Professional Documents
Culture Documents
B10Ph01 - Dermatologic Pharmacology
Uploaded by
Charles Jebb Belonio JuanitasCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
B10Ph01 - Dermatologic Pharmacology
Uploaded by
Charles Jebb Belonio JuanitasCopyright:
Available Formats
Block X | Pharmacology | Lesson 1
Dermatologic Pharmacology
Myrna L. Abello, MD, Ed.D.
SGD 4C
September 18, 2015
I
II
III
IV
V
VI
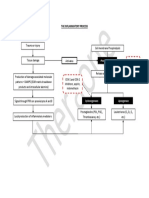
SUMMARY/OUTLINE
DERMATOLOGIC
PHARMACOLOGY
Dermatologic Pharmacology
Pharmacological Response
Absorption
Choice of a Vehicle
Topical Application
Glucocorticoids
A Anti-Inflammatory Effects
B 7 Classes
C Principles in the use of Steroids
D Adverse Effects
VII Systemic Glucocorticoids
A Adverse Effects
PHARMACOLOGICAL RESPONSE
VIII Tar Compounds
DETERMINED BY:
IX Topical Antibacterial Agents
A BACITRACIN
B GRAMICIDIN
C MUPIROCIN
D RETAPAMULIN
E POLYMYXIN B SULFATE
F NEOMYCIN
G GENTAMICIN
X Topical Antibiotic in Acne
A CLINDAMYCIN
B ERYTHROMYCIN
C METRONIDAZOLE
D TETRACYCLIN
E SODIUM SULFACETAMIDE
XI Acne Preparations
A RETENOIC ACID
B ISOTRETINOIN
C ETRITINATE
XII Anti-Pruritic Agents
A DOXEPIN
B PRAMOXINE
XIII Anti-histamines
A OLDER H1 RECEPTOR ANTAGONISTS
B NEWER H1 RECEPTOR ANTAGONISTS
C H2 RECEPTOR BLOCKERS
XIV Agents Affecting Pigmentation
A HYDROQUINONE & MONOBENZONE
B HYDROQUINONE
C MONOBENZONE
D GLUTATHIONE
E POLYPHENOLIC-GLUTATHION (GSH)
XV Sunscreens
XVI Keratolytic Agents
SGD
Page 1 of 14
4C|
GANZON,
Drugs used in the treatment of the skin can be:
1. Delivered Systemically
o Gets into the system
2. Applied Topically
o Apply to site where the drug is
wanted to act
3. Injected Directly to the Dermis
4. Phototherapy-Ultraviolet Radiation
1. Regional variation in drug penetration
Areas in the body are more permeable and
may require less drug for equivalent effect
Examples: scrotum, face, axilla and scalp >
forearm (in terms of permeability)
2. Concentration Gradient
An increase in concentration gradient
increases the mass of the drug transferred
per unit time
Example: Resistance to corticosteroids can
sometimes be overcome by use of higher
concentrations of drug
3. Dosing schedule
Local Half-life may be long enough to
permit once daily application with short
systemic half-lives
Example: steroids (given once a day) is as
effective as multiple applications in many
conditions
4. Vehicles & Occlusion
An appropriate vehicle maximizes the ability
of the drug to penetrate the outer layers of
the skin
o Vehicles
may
themselves
have
important therapeutic effects
Occlusion (plastic wrap to hold drug and
vehicle to skin)
JUMAWAN,
PINEDA,
UDDIN
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
o Extremely effective in maximizing efficacy
5. State of the stratum corneum
Topical absorption increased in dermatologic disorders due to the presence of
breaks/lesions in the skin
6. Presence of Penetration Enhancers
Examples: Organic solvents such as dimethyl sulfoxide (DMSO), urea, salicylic acid
o Added to the drug for better penetration
ABSORPTION CONTROLLED BY:
1. Concentration of drug in the vehicle
Rate of diffusion is proportional to concentration
The higher the concentration, the more effective it is
2. The partition coefficient of drug between the stratum corneum and the
vehicle
Partition coefficient is the Drugs ability to escape from the vehicle
Application of topical preparation is incorporated into a vehicle and will take time
for the drug to get out of vehicle and exert its effect
Increased lipid-solubility favors penetration through the skin in the relatively
lipophilic stratum corneum
3. Diffusion coefficient of the drug in the stratum corneum
Refers to the extent to which the matrix of the barrier restricts the mobility of the
drug
An Increase in the molecular size of the drug will decrease the diffusion coefficient.
Drugs with greater molecular size, would cross the membrane with difficulty while
drugs with smaller molecular size will cross the membrane with ease
CHOICE OF A VEHICLE
A vehicle is any of various media acting usually as solvents, carriers, or binders for active
ingredients.
A. Acute inflammation with oozing, vesiculation & crusting
Best treated with drying preparations (e.g. Tinctures, Wet dressings, lotions)
Lotions & Solutions are ideal for hairy & intertriginous areas
Choice of vehicle will depend on the type of lesion
B. Chronic Inflammation with xerosis, scaling & lichenification
Best treated with more lubricating preparations (e.g. Creams or Ointments)
Page 2 of 14
2 FTU
4 hand areas
FACE & NECK
2.5 FTU
(1.3g)
FRONT OF TRUNK
7 FTU (3.5g)
Block X |PHARMACOLOGY | Lesson 1
Dermatologic
Pharmacology
ONE
ARM
3 FTU (1.5g)
ONE HAND (FRONT
AND BACK)
ONE LEG
1 FTU (0.5g)
6 FTU (3.0g)
Cream
o Most
acceptable
and
common preparation
o Safer to use if in doubt if
lesion is wet or dry
o Emulsion of oil and water
Ointment
oMost
effective
hydrating
agents
oGreasy & often undesirable
(oleaginous base e.g. petrolatum,
mineral oil)
HOW MUCH TO APPLY?
o
o
Fingertip Unit (FTU)
Amount
of
ointment
when
squeezed out of a tube to the
palmar aspect of the index finger
from the distal skin crease to the
end of the finger
Sort of an estimate
Approximate Value
Males: 0.47g
Females: 0.42g
Generally rounded off to
0.50g or 1/2 g
TOPICAL GLUCOCORTICOIDS
Known as steroids in laymens
term
Therapeutic
effectiveness
based
primarily
on
their
antiinflammatory activity
Antimitotic activity on human
epidermis may account for additional
mechanism of action in psoriasis
Mechanism of Action:
All natural and synthetic glucocorticoids
act by:
Page 3 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
ANTI-INFLAMMATORY EFFECTS OF
GLUCOCORTICOIDS/STEROIDS
Decreased production of prostaglandins, cytokines & interleukins
o Inhibit synthesis of these substances which are called autacoids
Decreased proliferation & migration of lymphocytes & macrophages
o By the inhibition of accumulation of neutrophils and monocytes at the site of
inflammation
7 CLASSES OF TOPICAL
GLUCOCORTICOIDS
1
Betamethasone 0.05% Diproprionate (Diprolene) in optimized vehicle (ointment,
cream etc)
Highest
Clobetasol Propionate (Temovate) 0.05%
efficacy, most potent
Amcinonide ointment 0.1% (Cyclocort)
Betamethasone Dipropionate ointment 0.05% (Diprosone)
- High efficacy
Betamethasone Dipropionate Cream 0.05%
Betamethasone Valerate Ointment 0.1% (Valisone)
- Intermediate efficacy
Fluocinolone Acetonide Cream 0.025% (Synalar)
Triamcinolone Acetonide Ointment 0.9% (Kenalog)
- Low efficacy
5
6
Betamethasone Dipropionate Lotion 0.05% (Diprosone)
Aclomethasone Dipropionate Cream, Ointment 0.05% (Aclovate)
- Low efficacy
Page 4 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
Dexamethasone Sodium Phosphate Cream 0.1% (Decadron)
Hydrocortisone Cream, Ointment, Lotion 0.5% 1%, 2.5% (Hytone, Nutracort, Penicort)
- Lowest efficacy
- Least potent
Class 1 Most Potent Class 7 Least Potent
Important since there are instances when we need a high or low efficacy drugs
PRINCIPLES IN THE USE OF STEROIDS
Steroid to be used chosen on basis of potency, site of involvement &severity
o Face is easy to penetrate so we use dose with lesser efficacy
Often a more potent steroid is used initially- Class 1
Twice-a-day application is sufficient; more frequent application does not improve
response
o There is such a thing as half-life and it will stay there for a certain period of time
ADVERSE EFFECTS
Usually, the adverse effects may be found topically but our problem with adverse effects
is those that are absorbed into the system. As much as possible, we would not want
them to be absorbed in the system
All absorbable topical corticosteroids possess the potential to suppress the pituitaryadrenal axis
o See-saw effect
o From local application, they can be absorbed into the system
Applying potent corticosteroid to extensive areas of the body for prolonged periods
increases the likelihood of systemic effects
Children more susceptible & growth retardation is a concern
o Results to early closure of long bones
o Be more careful when dealing with children and steroids
Adverse local effects:
o Usually occurs when applying topical steroids
o Atrophy
- Present as depressed, shiny, often wrinkled Cigarette Paper
Page 5 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
- appearing skin with prominent telangiectasia
- Occurs in the site of application
A tendency to develop purpura & ecchymosis (aka Steroid Rosacea)
o Persistent erythema, telangiectatic vessels, pustules, & papules in central facial
distribution; Perioral dermatitis, steroid acne
Alterations of cutaneous infections, hypopigmentation, hypertrichosis, increased
intraocular pressure, & allergic contact dermatitis
Intralesional glucocorticoids can cause cutaneous atrophy & hypopigmentation
o They are not very safe drugs
SYSTEMIC GLUCOCORTICOIDS
Systemic: absorbed in the system
Reserve for acute treatment of transient illnesses or life-threatening dermatoses
Fewer side effects with every other day dosing & prednisone tapered to every other day
ASAP
o e.g. Daily dose of 3x a day then reduce to 2x a day, then to once a day, to every
other day
o Reason: reduced gradually for less adverse effects for withdrawal, and to prevent
ADRENAL CRISIS
ADVERSE EFFECTS: SYSTEMIC
GLUCOCORTICOIDS
Short Term Oral
o Psychiatric problems, cataracts, myopathy, avascular necrosis, hypertension
Pulsed IV
o Intravenous administration of steroids
o Hypo or hypertension, hypo or hyperkalemia, anaphylactic reaction, acute
psychosis, seizures,& sudden death
If we can avoid them, we avoid them.
TAR COMPOUNDS
Used mainly for the treatment of psoriasis, dermatitis & lichen simplex chronicus
Has Antipruritic properties (due to phenolic constituents)
Acute dermatitis may be irritated by even a weak preparation (Contraindicated)
Useful in sub-acute and chronic dermatitis and psoriasis
ADVERSE EFFECTS: irritant folliculitis, photoirritation, allergic contact dermatitis
TOPICAL ANTIBACTERIAL AGENTS
Not recommended because of possibility of sensitization
Not given systemically due to many side effects
Sensitization - main cause of the discontinuation of certain drug practices
o e.g. use of sulaminamide, applying penicillin to open wounds, discontinue of usage
of antihistaminic drugs
Page 6 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
BACITRACIN & GRAMICIDIN
Gram (+) organisms, streptococcus, pneumococcus & staphylococcus
Not used systemically because they are toxic
MOA: inhibits cell wall synthesis
Sensitization low in therapeutic concentrations
Most anaerobic cocci, Neisseriae, Tetanus bacilli, Diphtheria bacteria are sensitive
A. BACITRACIN
Compounded in ointment base alone or with neomycin, polymyxin B or both (aka BNP
ointment)
Microbial resistance may develop after prolonged use
Side Effects: Contact urticaria, anaphylaxis, systemic toxicity (rare), contact
dermatitis (frequent)
was isolated from a girl named Tracy
very harmful antibiotics in a sense that they have side-effects thats why theyre only
given locally and not systemically..
B. GRAMICIDIN
Combined with neomycin, polymyxin, bacitracin, nystatin
Available only for topical use
Neomycin is an aminoglycoside
o Side Effects: Nephrotoxic, Ototoxic, Neuromuscular defects
o Sensitization is low in therapeutic concentration
o Also used as antiseptic in surgery because aminoglycosides are not absorbed in
GI tract and stay in GI canal to disinfect area
C. MUPIROCIN (Bactroban)
Relatively new drug
Effective against most Gram (+) aerobic bacteria including MRSA
Effective in impetigo caused by S. Aureus & Group A Beta Hemolytic Strep
o Used to treat Impetigo contagiosa specifically
o Mercury was the former treatment but is now known to be toxic and banned
o E.g. mercurechrome and merthiolate
Not appreciably absorbed systemically on intact skin
Not absorbed systemically is preferred for topical drugs
D.
RETAPAMULIN
New synthetic drug, newer than mupirocin
Semisynthetic drug derived from pleuromutilin
Effective in treatment of uncomplicated superficial skin infection caused by Grp. A
beta-hemolytic strep and S. aureus excluding MRSA for adult and pediatric patients 9
months and older
E. POLYMYXIN B SULFATE
Page 7 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
Mixed with drugs mentioned earlier
Peptide antibody effective against Gram (-) organism including P. Aeruginosa, E. Coli,
Enterobacter & Klebsiella
Also effective with Proteus, Serratia, Gm (+) resistant species (Katzung: they are
resistant)
MOA: Act on cell membrane. Toxic because the normal cell membrane will be affected
Not to exceed 200mg when applied to denuded skin
o Causes neurotoxicity and nephrotoxicity
Hypersensitivity is uncommon because it is not usually used
F.
NEOMYCIN
Aminoglycoside
Gm (-) including E. Coli, Proteus, Klebsiella & Enterobacter
MOA: inhibits CHON synthesis
Available in topical formulation
Rarely detectable in serum concentrations
In presence of renal failure, it accumulates and results in neurotoxicity, nephrotoxicity
and ototoxicity, neuromuscular blockage
Adverse effects of aminoglycosides in general
Sensitization in eczematoid dermatitis
Cross sensitivity to streptomycin, kanamycin, paromomycin and gentamicin (other
aminoglycosides)
o Cross-sensitivity means that even if an individual has not been exposed to these
drugs, he may still develop allergies to other related drugs (same family and
structure)
o If the patient is allergic to one aminoglycoside, avoid administering other
aminoglycosides
G.
GENTAMICIN
Aminoglycoside, narrow spectrum antibiotic for Gram Negative
Greater activity against pseudomonas
More active against Staph & Group A Beta Hemolytic Streptococci
Used systemically, not topically
Widespread topical use should be avoided
o Produces gentamicin resistant strain
Serum concentration of 1-8 g
Accumulation in renal failure
o Results to Neurotoxicity, nephrotoxiciy and ototoxicity, neuromuscular blockage
Discouraged use for topical use to limit/prevent resistance since it is a potent broadspectrum antibacterial drug
Avoid topical use as much as possible unlike in neomycin which can be used topically
TOPICAL ANTIBIOTIC IN ACNE
Effectiveness of topical formulation is less than systemic.
Page 8 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
For mild to moderate cases only.
Systemic antibiotics to be used for severe cases
Blast from the past: A plant called earrings (plant with violet flowers) was said to
be effective against acne. Not studied yet.
A. CLINDAMYCIN
Very effective drug
Approximately 10% absorbed. May cause rare cases of bloody diarrhea &
pseudomembranous colitis when absorbed systemically
Known commercially as (Dalacin C) which is mixed in products such as Eskinol
Increased chance of systemic absorption and associated side effects with the use of
Eskinol daily
Water based gel vehicle well-tolerated
Not a good practice to use it left and right.
B.
C.
ERYTHROMYCIN
Used systemically; broad-spectrum antibiotic
Avoid topical use as much as possible
Inhibitory effect on P. Acnes
Complication: Development of Resistant strains of Staph
o Correlated with the use of the topical form
o If this occurs, topical form should be discontinued and systemic therapy started
Side Effects: Burning, drying, irritation
Prescribed in patients allergic to penicillin. Reserved for special cases
METRONIDAZOLE
Topical Gel effective in acne rosacea
Drug of choice (DOC) for Amoebiasis
MOA: UNKNOWN but may relate to the inhibitory effects on Demodex brevis (face
mite)
Oral form is carcinogenic in rats
o Main reason why we avoid giving topical use in pregnant women
Side Effect :Drying, Burning, Stinging
Caution when applying near eye
Not allowed for pregnant women
D.
TETRACYCLINE
Tetracyline HCl in a hydroalcoholic base containing N-Decyl Methyl Sulfoxide
Meclocycline sulfosalicylate in a cream base
No demonstrable absorption when applied twice daily
Inhibitory action on P. Acnes
Side effect: Staining of teeth and bones
No longer recommended today, just mentioned in the discussion for historys sake
Used to be a popular drug for acne
Page 9 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
According to Katzung, it is no longer mentioned for treating acne but other books say
otherwise. Dr. Abello also states that it is still effective
E. SODIUM SULFACETAMIDE
Available as a 10% lotion (Klaron) & as 10% wash (Ovace) combined with sulfur in the
treatment of acne vulgaris & acne rosacea
MOA: Inhibition of P. Acnes by competitive inhibition of PABA utilization
Approximately 4% is absorbed percutaneously
Contraindicated in patients sensitive to sulfonamides
ACNE PREPARATIONS
Very popular nowadays
A.
RETINOIC ACID
Topically applied
Remains in the epidermis with less than 10% systemic absorption
Action in acne is attributed to decreased cohesion between epidermal cells and
increased epidermal cell turnover
Results in expulsion of open comedones
Efficacious
B.
ISOTRETINOIN
For severe cystic acne
Recalcitrant to standard therapy
MOA: inhibit sebaceous gland size & function
Adverse effects: Similar to hypervitaminosis A
o Highly teratogenic
o Should not administer in pregnant women
o Stopped 6 months before pregnancy
C.
ETRETINATE
Still a Vitamin A/retinoid
Treatment of psoriasis especially pustular forms
Given orally 1-5mg/kg/day starting with 0.5mg
Adverse effects: Similar to hypervitaminosis A
o Should not be taken by women of childbearing age
o More teratogenic than other vitamin A preparations
ANTIPRURITIC AGENTS
For itchiness, we administer anesthetics or antihistaminics
Avoid antihistaminics locally because we expose the individual to development of
sensitization
A. DOXEPIN
MOA: H1 & H2 antagonists property percutaneous absorption
Page 10 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
B.
Can cause drowsiness like other antihistamines
Contraindications: Narrow angle glaucoma
Tend to cause urinary retention because of anticholinergic effects
Drug must be discontinued 2 weeks prior to use when patient uses Monoamine
oxidase inhibitor (MAOi)
o Doxepin enhances action of MAOi
PRAMOXINE
Topical anesthetic available as 1% Cream, Lotion, Gel
Applied 2-4x a day
Adverse effect: transient burning and stinging
ANTIHISTAMINES
A. OLDER H1 RECEPTOR ANTAGONISTS
1st generation antihistaminics
Have some Anticholinergic activity
Are sedating because they can cross the blood-brain barrier.
Advise patients taking antihistamines to avoid driving or operating machineries as
these drugs could cause sedation and drowsiness.
B. NEWER H1 RECEPTOR ANTAGONISTS
Have lesser side-effects because they do not cross the blood brain barrier
Generally do not cause drowsiness/sedation
Examples:
a.
Terfenadine
b.
Astemizole
c.
Loratadine
C. H2 RECEPTOR BLOCKERS
Better used for patients with peptic ulcer
o Decreases gastric acid secretion
o Examples
i. Cimetidine
enzyme inhibitor
Problem: inhibits cytochrome P450 which inhibits drug metabolizing
enzyme causing increased effect sensitive to these enzymes
ii. Ranitidine
iii. Famotidine
iv. Nizatidine
AGENTS AFFECTING PIGMENTATION
A. HYDROQUINONE & MONOBENZONE
Appears to involve inhibition of the enzyme tyrosinase thus interfering with the
synthesis of melanin
o E.g. Michael Jackson (MJ) who had irreversible depigmentation leading to VITILIGO
Do patch test prior to administration
o For local irritation/ allergic sensitization
Page 11 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
HYDROQUINONE
Causes temporary lightening
Found in lightening agents
MONOBENZONE
(Most likely what MJ used)
Causes irreversible depigmentation
TRIOXSALEN & METHOXSALEN
o Psoralens used for repigmentation of
depigmented molecules of vitiligo
o Intercalate with DNA inhibit DNA synthesis
o Major Risks:
- Cataracts
- Skin Cancer
B. GLUTATHIONE
not among the whitening agents listed in
pharmacologic books, just included because of
its increasing popularity
Principal intracellular non-protein thiol
Plays major role in maintenance of intracellular
redox state
very important and useful
C. POLYPHENOLIC-GLUTATHIONE (GSH)
Reduced glutathione
Conjugates and their metabolites retain the
electrophilic and redox properties of the parent
polyphenol
The reactivity of thioether metabolites exceed
that of the parent polyphenol
Contribute to the Nephrotoxicity,
Nephrocarcinogenicity& Neurotoxicity of a
variety of polyphenols
Side effects:
o Allergic reactions
o Zinc deficiency after long periods of use
o Skin whitening observed when taken in
high doses
- Made possible as antioxidant that aids
in cell regeneration & counteracts free
radicals
SUNSCREENS
Topical agents useful in protecting against sunlight
Page 12 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
A.
PABA (Para-AminoBenzoic Acid) & its
esters (Benzophenones, Dibenzoyl
Methanes)
Absorb UV light in UV B wavelength 280
320 nm (range for erythema & tan)
B.
SPF (Sun Protection Factor)
For light skin: SPF 15 or more
For dark skin: SPF 10-15
KERATOLYTIC AGENTS
A.
SALICYCLIC ACID
Solubilize cell-surface proteins that
keep the stratum corneum intact, resulting in
desquamation of keratotic disorders
Keratolytic in concentrations of 3-6%
Used in the treatment of warts
Care should be practiced when used
in patients with diabetes
mantica de papel
o Indication: warts removal
o MOA: Contains salicylic acid which
burns warts
Page 13 of 14
Block X |PHARMACOLOGY | Lesson 1
Dermatologic Pharmacology
REFERENCES:
Katzung, BG, Masters, SB and AJ Trevor. 2012. Basic and Clinical Pharmacology. 12th
Edition. USA:McGraw-Hill, Chapter 61, p 1061-1079.
Excelsior. 2014. Dermatologic Pharmacology Handouts.
Abello, ML. 2015. Dermatologic Pharmacology Lecture. September 18, 2015.
Page 14 of 14
You might also like
- Pedia TicklerDocument66 pagesPedia TicklerCharles Jebb Belonio JuanitasNo ratings yet
- Pediatrics Preceptorial JuanitasMDDocument5 pagesPediatrics Preceptorial JuanitasMDCharles Jebb Belonio JuanitasNo ratings yet
- Juanitas Photjournalism 2020 Philarts.Document3 pagesJuanitas Photjournalism 2020 Philarts.Charles Jebb Belonio JuanitasNo ratings yet
- Pedia TicklerDocument66 pagesPedia TicklerCharles Jebb Belonio JuanitasNo ratings yet
- EductionDocument45 pagesEductionCharles Jebb Belonio JuanitasNo ratings yet
- B20M05L05 - Ocular and Orbital TumorsDocument17 pagesB20M05L05 - Ocular and Orbital TumorsCharles Jebb Belonio JuanitasNo ratings yet
- Stanford - Trauma - Guidelines June 2016 Draft Adult and Peds FINALDocument166 pagesStanford - Trauma - Guidelines June 2016 Draft Adult and Peds FINALHaidir Muhammad100% (1)
- April Medical TipsheetsDocument5 pagesApril Medical TipsheetsCharles Jebb Belonio JuanitasNo ratings yet
- PGI Protocols 2018Document3 pagesPGI Protocols 2018Charles Jebb Belonio JuanitasNo ratings yet
- Charles Jebb Belonio Juanitas reaction paper on becoming a doctorDocument1 pageCharles Jebb Belonio Juanitas reaction paper on becoming a doctorCharles Jebb Belonio JuanitasNo ratings yet
- B18M03L01 - Chronic Myeloproliferative Diseases, Polycythemia Vera, ThrombocytosisDocument22 pagesB18M03L01 - Chronic Myeloproliferative Diseases, Polycythemia Vera, ThrombocytosisCharles Jebb Belonio JuanitasNo ratings yet
- Iloilo to Manila flight itineraryDocument4 pagesIloilo to Manila flight itineraryCharles Jebb Belonio JuanitasNo ratings yet
- Health Record STA BARBARA FinalDocument6 pagesHealth Record STA BARBARA FinalCharles Jebb Belonio JuanitasNo ratings yet
- The Inflammatory Process: Phospholipase ADocument1 pageThe Inflammatory Process: Phospholipase ACharles Jebb Belonio JuanitasNo ratings yet
- B10Ph01 - Dermatologic PharmacologyDocument14 pagesB10Ph01 - Dermatologic PharmacologyCharles Jebb Belonio JuanitasNo ratings yet
- B11R01 - Descriptive StatisticsDocument10 pagesB11R01 - Descriptive StatisticsCharles Jebb Belonio JuanitasNo ratings yet
- Blood Cell Morphology TutorialDocument176 pagesBlood Cell Morphology TutorialCharles Jebb Belonio JuanitasNo ratings yet
- Pandac NewDocument1 pagePandac NewCharles Jebb Belonio JuanitasNo ratings yet
- The Integumentary SystemDocument6 pagesThe Integumentary SystemCharles Jebb Belonio JuanitasNo ratings yet
- Blood Cell Morphology TutorialDocument176 pagesBlood Cell Morphology TutorialCharles Jebb Belonio JuanitasNo ratings yet
- What Are HallucinogensDocument4 pagesWhat Are HallucinogensCharles Jebb Belonio JuanitasNo ratings yet
- Bill of RightsDocument79 pagesBill of RightsCharles Jebb Belonio JuanitasNo ratings yet
- B03M02L4 Protein Chemistry 1Document8 pagesB03M02L4 Protein Chemistry 1Charles Jebb Belonio JuanitasNo ratings yet
- WVSU College of Nursing Care Plan TemplateDocument2 pagesWVSU College of Nursing Care Plan TemplateCharles Jebb Belonio JuanitasNo ratings yet
- Complicated UTI 9930dftDocument33 pagesComplicated UTI 9930dftRan GarciaNo ratings yet
- West Visayas State University: Student Nurses Association of The PhilippineDocument1 pageWest Visayas State University: Student Nurses Association of The PhilippineCharles Jebb Belonio JuanitasNo ratings yet
- The OdysseyDocument5 pagesThe OdysseyCharles Jebb Belonio JuanitasNo ratings yet
- DMsnapDocument11 pagesDMsnapCharles Jebb Belonio JuanitasNo ratings yet
- Jathroper Charcoal As Alternative Heat Source. Clyde2Document29 pagesJathroper Charcoal As Alternative Heat Source. Clyde2Charles Jebb Belonio JuanitasNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- ArcelorMittal Projects Steel Pipe ProductionDocument20 pagesArcelorMittal Projects Steel Pipe Productionanil-kumar-singh-6674No ratings yet
- Jyothy Institute of TechnologyDocument4 pagesJyothy Institute of TechnologyBasavaraj hsNo ratings yet
- 2 Basic Clinical Genetic - ppt-1Document24 pages2 Basic Clinical Genetic - ppt-1Najib M. NauvalNo ratings yet
- Instruction and Technical Manual for CentrifugesDocument56 pagesInstruction and Technical Manual for CentrifugesDiana RaieNo ratings yet
- II - ITP - Defect Work FabricationDocument5 pagesII - ITP - Defect Work Fabricationmohd as shahiddin jafriNo ratings yet
- Waterproofing: Hydrostop 4 Py-SDocument2 pagesWaterproofing: Hydrostop 4 Py-SPrashantBaruaNo ratings yet
- SIP MeenakshDocument17 pagesSIP MeenakshRati GuptaNo ratings yet
- Mineral NutritionDocument23 pagesMineral NutritionRahul KumarNo ratings yet
- Synthesis and Discriminative Stimulus Properties of N(6)-Alkyl Norlysergic Acid DerivativesDocument4 pagesSynthesis and Discriminative Stimulus Properties of N(6)-Alkyl Norlysergic Acid Derivativesmik100% (1)
- Alpha ProfileDocument2 pagesAlpha ProfileGovind SinghNo ratings yet
- Ips e PR 850 PDFDocument73 pagesIps e PR 850 PDFdeyanshu7No ratings yet
- As 2278.1-2008 Aerosol Containers Metal Aerosol Dispensers of Capacity 50 ML To 1000 ML InclusiveDocument7 pagesAs 2278.1-2008 Aerosol Containers Metal Aerosol Dispensers of Capacity 50 ML To 1000 ML InclusiveSAI Global - APAC50% (2)
- Final - Report Hydroelectric Power PlantDocument39 pagesFinal - Report Hydroelectric Power PlantnisarNo ratings yet
- Method Statement FOR Waste Polymer Slurry Disposal: PT Bauer Pratama IndonesiaDocument4 pagesMethod Statement FOR Waste Polymer Slurry Disposal: PT Bauer Pratama IndonesiaFendi Rang TigorNo ratings yet
- Urea MsdsDocument5 pagesUrea MsdsVinnyVidichiNo ratings yet
- Zuellig Pharma Corporation: Item Name of Medicine Brand Name Principal Name Quantity Unit PriceDocument2 pagesZuellig Pharma Corporation: Item Name of Medicine Brand Name Principal Name Quantity Unit PriceJZik SibalNo ratings yet
- Report GCWDocument34 pagesReport GCWArchit HaldiaNo ratings yet
- Food Chemistry: Miaomiao Shi, Zhiheng Zhang, Shujuan Yu, Kai Wang, Robert G. Gilbert, Qunyu GaoDocument7 pagesFood Chemistry: Miaomiao Shi, Zhiheng Zhang, Shujuan Yu, Kai Wang, Robert G. Gilbert, Qunyu GaoSNo ratings yet
- Kluebersynth GEM 4 N GB enDocument6 pagesKluebersynth GEM 4 N GB enIvan MarijanovićNo ratings yet
- 2593Document9 pages2593Zaid AhmadNo ratings yet
- Expwb3ans eDocument67 pagesExpwb3ans eOlivia LinNo ratings yet
- Johnson Industrial Screens PDFDocument20 pagesJohnson Industrial Screens PDFjaime palenzuela rodriguezNo ratings yet
- PVC FlamethrowerDocument21 pagesPVC FlamethrowerMike Nichlos100% (4)
- ANSWER A. Diesel Cycle Has Lower Efficiency Than Otto CycleDocument12 pagesANSWER A. Diesel Cycle Has Lower Efficiency Than Otto CycleParmeshwarPaulNo ratings yet
- Atracurium BesylateDocument4 pagesAtracurium BesylateStill DollNo ratings yet
- Analytical Techniques for Evaluating Quality of Herbal DrugsDocument7 pagesAnalytical Techniques for Evaluating Quality of Herbal DrugsZaidNo ratings yet
- TDS - Mastertop 1330Document2 pagesTDS - Mastertop 1330Venkata RaoNo ratings yet
- Astm D 2863Document13 pagesAstm D 2863Ma PonyNo ratings yet
- Dust Collection Design and Maintenance GuideDocument36 pagesDust Collection Design and Maintenance GuideMadan YadavNo ratings yet
- MN 206 Market Survey CopperDocument210 pagesMN 206 Market Survey CopperArjun MishraNo ratings yet