Professional Documents
Culture Documents
CHF Pathophys Paper
Uploaded by
Sarah SCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CHF Pathophys Paper
Uploaded by
Sarah SCopyright:
Available Formats
Running head: CONGESTIVE HEART FAILURE
Congestive Heart Failure
S. Schneider
**** **** College
Running head: CONGESTIVE HEART FAILURE
Congestive Heart Failure
Definition
Congestive heart failure (CHF), formerly referring to just left sided heart failure, is a common,
yet complex, clinical disorder that can result from any functional or structural cardiac disorder that
impairs the ventricles ability to fill with or eject blood.(Figueroa, M. and Peters, J., 2006, pg. 402).
Congestive heart failure may be acute or chronic and ranges from mild to severe in nature. There are
two sub-types: systolic and diastolic. Systolic heart failure results when the heart has insufficient
strength to contract forcefully enough to eject adequate amounts of blood into the circulation. Diastolic
heart failure occurs when the left ventricle cannot relax adequately during diastole (relaxation phase)
which prevents the ventricle from filling with sufficient blood to ensure normal cardiac output and
tissue perfusion.(Ignatavicius, D., and Workman, L., 2013, pg. 715). Within this paper we will be
focusing in systolic heart failure.
Risk factors
There are major unmodifiable and modifiable risk factors to congestive heart failure. The major
unmodifiable risk factors include age (over 65), family history, congenital heart defects, valvular heart
disease, past myocardial infarction (heart attack), irregular heart rhythms, and coronary artery disease.
(Mayo Clinic Staff, 2015). The major modifiable risk factors include sedentary lifestyle, obesity,
uncontrolled diabetes mellitus, uncontrolled hypertension, poor diet and nutrition, alcohol use, and
tobacco use (smoking, chewing, etc.) (American Heart Association (AHA), 2015).
Pathophysiology
Congestive heart failure (CHF) is both an acute and chronic disorder that develops when the heart is
unable to maintain adequate ejection of blood and perfusion of organs. Cardiac dysfunction causes a
drop in cardiac output which leads to the activation of several neurohormonal pathways. (Gorbunova,
S., n.d.). As noted by Hobbs, R., & Boyle, A. (2014, March 1), in systolic dysfunction the body
Running head: CONGESTIVE HEART FAILURE
activates the sympathetic nervous system (through neurohormonal tracts) that increases heart rate and
strength of contractions, which results in vasoconstriction that stimulates secretion of renin from the
juxtaglomerular apparatus of the kidney due to loss of perfusion. Stimulation of the renin-angiotensin
system as a result of increased sympathetic stimulation and decreased renal perfusion results in further
vasoconstriction, sodium and water retention, and release of aldosterone. An increased aldosterone
level, in turn, leads to sodium and water retention, and other complications. Preload and afterload
increase as sodium and water are retained. Angiotensin II furnishes ventricular changes resulting in
advancing myocyte contractile dysfunction. Natriuretic peptides are neurohormones that work to boost
vasodilation and diuresis through sodium excretion in the kidney tubules. Brain naturietic peptide
(BNP) is produced and excreted by the ventricles when the client has fluid volume excess from CHF.
(Ignatavicus, D. & Workman, L., 2013). Another compensatory mechanism is the enlargement of the
cardiac muscle, with or without the increase in ventricular size. These walls thicken to increase the
force of contractions but may hypertrophy faster than collateral circulation can supply adequate blood
supply. (Ignatavicius, D., & Workman, L., 2013).
Complications
The complications of CHF arise from the decrease in tissue perfusion. This decrease in
perfusion leads to serious tissue damage and in turn congestion of the circulatory system. Such
complications that can arise are: kidney damage/failure, heart valve problems, and liver damage. The
kidney damage and/or failure arises from the decrease in blood flow which may require dialysis for
treatment. Heart valve problems arise from the damage sustained from high pressure or from the
enlargement of the heart muscle. Liver damage is done via the fluid backup which leads to scarring of
the liver making it hard for the liver to function properly. (Mayo Clinic, 2015 August 18).
Running head: CONGESTIVE HEART FAILURE
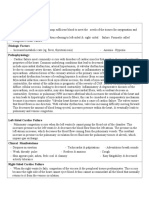
Table 1
Client to Textbook Comparison
Textbook
Client
Clinical Manifestations
1. Cough
2. Breathlessness
3. Weakness
4. Dizziness
5. Acites
6. Peripheral Edema
7. JVD
8. Cardiomegaly
9. Decreased Mentation
10. Decreased SpO2
11. Reduced Kidney Function
12. Chest Pain
13. Weight Gain
1. None upon assessment
2. Exertional related to pain from
RLE infection
3. Present, unable to hold self
over while turning in bed.
Weak to moderated grips and
plantar/dorsifelxion.
4. None noted upon assessment
5. None noted upon assessment
Abdominal obesity.
6. +2-3 pitting edema on
bilateral lower extremities,
and +1 on bilateral upper
extremities.
7. None upon assessment or
admission
8. None noted upon admission
9. Some
forgetfulness/disorientation at
times. Re-orientated easily.
Noted that opioid pain
medications have caused this
in the past.
10. Upon admission O2 Sat was
in high 90s but currently in
low 90s.
11. GFR 66/57
12. None upon assessment or
admission
13. Upon admission had gained
2-4 lbs; diuresing with Lasix.
Current weight 80.28 kg.
Diagnostic Labs, Tests,
Procedures
1. History and Physical
1. Past smoker history for 30
2. Urinalysis
years (quit in 2006), HTN,
3. Troponin
COPD, cataracts (surgeries in
4. BNP
08 and 13) worked as a sales
5. Serum Electrolytes
manager at a department store
6. Arterial Blood Gases
and homemaker.
7. Hemoglobin and Hematocrit 2. Clear, straw colored, voided
8. BUN and Creatinine & Protein 25 mL, Sp. Gravity 1.004
9. Chest X-Ray
(low), pH 5.0 - 9/14/15.
10. Echocardiogram
3. <0.04 - 9/15/15
Running head: CONGESTIVE HEART FAILURE
H&P
Medical Management
11. EKG
12. MUGA
4. 216 9/14/15
5. K+ = 3.8, Na+ = 137,
CO2 = 26
6. Not ordered
7. HgB: 10.3, Hct: 31.2
9/15/15
8. Protein: 3.9 6/5/15, BUN
and Creatinine not ordered
9. Cardiac silhouette and
pulmonary vasculature show
mildly prominent congestion,
increased opacity in bases
5/19/15
10. Not ordered
11. Normal Sinus 9/14/15
12. Not ordered
1. Past Medical History
2. Home Meds
3. Vitals and Pain
4. Respiratory Status
5. Family Hx.
1. Hx. COPD, essential
hypertension, cataracts
(surgeries in 08 and 13),
obesity, hyperlipidemia,
anemia and depression.
2. ASA 81 mg qd, Celexa 20 mg
qd, ferrous sulfate 325 mg (65
mg Fe) qd, Hydralazine 50 mg
bid, Imdur 30 mg qd, Cozaar
50 mg qd, Multivitamin qd,
Simvastatin 20 mg qPM,
Spiriva inhal 18 mcg qd,
Vitamin B-12 500 mcg qd.
3. Bp: 149/48 (0755 9/15/15)
150/49 (1200 9/15/15); Temp:
98.2 (0755 9/15/15) 98.1
(1200 9/15/15); Pulse: 78
(0755 9/15/15) 74 (1200
9/15/15); SpO2: 93% RA
(0755 9/15/15) 94% RA
(1200 9/15/15); Pain: 0 (0755
9/15/15) 10/10 (1200
9/15/15).
4. Room air, unlabored
breathing, equal chest
expansion, lungs CTA.
5. Not on file
1. Drug Therapy
a. Beta-Blockers
1. Meds
a. Not ordered
Running head: CONGESTIVE HEART FAILURE
b. ACE-inhibitors
c. Angiotensin Receptor
Blockers
d. Hydralazine and Nitrates
e. Aldosterone agonists
f. Diuretics
g. Digoxin
h. Heparin
2. CPAP
3. Cardiac Resynchronization
Therapy
4. Investigative Gene Therapy
5. Oxygen Therapy
6. Diet Therapy
7. Fluid Restriction
8. Strict I&O
b. Not ordered
c. Cozaar 50 mg qd
d. Hydralazine 50 mg bid,
Imdur 30 mg qd.
e. Not ordered
f. Lasix 40 mg qd
g. Not ordered
h. Heparin 5,000 units q 8hr
for DVT prevention
2. Not indicated for pt.
3. Not indicated for pt.
4. Not indicated for pt.
5. Room air
6. Cardiac, Low Na diet.
7. Not ordered
8. Not ordered
Surgical Management
1. Heart Transplant
2. Ventricular Assist Devices
3. Partial Left Ventriculectomy
4. Endoventricular Patch
5. Acorn Cardiac Support Device
6. Myosplint
1. Not indicated for pt.
2. Not indicated for pt.
3. Not indicated for pt.
4. Not indicated for pt.
5. Not indicated for pt.
6. Not indicated for pt.
Nursing Management
1. Administer Meds as Ordered
2. Health Teaching and
Promotion
3. Assess Patient for Clinical
Manifestations
4. Monitor Vital Signs
5. Monitoring I&O and Weight
6. Monitoring Lab Studies
7. Maintaining HOB Elevation
1. RN assigned to patient
administered medications as
ordered.
2. Taught client: how to use the
incentive spirometer and to
breathe in deeply and slowly
to increase the amount of
oxygen the body receives,
choosing healthy choices for
food, and importance of doing
some physical activity (even if
it is just ROM exercises).
3. Completed physical
assessment on patient and
noted no other signs of
congestive heart failure (CHF)
except for edema, and some
weakness.
4. Monitored vital signs in the
morning and afternoon.
5. Charted when patient voided
urine. Check chart for updated
weight.
Running head: CONGESTIVE HEART FAILURE
6. Looked up lab studies for
patient. 0500 labs were
resulted, however no
additional labs were
ordered/resulted.
7. Maintained HOB at 30-45
degrees unless patient was
eating then at 90 degrees and
when placing patient on
bedpan and taking patient off
bedpan lowered head of bed.
(Winkelman, C., 2013, pp. 351-355) (Ignatavicius, D., & Workman, L., 2013, pp. 751-754)
Contributing Factors Relating to the Pathology
This is a 85 year old female that also suffers from COPD, anemia, obesity, hyperlipidemia,
essential hypertension and depression. She is currently 28.6 pounds overweight for her age and height.
While at the hospital she does not have much of an appetite. She does not exercise regularly due to age,
weakness, COPD, and going to cancer appointments with her husband. She complains of right lower
extremity pain. She is also a past pack a day smoker for 30 years and quit in 2006. Upon review of this
patient's health history, the contributing factors leading to her development of CHF include obesity,
hyperlipidemia, COPD, hypertension, sedentary lifestyle, age, and previous smoking history.
Running head: CONGESTIVE HEART FAILURE
References
American Heart Association (AHA). (2015, July 29). Causes and Risks for Heart Failure. Retrieved
September 20, 2015, from
http://www.heart.org/HEARTORG/Conditions/HeartFailure/UnderstandYourRiskforHeart
Failure/Causes-and-Risks-for-Heart-Failure_UCM_002046_Article.jsp
Hobbs, R., & Boyle, A. (2014, March 1). Heart Failure. Retrieved September 20, 2015, from
http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/heartfailure/Default.htm
Figueroa, M., & Peters, J. (2006). Congestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and
Implications for Respiratory Care. Respiratory Care, 51(4), 402-412. Retrieved September 14,
2015, from http://www.rcjournal.com/contents/04.06/04.06.0403.pdf
Gorbunova, S. (n.d.). What is Heart Failure? Retrieved September 18, 2015, from
http://www.queri.research.va.gov/chf/products/nurse_education/What-is-Heart-Failure.pdf
Ignatavicius, D., & Workman, L. (2013). Medical-surgical nursing: Patient-centered collaborative
care (7th ed., pp. 747-758). St. Louis, MO: Saunders/Elsevier.
Mayo Clinic. (2015, August 18). Heart failure (R. Mankad, Ed.). Retrieved September 19, 2015, from
http://www.mayoclinic.org/diseases-conditions/heart-failure/basics/complications/con20029801
Mayo Clinic. (2015, August 18). Heart failure (R. Mankad, Ed.). Retrieved September 16, 2015, from
http://www.mayoclinic.org/diseases-conditions/heart-failure/basics/risk-factors/con-20029801
Winkelman, C. (2013). Clinical companion, Ignatavicius Workman, Medical-surgical nursing: Patientcentered collaborative care. (7th ed., pp. 349-355). St. Louis, MO: Elsevier Saunders.
You might also like
- Chronic Heart FailureDocument11 pagesChronic Heart FailurelaydyNo ratings yet
- Heart Failure in ChildrenDocument47 pagesHeart Failure in ChildrenDr.P.NatarajanNo ratings yet
- NCM 106 Acute Biologic CrisisDocument142 pagesNCM 106 Acute Biologic CrisisEllamae Chua88% (8)
- Pharmacology II Sovan Sarkar 186012111012Document14 pagesPharmacology II Sovan Sarkar 186012111012Sovan SarkarNo ratings yet
- Understanding Major Chronic Illnesses of Older AdultsDocument21 pagesUnderstanding Major Chronic Illnesses of Older AdultsSteffiNo ratings yet
- Heart Failure IntroductionDocument12 pagesHeart Failure IntroductionJasper VictoryNo ratings yet
- Lec 3 Heart FailureDocument25 pagesLec 3 Heart FailureDelete AccountNo ratings yet
- PEMICU 4 KV CynthiaDocument55 pagesPEMICU 4 KV CynthiaEko SiswantoNo ratings yet
- Tugass Paper BryanDocument10 pagesTugass Paper BryanMauritius BryanNo ratings yet
- CHFDocument61 pagesCHFAngeline Lareza-Reyna VillasorNo ratings yet
- Cardiac FailureDocument63 pagesCardiac FailureNina OaipNo ratings yet
- NURSING CARE PLAN for 8yo Male with CHDDocument5 pagesNURSING CARE PLAN for 8yo Male with CHDDonna Co IgNo ratings yet
- Cardiac Case Study on Coronary Artery Disease RiskDocument4 pagesCardiac Case Study on Coronary Artery Disease RiskElizabeth SpokoinyNo ratings yet
- Gerontic Nursing: Elderly With Hypertension: Arranged Group 11: Suci Aulia (1714201042)Document15 pagesGerontic Nursing: Elderly With Hypertension: Arranged Group 11: Suci Aulia (1714201042)anisaNo ratings yet
- Case Study 8 9 10 11Document12 pagesCase Study 8 9 10 11jovan teopizNo ratings yet
- Heart Failure (Recovered)Document43 pagesHeart Failure (Recovered)Binal Joshi100% (1)
- EndocarditisDocument6 pagesEndocarditisMerry Joy DeliñaNo ratings yet
- PBL 3 FixDocument37 pagesPBL 3 FixYusril DjibranNo ratings yet
- Heart FailureDocument8 pagesHeart FailureSophia MarieNo ratings yet
- Cardiomyopathy Self StudyDocument3 pagesCardiomyopathy Self StudySolomon Seth SallforsNo ratings yet
- Nutrition Case StudyDocument17 pagesNutrition Case Studymacedon14100% (18)
- CHF PBLDocument3 pagesCHF PBLqtiefyNo ratings yet
- Congestive Heart Failure (CHF) : BY Miss. S. D. Ajetrao Assistant Professor ADCDP, AshtaDocument16 pagesCongestive Heart Failure (CHF) : BY Miss. S. D. Ajetrao Assistant Professor ADCDP, AshtaChandraprakash JadhavNo ratings yet
- Nursing Care Process Case StudyDocument6 pagesNursing Care Process Case StudyEunice RosalesNo ratings yet
- Observation Report - Hemodialysis - Kit P. RoaquinDocument15 pagesObservation Report - Hemodialysis - Kit P. Roaquineljhayar_18No ratings yet
- Congestive Heart FailureDocument17 pagesCongestive Heart FailureLyana StarkNo ratings yet
- Nursing Study GuideDocument21 pagesNursing Study GuideYanahNo ratings yet
- Deborah Mukendenge Mujinga Nurs201Document6 pagesDeborah Mukendenge Mujinga Nurs201Lois MpangaNo ratings yet
- High output heart failure: a reviewDocument7 pagesHigh output heart failure: a reviewChanvira Aria CandrayanaNo ratings yet
- MR Kumar Case Study: Student Name Department, University Course Name Professor NameDocument7 pagesMR Kumar Case Study: Student Name Department, University Course Name Professor NameVincent Karimi GichimuNo ratings yet
- Literature Review On Congestive Heart FailureDocument4 pagesLiterature Review On Congestive Heart Failurefihynakalej2100% (1)
- Kel 7Document13 pagesKel 7hananNo ratings yet
- Tgs Bhs InggrisDocument22 pagesTgs Bhs InggrisHarda DedaliNo ratings yet
- Latar BelakangDocument25 pagesLatar BelakangririnagustinNo ratings yet
- Clinical Symptoms Due To Fluid CongestionDocument5 pagesClinical Symptoms Due To Fluid CongestionBrandedlovers OnlineshopNo ratings yet
- Cardiogenic Shock NDDocument8 pagesCardiogenic Shock NDLizbet CLNo ratings yet
- Hypertension: Pathophysiology, Diagnostic Test, Medical Management, and Nursing Care PlanDocument12 pagesHypertension: Pathophysiology, Diagnostic Test, Medical Management, and Nursing Care PlanMaulidyaFadilahNo ratings yet
- Medical Nutrition Therapy A Case Study Approach 5th Edition Nelms Solutions ManualDocument8 pagesMedical Nutrition Therapy A Case Study Approach 5th Edition Nelms Solutions Manualsophiechaurfqnz100% (31)
- Medical Nutrition Therapy A Case Study Approach 5Th Edition Nelms Solutions Manual Full Chapter PDFDocument29 pagesMedical Nutrition Therapy A Case Study Approach 5Th Edition Nelms Solutions Manual Full Chapter PDFStephanieMckayeqwr100% (7)
- Reflective Journaling 1Document12 pagesReflective Journaling 1Nosheen ShahNo ratings yet
- Heart Failure: Causes, Symptoms, and TreatmentDocument36 pagesHeart Failure: Causes, Symptoms, and TreatmentnathanNo ratings yet
- Fluid and Electrolytes for Nursing StudentsFrom EverandFluid and Electrolytes for Nursing StudentsRating: 5 out of 5 stars5/5 (12)
- Heart Failure: Definition and EpidemiologyDocument6 pagesHeart Failure: Definition and EpidemiologyIshwarya SivakumarNo ratings yet
- Case Study For Chronic Renal FailureDocument6 pagesCase Study For Chronic Renal FailureGabbii CincoNo ratings yet
- Heart Failure: Causes, Signs, TestsDocument6 pagesHeart Failure: Causes, Signs, Testsصفا رياض محمد /مسائيNo ratings yet
- Congestive Heart FailureDocument39 pagesCongestive Heart FailureEthiopia TekdemNo ratings yet
- Cardiac Failure & Myocardial Infarction GuideDocument6 pagesCardiac Failure & Myocardial Infarction GuideDaniel GeduquioNo ratings yet
- Angina Pectoris: Chest Pain Causes and TreatmentsDocument7 pagesAngina Pectoris: Chest Pain Causes and TreatmentsTruptilata SahooNo ratings yet
- Congestive Heart Failure: EtiologyDocument3 pagesCongestive Heart Failure: EtiologyJoshua VillarbaNo ratings yet
- Managing A Patient With Es RD 23Document3 pagesManaging A Patient With Es RD 23Undefined RegisterNo ratings yet
- EPP SEMESTER 6 Baru BNGTDocument8 pagesEPP SEMESTER 6 Baru BNGTLisa FitrianiNo ratings yet
- Understanding Hypertension: A Report on Causes, Symptoms and TreatmentDocument11 pagesUnderstanding Hypertension: A Report on Causes, Symptoms and TreatmentanggaraNo ratings yet
- Final Research PaperDocument8 pagesFinal Research Paperapi-301053941No ratings yet
- Congestive Heart FailureDocument14 pagesCongestive Heart FailureBella Trix PagdangananNo ratings yet
- Chapter 33 HypertensionDocument5 pagesChapter 33 HypertensiongytmbiuiNo ratings yet
- Case Analysis: Medical Surgical NursingDocument7 pagesCase Analysis: Medical Surgical NursingMaria ThereseNo ratings yet
- CHF Case OutputDocument3 pagesCHF Case OutputJethro Floyd QuintoNo ratings yet
- Assignment 3Document5 pagesAssignment 3api-577583685No ratings yet
- Nurs220 F and e Case Study Gfranklin220 Doc-2Document9 pagesNurs220 F and e Case Study Gfranklin220 Doc-2api-355433171No ratings yet
- Report About HypertensionDocument11 pagesReport About HypertensionZA IDNo ratings yet
- Sensory EOs Part 2Document12 pagesSensory EOs Part 2Sarah SNo ratings yet
- GP PresentationDocument11 pagesGP PresentationSarah SNo ratings yet
- NSG 222 Test 3 Part One EODocument7 pagesNSG 222 Test 3 Part One EOSarah SNo ratings yet
- N126 Student WorksheetDocument2 pagesN126 Student WorksheetSarah SNo ratings yet
- Pharmacology Alphabet AllDocument4 pagesPharmacology Alphabet Allsflower85No ratings yet
- Study Guide For DiasterDocument7 pagesStudy Guide For DiasterSarah SNo ratings yet
- Hints For Remembering Medication ClassificationsDocument2 pagesHints For Remembering Medication ClassificationsSarah SNo ratings yet
- Final Exam Review Sheet1 Mental Health NursingDocument30 pagesFinal Exam Review Sheet1 Mental Health NursingSarah S100% (5)
- Bumex Pharmacology Data SheetDocument1 pageBumex Pharmacology Data SheetSarah SNo ratings yet
- Clinical Organization Sheet for N126 PatientDocument1 pageClinical Organization Sheet for N126 PatientSarah S100% (1)
- Application of Theories NSG 221 Module 1.1Document20 pagesApplication of Theories NSG 221 Module 1.1Sarah SNo ratings yet
- IV Therapy ComplicationsDocument6 pagesIV Therapy ComplicationsSarah SNo ratings yet
- Cultural Presentation For Nursing SchoolDocument9 pagesCultural Presentation For Nursing SchoolSarah SNo ratings yet
- Fluid Balance NotesDocument4 pagesFluid Balance NotesSarah SNo ratings yet
- Fluid Balance Notes-1Document3 pagesFluid Balance Notes-1Sarah SNo ratings yet
- Fluid and Electrolytes PracticeDocument16 pagesFluid and Electrolytes PracticeSarah SNo ratings yet
- Fluid and Electrotlytes WorksheetDocument2 pagesFluid and Electrotlytes WorksheetSarah SNo ratings yet
- M7 Nutrition and HealthDocument2 pagesM7 Nutrition and HealthErykah Faith PerezNo ratings yet
- How and When To Be Your Own Doctor by Moser, IsabelDocument135 pagesHow and When To Be Your Own Doctor by Moser, IsabelGutenberg.org100% (2)
- Singapore Tops Global Average Peak Internet SpeedDocument7 pagesSingapore Tops Global Average Peak Internet Speedgusti annisaNo ratings yet
- Complications of Diabetes MellitusDocument147 pagesComplications of Diabetes MellitusNisrina SariNo ratings yet
- Nutritional TherapyDocument34 pagesNutritional TherapyArshi BatoolNo ratings yet
- Q & A (NCLEX) 2Document146 pagesQ & A (NCLEX) 2verzonicNo ratings yet
- Alpha Calc IdolDocument34 pagesAlpha Calc IdolSaroj Poudyal0% (1)
- Jelang Jelku D. SangmaDocument7 pagesJelang Jelku D. Sangmahaftamu GebreHiwotNo ratings yet
- Feed Enzymes Can Help Manage Price Volatility: FeedstuffsDocument3 pagesFeed Enzymes Can Help Manage Price Volatility: FeedstuffsAbtl EnzymesNo ratings yet
- Dietary Guidelines For IndiansDocument126 pagesDietary Guidelines For IndiansVivek PoojaryNo ratings yet
- SOP FinalDocument7 pagesSOP FinalsabaNo ratings yet
- Effect of Endurance Trainingg On Parameters of Aerobic FitnessDocument14 pagesEffect of Endurance Trainingg On Parameters of Aerobic FitnessClaudia LoughnaneNo ratings yet
- Luciano Passuello One Small Step Can Change Your Life FullDocument1 pageLuciano Passuello One Small Step Can Change Your Life FullSridhar ReddyNo ratings yet
- Pes Statements SamplesDocument19 pagesPes Statements SamplesJennie ManobanNo ratings yet
- Double Shaft Paddle MixerDocument4 pagesDouble Shaft Paddle MixerAntonio ReisNo ratings yet
- Super Immune System: Detoxification GuidelinesDocument6 pagesSuper Immune System: Detoxification GuidelinesRoxanaDucaNo ratings yet
- OCN Exam Flashcard Study System - OCN Test Practice Questions & Review For T-1Document1,255 pagesOCN Exam Flashcard Study System - OCN Test Practice Questions & Review For T-1NicoleNo ratings yet
- Ursolic Acid and Mechanisms of Actions On Adipose and Muscle Tissue A Systematic ReviewDocument12 pagesUrsolic Acid and Mechanisms of Actions On Adipose and Muscle Tissue A Systematic ReviewIgor BiggieNo ratings yet
- 5th Probiotics Prebiotics NewfoodDocument356 pages5th Probiotics Prebiotics NewfoodMichael HerreraNo ratings yet
- EMF SensitivityDocument25 pagesEMF SensitivitySundeeNo ratings yet
- HormonesBalance Superfoods Powerherbs Guides FINALDocument28 pagesHormonesBalance Superfoods Powerherbs Guides FINALAndrada Faur100% (1)
- Remaja - Skripsi. Universitas Sumatera Utara.: Daftar PustakaDocument5 pagesRemaja - Skripsi. Universitas Sumatera Utara.: Daftar PustakaimNo ratings yet
- Best 5-HTP Supplements of 2020: RatingDocument22 pagesBest 5-HTP Supplements of 2020: RatingTanjil TafsirNo ratings yet
- Faisal Coke 2Document85 pagesFaisal Coke 2Md FaisalNo ratings yet
- AnumwraDocument30 pagesAnumwratejasNo ratings yet
- Caring For Children 2: Babysitting BasicsDocument56 pagesCaring For Children 2: Babysitting BasicsmaureenlesNo ratings yet
- Omega-3 Benefits for All AgesDocument6 pagesOmega-3 Benefits for All Agescinefil70No ratings yet
- ResumeDocument2 pagesResumeapi-347141638No ratings yet
- Impact of Dietary Habits on Nutrition Status of StudentsDocument15 pagesImpact of Dietary Habits on Nutrition Status of StudentsEdcel BaragaNo ratings yet
- Open EPQ (7993) - Example A Star ProjectDocument58 pagesOpen EPQ (7993) - Example A Star Projectitssjustmariaxo4No ratings yet