Professional Documents
Culture Documents
Kolestasis
Uploaded by
Nur Ainatun NadrahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kolestasis
Uploaded by
Nur Ainatun NadrahCopyright:
Available Formats
RECOMMENDATIONS
Management of Neonatal Cholestasis: Consensus Statement of the
Pediatric Gastroenterology Chapter of Indian Academy of Pediatrics
VIDYUT BHATIA, *ASHISH BAVDEKAR, $JOHN MATTHAI, #YOGESH WAIKAR AND ANUPAM SIBAL
From Apollo Center for Advanced Pediatrics, Indraprastha Apollo Hospital, New Delhi; *Department of Pediatrics, King Edwards
Memorial Hospital, Pune; $Department of Pediatrics, PSG Institute of Medical Sciences, Coimbatore and #Pediatric
Gastroenterology Clinic, Care hospital, Nagpur, India.
Correspondence to: Dr Vidyut Bhatia, Apollo Center for Advanced Pediatrics, Indraprastha Apollo Hospital, New Delhi 110 076,
India. drvidyut@me.com
Justification: Neonatal cholestasis is an important cause of
chronic liver disease in young children. Late referral and lack of
precise etiological diagnosis are reasons for poor outcome in
substantial number of cases in India. There is a need to create
better awareness among the pediatricians, obstetricians and
primary care physicians on early recognition, prompt evaluation
and referral to regional centers.
from India and the West, to discuss current diagnostic and
management practices in major centers in India, and to identify
various problems in effective diagnosis and ways to improve the
overall outcome. Current problems faced in different areas were
discussed and possible remedial measures were identified. The
ultimate aim would be to achieve results comparable to the
West.
Process: Eminent national faculty members were invited to
participate in the process of forming a consensus statement.
Selected members were requested to prepare guidelines on
specific issues, which were reviewed by two other members.
These guidelines were then incorporated into a draft statement,
which was circulated to all members. A round table conference
was organized; presentations, ensuing discussions, and
opinions expressed by the participants were incorporated into
the final draft.
Recommendations: Early recognition, prompt evaluation and
algorithm-based management will improve outcome in neonatal
cholestasis. Inclusion of stool/urine color charts in well baby
cards and sensitizing pediatricians about differentiating
conjugated
from
the
more
common
unconjugated
hyperbilirubinemia are possible effective steps. Considering the
need for specific expertise and the poor outcome in suboptimally managed cases, referral to regional centers is
warranted.
Objectives: To review available published data on the subject
Keywords: Cholestatic jaundice, Neonate, Practice guidelines.
Laboratories in many private and other medical centers are
now able to do newer tests for precise diagnosis. This
meeting was held to discuss the impact of those programs
and to make appropriate changes in the management
protocol in the light of recent advances in the subject.
eonatal cholestasis (NC) is being increasingly
recognized as an important cause of chronic
liver disease in infants and young children.
The etiology and management of cholestasis
has changed significantly since the consensus statement
last published in 2000 [1]. Three objectives were
identified at the previous meeting. First, age at which
infants are referred to tertiary care centers is very late for
effective evaluation and management and steps need to
be taken to address this problem. Second, tertiary centers
with pediatric gastroenterology units should follow a
uniform protocol of evaluation, and third, the
investigation facilities at some centers need to be
strengthened, so that a more precise final diagnosis,
particularly metabolic disorders, can be arrived at.
DEFINITION
Neonatal cholestasis is defined as conjugated
hyperbilirubinemia occurring in the newborn as a
consequence of diminished bile flow. Conjugated
hyperbilirubinemia in a neonate is defined as a serum
direct/conjugated bilirubin concentration greater than 1.0
mg/dL if the total serum bilirubin (TSB) is <5.0 mg/dL or
greater than 20 percent of TSB if the TSB is >5.0 mg/dL
[4]. It is important to note that the diazo method of
estimating bilirubin, that is still practiced in many Indian
centers, tends to overestimate the direct fraction at lower
bilirubin levels. The group however felt that the above
mentioned definition has to be retained since it is an
internationally accepted one.
A number of steps including a public campaign on
Yellow alert and educational programs at pediatric
meetings were since held to address the key issues [2,3].
The algorithm put in place in 2001 was followed at almost
all major centers, until newer advances were reported.
INDIAN PEDIATRICS
203
VOLUME 51__MARCH 15, 2014
BHATIA, et al.
MANAGEMENT OF NEONATAL CHOLESTASIS
Conjugated hyperbilirubinemia at any age in a
newborn is pathological and requires evaluation. Any
newborn with jaundice and dark yellow urine staining the
diaper with or without pale stools should be strongly
suspected to have NC. Such babies must be referred to an
appropriate center for further investigations and
treatment at the earliest [1]. Sick newborns and younger
infants with deranged liver function tests, particularly
uncorrected coagulopathy, require urgent referral to rule
out infective or metabolic causes of NC.
it is suggestive of cholestasis. The sensitivity, specificity,
and positive predictive value of pale stools for the
detection of biliary atresia (BA) before 60 days as
determined by a color-coded stool chart was noted to be
89.7%, 99.9% and 28.6%, respectively [19]. Although
cholestasis is known to occur in babies with early onset
sepsis [14]. Yet simultaneous screening should be done
for metabolic causes. Galactosemia, a treatable cause,
may be present even in babies with culture proven sepsis.
Babies with tyrosinemia, herpes infection and congenital
hemochromatosis may present in a sick state early in life,
and their recognition and treatment needs to be
incorporated [20]. Non-normalization of liver function
tests (LFTs) even after treatment with appropriate
antibiotics is a pointer towards an underlying metabolic
cause for sepsis [14].
ETIOLOGY
NC affects 1 in 2500 infants in the West [4,5]. In India it
constitutes 19% to 33% of all chronic liver diseases in
children reporting to tertiary care hospitals [1,6-8].
Table I summarizes the etiologic profile of NC in India.
Hepatocellular causes constitute 45% to 69% while
obstructive causes account for 19% to 55% of all cases
[1,6-12].
Yachha, et al. showed that the age of onset of
jaundice in BA was 3-12 days and that of hepatocellular
causes was 16-24 days [2]. However, the mean age of
presentation to a tertiary care center was 2.83.9 months
compared to the desired age of evaluation, that is 4-6
weeks [2,3,15]. Babies with BA appear well and have
normal growth and development in spite of their
jaundice, and this leads to parents and physicians
underestimating the seriousness of the problem [3]. Many
health care professionals also have a misconception that
all well babies with icterus have physiological jaundice
(which is unconjugated and associated with normal urine
color). The group felt that it was a matter of concern that
in India the average age of presentation to tertiary care
centers has shown little change in the last decade. The
group felt that there is a need for creating more awareness
among pediatricians and obstetricians on NC and this can
be achieved through continuing medical education
(CME) programs with the speakers giving the same
message by highlighting the recommendations of this
consensus statement. Enlarging the scope of the yellow
alert to include the whole country through visual and
print media would also be beneficial. The Group
recommended urine and stool color assessment
(minimum 3 stool samples) by the mother and physician
in a stool color card incorporated in all well baby cards
(Indian Academy of Pediatrics and the Government of
India cards). The group also felt that the Taiwanese
experience with stool color cards (subsequently
replicated in other countries) should be possible in India
as well [21].
While 20 to 30% of cases of NC were idiopathic in
earlier studies, [1,6,7,9], recent reports documented this
proportion to be lower [2,8,13-18]. The group felt that
this emphasizes the need for more exhaustive work up
than was recommended earlier. A recent publication with
exhaustive workup has shown that Pi-Z and Pi-S alleles
responsible for alpha-1 antitrypsin deficiency may be rare
in our population [7].
CLINICAL PRESENTATION
Jaundice in newborns is most commonly physiological or
due to ABO/Rh hemolytic incompatibility. However, if
jaundice is associated with dark urine and/or pale stools,
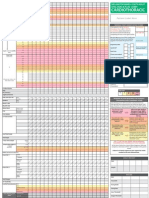
TABLE I ETIOLOGIC PROFILE
INDIA
Etiologic Factor
OF
NEONATAL CHOLESTASIS
N-1008* (%)
IN
N-420#(%)
Obstructive causes
Biliary atresia
34
30
Choledochal cysts
Infections
17
18
Metabolic causes
12
Miscellaneous
Unknown etiology
30
31
Ductal paucity
Undifferentiated
1.2
Hepatocellular causes
*Based
Persistent cholestasis from any cause leads to liver
damage and cirrhosis. Therefore, determining the
specific etiology (medical or surgical) at the earliest is
critical. Also, the outcome of Kasai portoenterostomy
(PE) is directly related to the age of surgery and the
on cumulative data from eight tertiary care centers [1];
#Data from the largest single series (7).
INDIAN PEDIATRICS
204
VOLUME 51__MARCH 15, 2014
BHATIA, et al.
MANAGEMENT OF NEONATAL CHOLESTASIS
expertise of the treating unit. PE when performed earlier
than 60 days of age established adequate bile flow in
64.7% of patients compared with 31.8% when performed
later [22,23]. Improved outcome is also noted in centers
with a higher case load [24]. In the United Kingdom, a
center performing >5 Kasai PE per year, reported
significantly better outcome [25]. Hence, babies
suspected to have BA require early referral to an
appropriate center with expertise in performing PE.
by specific radiological and histopathological tests
(Fig. 1). The principal diagnostic concerns are to
differentiate hepatocellular diseases from anatomical
disorders, and diseases that are managed medically from
those requiring surgical intervention. The most important
initial investigation is to establish cholestasis by measuring
serum bilirubin (total and differential) levels. Severity of
liver dysfunction can be measured by estimating the
prothrombin time or international normalized ratio (INR)
and serum albumin. No single laboratory or imaging test
exists which differentiates biliary obstruction from other
causes of NC reliably in all cases. The serum
transaminases are sensitive indicators of hepatocellular
injury, but lack specificity and prognostic value. High
alkaline phosphatase levels can be seen in biliary
obstruction, but has very low specificity. Gamma-glutamyl
transpeptidase (GGTP) is a marker of biliary obstruction
and is elevated in most cholestatic disorders;
paradoxically low or normal levels are found in patients
with progressive familial intrahepatic cholestasis (PFIC)
and disorders of bile acid synthesis [26].
INVESTIGATIONS
Most centers have been following the protocol that was
outlined in the earlier consensus statement. However in the
light of recent publications and better laboratory support,
modifications are required in the evaluation and
management protocol. The group felt that laboratory
facilities and histopathology support has improved
tremendously in the last decade and hence better work up
is now possible in many centers. The initial evaluation of
an infant with NC includes a complete liver function test
(LFT), thyroid function test, and a sepsis screen followed
NC
Sick
Not Sick
Sepsis Screen +ve
Sepsis Screen ve
Pale stools
Pigmented stools
Fasting USG (see
for contractility
post-feed)
GCT*, Fasting USG
(If the USG show a
choledochal cyst,
the child needs to be
referred for
surgery), Metabolic
tests, Genetic tests,
Liver Biopsy
Test for CMV, HSV, Urinary
Succinylacetone, Ferritin,
GALT if urine reducing sugar
is positive
Normal
------
Treat sepsis
(Galactosemia
needs to be
excluded by urine
reducing sugar by
Benedicts test as
sepsis can be
associated with
Galactosemia)
Liver biopsy
Small gall
bladder
Absent gall
bladder
Choledochal
cyst
Biliary atresia to be
excluded (see Fig.2)
Specific
treatment
Surgery
-----------
Specific
treatment
Optional
* GGT is normal in PFIC
I and II and some inborn
errors of bile acid
metabolism
FIG. 1 Diagnostic algorithm for management of neonatal cholestasis (Part 1).
INDIAN PEDIATRICS
205
VOLUME 51__MARCH 15, 2014
BHATIA, et al.
MANAGEMENT OF NEONATAL CHOLESTASIS
Abdominal ultrasonography may provide findings
suggestive of BA and can also be used to confirm the
existence of other surgically treatable conditions like
choledochal cyst, inspissated bile plug syndrome and
choledocholithiasis.
Abdominal
ultrasonography
findings described in BA include the triangular cord sign
[27], abnormal gallbladder morphology (not visualized
or length <1.9 cm or lack of smooth/complete echogenic
mucosal lining with an indistinct wall or irregular/lobular
contour) [19], no contraction of the gallbladder after oral
feeding and non-visualized common bile duct (CBD). A
distended gall bladder, however, does not rule out a
proximal BA with a distal patent bile duct and mucus
filled gallbladder. It is recommended that ultrasound
should be done after 4 hours of fasting.
structure of the gene and the presence of novel mutations
[30,31]. Hereditary fructose intolerance (HFI) is not an
uncommon cause of neonatal cholestasis in our country as
there are many states where sugar water continues to be
given to newborns until lactation is fully established. It
should be considered in clinical settings where sucrose or
fruit juices have been given to babies. Assay of aldolase B
enzyme in liver biopsy sample confirms HFI. Fructose
challenge test can make the child very ill and is now
obsolete. Plasma tyrosine levels are unreliable in the
diagnosis of tyrosinemia. Measurement of urinary
succinylacetone and succinyl acetoacetate or assay of the
FAH gene is diagnostic [32]. Among the congenital
infections, cytomegalovirus (CMV) is most commonly
implicated. Serum IgM level is unreliable in diagnosis
and should not be used. Assay of pp65 antigen and CMV
polymerase chain reaction (PCR) are more specific and
reliable, if the biochemical tests and histology are
consistent with the diagnosis. Markedly raised serum
ferritin and uncorrected coagulopathy are suggestive of
hemochromatosis that may be confirmed by a buccal
mucosal biopsy.
Hepatobiliary-imino-di-acetic acid (HIDA) scan has
limited role in evaluation of NC especially if the baby has
clearly documented pale or pigmented stools. The time
required (5-7 days) for priming before the scan,
especially in patients who are referred late, is a limitation.
The group felt that good-quality HIDA scan may not be
available everywhere in our country, and therefore,
delaying the liver biopsy for it is not justified. Performing
a HIDA scan is optional and one may go for a liver biopsy
straightaway (Fig. 2). HIDA is, however, useful in the
diagnosis of the uncommon causes like spontaneous
perforation of the bile duct [28]. Intra-operative
cholangiogram (IOC) remains the gold standard for
diagnosis of BA.
A two part diagnostic algorithm to help in the
management of NC is given in Fig.1 and Fig. 2.
TREATMENT
General Medical Management
Most infants with NC are underweight and will need
nutritional support. The goal is to provide adequate
calories to compensate for steatorrhea and to prevent/
treat malnutrition. The calorie requirement is
approximately 125% of the recommended dietary
allowance (RDA) based on ideal body weight [33]. In
breastfed infants, breastfeeding should be encouraged
and medium-chain triglyceride (MCT) oil should be
administered in a dose of 1-2 mL/kg/d in 2-4 divided
doses in expressed breast milk [34]. In older infants, a
milk-cereal-mix fortified with MCT is preferred. Adding
puffed rice powder and MCT to milk can make feeds
energy-dense. Essential fatty acids should constitute 23% of the energy provided. Vegetable protein at 2-3 g/kg/
d is recommended [34].
Liver biopsy is an essential investigation in the
evaluation of NC. Early recognition of BA by liver biopsy
can avoid unnecessary laparotomy (5). The characteristic
histopathology features of BA are bile duct proliferation,
bile plugs in ducts, fibrosis and lymphocytic infiltrates in
the portal tracts. The reported sensitivity, specificity and
accuracy of liver biopsy in the diagnosis of BA are 8999%, 82-98% and 60-95%, respectively [16].
Percutaneous liver biopsy in early infancy under local
anesthesia and sedation is a safe procedure, if performed
by competent physicians [29]. The group opined that the
biopsy must be interpreted by an experienced pathologist
in conjunction with the clinical profile and results of the
other investigations. In cases of doubt, a second opinion
should be sought.
Infants with cholestasis require supplementation with
fat-soluble vitamins administered orally as water-soluble
preparations. Suggested daily vitamin and mineral
supplementation are given in Table II. In treatment of
vitamin deficiencies, standard deficiency protocols
should be followed. 1,25 dihydroxy Vitamin D3 (0.05-0.2
ug/kg/d) is recommended in the presence of significant
bone changes or patients having severe cholestasis [34].
Vitamin K is administered at a dose of 5 mg
In galactosemia, urine is positive for non-glucose
reducing substances while the infant is on lactose feeds.
E. coli sepsis in the presence of liver cell dysfunction is
very characteristic of galactosemia. Assay of Galactose-1
phosphate uridyl transferase (GALT) enzyme is used for
confirmation. Mutational analysis of the GALT gene from
Indian subjects has revealed heterogeneity in the
INDIAN PEDIATRICS
206
VOLUME 51__MARCH 15, 2014
BHATIA, et al.
MANAGEMENT OF NEONATAL CHOLESTASIS
Billary atresia to be
excluded
(Baby not sick, pale stools, small or absent gall bladder on
fasting ultrasound)
Age <6 weeks
Age 6 weeks
Age >90 days with ascites
Age >120 days
-------
HIDA scan after 3
days of priming
Excretion
No Excretion
Refer to a transplant center
Liver Biopsy
Specific
treatment
Inconclusive
Biliary atresia
Intra operative Cholangiogram +
Kasai operation
----------- Optional
FIG. 2 Diagnostic algorithm to help in the management of neonatal cholestasis (Part 2).
(5-10 mg/kg/d), and phenobarbitone (510 mg/kg/d).
Symptom chart should be made for pruritus. Depending
on severity and response to previous agent, add-on drug
can be considered. Appropriate antibiotics depending on
the site of infection and culture sensitivity reports need to
be administered in patients with bacterial sepsis.
intramuscular, subcutaneously or intravenously, at
diagnosis to correct the coagulopathy. If the INR is
markedly prolonged, intramuscular injections should be
avoided. Vitamin supplementation should be continued
till 3 months after resolution of jaundice [35].
Specific treatment
Kasais PE consists of removal of the atretic extrahepatic tissue and a Roux-en-Y jejunal loop anastomosis to
the hepatic hilum. PE may be considered successful if
serum bilirubin normalizes after surgery. In general, over
half the patients normalize their bilirubin after Kasais PE if
performed within six months [36]. About 20% of all
patients undergoing Kasais PE during infancy survive into
adulthood with their native liver [36,37]. In children with
progressive familial intrahepatic cholestasis (PFIC)
without decompensated cirrhosis, external and internal
biliary diversion has been shown to be of benefit [38].
Surgery gives excellent results for choledochal cysts and
should be performed as soon as the diagnosis is made. The
recent consensus statement of the Pediatric
Gastroenterology chapter on Acute liver failure gives more
details on the management of liver failure in NC [39].
Special infant formula and diets are recommended for
children with specific diagnosis (galactosemia,
fructosemia and tyrosinemia). However these formulae
are currently not available in India. The group feels that
steps must be taken to make them available at the earliest.
Treatment with nitisinone (1 mg/kg/d) in addition to
dietary restriction leads to rapid reduction of toxic
metabolites in tyrosinemia. Specific therapy is
recommended for patients with CMV (associated
neurological involvement), herpes and toxoplasmosis
related cholestasis. There is no role for steroids in
idiopathic neonatal hepatitis.
In infants with pruritus due to severe cholestasis, the
group recommended, in the following order:
Ursodeoxycholic acid (UDCA) (20 mg/kg/d), rifampicin
INDIAN PEDIATRICS
207
VOLUME 51__MARCH 15, 2014
BHATIA, et al.
MANAGEMENT OF NEONATAL CHOLESTASIS
TABLE II SUGGESTED DAILY VITAMIN AND MINERAL
REQUIREMENTS IN INFANTS WITH CHOLESTASIS
Route
Dose*
Vitamin A#
Oral
5000-25,000 IU/d
Vitamin D
Oral
400-1200 IU/d
Vitamin E
Oral
50-400 IU/d or 15-25 IU/
kg/d of TPGS form if
available
Vitamin K$
Oral
2.5 twice/week to 5 mg/d
Parenteral
2-5 mg IM, SC or IV
4 weekly
Water soluble vitamins Oral
1-2 times the RDA
Calcium**
Oral
20-100 mg/kg/d
Phosphorus
Oral
25-50 mg/kg/d
Zinc
Oral
1 mg/kg/d
Magnesium
Oral
1-2 mEq/kg/d
Intravenous 0.3-0.5 mEq/ kg over
3 hours of 50% solution
Elemental iron
Oral
5-6 mg/kg/d
Adapted from Ref. 39
*Doses are provided as a guide only and will need to be adjusted
based on response and levels of the vitamins. #Careful monitoring
required as Vitamin A itself is hepatotoxic; $Vitamin K1 preparation
preferred, as it is safe for G6PD deficient individuals; **Calcium should
always be supplemented along with Vitamin D.
Liver transplantation
Liver Transplantation, the standard therapy for
decompensated cirrhosis due to any cause, is now well
established in India as well [40]. Any baby, who has had
Kasais PE and the bilirubin remains >6 mg/dL, three
months after surgery, should be referred to a transplant
center. Babies with BA who present with decompensated
cirrhosis (low albumin, prolonged INR, ascites) are not
likely to improve with a Kasai PE and should be referred
for liver transplantation. Of the 355 transplants in children
that have been performed in India till 2012, 30% have been
for BA [41]. Living related liver transplantation (the vast
majority of liver transplants in India are living related),
performed at experienced centers, is associated with
favorable outcomes, with 5- and 10-year survival rates of
98% and 90%, respectively [42-44].
APPENDIX
List of Invited Participants
AK Patwari, Akshay Kapoor, Akshay Saxena, Alok Hemal,
Anjali Kulkarni, Anshu Srivastava, Anupam Sibal (AS), Ashish
Bavdekar (AB), BD Dwivedi, BR Thapa, Dhanasekhar K., John
Mathai (JM), Lalit Bharadia, Malathi Sathiyasekharan, Manoja
Das, Narendra K Arora, Neelam Mohan*, Nishant Wadhwa,
Pankaj Vohra, Pawan Rawal*, Praveen Kumar, Rajeev Tomar,
Rajiv Redkar, Rakesh Mishra, SK Mittal*, S Srinivas, Sarath
Gopalan, Seema Alam*, Shrish Bhatnagar*, Subash Gupta, Sujit
NC constitutes almost one-third of children with
chronic liver disease in major hospitals in India. BA,
NH and metabolic causes are the most important
causes in India.
INDIAN PEDIATRICS
Malnutrition adversely affects the outcome in infants
with cholestasis. Nutritional support and vitamin/
mineral supplementation is recommended in all babies
with NC. Special formulae may have a role in select
cases.
When NC leads to liver failure, LT should be offered.
Success rates in India are comparable to those in the
West.
Contributors: VB composed the first draft of this statement,
which after input from AB, JM, YW and AS was circulated to all
the participants.
Funding: Rakhi and Adish Oswal funded the Round Table
Conference in memory of their son Kunwar Viren Oswal.
Competing interests: None stated
CONCLUSIONS AND RECOMMENDATIONS
Early identification of the cause is essential for a
favorable outcome. This requires specific biochemical
tests, imaging studies and interpretation of
histopathology by experienced personnel and is now
possible in major centers all over India.
The overall outcome in India is far from satisfactory,
due to late referral. The mean age at presentation in
tertiary care centers is still over 3 months compared to
recommended age of less than 60 days.
To ensure early referral, there is an urgent need to
sensitize pediatricians, obstetricians and other
primary-care physicians on the need for early
evaluation. Yellow alert should be extended to an AllIndia level and the stool color card should be
incorporated in the well-baby cards of IAP and the
Government of India.
Metabolic diseases (e.g. galactosemia, fructosemia,
hemochromatosis, tyrosinemia) and inherited diseases
like PFIC are increasingly being diagnosed in tertiary
centers. Establishment of regional referral labs will
enable greater diagnosis of causes of NC.
Ultrasound, isotope scan and liver biopsy
interpretation in experienced hands are effective in
ruling out surgical causes in a majority of cases. If BA
cannot be ruled out with certainty, an experienced
surgeon should perform a laparotomy andintraoperative cholangiography.
208
VOLUME 51__MARCH 15, 2014
BHATIA, et al.
MANAGEMENT OF NEONATAL CHOLESTASIS
Chowdhary*, Sumathi B., Sutapa Ganguly, Ujjal Poddar*, VS
Sankaranarayanan, Veena Malhotra, Vibhor Borkar, Vidyut
Bhatia (VB), Vishnu Biradar, Yogesh Waikar (YW)
*Contributed but could not attend the Round Table Conference
th
on 8 December 2012.
16. Rastogi A, Krishnani N, Yachha SK, Khanna V, Poddar U,
Lal R. Histopathological features and accuracy for
diagnosing biliary atresia by prelaparotomy liver biopsy in
developing countries. J Gastroenterol Hepatol.
2009;24:97-102.
17. Shah I, Bhatnagar S. Clinical profile of chronic
hepatobiliary disorders in children: experience from
tertiary referral centre in Western India. Trop
Gastroenterol. 2010;31:108-10.
18. Yachha SK, Mohindra S. Neonatal cholestasis syndrome:
Indian scene. Ind J Pediatr. 1999;66:S94-6.
19. Chen SM, Chang MH, Du JC, Lin CC, Chen AC, Lee HC,
et al. Screening for biliary atresia by infant stool color card
in Taiwan. Pediatrics. 2006;117:1147-54.
20. Burton BK. Inborn errors of metabolism in infancy: a guide
to diagnosis. Pediatrics. 1998;102:E69.
21. Lien TH, Chang MH, Wu JF, Chen HL, Lee HC, Chen AC,
et al. Effects of the infant stool color card screening
program on 5-year outcome of biliary atresia in Taiwan.
Hepatology. 2011;53:202-8.
22. Lally KP, Kanegaye J, Matsumura M, Rosenthal P, Sinatra
F, Atkinson JB. Perioperative factors affecting the outcome
following repair of biliary atresia. Pediatrics. 1989;83:7236.
23. Serinet MO, Wildhaber BE, Broue P, Lachaux A, Sarles J,
Jacquemin E, et al. Impact of age at Kasai operation on its
results in late childhood and adolescence: a rational basis
for biliary atresia screening. Pediatrics. 2009;123:1280-6.
24. Lampela H, Ritvanen A, Kosola S, Koivusalo A, Rintala R,
Jalanko H, et al. National centralization of biliary atresia
care to an assigned multidisciplinary team provides highquality outcomes. Scand J Gastroenterol. 2012;47:99-107.
25. McKiernan PJ, Baker AJ, Kelly DA. The frequency and
outcome of biliary atresia in the UK and Ireland. Lancet.
2000;355:25-9.
26. Whitington PF, Freese DK, Alonso EM, Schwarzenberg
SJ, Sharp HL. Clinical and biochemical findings in
progressive familial intrahepatic cholestasis. J Pediatr
Gastroenterol Nutr. 1994;18:134-41.
27. Hsiao CH, Chang MH, Chen HL, Lee HC, Wu TC, Lin CC,
et al. Universal screening for biliary atresia using an infant
stool color card in Taiwan. Hepatology. 2008;47:1233-40.
28. Niedbala A, Lankford A, Boswell WC, Rittmeyer C.
Spontaneous perforation of the bile duct. Am Surg.
2000;66:1061-3.
29. Lee WS, Looi LM. Usefulness of a scoring system in the
interpretation of histology in neonatal cholestasis. World J
Gastroenterol. 2009;15:5326-33.
30. Singh R, Thapa BR, Kaur G, Prasad R. Biochemical and
molecular characterization of GALT gene from Indian
galactosemia patients: identification of 10 novel mutations
and their structural and functional implications. Clin Chim
Acta. 2012;414:191-6.
31. Singh R, Kaur G, Thapa BR, Prasad R, Kulkarni K. A case
of
classical
galactosemia:
identification
and
characterization of 3 distinct mutations in galactose-1phosphate uridyl transferase (GALT) gene in a single
family. Indian J Pediatr. 2011;78:874-6.
32. Bijarnia S, Puri RD, Ruel J, Gray GF, Jenkinson L, Verma
REFERENCES
1. Consensus report on neonatal cholestasis syndrome.
Pediatric Gastroenterology Subspecialty Chapter of Indian
Academy of Pediatrics. Indian Pediatr. 2000;37:845-51.
2. Yachha SK, Sharma A. Neonatal cholestasis in India.
Indian Pediatr. 2005;42:491-2.
3. Yachha SK. Cholestatic jaundice during infancy. Indian J
Gastroenterol. 2005;24:47-8.
4. Davis AR, Rosenthal P, Escobar GJ, Newman TB.
Interpreting conjugated bilirubin levels in newborns. J
Pediatr. 2011;158:562-5.
5. Moyer V, Freese DK, Whitington PF, Olson AD, Brewer F,
Colletti RB, et al. Guideline for the evaluation of
cholestatic jaundice in infants: recommendations of the
North American Society for Pediatric Gastroenterology,
Hepatology and Nutrition. J Pediatr Gastroenterol Nutr.
2004;39:115-28.
6. Yachha SK, Khanduri A, Kumar M, Sikora SS, Saxena R,
Gupta RK, et al. Neonatal cholestasis syndrome: an
appraisal at a tertiary center. Indian Pediatr. 1996;33:72934.
7. Arora NK, Arora S, Ahuja A, Mathur P, Maheshwari M,
Das MK, et al. Alpha 1 antitrypsin deficiency in children
with chronic liver disease in North India. Indian Pediatr.
2010;47:1015-23.
8. Yachha SK, Sharma BC, Khanduri A, Srivastava A.
Current spectrum of hepatobiliary disorders in northern
India. Indian Pediatr. 1997;34:885-90.
9. Alagille D, Habib EC, Thomassin N. Latresie des voies
biliaires extrahepatiques permeables chez lenfant. J Par
Pediatr 1969:301-18.
10. Kamath BM, Spinner NB, Piccoli DA. Alagille Syndrome.
In: Suchy F, Sokol RJ, Balistreri WF, editors. Liver
Disease in Children. Third ed. New York: Cambridge
University Press; 2007. p. 326-45.
11. Mizuta K, Sanada Y, Wakiya T, Urahashi T, Umehara M,
Egami S, et al. Living-donor liver transplantation in 126
patients with biliary atresia: single-center experience.
Transplant Proc. 2010;42:4127-31.
12. Sanghai SR, Shah I, Bhatnagar S, Murthy A. Incidence and
prognostic factors associated with biliary atresia in
Western India. Ann Hepatol. 2009;8:120-2.
13. Ahmad M, Jan M, Ali W, Shabir ud d, Bashir C, Iqbal Q, et
al. Neonatal cholestasis in Kashmiri children. JK Pract.
2000;7:125-6.
14. Khalil S, Shah D, Faridi MM, Kumar A, Mishra K.
Prevalence and outcome of hepatobiliary dysfunction in
neonatal septicaemia. J Pediatr Gastroenterol Nutr.
2012;54:218-22.
15. Poddar U, Thapa BR, Das A, Bhattacharya A, Rao KL,
Singh K. Neonatal cholestasis: differentiation of biliary
atresia from neonatal hepatitis in a developing country.
Acta Paediatr. 2009;98:1260-4.
INDIAN PEDIATRICS
209
VOLUME 51__MARCH 15, 2014
BHATIA, et al.
33.
34.
35.
36.
37.
38.
39.
MANAGEMENT OF NEONATAL CHOLESTASIS
IC. Tyrosinemia type Idiagnostic issues and prenatal
diagnosis. Indian J Pediatr. 2006;73:163-5.
Suchy FJ. Neonatal cholestasis. Pediatr Rev. 2004;25:38896.
Feranchak AP, Sokol RJ. Medical and nutritional
mManagement of cholestasis in infants and children. In:
Suchy FJ, Sokal RJ, Balistreri WF, editors. Liver Diseases
in Children. 3rd ed. New York: Cambridge University
Press; 2007. p. 190-231.
Venigalla S, Gourley GR. Neonatal cholestasis. Semin
Perinatol. 2004;28:348-55.
Sokol RJ, Shepherd RW, Superina R, Bezerra JA, Robuck
P, Hoofnagle JH. Screening and outcomes in biliary
atresia: summary of a National Institutes of Health
workshop. Hepatology. 2007;46:566-81.
Bassett MD, Murray KF. Biliary atresia: recent progress. J
Clin Gastroenterol. 2008;42:720-9.
Sharma D, Shah UH, Sibal A, Chowdhary SK.
Cholecystoappendicostomy for progressive familial
intrahepatic cholestasis. Indian Pediatr. 2010;47:626-8.
Bhatia V, Bavdekar A, Yachha SK. Management of acute
INDIAN PEDIATRICS
40.
41.
42.
43.
44.
210
liver failure in infants and children: Consensus statement of
the Pediatric Gastroenterology Chapter, Indian Academy
of Pediatrics. Indian Pediatr. 2013;50:477-82.
Poonacha P, Sibal A, Soin AS, Rajashekar MR,
Rajakumari DV. Indias first successful pediatric liver
transplant. Indian Pediatr. 2001;38:287-91.
Sibal A. Pediatric Liver transplantation in India: Past,
Present and future. 21th Annual Conference of Indian
National Association for Study of the Liver [INASL] 2013;
Hyderabad, India.
Utterson EC, Shepherd RW, Sokol RJ, Bucuvalas J, Magee
JC, McDiarmid SV, et al. Biliary Atresia: Clinical Profiles,
Risk Factors, and Outcomes of 755 Patients Listed for
Liver Transplantation. J Pediatr. 2005;147:180-5.
Wang SH, Chen CL, Concejero A, Wang CC, Lin CC, Liu
YW, et al. Living donor liver transplantation for biliary
atresia. Chang Gung Med J. 2007;30:103-8.
Kaur S, Wadhwa N, Sibal A, Jerath N, Sasturkar S.
Outcome of live donor liver transplantation in Indian
children with bodyweight 7.5 kg. Indian Pediatr.
2011;48:51-4.
VOLUME 51__MARCH 15, 2014
You might also like
- Journal of Pediatric Surgery: Ibrahim UygunDocument4 pagesJournal of Pediatric Surgery: Ibrahim UygunNur Ainatun NadrahNo ratings yet
- Journal of Pediatric Surgery: Shawn T. Liechty, Douglas C. Barnhart, Jordan T. Huber, Sarah Zobell, Michael D. RollinsDocument4 pagesJournal of Pediatric Surgery: Shawn T. Liechty, Douglas C. Barnhart, Jordan T. Huber, Sarah Zobell, Michael D. RollinssuperwymNo ratings yet
- 1 s2.0 S002234681500617X MainDocument7 pages1 s2.0 S002234681500617X MainNur Ainatun NadrahNo ratings yet
- Journal of Pediatric Surgery: Shawn T. Liechty, Douglas C. Barnhart, Jordan T. Huber, Sarah Zobell, Michael D. RollinsDocument4 pagesJournal of Pediatric Surgery: Shawn T. Liechty, Douglas C. Barnhart, Jordan T. Huber, Sarah Zobell, Michael D. RollinssuperwymNo ratings yet
- Journal of Pediatric SurgeryDocument6 pagesJournal of Pediatric SurgeryNur Ainatun NadrahNo ratings yet
- Journal of Pediatric SurgeryDocument6 pagesJournal of Pediatric SurgeryNur Ainatun NadrahNo ratings yet
- Journal of Pediatric Surgery: Indepent Review ArticlesDocument4 pagesJournal of Pediatric Surgery: Indepent Review ArticlesNur Ainatun NadrahNo ratings yet
- 1 s2.0 S002234681500617X MainDocument7 pages1 s2.0 S002234681500617X MainNur Ainatun NadrahNo ratings yet
- Journal of Pediatric SurgeryDocument5 pagesJournal of Pediatric SurgeryNur Ainatun NadrahNo ratings yet
- Journal of Pediatric SurgeryDocument3 pagesJournal of Pediatric SurgeryNur Ainatun NadrahNo ratings yet
- 1 s2.0 S0022346815006351 MainDocument6 pages1 s2.0 S0022346815006351 MainNur Ainatun NadrahNo ratings yet
- 1 s2.0 S0022346815006399 MainDocument6 pages1 s2.0 S0022346815006399 MainNur Ainatun NadrahNo ratings yet
- Journal of Pediatric Surgery: Contents Lists Available atDocument6 pagesJournal of Pediatric Surgery: Contents Lists Available atNur Ainatun NadrahNo ratings yet
- Journal of Pediatric SurgeryDocument4 pagesJournal of Pediatric SurgeryNur Ainatun NadrahNo ratings yet
- 1 s2.0 S0022346815007198 MainDocument2 pages1 s2.0 S0022346815007198 MainNur Ainatun NadrahNo ratings yet
- 1 s2.0 S0022346815006417 MainDocument6 pages1 s2.0 S0022346815006417 MainNur Ainatun NadrahNo ratings yet
- Journal of Pediatric SurgeryDocument4 pagesJournal of Pediatric SurgeryNur Ainatun NadrahNo ratings yet
- 1 s2.0 S0022346815006478 MainDocument6 pages1 s2.0 S0022346815006478 MainNur Ainatun NadrahNo ratings yet
- Paediatric Cholestatic Liver Disease: Diagnosis, Assessment of Disease Progression and Mechanisms of FibrogenesisDocument16 pagesPaediatric Cholestatic Liver Disease: Diagnosis, Assessment of Disease Progression and Mechanisms of FibrogenesiswintannNo ratings yet
- 1 s2.0 S0022346815006430 MainDocument5 pages1 s2.0 S0022346815006430 MainNur Ainatun NadrahNo ratings yet
- 1 s2.0 S0022346815006454 MainDocument5 pages1 s2.0 S0022346815006454 MainNur Ainatun NadrahNo ratings yet
- 1 s2.0 S1063458415013187 MainDocument13 pages1 s2.0 S1063458415013187 MainNur Ainatun NadrahNo ratings yet
- 1 s2.0 S0022346815006466 MainDocument5 pages1 s2.0 S0022346815006466 MainNur Ainatun NadrahNo ratings yet
- 4200 p167 PDFDocument26 pages4200 p167 PDFNur Ainatun NadrahNo ratings yet
- GH 04 691Document3 pagesGH 04 691Nur Ainatun NadrahNo ratings yet
- Fetal Growth and Body Proportion in Preeclampsia.26Document9 pagesFetal Growth and Body Proportion in Preeclampsia.26Nur Ainatun NadrahNo ratings yet
- 2248Document14 pages2248Nur Ainatun NadrahNo ratings yet
- Health Problems and Health Seeking Behaviour of Hospital Cleaners in A Tertiary Health Facility in South West NigeriaDocument6 pagesHealth Problems and Health Seeking Behaviour of Hospital Cleaners in A Tertiary Health Facility in South West NigeriaNur Ainatun NadrahNo ratings yet
- Apert Syndrome: Anaesthetic Concerns and Challenges: Egyptian Journal of AnaesthesiaDocument3 pagesApert Syndrome: Anaesthetic Concerns and Challenges: Egyptian Journal of AnaesthesiaNur Ainatun NadrahNo ratings yet
- G-Tze Et Al-2015-Frontiers in PediatricsDocument32 pagesG-Tze Et Al-2015-Frontiers in PediatricsNur Ainatun NadrahNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Orthobullets Foot and AnkleDocument88 pagesOrthobullets Foot and AnkleStevent Richardo100% (1)
- Bahasa InggrisDocument6 pagesBahasa InggrisSofi SusantoNo ratings yet
- Adult Early Warning Score Observation Chart For Cardiothoracic UnitDocument1 pageAdult Early Warning Score Observation Chart For Cardiothoracic UnitalexipsNo ratings yet
- DOPR Vision 2030Document36 pagesDOPR Vision 2030Hendi HendriansyahNo ratings yet
- MBF90324234Document407 pagesMBF90324234Emad Mergan100% (1)
- Satyug Darshan Vidalaya1Document30 pagesSatyug Darshan Vidalaya1Naina GuptaNo ratings yet
- Fertilization Reflection PaperDocument2 pagesFertilization Reflection PaperCrisandro Allen Lazo100% (2)
- Development of The Vertebrate EyeDocument5 pagesDevelopment of The Vertebrate Eyezari_pak2010No ratings yet
- Eaves Nickolas A 201211 MASc ThesisDocument69 pagesEaves Nickolas A 201211 MASc Thesisrajeev50588No ratings yet
- Medical FlyerDocument2 pagesMedical FlyerThana PalNo ratings yet
- Electronic Physician (ISSN: 200 08-5842)Document10 pagesElectronic Physician (ISSN: 200 08-5842)Sapi KemploNo ratings yet
- Carbon Monoxide PoisoningDocument31 pagesCarbon Monoxide PoisoningDheerajNo ratings yet
- CATHETERIZATIONDocument3 pagesCATHETERIZATIONrnrmmanphdNo ratings yet
- Aldrine Ilustricimo VS Nyk Fil Sjip Management IncDocument11 pagesAldrine Ilustricimo VS Nyk Fil Sjip Management Inckristel jane caldozaNo ratings yet
- Standardised Nomenclature of Animal Parasitic Diseases (Snopad)Document67 pagesStandardised Nomenclature of Animal Parasitic Diseases (Snopad)Pwaveno BamaiyiNo ratings yet
- Sample Chapter of Assessment Made Incredibly Easy! 1st UK EditionDocument28 pagesSample Chapter of Assessment Made Incredibly Easy! 1st UK EditionLippincott Williams and Wilkins- Europe100% (1)
- Cellular Aberration Acute Biologic Crisis 100 Items - EditedDocument8 pagesCellular Aberration Acute Biologic Crisis 100 Items - EditedSherlyn PedidaNo ratings yet
- Week 6 Nursing Care of The Family With Reproductive DisordersDocument27 pagesWeek 6 Nursing Care of The Family With Reproductive DisordersStefhanie Mae LazaroNo ratings yet
- Aynı MakaleDocument95 pagesAynı MakalesalihcikkNo ratings yet
- 10a General Pest Control Study GuideDocument128 pages10a General Pest Control Study GuideRomeo Baoson100% (1)
- Bipolar Disorder - A Cognitive Therapy Appr - Cory F. NewmanDocument283 pagesBipolar Disorder - A Cognitive Therapy Appr - Cory F. NewmanAlex P100% (1)
- ETT IntubationDocument27 pagesETT IntubationGilbert Sterling Octavius100% (1)
- Towards A Sociology of Health Discourse in AfricaDocument172 pagesTowards A Sociology of Health Discourse in AfricaDavid Polowiski100% (2)
- ANIOSPRAY QUICK-Fiche Technique-00000-ENDocument2 pagesANIOSPRAY QUICK-Fiche Technique-00000-ENGustea Stefan AlinNo ratings yet
- Growth Comparison in Children With and Without Food Allergies in 2 Different Demographic PopulationsDocument7 pagesGrowth Comparison in Children With and Without Food Allergies in 2 Different Demographic PopulationsMaria Agustina Sulistyo WulandariNo ratings yet
- Thesis On Hypertension in PregnancyDocument7 pagesThesis On Hypertension in Pregnancydwt29yrp100% (2)
- Nursing Management of HypertensionDocument152 pagesNursing Management of HypertensionEnfermeriaAncam100% (3)
- Environmental Studies-FIRST UNIT-vkmDocument59 pagesEnvironmental Studies-FIRST UNIT-vkmRandomNo ratings yet
- National Geographic USA - January 2016Document148 pagesNational Geographic USA - January 2016stamenkovskib100% (4)
- Geria NCPDocument4 pagesGeria NCPBrylle CapiliNo ratings yet