Professional Documents
Culture Documents
The Search For Elusive Structure: A Promiscuous Realist Case For Researching Specific Psychotic Experiences Such As Hallucinations
Uploaded by
Susana Campos SotoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Search For Elusive Structure: A Promiscuous Realist Case For Researching Specific Psychotic Experiences Such As Hallucinations
Uploaded by
Susana Campos SotoCopyright:
Available Formats
Schizophrenia Bulletin vol. 40 suppl. no. 4 pp.
S198S201, 2014
doi:10.1093/schbul/sbu044
The Search for Elusive Structure: A Promiscuous Realist Case for Researching
Specific Psychotic Experiences Such as Hallucinations
Richard P.Bentall*,1
School of Psychological Sciences, Institute of Psychology, Health and Society, University of Liverpool, Liverpool, UK
*To whom correspondence should be addressed; School of Psychological Sciences, Institute of Psychology, Health and Society,
University of Liverpool, Liverpool L69 3GL, UK; tel: +44-151-795-5367, e-mail: richard.bentall@liverpool.ac.uk
Key words: hallucinations/diagnosis/schizophrenia
The past three decades have seen a steady increase in
the volume of research on psychotic phenomena. In the
early 1980s, publications on symptoms were rare (36
papers with hallucinations in their titles were published in 1983 with a cumulative number of 1630 papers
until that time; Google Scholar, accessed February
14, 2014). Thirty years later, research on symptoms is
more vibrant (336 papers with hallucinations in their
title published in 2013 with a cumulative total of 6320
papers). This development has been fueled by the invention of new research technologies (notably functional
magnetic resonance imaging) that have made symptoms
more tractable objects of scientific inquiry, and by a need
to understand underlying mechanisms prompted by the
emergence of novel interventions. In introducing this
Special Supplement on Hallucinations, I want to focus
on a third compelling reason for focusing research on
particular kinds of psychotic experience such as hallucinations: the apparently intractable problem of psychiatric classification.
Recent Attempts to Solve Problems of Psychiatric
Classification
Toward the end of the first century of schizophrenia
research, a few observers noted that broad diagnoses such
as schizophrenia were scarcely adequate as independent
variables in research because they were defined inconsistently, failed to cleave nature at its joints, and grouped
together problems which probably had little in common.1,2 At the time this was a minority position. However,
the need for a nondiagnosis-based research strategy has
become much more widely accepted in the intervening
years, most notably among biological researchers such
as geneticists,3 and pharmacologists,4 leading NIMH to
recently propose the Research Domain Criteria (RDoC)
approach.5 This debate has not been resolved by the publication of successive editions of the DSM6 and, indeed,
seems to have intensified with the publication of DSM-5
which, claims to the contrary notwithstanding, has
achieved poor reliability in field trials.7
One solution to this problem is to attempt to develop
empirically based classification systems. Two proposals appear to be gaining traction at the time of writing.
First, analyses of patterns of comorbidity between different diagnoses suggest that the common psychiatric
conditions fall into 2 broad spectra of internalizing and
externalizing disorders, the former subdividing into anxious misery and fear and the latter including conduct
and substance abuse disorders.8 A large international
study of nonpsychotic DSM-defined disorders9 recently
found considerable comorbidity within the spectra (eg,
individuals who met the criteria for depressionan internalizing disorderhad a high probability of meeting
the criteria for generalized anxiety, also an internalizing
disorder) but not across the spectra. Interestingly, there
was no particular order of acquisition when comorbidity
occurred (eg, some people became anxious before they
became depressed and vice versa). Recent studies have
The Author 2014. Published by Oxford University Press on behalf of the Maryland Psychiatric Research Center.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0/), which
permits unrestricted reuse, distribution, and reproduction in any medium, provided the original work is properly cited.
S198
Downloaded from http://schizophreniabulletin.oxfordjournals.org/ at UTALCA on August 5, 2014
Problems in psychiatric classification have impeded
research into psychopathology for more than a century.
Here, I briefly review several new approaches to solving
this problem, including the internalizing-externalizing-psychosis spectra, the 5-factor model of psychotic symptoms,
and the more recent network approach. Researchers and
clinicians should probably adopt an attitude of promiscuous realism and assume that a single classification system
is unlikely to be effective for all purposes, and that different systems will need to be chosen for research into etiology, public mental health research, and clinical activities.
Progress in understanding the risk factors and mechanisms
that lead to psychopathology is most likely to be achieved
by focusing on specific types of experience or symptoms
such as hallucinations.
The Search for Elusive Structure
instructive. Nearly two and a half centuries after the death
of Carl Linnaeus, who devised the general approach to
biological classification, some observers have argued that
continuing disputes about how to define the boundaries
between species cannot be definitively resolved, so that
biologists should accept a doctrine of promiscuous realism.17 Adopting the same doctrine, psychopathologists
should perhaps accept that, while there is structure in the
way that symptoms co-occur, the structure is so complex
that a one size-fits-all method of classification cannot be
expected to suit all purposes. What works in etiological
research, for the purposes of investigating public mental
health and in the clinic may well be different.
Recognizing Complexity
When a problem seems intractable it is sensible to examine some of the underlying assumptions that have driven
past attempts to solve it. Borsboom18 reminds us that one
such assumption is that syndromes are caused by latent
entities. Hence, it is assumed that, if there is a cluster
of symptoms corresponding to the diagnosis of schizophrenia, this implies that schizophrenia is the cause
of the symptoms. This idea leads to the diagnosis being
employed as an independent variable when attempting to
investigate the etiology of psychiatric disorders. However,
structure may arise for many reasons and, as Borsboom
points out, is not always best interpreted as evidence of a
causal latent entity.
Developing this idea further, Borsboom and Cramer19
have proposed that syndromes can arise because symptoms create the conditions in which other symptoms are
likely to occur. To take the simplest example possible,
sleep problems and problems of concentration both
appear in lists of the symptoms of depression but this is
not because depression (a latent entity inferred from
the symptoms) causes both sleep problems and poor concentration but because sleep problems lead to problems
of concentration. Moreover, it is also no surprise that
depression and anxiety tend to be comorbid diagnoses
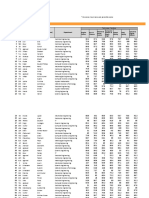
Fig.1. Speculative hierarchical partial classification of psychopathology, integrating the bifactor, internalizing-externalizing-psychosis,
and 5-factor models.
S199
Downloaded from http://schizophreniabulletin.oxfordjournals.org/ at UTALCA on August 5, 2014
extended this model to establish that the psychotic disorders appear to form a separate, third spectrum.10
Research on the symptoms of psychotic patients, however, has produced a somewhat different picture. Using
factor analysis, Liddle11 first reported 3 clusters of positive, negative, and cognitive disorganization symptoms,
but more recent research has converged on 5 factors by
adding depression and mania as separate factors.12,13
To add further levels of complexity, some studies have
suggested that, superordinate to both the internalizingexternalizing-psychosis spectra14 and the 5-factor model
of psychosis,15 there is a general psychopathology or
P factor common to all psychiatric disorders, perhaps
reflecting neuroticism or emotional instability (this latter
type of model is known as a bifactor model).
It is not yet clear if or how these models can be reconciled. As depression seems to belong to anxious misery in the internalizing spectrum and mania presumably
belongs to the externalizing spectrum, it is tempting to
nest the remaining psychosis factors within the psychosis
spectrum (see figure1) leading to a hierarchical classification scheme similar to the system used by biologists when
classifying species (note that this scheme can, in principle,
be continued further, eg, by dividing hallucinations into
different subtypes; see McCarthy-Jones etal16). However,
such a scheme would have to overcome many obstacles.
It should be recognized, to begin with, that it is a classification of symptoms and not people (a distinction which
is sometimes overlooked). Indeed, patients can obviously
experience more than one type of symptom, whichever
level we decide to describe them on. There is as yet no
evidence that either the Internalizing-ExternalizingPsychosis, 5 factor or hybrid models efficiently predict,
eg, responses to particular treatments or map on to etiological factors such as genetic or neuropsychological
variables. It is no wonder that many researchers believe
that, pragmatically, we have no alternative but to cling to
categorical diagnoses for the time being.
Clearly, psychiatric taxonomy is a work in progress,
and the comparison with biological species may be
R. P.Bentall
Shortcutting the Quest for Elusive Structure
Research targeted at particular symptoms such as hallucinations has long been recognized as a rational strategy
for bypassing the unsolved problem of psychiatric classification,25 as exemplified by the contributions to this
special supplement, none of which focus specifically on
schizophrenia. Borsbooms19 network analysis provides
further impetus for this approach, because the attempt
to understand the mechanisms underlying each symptom
will help us understand the networks of causal relationships between them. For example, to understand that
delusions can sometimes lead to hallucinations it helps
to know that the perceptual judgments of hallucinating
patients are excessively influenced by their prior beliefs.
Further advantages of a symptom-based research strategy have been noted by others, eg, the likelihood of
revealing mechanisms that are suitable targets for pharmacological4 or psychological26 intervention.
However, the comorbidity between symptoms observed
in taxonomic research and explained by the network
model also raises the hazard that factors attributed to one
symptom will be misattributed to a comorbid symptom.
Avoiding this hazard requires the use of careful designs
and appropriate statistical techniques. For example, a
wide range of social adversities are known to increase the
risk of psychosis, including childhood trauma and the
loss of a parent at an early age but, only by controlling
for the comorbidity between symptoms is it possible to
show that childhood sexual abuse is a more potent risk
factor for hallucinations than paranoid delusions and
that, conversely, attachment-threatening events are a
S200
greater risk factor for paranoia than hallucinations.27,28
Similarly, although abnormal metacognitive beliefs have
sometimes been thought to play a causal role in hallucinations,29 when controlling for comorbid symptoms,
it seems that metacognitive beliefs are implicated in the
distress associated with hallucinations rather than their
occurrence.30
As the contributors to this special supplement demonstrate, further progress in symptom-based research will
require multiple methodologies and perspectives, ranging from the humanities,31 through psychology (many of
the contributions) to the neurosciences.32 Attention must
be given to phenomenology (as demonstrated by most
of the other contributions). For some purposes it will
be important to study subtypes,16 particular modalities
(visual hallucinations having been relatively neglected;
Waters et al33) or dimensions of experience.34 Research
must not only focus on patients but also healthy individuals35 and should consider special groups such as children36
or people living in non-Western cultures.37 Undoubtedly,
symptom-based research has the potential to enhance
our ability to help people who are distressed by their psychotic experiences, either through novel interventions26 or
by aligning itself with service user and expert-by-experience initiatives.38
Symptom-based research is compatible with the NIMH
RDoC approach5 because the strategy concerns the
objects of research whereas RDoC concerns the mechanisms to be investigated. I have argued elsewhere that it
has the potential to lead to an entirely satisfactory account
of psychopathology20 but, in the spirit of promiscuous
realism, perhaps Ishould now say that it might have this
potential. Whether, after a second century of research on
psychosis, we will still need the kind of categorical diagnoses that have been used so often during the first century
seems doubtful, but will only become evident with time.
Acknowledgment
The author has declared that there are no conflicts of
interest in relation to the subject of this study.
References
1. Brockington I. Schizophrenia: yesterdays concept. Eur
Psychiatry. 1992;7:203207.
2. Bentall RP. The syndromes and symptoms of psychosis: or
why you cant play 20 questions with the concept of schizophrenia and hope to win. In: Bentall RP, ed. Reconstructing
Schizophrenia. London: Routledge; 1990:2360.
3. Craddock N, Owen MJ. The beginning of the end for the
Kraepelinian dichotomy. Br J Psychiatry. 2005;186:364366.
4. Fibiger HC. Psychiatry, the pharmaceutical industry, and the
road to better therapeutics. Schizophr Bull. 2012;38:649650.
5. Ford JM, Morris SE, Hoffman RE, et al. Studying hallucinations within the NIMH RDoC framework. Schizophr Bull.
2014.
Downloaded from http://schizophreniabulletin.oxfordjournals.org/ at UTALCA on August 5, 2014
because problems of concentration are often regarded as
symptoms of both. Syndromes and comorbidity between
diagnoses therefore emerge as a consequence of networks
of causal relations between symptoms.
In an analysis of the positive syndrome which anticipated Borsbooms work, Ipreviously noted that hallucinations might sometimes give rise to delusions and vice
versa.20 For example, it has long been recognized that
delusional beliefs can be prompted by attempts to explain
anomalous experiences21 and one well-known psychological model of paranoia gives priority to this mechanism.22 It is less recognized that the perceptual judgments
of hallucinating patients can be influenced by suggestions
affecting their beliefs about what they are likely to experience.23 Consistent with this network account, a recent
study investigated whether hallucinations precede delusions or vice versa in first episode psychosis, and found
that 18.2% of patients experienced delusions only, in
19.5% of cases delusions preceded hallucinations by at
least 1 month, and in 16.4% hallucinations preceded delusions.24 In the remaining 45.9% both symptoms appeared
within the same month (interestingly, no patients who
experienced hallucinations alone were recorded).
The Search for Elusive Structure
24. Compton MT, Potts AA, Wan CR, Ionescu DF. Which came
first, delusions or hallucinations? An exploration of clinical
differences among patients with first-episode psychosis based
on patterns of emergence of positive symptoms. Psychiatry
Res. 2012;200:702707.
25. Bentall RP, Jackson HF, Pilgrim D. Abandoning the concept
of schizophrenia: some implications of validity arguments
for psychological research into psychotic phenomena. Br J
Clin Psychol. 1988;27(pt 4):303324.
26. Thomas N, Hayward M, Peters E, et al. Psychological therapies for auditory hallucinations (voices): current status and
key directions for future research. Schizophr Bull. 2014.
27. Bentall RP, Wickham S, Shevlin M, Varese F. Do specific
early-life adversities lead to specific symptoms of psychosis? Astudy from the 2007 the Adult Psychiatric Morbidity
Survey. Schizophr Bull. 2012;38:734740.
28. Sitko K, Bentall RP, Shevlin M, OSullivan N, Sellwood, W.
Associations between specific psychotic symptoms and specific childhood adversities are mediated by attachment styles.
Psychiatry Res. In press.
29. Morrison AP. The interpretation of intrusions in psychosis:
an integrative cognitive approach to hallucinations and delusions. Behav Cogn Psychother. 2001;29:257276.
30. Varese F, Bentall RP. The metacognitive beliefs account of
hallucinatory experiences: a literature review and meta-analysis. Clin Psychol Rev. 2011;31:850864.
31. Woods A, Jones N, Bernini M, et al. Interdisciplinary
approaches to the phenomenology of auditory verbal hallucinations. Schizophr Bull. 2014.
32. Ffytche DH, Wible CG. From tones in tinnitus to sensed
social interaction in schizophrenia: how understanding cortical organization can inform the study of hallucinations and
psychosis. Schizophr Bull. 2014.
33. Waters F, Collerton D, Ffytche D, et al. Information from
neurodegenerative disorders and eye disease. Schizophr Bull.
2014.
34. Woodward TS, Jung K, Hwang H, et al. Symptom dimensions of the psychotic symptom rating scales (PSYRATS) in
psychosis: a multi-site study. Schizophr Bull. 2014.
35. Johns L, Kompus K, Connell M, et al. Auditory verbal hallucinations in persons with and without a need for care.
Schizophr Bull. 2014.
36. Jardri R, Bartels-Velthuis AA, Debban M, et al. From phenomenology to neurophysiological understanding of hallucinations in children and adolescents. Schizophr Bull. 2014.
37. Lari F, Luhrmann T, Bell V, et al. Culture and hallucinations: overview and future directions. Schizophr Bull. 2014.
38. Corstens D, Longden E, McCarthy-Jones S, Waddingham R,
Thomas N. Emerging perspectives from the Hearing Voices
Movement: implications for research and practice. Schizophr
Bull. 2014.
S201
Downloaded from http://schizophreniabulletin.oxfordjournals.org/ at UTALCA on August 5, 2014
6. Bentall RP. Doctoring the Mind: Why Psychiatric Treatments
Fail. London: Penguin; 2009.
7. Freedman R, Lewis DA, Michels R, etal. The initial field trials of DSM-5: new blooms and old thorns. Am J Psychiatry.
2013;170:15.
8. Krueger RF. The structure of common mental disorders.
Arch Gen Psychiatry. 1999;56:921926.
9. Kessler RC, Ormel J, Petukhova M, et al. Development
of lifetime comorbidity in the World Health Organization
world mental health surveys. Arch Gen Psychiatry.
2011;68:90100.
10. Kotov R, Chang SW, Fochtmann LJ, etal. Schizophrenia in
the internalizing-externalizing framework: a third dimension?
Schizophr Bull. 2011;37:11681178.
11. Liddle PF. The symptoms of chronic schizophrenia. A reexamination of the positive-negative dichotomy. Br J
Psychiatry. 1987;151:145151.
12. Demjaha A, Morgan K, Morgan C, et al. Combining
dimensional and categorical representation of psychosis:
the way forward for DSM-V and ICD-11? Psychol Med.
2009;39:19431955.
13. van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635645.
14. Caspi A, Houts RM, Belsky DW, etal. The p factor: one general psychopathology factor in the structure of psychiatric
diorders? Clin Psychol Sci. 2014;2:119137.
15. Reininghaus U, Priebe S, Bentall RP. Testing the psychopathology of psychosis: evidence for a general psychosis dimension. Schizophr Bull. 2013;39:884895.
16. McCarthy-Jones S, Thomas N, Strauss C, et al. Better than
mermaids and stray dogs? Subtyping auditory verbal hallucinations and its implications for research and practice.
Schizophr Bull. 2014.
17. Dupr J. The Disorder of Things: Metaphysical Foundations of
the Disunity of Science. Cambridge, MA: Harvard University
Press; 1993.
18. Borsboom D. Psychometric perspectives on diagnostic systems. J Clin Psychol. 2008;64:10891108.
19. Borsboom D, Cramer AO. Network analysis: an integrative
approach to the structure of psychopathology. Annu Rev Clin
Psychol. 2013;9:91121.
20. Bentall RP. Madness Explained: Psychosis and Human
Nature. London: Penguin; 2003.
21. Maher BA. Delusional thinking and perceptual disorder.
J Individ Psychol. 1974;30:98113.
22. Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington
PE. A cognitive model of persecutory delusions. Br J Clin
Psychol. 2002;41:331347.
23. Haddock G, Slade PD, Bentall RP. Auditory hallucinations
and the verbal transformation effect: the role of suggestions.
Pers Indiv Differ. 1995;19:301306.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- English II Homework Module 6Document5 pagesEnglish II Homework Module 6Yojana DubonNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- 2 How To - Tests of Copy Configuration From Client 000 - Note 2838358 - Part3Document15 pages2 How To - Tests of Copy Configuration From Client 000 - Note 2838358 - Part3Helbert GarofoloNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Innoventure List of Short Listed CandidatesDocument69 pagesInnoventure List of Short Listed CandidatesgovindmalhotraNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Chemical EngineeringDocument26 pagesChemical EngineeringAnkit TripathiNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- CLOCKSDocument62 pagesCLOCKSdasarajubhavani05No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Sasi EnriquezDocument9 pagesSasi EnriquezEman NolascoNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Expanding UNIT 1 For 2º ESO.-the History of Music NotationDocument1 pageExpanding UNIT 1 For 2º ESO.-the History of Music NotationEwerton CândidoNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Solar Water Pump Supreme RevDocument22 pagesSolar Water Pump Supreme RevBelayneh TadesseNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Gate Question (Limit) PDFDocument4 pagesGate Question (Limit) PDFArpit Patel75% (4)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Director Engineering in Detroit MI Resume Shashank KarnikDocument3 pagesDirector Engineering in Detroit MI Resume Shashank Karnikshashankkarnik100% (1)
- D062/D063/D065/D066 Service Manual: (Book 1 of 2) 004778MIU MainframeDocument1,347 pagesD062/D063/D065/D066 Service Manual: (Book 1 of 2) 004778MIU MainframeevpsasaNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- MODBUSDocument19 pagesMODBUSJosé Luis MartínezNo ratings yet
- About Karmic Debt Numbers in NumerologyDocument3 pagesAbout Karmic Debt Numbers in NumerologyMarkMadMunki100% (2)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Unit 3Document9 pagesUnit 3Estefani ZambranoNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Green ManagementDocument58 pagesGreen ManagementRavish ChaudhryNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Backup Archive and Recovery Archive Users and PermissionsDocument5 pagesBackup Archive and Recovery Archive Users and PermissionsgabilovesadellaNo ratings yet
- Modicon M580 Quick Start - v1.0 - Training ManualDocument169 pagesModicon M580 Quick Start - v1.0 - Training Manualaryan_iust0% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Leadership and FollowershipDocument43 pagesLeadership and FollowershipNishant AgarwalNo ratings yet
- Testing: Instructor: Iqra JavedDocument32 pagesTesting: Instructor: Iqra Javedzagi techNo ratings yet
- Effective Problem Solving and Decision MakingDocument46 pagesEffective Problem Solving and Decision MakingAndreeaMare1984100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- F PortfolioDocument63 pagesF PortfolioMartin SchmitzNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Daily Lesson Log: Department of EducationDocument10 pagesDaily Lesson Log: Department of EducationStevenson Libranda BarrettoNo ratings yet
- Absolute Duo 1 PDFDocument219 pagesAbsolute Duo 1 PDFAgnieškaRužičkaNo ratings yet
- Lab ManualDocument69 pagesLab ManualPradeepNo ratings yet
- Titanic Is A 1997 American Romantic Disaster Film Directed, Written. CoDocument13 pagesTitanic Is A 1997 American Romantic Disaster Film Directed, Written. CoJeric YutilaNo ratings yet
- A Brief About Chandrayaan 1Document3 pagesA Brief About Chandrayaan 1DebasisBarikNo ratings yet
- Fall 2011 COP 3223 (C Programming) Syllabus: Will Provide The Specifics To His SectionDocument5 pagesFall 2011 COP 3223 (C Programming) Syllabus: Will Provide The Specifics To His SectionSarah WilliamsNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Carl Jung - CW 18 Symbolic Life AbstractsDocument50 pagesCarl Jung - CW 18 Symbolic Life AbstractsReni DimitrovaNo ratings yet
- DonnetDocument12 pagesDonnetAsia SzmyłaNo ratings yet
- Lip Prints: IntroductionDocument4 pagesLip Prints: Introductionkaran desaiNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)