate of accumulation of mtDNA deletions has not
been observed in patients with mitochondrial
disorders. Using a specific PCR approach to
detect the so-called mtDNA common deletion
and long PCR to detect a plethora of mtDNA
rearrangements, Tengan et al. could not find an
increase in mtDNA deletions in muscle of patients
with pathogenic mtDNA point mutations. 32 This
observation argues against the vicious cycle theory,
as one would expect that the ETC defect caused
by the mtDNA point mutations should lead to an
increase in ROS, and consequently an increase in
mtDNA rearrangements. Therefore, the vicious
cycle hypothesis [Figure 1(b)] continues to be an
attractive but unproven hypothesis.
Several studies have demonstrated that mtDNA
mutations associated with human disease lead to
ETC complex dysfunction, increased production of
ROS, and oxidative damage, as is the situation in
MELAS, where hydroxyl radical damage to mtDNA
can be accelerated by a specific mitochondrial
genotype associated with the disease. 33 In MELAS
and MERRF patients, the intracellular levels of
hydrogen peroxide and oxidative damage to DNA
and lipids were increased in skin fibroblasts. 34 In
whole blood cells of patients with MELAS-related
mitochondriopathy and patients with LHON, ROSassociated telomere shortening was observed. 35
Finally in a mouse model of sarcopenia, mtDNA
deletion mutations in muscle fibers co-localized
with increased levels of oxidative damage to nucleic
acids. 36 Furthermore, ROS-mediated damage
selectively to mtDNA has been reported in other
diseases, like Down syndrome, 37 acute pancreatitis, 38
multiple sclerosis, 39 end-stage renal disease, 40 and
left ventricular remodeling and failure following
myocardial infarction. 41
As discussed above, most mitochondrial ROS
are formed at complexes I and III. Many clinical
syndromes have been associated with isolated
complex I deficiencies have been described,
including fatal infantile lactic acidosis, adultonset exercise intolerance, focal dystonia, LHON,
cardiomyopathy
with
cataracts,
hepatopathy
with tubulopathy, Leighs disease, cataracts and
developmental delay, and lacticacademia in the
neonatal period followed by mild symptoms. 4247 It
is unclear at this point if some of these symptoms
are exacerbated by increased ROS production, even
though complex I impairment leads to increased ROS
production in submitochondrial particles 6 and cell
systems. 46,48 In studies of human xenomitochondrial
or suggested. For the scope of this paper we will
consider all diseases potentially affected by ROS
as having a mitochondrial component. The main
concept connecting mitochondrial diseases and ROS
is that increases in ROS production and decreases in
ATP production can cause oxidative phosphorylation
deficiency, leading to mitochondrial disease. 30 Also,
a primary defect in oxidative phosphorylation may
increase superoxide production, thereby increasing
oxidative stress.
Mitochondrial diseases
In the last 15 years, several clinical syndromes were
associated with mtDNA mutations, the most common
being NARP (neurogenic muscle weakness, ataxia
and retinitis pigmentosa), MELAS (mitochondrial
encephalomyopathy lactic acidosis, and strokelike episodes), MERRF (myoclonic epilepsy and
ragged-red fibers), LHON (Leber hereditary optic
neuropathy), and KSS (Kearns-Sayre syndrome,
ophthalmoplegia, ataxia, retinitis pigmentosa,
cardiac conduction defect and elevated cerebrospinal
fluid protein) (see article by DiMauro in this issue).
MtDNA encodes few proteins which are involved
in the electron transport chain, the main source
of ROS in cells. This special situation highlights
the theory of the vicious cycle, a theory attractive
within the realm of degenerative processes. In this
cycle, an inherited or random primary mitochondrial
mutation initially induces a respiratory defect, that
increases the leakage of ROS from the electron
transport chain. Subsequently, ROS may trigger
accumulation of secondary mtDNA mutations
exacerbating mitochondrial respiratory defects and
consequently increasing production of ROS and lipid
peroxides from mitochondria.
It has been demonstrated that after exposing
cells to oxidative stress, mtDNA damage is more
extensive and persists longer than damage in nuclear
DNA (nDNA). 31 Several reasons may contribute
to this selective vulnerability: (i) mtDNA lacks
histones which are protective against free radical
damage, (ii) mtDNA lacks an adequate repair
system, rendering it unable to cope with extensive
damage, especially strand breaks, (iii) mtDNA has
very few non-coding sequences, therefore increasing
the likelihood of a DNA alteration to affect a
gene, and (iv) mtDNA is located near the inner
mitochondrial membrane, a major site of oxygen
radical production. 2 However, a correlation between
defective oxidative phosphorylation and increased
452
Reactive oxygen species and mitochondrial diseases
These changes can lead to neuronal death, mainly
through excitotoxic pathways, involving oxidation of
macromolecules and apoptosis.
More than a decade ago, the first strong evidence
of mitochondrial involvement in the pathogenesis
of a neurodegenerative disease came to light
when complex I deficiency was identified in
substantia nigra 56 and platelet mitochondria
of Parkinson disease patients. 57 Subsequently,
enzymatic deficiencies in the electron transport chain
were identified in additional neurodegenerative
diseases: complex IV deficiency in AD and ALS, 5860
and complex II and III in HD and FA. 61 The
common denominator of mitochondrial dysfunction
in these diseases led to hypotheses related to
mtDNA involvement. In HD and FA the genetic
defects appear to be in nuclear genes that encode
non-respiratory proteins (huntingtin for HD,
and frataxin for FA). This fact suggests that the
observed respiratory deficiencies are secondary to
the pathogenic initiating factors. For PD and AD
the picture is unclear. Some reports showed that
a proportion of patients, have evidence of mtDNA
abnormalities as a key player in the progress of
disease. 62 Additional evidence of an association
between ROS and mitochondrial dysfunction
comes from the observation that mutations in the
SOD1 gene can cause ALS. 63 Also, mitochondrial
abnormalities are seen early in the development
of the disease. 60 However, it is still unclear if
the mutated SOD1 alters ROS production, or
even whether the mitochondrial abnormalities are
secondary to a cell death stimulus.
Oxidative damage is also a common finding in all
neurodegenerative diseases. Evidence of oxidative
damage in PD, 48,62,6467 AD, 6870 ALS, 7174 HD, 7577
and FA 78,79 strengthened the link between abnormal
mitochondrial function, increased ROS production,
and neurodegeneration. Recent interesting evidence
suggest that motor neurons are particularly
susceptible to damage from endogenously produced
ONOO , 80,81 and protein bound nitrotyrosine
has been observed in motor neurons from human
ALS patients and tissue of a mouse model harboring a
transgene coding for a mutated form of SOD1 found
in some patients (G93A-SOD1). 82 An interesting
hypothesis is that the high polyunsaturate level of
brain mitochondrial phospholipids might predispose
them to peroxidation, hence brain mitochondria may
be more susceptible to neurodegenerative disorders
that progress via mechanisms of mitochondrial
oxidative damage. 83
cybrids harboring a 40% complex I deficiency and
a drug-induced model of complex I inhibition, 49,50
correlations between the levels of complex I
impairment and cell respiration, cell growth,
ROS production, lipid peroxidation, mitochondrial
membrane potential, and apoptosis were observed.
Interestingly, cell death was quantitatively associated
with ROS production, rather than with complex I
deficiency. 51 This suggests that partial ETC defects
may, in some instances, mediate cellular damage by
ROS-related processes.
It has been shown that complex I impairment
induces MnSOD and/or increases ROS production. 45,46,52 Therefore, a complex I defect may not
be accompanied by increased ROS, if MnSOD is
elevated. However, MnSOD as the only scavenger
might not be sufficient to prevent oxidative damage.
Its action need to be coupled with GSPx/GSH
detoxification of H2 O2 , in order to avoid the
formation of the highly reactive OH, as observed
in cells from a patient with cardiomyopathy with
cataracts. 45
Fewer studies have been described for complex III
deficiencies. Mutations in the apocytochrome
b gene have been described in patients with
myopathies 53 but also with encephalopathies. 54 In
transmitochondrial cybrids containing mtDNA from
a patient with Parkinsonism and MELAS, high levels
of a mtDNA with a mutation in the apocytochrome
b gene were associated with respiratory deficiency
and complex III defect. This deficiency was also
associated with increased hydrogen peroxide
production. 55 Such an increase in the ROS levels
in the central nervous systems could explain the
Parkinsonism in this patient.
Neurodegenerative diseases
Increasingly, research efforts are investigating
the involvement of ROS and mitochondria in
the pathogenesis of common neurodegenerative
diseases: Parkinson disease (PD), Alzheimers
disease (AD), amyotrophic lateral sclerosis (ALS),
Huntingtons disease (HD), and Friedreichs
ataxia (FA). Although an extensive review of research
efforts in this field would be beyond the scope of
this paper, we will briefly discuss the mitochondrial
and ROS involvement in these conditions. Increased
ROS production in neurodegenerative processes
may affect normal mitochondrial parameters like
ATP production, membrane potential, permeability
transition pore activation, and calcium uptake.
453
I. G. Kirkinezos and C. T. Moraes
in this area, the next few years should bring answers
to many of these questions.
Aging
Although it is doubtful that aging is a disease,
mitochondrial ROS involvement in this process
is strongly suggested by experimental data. A
prevalent theory for aging is a variant of the
vicious cycle concept we described previously.
MtDNA is constantly exposed to ROS generated by
the mitochondrial electron transport chain, and
mutations may accumulate exponentially with age.
The simultaneous increase in lipid peroxidation
and oxidation of mitochondrial proteins adds to the
oxidative stress effects, initiating the vicious cycle
of molecular degeneration. This putative vicious
cycle can operate at different rates in various tissues,
leading to differential accumulation of oxidative
damage, which could explain the differences in
functional impairment and deterioration of different
tissues in the aging process.
There is substantial evidence that damage to
mtDNA accumulates with age. Among them, the
most significant is the 10-fold increase in an oxidative
damage marker (8-hydroxy-2-deoxyguanosine) in
mtDNA versus nDNA from human brain. 84 A study
of aging in rhesus monkeys revealed that there
are significant decreases with increasing age in
the activities of complex I and IV, as well as in
mitochondrial ATP generation. 85 Finally, several
mtDNA point mutations also increase with normal
aging. 8689 What is not clear at this point, is whether
such mutations are generated by ROS-mediated
damage.
Acknowledgements
The work from our laboratory is supported by National Institutes of Health Grants GM55766, CA85700
and EY10804 and by the Muscular Dystrophy Association.
References
1. Chance B, Sies H, Boveris A (1979) Hydroperoxide
metabolism in mammalian organs. Physiol Rev 59:527605
2. Shigenaga MK, Hagen TM, Ames BN (1994) Oxidative
damage and mitochondrial decay in aging. Proc Natl Acad
Sci USA 91:1077110778
3. Melov S, Schneider JA, Day BJ, Hinerfeld D, Coskun P,
Mirra SS, Crapo JD, Wallace DC (1998) A novel neurological
phenotype in mice lacking mitochondrial manganese superoxide dismutase. Nat Genet 18:159163
4. Boveris A, Chance B (1973) The mitochondrial generation
of hydrogen peroxide. General properties and effect of
hyperbaric oxygen. Biochem J 134:707716
5. Nohl H, Hegner D (1978) Do mitochondria produce oxygen
radicals in vivo? Eur J Biochem 82:563567
6. Turrens JF, Boveris A (1980) Generation of superoxide anion
by the NADH dehydrogenase of bovine heart mitochondria.
Biochem J 191:421427
7. Turrens JF, Freeman BA, Levitt JG, Crapo JD (1982) The
effect of hyperoxia on superoxide production by lung submitochondrial particles. Arch Biochem Biophys 217:401410
8. Goldstein S, Meyerstein D, Czapski G (1993) The Fenton
reagents. Free Radic Biol Med 15:435445
9. Tatoyan A, Giulivi C (1998) Purification and characterization
of a nitric-oxide synthase from rat liver mitochondria. J Biol
Chem 273:1104411048
10. Giulivi C (1998) Functional implications of nitric oxide
produced by mitochondria in mitochondrial metabolism.
Biochem J 332:673679
11. Giulivi C, Poderoso JJ, Boveris A (1998) Production of nitric
oxide by mitochondria. J Biol Chem 273:1103811043
12. Brown GC (1995) Nitric oxide regulates mitochondrial
respiration and cell functions by inhibiting cytochrome
oxidase. FEBS Lett 369:136139
13. Packer MA, Porteous CM, Murphy MP (1996) Superoxide
production by mitochondria in the presence of nitric oxide
forms peroxynitrite. Biochem Mol Biol Int 40:527534
14. Hogg N, Singh RJ, Kalyanaraman B (1996) The role of
glutathione in the transport and catabolism of nitric oxide.
FEBS Lett 382:223228
15. Murphy ME, Sies H (1991) Reversible conversion of nitroxyl
anion to nitric oxide by superoxide dismutase. Proc Natl Acad
Sci USA 88:1086010864
16. Sharpe MA, Cooper CE (1998) Reactions of nitric oxide
with mitochondrial cytochrome c: a novel mechanism for the
formation of nitroxyl anion and peroxynitrite. Biochem J
332:919
17. Poderoso JJ, Lisdero C, Schopfer F, Riobo N, Carreras MC,
Cadenas E, Boveris A (1999) The regulation of mitochondrial
Concluding remarks
Clearly, our understanding of the intricate relationship between mitochondrial function, ROS production, ROS damage and the development of a clinical
phenotype is still very limited. Even the link between
ROS and mtDNA mutations is still a matter of controversy, lacking experimental evidence and relying
mostly on hypothetical models. This is particularly evident for mtDNA deletions, a widely accepted marker
of aging. The origin of such mtDNA rearrangements
is unclear, and oxidative damage does not provide an
adequate model for the generation of mtDNA deletions. In addition, the role of ROS and mitochondria in neurodegenerative disorders and aging is also
a matter of constant debate, as increased oxidative
damage may be a consequence rather than the cause
of the disease process. Because of the growing interest
454
Reactive oxygen species and mitochondrial diseases
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
enzyme system. Chin J Physiol 44:111
35. Oexle K, Zwirner A (1997) Advanced telomere shortening in
respiratory chain disorders. Hum Mol Genet 6:905908
36. Wanagat J, Cao Z, Pathare P, Aiken JM (2001) Mitochondrial
DNA deletion mutations colocalize with segmental electron
transport system abnormalities, muscle fiber atrophy, fiber
splitting, and oxidative damage in sarcopenia. FASEB J
15:322332
37. Druzhyna N, Nair RG, LeDoux SP, Wilson GL (1998)
Defective repair of oxidative damage in mitochondrial DNA
in Downs syndrome. Mutat Res 409:8189
38. Ehlers RA, Hernandez A, Bloemendal LS, Ethridge RT,
Farrow B, Evers BM (1999) Mitochondrial DNA damage and
altered membrane potential (delta psi) in pancreatic acinar
cells induced by reactive oxygen species. Surgery 126:148155
39. Lu F, Selak M, OConnor J, Croul S, Lorenzana C, Butunoi C,
Kalman B (2000) Oxidative damage to mitochondrial DNA
and activity of mitochondrial enzymes in chronic active
lesions of multiple sclerosis. J Neurol Sci 177:95103
40. Lim PS, Cheng YM, Wei YH (2000) Large-scale mitochondrial
DNA deletions in skeletal muscle of patients with end-stage
renal disease. Free Radic Biol Med 29:454463
41. Ide T, Tsutsui H, Hayashidani S, Kang D, Suematsu N,
Nakamura K, Utsumi H, Hamasaki N, Takeshita A (2001)
Mitochondrial DNA damage and dysfunction associated
with oxidative stress in failing hearts after myocardial
infarction. Circ Res 88:529535
42. Robinson BH, McKay N, Goodyer P, Lancaster G (1985) Defective intramitochondrial NADH oxidation in skin fibroblasts
from an infant with fatal neonatal lactic acidemia. Am J Hum
Genet 37:938946
43. Wallace DC, Singh G, Lott MT, Hodge JA, Schurr TG,
Lezza AM, Elsas LJ 2nd, Nikoskelainen EK (1988) Mitochondrial DNA mutation associated with Lebers hereditary optic
neuropathy. Science 242:14271430
44. Robinson BH (1993) Lacticacidemia. Biochim Biophys Acta
1182:231244
45. Luo X, Pitkanen S, Kassovska-Bratinova S, Robinson BH,
Lehotay DC (1997) Excessive formation of hydroxyl radicals
and aldehydic lipid peroxidation products in cultured skin
fibroblasts from patients with complex I deficiency. J Clin
Invest 99:28772882
46. Pitkanen S, Robinson BH (1996) Mitochondrial complex
I deficiency leads to increased production of superoxide
radicals and induction of superoxide dismutase. J Clin Invest
98:345351
47. Robinson BH (1998) Human complex I deficiency: clinical
spectrum and involvement of oxygen free radicals in
the pathogenicity of the defect. Biochim Biophys Acta
1364:271286
48. Seaton TA, Cooper JM, Schapira AH (1997) Free radical
scavengers protect dopaminergic cell lines from apoptosis
induced by complex I inhibitors. Brain Res 777:110118
49. Kenyon L, Moraes CT (1997) Expanding the functional
human mitochondrial DNA database by the establishment of
primate xenomitochondrial cybrids. Proc Natl Acad Sci USA
94:91319135
50. Barrientos A, Kenyon L, Moraes CT (1998) Human xenomitochondrial cybrids. Cellular models of mitochondrial complex
I deficiency. J Biol Chem 273:1421014217
51. Barrientos A, Moraes CT (1999) Titrating the effects of
mitochondrial complex I impairment in the cell physiology.
J Biol Chem 274:1618816197
52. Robinson BH (1998) Diagnosis of mitochondrial energy
metabolism defects in tissue culture. Induction of MnSOD
oxygen uptake by redox reactions involving nitric oxide and
ubiquinol. J Biol Chem 274:3770937716
Esposito LA, Melov S, Panov A, Cottrell BA,
Wallace DC (1999) Mitochondrial disease in mouse
results in increased oxidative stress. Proc Natl Acad Sci USA
96:48204825
Chiueh CC (1999) Neuroprotective properties of nitric oxide.
Ann NY Acad Sci 890:301311
Brown GC (1997) Nitric oxide inhibition of cytochrome
oxidase and mitochondrial respiration: implications for
inflammatory, neurodegenerative and ischaemic pathologies.
Mol Cell Biochem 174:189192
Brookes PS, Salinas EP, Darley-Usmar K, Eiserich JP,
Freeman BA, Darley-Usmar VM, Anderson PG (2000)
Concentration-dependent effects of nitric oxide on mitochondrial permeability transition and cytochrome c release.
J Biol Chem 275:2047420479
Stewart VC, Sharpe MA, Clark JB, Heales SJ (2000) Astrocytederived nitric oxide causes both reversible and irreversible
damage to the neuronal mitochondrial respiratory chain.
J Neurochem 75:694700
Ischiropoulos H, al-Mehdi AB (1995) Peroxynitrite-mediated
oxidative protein modifications. FEBS Lett 364:279282
Brown GC (1999) Nitric oxide and mitochondrial respiration.
Biochim Biophys Acta 1411:351369
Ghafourifar P, Schenk U, Klein SD, Richter C (1999)
Mitochondrial nitric-oxide synthase stimulation causes cytochrome c release from isolated mitochondria. Evidence
for intramitochondrial peroxynitrite formation. J Biol Chem
274:3118531188
Bringold U, Ghafourifar P, Richter C (2000) Peroxynitrite
formed by mitochondrial NO synthase promotes mitochondrial Ca2+ release. Free Radic Biol Med 29:343348
MacMillan-Crow LA, Thompson JA (1999) Tyrosine modifications and inactivation of active site manganese superoxide
dismutase mutant (Y34F) by peroxynitrite. Arch Biochem
Biophys 366:8288
Bolanos JP, Heales SJ, Land JM, Clark JB (1995) Effect of peroxynitrite on the mitochondrial respiratory chain: differential
susceptibility of neurones and astrocytes in primary culture.
J Neurochem 64:19651972
Ju C, Yoon KN, Oh YK, Kim HC, Shin CY, Ryu JR, Ko KH,
Kim WK (2000) Synergistic depletion of astrocytic glutathione by glucose deprivation and peroxynitrite: correlation
with mitochondrial dysfunction and subsequent cell death.
J Neurochem 74:19891998
Wallace DC (1997) in The Molecular and Genetic Basis of
Neurological Disease (Rosenberg RN, Prusiner SB, DiMauro
S, Barchi RL, eds) pp. 237269. Butterworth-Heinemann,
Boston
Yakes FM, Van Houten B (1997) Mitochondrial DNA damage
is more extensive and persists longer than nuclear DNA
damage in human cells following oxidative stress. Proc Natl
Acad Sci USA 94:514519
Tengan CH, Gabbai AA, Shanske S, Zeviani M,
Moraes CT (1997) Oxidative phosphorylation dysfunction
does not increase the rate of accumulation of age-related
mtDNA deletions in skeletal muscle. Mutat Res 379:111
Tanaka M, Kovalenko SA, Gong JS, Borgeld HJ, Katsumata K,
Hayakawa M, Yoneda M, Ozawa T (1996) Accumulation of
deletions and point mutations in mitochondrial genome in
degenerative diseases. Ann N y Acad Sci 786:102111
Wei YH, Lu CY, Wei CY, Ma YS, Lee HC (2001) Oxidative stress
in human aging and mitochondrial disease-consequences of
defective mitochondrial respiration and impaired antioxidant
455
I. G. Kirkinezos and C. T. Moraes
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
and bcl-2 in mitochondria from patients with complex I
(NADH-CoQ reductase) deficiency. Biofactors 7:229230
Andreu AL et al. (1999) Exercise intolerance due to mutations
in the cytochrome b gene of mitochondrial DNA. N Engl
J Med 341:10371044
De Coo IF, Renier WO, Ruitenbeek W, Ter Laak HJ,
Bakker M, Schagger H, Van Oost BA, Smeets HJ (1999) A
4-base pair deletion in the mitochondrial cytochrome b gene
associated with parkinsonism/MELAS overlap syndrome. Ann
Neurol 45:130133
Rana M, de Coo I, Diaz F, Smeets H, Moraes CT (2000)
An out-of-frame cytochrome b gene deletion from a patient
with parkinsonism is associated with impaired complex III
assembly and an increase in free radical production. Ann
Neurol 48:774781
Schapira AH, Cooper JM, Dexter D, Clark JB, Jenner P,
Marsden CD (1990) Mitochondrial complex I deficiency in
Parkinsons disease. J Neurochem 54:823827
Parker WD Jr, Boyson SJ, Parks JK (1989) Abnormalities of
the electron transport chain in idiopathic Parkinsons disease.
Ann Neurol 26:719723
Mutisya EM, Bowling AC, Beal MF (1994) Cortical cytochrome oxidase activity is reduced in Alzheimers disease.
J Neurochem 63:21792184
Borthwick GM, Johnson MA, Ince PG, Shaw PJ, Turnbull DM (1999) Mitochondrial enzyme activity in amyotrophic lateral sclerosis: implications for the role of
mitochondria in neuronal cell death. Ann Neurol 46:787790
Xu GP, Dave KR, Moraes CT, Busto R, Sick TJ, Bradley WG,
Perez-Pinzon MA (2001) Dysfunctional mitochondrial respiration in the wobbler mouse brain. Neurosci Lett 300:141144
Schapira AH (1999) Mitochondrial involvement in Parkinsons disease, Huntingtons disease, hereditary spastic paraplegia and Friedreichs ataxia. Biochim Biophys Acta
1410:159170
Smith TS, Bennett JP Jr (1997) Mitochondrial toxins in
models of neurodegenerative diseases. I: In vivo brain
hydroxyl radical production during systemic MPTP treatment
or following microdialysis infusion of methylpyridinium or
azide ions. Brain Res 765:183188
Tu PH, Raju P, Robinson KA, Gurney ME, Trojanowski JQ,
Lee VM (1996) Transgenic mice carrying a human mutant
superoxide dismutase transgene develop neuronal cytoskeletal pathology resembling human amyotrophic lateral sclerosis
lesions. Proc Natl Acad Sci USA 93:31553160
Cassarino DS, Fall CP, Swerdlow RH, Smith TS,
Halvorsen EM, Miller SW, Parks JP, Parker WD Jr,
Bennett JP Jr (1997) Elevated reactive oxygen species
and antioxidant enzyme activities in animal and cellular
models of Parkinsons disease. Biochim Biophys Acta
1362:7786
Merad-Boudia M, Nicole A, Santiard-Baron D, Saille C,
Ceballos-Picot I (1998) Mitochondrial impairment as an early
event in the process of apoptosis induced by glutathione
depletion in neuronal cells: relevance to Parkinsons disease.
Biochem Pharmacol 56:645655
Merad-Saidoune M, Boitier E, Nicole A, Marsac C, Martinou JC, Sola B, Sinet PM, Ceballos-Picot I (1999) Overproduction of Cu/Zn-superoxide dismutase or Bcl-2 prevents
the brain mitochondrial respiratory dysfunction induced by
glutathione depletion. Exp Neurol 158:428436
Thomas B, Muralikrishnan D, Mohanakumar KP (2000)
In vivo hydroxyl radical generation in the striatum following systemic administration of 1-methyl-4-phenyl-1,2,3,6tetrahydropyridine in mice. Brain Res 852:221224
68. Mecocci P, MacGarvey U, Beal MF (1994) Oxidative damage
to mitochondrial DNA is increased in Alzheimers disease.
Ann Neurol 36:747751
69. Mecocci P, Beal MF, Cecchetti R, Polidori MC, Cherubini A, Chionne F, Avellini L, Romano G, Senin U (1997)
Mitochondrial membrane fluidity and oxidative damage
to mitochondrial DNA in aged and AD human brain. Mol
Chem Neuropathol 31:5364
70. Mecocci P, Cherubini A, Senin U (1997) Increased oxidative
damage in lymphocytes of Alzheimers disease patients. J Am
Geriatr Soc 45:15361537
71. Yim MB, Kang JH, Yim HS, Kwak HS, Chock PB, Stadtman ER (1996) A gain-of-function of an amyotrophic lateral sclerosis-associated Cu, Zn-superoxide dismutase mutant:
An enhancement of free radical formation due to a decrease
in Km for hydrogen peroxide. Proc Natl Acad Sci USA
93:57095714
72. Yim HS, Kang JH, Chock PB, Stadtman ER, Yim MB (1997)
A familial amyotrophic lateral sclerosis-associated A4V Cu,
Zn-superoxide dismutase mutant has a lower Km for
hydrogen peroxide. Correlation between clinical severity and
the Km value. J Biol Chem 272:88618863
73. Wiedau-Pazos M, Goto JJ, Rabizadeh S, Gralla EB, Roe JA,
Lee MK, Valentine JS, Bredesen DE (1996) Altered reactivity
of superoxide dismutase in familial amyotrophic lateral
sclerosis. Science 271:515518
74. Warita H, Hayashi T, Murakami T, Manabe Y, Abe K (2001)
Oxidative damage to mitochondrial DNA in spinal motoneurons of transgenic ALS mice. Brain Res Mol Brain Res
89:147152
75. Schapira AH (1998) Mitochondrial dysfunction in neurodegenerative disorders. Biochim Biophys Acta 1366:225233
76. Polidori MC, Mecocci P, Browne SE, Senin U, Beal MF (1999)
Oxidative damage to mitochondrial DNA in Huntingtons disease parietal cortex. Neurosci Lett 272:5356
77. Browne SE, Bowling AC, MacGarvey U, Baik MJ, Berger SC,
Muqit MM, Bird ED, Beal MF (1997) Oxidative damage
and metabolic dysfunction in Huntingtons disease: selective
vulnerability of the basal ganglia. Ann Neurol 41:646653
78. Rotig A, de Lonlay P, Chretien D, Foury F, Koenig M, Sidi D,
Munnich A, Rustin P (1997) Aconitase and mitochondrial
ironsulphur protein deficiency in Friedreich ataxia. Nat
Genet 17:215217
79. Pandolfo M (1998) Molecular genetics and pathogenesis of
Friedreich ataxia. Neuromuscul Disord 8:409415
80. Estevez AG, Spear N, Manuel SM, Barbeito L, Radi R,
Beckman JS (1998) Role of endogenous nitric oxide and
peroxynitrite formation in the survival and death of motor
neurons in culture. Prog Brain Res 118:269280
81. Estevez AG, Crow JP, Sampson JB, Reiter C, Zhuang Y,
Richardson GJ, Tarpey MM, Barbeito L, Beckman JS (1999)
Induction of nitric oxide-dependent apoptosis in motor neurons by zinc-deficient superoxide dismutase. Science
286:24982500
82. Beal MF, Ferrante RJ, Browne SE, Matthews RT, Kowall NW,
Brown RH Jr (1997) Increased 3-nitrotyrosine in both
sporadic and familial amyotrophic lateral sclerosis. Ann
Neurol 42:644654
83. Brookes PS, Land JM, Clark JB, Heales SJ (1998) Peroxynitrite
and brain mitochondria: evidence for increased proton leak.
J Neurochem 70:21952202
84. Mecocci P, MacGarvey U, Kaufman AE, Koontz D,
Shoffner JM, Wallace DC, Beal MF (1993) Oxidative
damage to mitochondrial DNA shows marked age-dependent
increases in human brain. Ann Neurol 34:609616
456
Reactive oxygen species and mitochondrial diseases
85. Bowling AC, Mutisya EM, Walker LC, Price DL, Cork LC,
Beal MF (1993) Age-dependent impairment of mitochondrial
function in primate brain. J Neurochem 60:19641967
86. Michikawa Y, Mazzucchelli F, Bresolin N, Scarlato G,
Attardi G (1999) Aging-dependent large accumulation of
point mutations in the human mtDNA control region for
replication. Science 286:774779
87. Wang Y et al. (2001) Muscle-specific mutations accumulate
with aging in critical human mtDNA control sites for
replication. Proc Natl Acad Sci USA 98:40224027
88. Munscher C, Rieger T, Muller-Hocker J, Kadenbach B (1993)
The point mutation of mitochondrial DNA characteristic for
MERRF disease is found also in healthy people of different ages. FEBS Lett 317:2730
89. Zhang C, Linnane AW, Nagley P (1993) Occurrence of a
particular base substitution (3243 A to G) in mitochondrial
DNA of tissues of ageing humans. Biochem Biophys Res
Commun 195:11041110
457
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Nitric Oxide, and Inflammation Molecular, BiochemistryDocument264 pagesNitric Oxide, and Inflammation Molecular, BiochemistryNickKyzNo ratings yet
- Khan Academy Cellular Development QuestionsDocument3 pagesKhan Academy Cellular Development QuestionsLoraNo ratings yet
- The Enzyme List Class 7 - Translocases: ExplorenzDocument35 pagesThe Enzyme List Class 7 - Translocases: ExplorenzgustasconNo ratings yet
- Biological OxidationDocument51 pagesBiological OxidationGorav Sharma100% (2)
- BBO 2013 Round 2 PaperDocument25 pagesBBO 2013 Round 2 PapermartynapetNo ratings yet
- Abstract Book DraftDocument224 pagesAbstract Book DraftЛюбовь КрыловаNo ratings yet
- Biology Module 2Document20 pagesBiology Module 2Joemmel MagnayeNo ratings yet
- Barbier 2010Document15 pagesBarbier 2010Amod KumarNo ratings yet
- Learning Activity Sheet Grade 10-Science: Name: Zarzoso, Terence John J. Date: March 29, 2022 Rating/ScoreDocument4 pagesLearning Activity Sheet Grade 10-Science: Name: Zarzoso, Terence John J. Date: March 29, 2022 Rating/ScoreG03Angulo, Jamaica Bianca B.No ratings yet
- Apoptosis: Dr. Prabesh K Choudhary Final Year Resident MD PathologyDocument47 pagesApoptosis: Dr. Prabesh K Choudhary Final Year Resident MD PathologyAhmed BioNo ratings yet
- Worksheet in General Biology 2: Quarter 1 - Week 4: Evidences of Evolution and Evolutionary Relationships of OrganismsDocument8 pagesWorksheet in General Biology 2: Quarter 1 - Week 4: Evidences of Evolution and Evolutionary Relationships of OrganismsShastine Claor100% (1)
- Detailed Lesson Plan Grade 12 StemDocument15 pagesDetailed Lesson Plan Grade 12 Stemlibertty lumintacNo ratings yet
- Anti AgingDocument73 pagesAnti AgingAnonymous 6GiP55M3Ib100% (1)
- Cell Injury, Cell Death, and AdaptationsDocument81 pagesCell Injury, Cell Death, and AdaptationsDrSyeda RimaNo ratings yet
- Biology OxidationDocument50 pagesBiology Oxidationderhangker100% (3)
- Paracetamol-Induced Renal Tubular Injury: A Role For ER StressDocument10 pagesParacetamol-Induced Renal Tubular Injury: A Role For ER StressمحمدأميندماجNo ratings yet
- The Cell Cycle & ApoptosisDocument20 pagesThe Cell Cycle & ApoptosisSathiyaraj100% (4)
- Basic Inorganic Chemistry Part 3 Bioinorganic ChemistryDocument44 pagesBasic Inorganic Chemistry Part 3 Bioinorganic ChemistryGuru P MNo ratings yet
- Organic Chemistry A Mechanistic Approach 1st Chaloner Solution ManualDocument3 pagesOrganic Chemistry A Mechanistic Approach 1st Chaloner Solution ManualPhyllis Sollenberger100% (29)
- Perbedaan MCF 7 Dan t47dDocument9 pagesPerbedaan MCF 7 Dan t47dmuflihNo ratings yet
- CH5 - Lesson 16 The Process of Evolution PDFDocument5 pagesCH5 - Lesson 16 The Process of Evolution PDFgwynethNo ratings yet
- Gel Electrophoresis: How Does It Work?: Dye Electrophoresis Purdue University Van ProjectDocument19 pagesGel Electrophoresis: How Does It Work?: Dye Electrophoresis Purdue University Van ProjectAnuradha KumariNo ratings yet
- Mechanisms of Drug-Induced HepatotoxicityDocument20 pagesMechanisms of Drug-Induced Hepatotoxicityfebri kusuma arfiskaNo ratings yet
- Maccarone 2000Document37 pagesMaccarone 2000Матиас Себальос ГусманNo ratings yet
- Metabolic Effects of 3,5-Diiodo-L-Thyronine Giammanco M Et AlDocument11 pagesMetabolic Effects of 3,5-Diiodo-L-Thyronine Giammanco M Et AlMarco GiammancoNo ratings yet
- Amino Acid Sequences: Indicators of Evolution: ProblemDocument5 pagesAmino Acid Sequences: Indicators of Evolution: ProblemRachele AmoraNo ratings yet
- Chapter 16 Lab Amino Acid Sequences - Indicators of EvolutionDocument6 pagesChapter 16 Lab Amino Acid Sequences - Indicators of EvolutionayshahabuahyehNo ratings yet
- Genbio Mod 2Document10 pagesGenbio Mod 2ScionNo ratings yet
- Electron Transport and Oxidative PhosphorylationDocument34 pagesElectron Transport and Oxidative PhosphorylationAbeWatanabeNo ratings yet
- Dosis DoxoDocument12 pagesDosis DoxodeyaNo ratings yet