Professional Documents
Culture Documents
SalivaryGlandsEsophagus
Uploaded by
Anonymous 4txA8N8etOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SalivaryGlandsEsophagus
Uploaded by
Anonymous 4txA8N8etCopyright:
Available Formats
SALIVARY GLANDS
Overview
o Produced by a collection of three major (parotid,
submandibular, lingual) and a number of minor (lingual,
buccal) glands
o Acinar-ductular glands
Acinar cells are classified as either serous or mucous
Surrounded by contractile myoepithelial cells
o Serous acinar cells
Secrete a watery fluid containing soluble proteins such
as salivary amylase
o Mucous acinar cells
Secrete a viscous fluid containing mucus
Contents of saliva
o H2O
o Ions (HCO3-)
o Enzymes (amylase)
o Antibacterial compounds (lysozyme, lactoferrin, IgA), Mucus
Functions of saliva
o Lubrication for food (mucins)
o Partial digestion of polysacchardies
Salivary amylase
Cleaves internal alpha-1,4 bonds in starch
Can break down up to 50% of starch before being
inactivated by gastric acid
o Moisten mouth and wash away dissolved food
o Mild antibacterial (lysozyme, lactoferrin)
o Neutralize acids in food and regurgitated stomach acid
o Maintanence of teeth (Ca2+, fluoride)
Xerostomia
o Absence of saliva
o Causes: drug side effects, head and neck radiation therapy,
systemic diseases (Sjogrens syndrome)
o Absence leads to infections, tooth decay, and sever
discomfort
Control of Salivary Secretions
o Primarily by autonomic nervous system
Only area of GI tract not regulated by GI hormones
Parasympathetic innervation
Predominant control begins in the salivatory nuclei
of medulla which is stimulated by taste, smell,
and chewing and is inhibited by sleep, fatigue,
and fear
Sympathetic innervation
Reaches glands through superior cervical ganglia
and acts on glandular beta-adrenergic receptors
(Ach is the major neurotransmitter)
Production of Saliva
o Saliva glands have a high resting blood flow due to high rate
of fluid secretion
Further increased upon secretion by parasympathetic
innervation of blood vessels
o Fluid secreted by acinar cells is plasma like in composition
o Finished hypotonic
As it moves down ducts Na and Cl are reabsorbed and K
is secreted due to abundant Na-K ATPase activity in duct
cells
Cl-HCO3 exchanger in apical membrane is responsible
for alkalinization of salvid
o Increase in flow leads to decrease in hypotonicity of saliva
Less time for ductular modulation
ESOPHAGUS
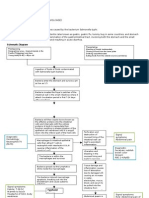
Chewing and Swallowing
o Under voluntary neuromuscular control
Controlled by the swallowing center in the brainstem
Begins as a voluntary action but proceeds reflexively
Anatomy
o Muscular tube about 25 cm long with a sphincter at each end
Upper sphincter anatomical
Lower sphincter is functional
o Swallowing followed by a wave of primary peristalsis which
moves 2-4 cm/sec
When the wave reaches the LES, it relaxes to let food
enter the stomach
Secondary peristalsis can be initiated by distension in
the absence of swallowing
Esophageal Pressures
o Between swallows
Pressure at upper and lower sphincter is positive due to
intrinsic muscular tone
In thoracic cavity reflect intrathoracic pressure so is
negative
In abdominal cavity reflect intra-abdominal pressure
(positive)
o Upon swallowing
UES relaxes and then contracts contraction followed
by peristaltic contraction of the body of the esophagus
LES and fundus relax before contraction arrives
Receptive relaxation
Neural Innervation
o Efferent innervation through Vagus Nerve
o Visceral somatic fibers directly innervate the striated muscle
of the upper 1/3 of the esophagus
o Vagal preganglionic fibers synapse on ganglion cells which
then innervate lower portion of smooth muscle
Regulation of LES
o Contraction regulated by intrinsic properties of smooth
muscle, nerves, and hormones
o Basal tone is myogenic but increased by ACh and Gastrin
o Transient relaxation mediated by inhibitory neurons that use
VIP or NO
o Sphincter tone lacking in newborns and decreased during
pregnancy
o Abnormalities
Failure of LES to function as a sphincter leads to reflux
esophagitis
GERDGastroesophageal Reflux Disease
Failure of LES to relax results in achalsia (over time will
lead to dilation of esophagus)
o
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Genetics 50qDocument62 pagesGenetics 50qAnonymous 4txA8N8etNo ratings yet
- Bile Duct Injuries: Hiwot Fentahun (MD) Year II Surgery ResidentDocument47 pagesBile Duct Injuries: Hiwot Fentahun (MD) Year II Surgery ResidentTsega WesenNo ratings yet
- SeminarDocument33 pagesSeminarTushar GuptaNo ratings yet
- Cholecystitis: Bonoan, Camille Grace Chua, ManilynDocument29 pagesCholecystitis: Bonoan, Camille Grace Chua, ManilynCams BonoanNo ratings yet
- Anatomy of The LiverDocument25 pagesAnatomy of The Liverapi-354184238100% (1)
- Pathophysiology of Typhoid Fever and Acute GastroenteritisDocument3 pagesPathophysiology of Typhoid Fever and Acute Gastroenteritisteddydeclines14100% (5)
- EMQExample RacpDocument5 pagesEMQExample RacpAnonymous 4txA8N8etNo ratings yet
- Operative Solutions in Hepatobiliary and Pancreatic SurgeryDocument352 pagesOperative Solutions in Hepatobiliary and Pancreatic SurgerycirgeralNo ratings yet
- Hanzi Pinyin English: HSK Level 2Document5 pagesHanzi Pinyin English: HSK Level 2Anonymous 4txA8N8etNo ratings yet
- Lap Chole DictationDocument2 pagesLap Chole DictationAshish DongreNo ratings yet
- GI Ch.44-47Document40 pagesGI Ch.44-47W11795800% (1)
- Assignment GiDocument14 pagesAssignment GiVoid LessNo ratings yet
- Hp165-02b-Nash (FF 050816v) ProtegidoDocument9 pagesHp165-02b-Nash (FF 050816v) ProtegidoAnonymous 4txA8N8etNo ratings yet
- 7 DepressionDocument18 pages7 DepressionAnonymous 4txA8N8etNo ratings yet
- Pass Paces EbDocument10 pagesPass Paces EbAnonymous 4txA8N8etNo ratings yet
- An Astronaut at 80 - The SpectatorDocument12 pagesAn Astronaut at 80 - The SpectatorAnonymous 4txA8N8etNo ratings yet
- Remembering Bob ShamrockDocument18 pagesRemembering Bob ShamrockAnonymous 4txA8N8etNo ratings yet
- H IsselbacherDocument5 pagesH IsselbacherAnonymous 4txA8N8etNo ratings yet
- Adpkd: Autosomal Dominant Polycystic Kidney DiseaseDocument7 pagesAdpkd: Autosomal Dominant Polycystic Kidney DiseaseAnonymous 4txA8N8etNo ratings yet
- 4 Things Astronauts Can Teach You About A Good Night's SleepDocument5 pages4 Things Astronauts Can Teach You About A Good Night's SleepAnonymous 4txA8N8etNo ratings yet
- Continuing Medical Examination Cme RationaleDocument2 pagesContinuing Medical Examination Cme RationaleAnonymous 4txA8N8etNo ratings yet
- Topics Runtime: Subjects AnatomyDocument2 pagesTopics Runtime: Subjects AnatomyAnonymous 4txA8N8etNo ratings yet
- Fecal Microbiota Transplantation Induces Remission in Patients With Active Ulcerative Colitis in A Randomized Controlled Trial - GastroenterologyDocument2 pagesFecal Microbiota Transplantation Induces Remission in Patients With Active Ulcerative Colitis in A Randomized Controlled Trial - GastroenterologyAnonymous 4txA8N8etNo ratings yet
- Emergency Medicine PodcastDocument8 pagesEmergency Medicine PodcastAnonymous 4txA8N8etNo ratings yet
- 6 Steps in Assisting in Cardiac Rhythm InterpretationDocument1 page6 Steps in Assisting in Cardiac Rhythm InterpretationAnonymous 4txA8N8etNo ratings yet
- Med Onc JNR HandbookDocument35 pagesMed Onc JNR HandbookAnonymous 4txA8N8etNo ratings yet
- Abdominal Exam DATEDocument3 pagesAbdominal Exam DATEAnonymous 4txA8N8etNo ratings yet
- Radiology Reviewed Meds Reviewed Pathology Reviewed Micro Reviewed "FASTHUG" CheckedDocument1 pageRadiology Reviewed Meds Reviewed Pathology Reviewed Micro Reviewed "FASTHUG" CheckedAnonymous 4txA8N8etNo ratings yet
- MalabsorptionClinicalCasesDocument5 pagesMalabsorptionClinicalCasesAnonymous 4txA8N8etNo ratings yet
- giphysiologySmallGroupCaseDocument2 pagesgiphysiologySmallGroupCaseAnonymous 4txA8N8etNo ratings yet
- 1 Cheng TestDocument7 pages1 Cheng TestAnonymous 4txA8N8etNo ratings yet
- Blood Pressure Measure Machinery MachinesDocument20 pagesBlood Pressure Measure Machinery MachinesAnonymous 4txA8N8etNo ratings yet
- Moraca - The Role of EpiduralDocument11 pagesMoraca - The Role of EpiduralAnonymous 4txA8N8etNo ratings yet
- Human Smoke Questions USDocument12 pagesHuman Smoke Questions USAnonymous 4txA8N8etNo ratings yet
- Brunicardi-1996-Time Management - A RDocument7 pagesBrunicardi-1996-Time Management - A RAnonymous 4txA8N8etNo ratings yet
- Abdominal Exam DATEDocument3 pagesAbdominal Exam DATEAnonymous 4txA8N8etNo ratings yet
- 1Document39 pages1Nadine WangNo ratings yet
- Quick Brown FoxesDocument4 pagesQuick Brown FoxesAnonymous 4txA8N8etNo ratings yet
- Gastro-Quiz-GERDDocument3 pagesGastro-Quiz-GERDIja Lourice RosalNo ratings yet
- Baita, Jonamae S. FEB.18 2022 EDU SCI07 31480Document1 pageBaita, Jonamae S. FEB.18 2022 EDU SCI07 31480Jona BaitaNo ratings yet
- Health - Gastrointestinal DiseasesDocument6 pagesHealth - Gastrointestinal DiseasesMojaro SonNo ratings yet
- Chapter 24 (Digestive System) Chapter 24 (Digestive System)Document30 pagesChapter 24 (Digestive System) Chapter 24 (Digestive System)Pranali BasuNo ratings yet
- ColostomyDocument4 pagesColostomyleslie_macasaetNo ratings yet
- Digestion NewDocument42 pagesDigestion NewPradeepa SamagaNo ratings yet
- Case Presentation (October 3)Document54 pagesCase Presentation (October 3)Ayessa Camelle DumileNo ratings yet
- Bhagatwala Et Al 2015, Indications and ContraindicationsDocument27 pagesBhagatwala Et Al 2015, Indications and Contraindicationsedo adimastaNo ratings yet
- Chapter - 2: Nutrition in AnimalsDocument22 pagesChapter - 2: Nutrition in AnimalsALLURI DEDEEPYA LAKSHYA100% (1)
- Anatomi & Histologi GasterDocument24 pagesAnatomi & Histologi Gastersalvaryn neNo ratings yet
- AMOEBIASISDocument36 pagesAMOEBIASISKhei Laqui SNNo ratings yet
- Chronic Pancreatitis or Pancreatic TumorDocument18 pagesChronic Pancreatitis or Pancreatic Tumorpunct_org3256No ratings yet
- L 17. Symptoms and Signs of GIT Disorders 1Document21 pagesL 17. Symptoms and Signs of GIT Disorders 1sjfk1416No ratings yet
- Gs Toronto Nots PdaDocument34 pagesGs Toronto Nots PdaAhmed AttiaNo ratings yet
- Gastroenterology-Liver, Pancreas and Gall Bladder LecturesDocument7 pagesGastroenterology-Liver, Pancreas and Gall Bladder LecturesMarco Paulo Reyes NaoeNo ratings yet
- EndosDocument8 pagesEndosAli ZainNo ratings yet
- 10 Pepsin On Egg WhiteDocument4 pages10 Pepsin On Egg WhiteZllison Mae Teodoro MangabatNo ratings yet
- Obstructive Jaundice - Center For Advanced Digestive Care - NewYork-Presbyterian:Weill Cornell MedicDocument3 pagesObstructive Jaundice - Center For Advanced Digestive Care - NewYork-Presbyterian:Weill Cornell MedicImam GodlyNo ratings yet
- Lesson Plan - Digestive SystemDocument3 pagesLesson Plan - Digestive SystemLouise GongoraNo ratings yet
- Pancreas Anatomy and PhysiologyDocument34 pagesPancreas Anatomy and PhysiologySourabh MishraNo ratings yet
- Kelompok 3-SIstem PencernaanDocument103 pagesKelompok 3-SIstem PencernaanNurul Fadhillah IsaNo ratings yet