Professional Documents
Culture Documents
Fulltext Schizophrenia v2 Id1013
Uploaded by
RanggaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fulltext Schizophrenia v2 Id1013
Uploaded by
RanggaCopyright:
Available Formats
Open Access
Journal of Schizophrenia Research
Short Communication
Open Dialogue Approach An Alternative to
Neuroleptics or Development of Pharmacologically
Cautious Treatment of Schizophrenia?
Received: June 03, 2015; Accepted: July 13, 2015;
Published: July 15, 2015
therapy, while as many as 84% of the treated patients resumed their
careers or education [8,9]. Neuroleptics were used less frequently and
were prescribed in only 33% of cases during the assessed periods [7].
Even though the described data showed long-term stability in a study
conducted after 10 years of introducing the approach [7-9], ODA
critics questioned the methodological accuracy of the quantitative
analysis (limited cohorts of patients impede the generalization of the
outcomes, the use of historical controls hampers the comparison of
data obtained by other researchers). They suggested that some of the
patients who dropped out may have been treated in more biologicallyoriented institutions [10,11]. Many scientists acknowledge the
positive impact of ODA on the service culture in the public mental
health sector. However, some experts question the extent to which
ODA theoretical principles should be followed [11,12].
Introduction
Aim of the Article
In Finnish Western Lapland, a family- and network-oriented,
comprehensive, psychotherapeutic model of psychiatric care has
been developed within public mental health services since the
1980s [1]. It was primarily aimed to optimize treatment of acute
psychosis inpatients and their families. A number of nation-wide
research projects conducted from the 1960s to 80s by alanen and his
co workers led to the formulation of the Need-Adapted Approach
(NAA) [2-6]. In the mid-1990s, this further evolved in Western
Lapland into the Open Dialogue Approach (ODA) [7]. ODA is based
on three core elements: i) family network orientated team treatment,
ii) the provision of elaborate psychotherapeutic training for all mental
health professionals and iii) carrying out scientific measurements
assessing the quality of the care provided in combination with the
development of the method [8,9]. During the application of ODA
over several years, Finnish researchers formulated seven leading
principles that serve as guidelines form entail health practitioners: (1)
the organization of a meeting with the patient and his network within
24 hours of the first contact with the psychiatric unit (2) focusing
on the patients social network (3) the formulation of a tailor-made
treatment plan adapted to the patients changing needs (4) the
shifting of responsibility of arranging case-specific teams onto mental
health professionals (5) maintenance of a psychological continuity by
enabling collaboration between personnel from various facilities (6)
restoring a sense of security in order to tolerate uncertainty related to
the crisis situation (7) supporting the fundamental value of polyphony
(every voice present at the joint meeting has a right to speak and to
be heard) and dialogicity (seeking dialogue to recognize what was
said),which help find a new language that enables patients to describe
cryptic experiences. Seikkula et al. presented challenging treatment
outcomes, where up to 81% of patients with a first-episode psychosis
did not reveal any residual psychotic symptoms at the end of the
The aim of this paper is to present a peer supported perspective on
ODA as an alternative or complementary approach to the Treatmentas-Usual [TAU], which has a psychosocially - based, comprehensive,
development approach.
Kapciski M1*, Wojtynska R2 and Rymaszewska
J1
1
Department of Psychiatry, Division of ConsultationLiasion Psychiatry and Neuroscience, Wrocaw Medical
University, Wrocaw, Poland
2
Department of Psychiatry, Faculty of Postgraduate
Medical Training, Wrocaw Medical University, Wrocaw,
Poland
*Corresponding author: Kapciski M, Department of
Psychiatry, Division of Consultation-Liasion Psychiatry
and Neuroscience, Wrocaw Medical University, Pasteura
St 10, 50-367 Wrocaw, Poland, Tel: 0048 506 582 405;
Email: michal.klapcinski@gmail.com
J Schizophr Res - Volume 2 Issue 2 - 2015
Submit your Manuscript | www.austinpublishinggroup.com
Kapciski et al. All rights are reserved
Discussion
In his review of ODA literature, Lakeman argues that the Finnish
approach gained much international attention due to the reported
reduction of the incidence of schizophrenia and a minimal use of
neuroleptics [1,12]. Furthermore, the psychiatric service culture in
Western Planeshifted towards a more humanistic and community
based approach, which was well accepted by the service users. This
was due to the fact that 5-10% of the local population came into
contact with psychiatric facilities each year and was deeply engaged in
the therapeutic process of their distressed relatives [7]. Thus, patients
and their social networks were given the responsibility to draw up a
recovery plan, where the patients choice on treatment was to be taken
into consideration. Morrison [13] reveals that multiple uncertainties
emerge when discussing antipsychotic pharmacotherapy, due to the
overestimation of the efficacy of neuroleptics and the underestimation
of their harmful potential. Lehtinen et al. [14] questions the immediate
neuroleptisation among patients with first-episode non-affective
psychosis, pointing out a similar two-year outcome of an experimental
(with a minimal neuroleptic regime) and control (neuroleptics used
according to TAU) group. Thereby, he recommends an integrative
treatment model where intense psychosocial activities remain at the
core of the therapy. Stratford et al. [15] note that focusing on recovery
is not an anti-medication attitude towards treatment. However, this
does require psychiatrists to show trans-disciplinary team-work and a
relational orientation in their approach to the patients. There is some
evidence supporting the rationale behind creating early intervention
Citation: Kapciski M, Wojtynska R and Rymaszewska J. Open Dialogue Approach An Alternative to
Neuroleptics or Development of Pharmacologically Cautious Treatment of Schizophrenia?. J Schizophr Res.
2015;2(2): 1013.
Kapciski M
Austin Publishing Group
teams together with phase specific treatment. However, these findings
should be confirmed in methodologically well-designed surveys
[16]. It seems important, though, to consider functional recovery
together with the patients social network [17]. Family members are
periled by the eruption of psychotic symptoms; therefore they seek
understanding of the situation. The medical narrative provides an
opportunity to better understand a suffering family member, try to
help him and understand the treatment. On the other hand, there is
social stigma associated with the term schizophrenia, with people
associating the condition with deterioration and chronicity. The
patient and his family members are put in an in-the-corner lifestyle
[18]. Creating an alternative narrative may be the ultimate goal of
psychotherapy aiming to re-authorize the patient and deal with the
disturbance associated with the dialogical self-concept [19,20]. The
above-listed ODA principles may assist in creating a secure setting,
particularly through polyphony and dialogism, where individuals
may work to support the patient [21]. McAdams accentuates the
integrative character of auto narration and its fundamental role in
giving sense of control over the patients boundary experience [22].
Handling a psychotic crisis and finding its meaning require quite
complex adaptation skills that patients usually lack. It seems of utmost
importance that staff support patient networks through gaining
competence to deal with severe mental illness. From the authors
point of view, the ODA therapeutic joint meeting may help all those
involved adapt to the new situation. This should translate into better
treatment outcomes [23,24]. Nonetheless, there is a need for longer
and more replicable trials that may assess prolonged treatment results
among people with diagnosed schizophrenia.
References
1. Aaltonen J, Seikkula J, Lehtinen K. The Comprehensive Open-Dialogue
Approach in Western Lapland: I. The incidence of non-affective psychosis
and prodromal states. Psychosis. 2011; 3: 179-191.
2. Alanen YO, Anttinen EE, Kokkola A, Lehtinen K, Ojanen M, Pylkkanen K,
et al. Treatment and rehabilitation of schizophrenic psychoses. The Finnish
treatment model. Nord J Psychiatry.1990; 44.
of the National Program for the Study, Treatment and Rehabilitation of
Schizophrenic Patients in Finland. Laakinto- hallituksenopassarja No. 4.
Helsinki: National Board of Health, Association of Mental Hospitals, League
of Hospitals in Finland. 1988.
7. Seikkula J, Alakare B, Aaltonen J. The Comprehensive Open-Dialogue
Approach in Western Lapland: II. Long-term stability of acute psychosis
outcomes in advanced community care. Psychosis. 2011: 3: 192-204.
8. SeikkulaJ, Aaltonen J, Alakare B, Haarakangas K, Keranen J, Lehtinen K.
Five-year experience of first-episode nonaffective psychosis in open-dialogue
approach: Treatment principles, follow-up outcomes, and two case studies.
Psychotherapy Research. 2006; 16: 214228.
9. Seikkula J, Alakare B, Aaltonen J, Holma J, Rasinkangas A, Lehtinen V.
Open dialogue approach: Treatment principles and preliminary results of
a two-year follow-up on first episode schizophrenia. Ethical Hum Sci Serv.
2003; 5: 163182.
10. Friis S, Larsen TK, Melle I. [Therapy of psychoses]. Tidsskr Nor Laegeforen.
2003; 123: 1393.
11. Bladzinski P, Cechcnicki A, Bogacz J, Cichocki L. The place of Open
Dialogue in the treatment of people suffering from schizophrenia. Advances
in Psychiatry and Neurology. 2014; 23: 134-139.
12. Lakeman R. The Finnish open dialogue approach to crisis intervention in
psychosis: A review. Psychother Aust. 2014; 3: 26-33.
13. Morrison AP, Hutton P, Shiers D, Turkington D. Antipsychotics: is it time to
introduce patient choice? Br J Psychiatry. 2012; 201: 83-84.
14. Lehtinen V, Aaltonen J, Koffert T, Rakkolainen V, Syvalahti E. Two-year
outcome in first-episode psychosis treated according to an integrated model.
Is immediate neuroleptisation always needed? Eur Psychiatry. 2000; 15: 312320.
15. Stratford A, Brophy L, Beaton T, Castle D. Recovery, medication and shared
responsibility in mental health care. Australas Psychiatry. 2013; 21: 550-553.
16. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database
Syst Rev. 2011.
17. Valencia M, Diaz A, Juarez F. Integration of Pharmacological and Psychosocial
Treatment for Schizophrenia in Mexico: The Case of a Developing Country
Proposal. Badria F, editor. In: Pharmacotherapy. InTech. 2012; 41-68.
18. White M. Family therapy and schizophrenia: Addressing the in-the-corner
life-style. Dulwich Centre Newsletter. 1987; 14-21.
3. Alanen Y. Towards a more humanistic psychiatry: Development of needadapted treatment of schizophrenia group psychoses. Psychosis. 2009; 1:
156166.
19. Lysaker PH, Lysaker JT. Schizophrenia and the collapse of the dialogical self:
Recovery, narrative and psychotherapy. Psychotherapy. 2001; 38: 252-261.
4. Aaltonen J, Koffert T, Ahonen J, Lehtinen V. Skitsofreniantarpeenmukainenhoito
on
ryhmatyota.
RaporttiAkuutinpsykoosinintegroituhoito
projektintuottamistahoitoperiaatteista. [The Need-Adapted treatment of
schizophreina is team work.] In Finnish with English summary. Stakes,
Raportteja, 257. Helsinki: Stakes. 2000.
21. Lorem GF. Making sense of stories: the use of patient narratives within
mental health care research. Nurs Philos. 2008; 9: 62-71.
5. Lehtinen V, Aaltonen J, Koffert T, Rakkolainen V, Syvalahti E, Vuorio K.
Integrated treatment model for first-contact patients with a schizophrenia-type
psychosis.The Finnish API project. Nord J Psychiatry. 1996; 50: 281287.
6. National
Board
of
Health.
Skitsofreniaprojekti
19811987.
Skitsofreniantutkimuksen,
hoidonjakuntoutuksenvaltakunnallisenkehittamisobjelmanloppuraportti.
[English summary: The Schizophrenia Project 19811987. Final report
J Schizophr Res - Volume 2 Issue 2 - 2015
Submit your Manuscript | www.austinpublishinggroup.com
Kapciski et al. All rights are reserved
Submit your Manuscript | www.austinpublishinggroup.com
20. White M. Deconstruction and therapy. Dulwich Centre Newsletter. 1991; 3:
21-40.
22. McAdams DP. Personality, modernity and the storied self: A contemporary
framework for studying persons. Psychological Inquiry. 1996; 7: 295-321.
23. Werbart A, Levander S. Understanding the incomprehensible: private theories
of first-episode psychotic patients and their therapists. Bull Menninger Clin.
2005; 69: 103-136.
24. Klapcinski M, Rymaszewska J. Open Dialogue Approach, about the
phenomenon of Scandinavian Psychiatry. Psychiatr Pol (accepted to print).
Citation: Kapciski M, Wojtynska R and Rymaszewska J. Open Dialogue Approach An Alternative to
Neuroleptics or Development of Pharmacologically Cautious Treatment of Schizophrenia?. J Schizophr Res.
2015;2(2): 1013.
J Schizophr Res 2(2): id1013 (2015) - Page - 02
You might also like
- Boom Esports Reveals The TeamDocument1 pageBoom Esports Reveals The TeamRanggaNo ratings yet
- VGJ - Storm Continues To Reign Supreme in Group B at The International 2018Document5 pagesVGJ - Storm Continues To Reign Supreme in Group B at The International 2018RanggaNo ratings yet
- SecretDocument7 pagesSecretRanggaNo ratings yet
- Cis Re Shuffle Pre-TiDocument5 pagesCis Re Shuffle Pre-TiRanggaNo ratings yet
- Na Rank Before Ti 8Document4 pagesNa Rank Before Ti 8RanggaNo ratings yet
- Another Spectacular Day For Evil Geniuses Remain at The Top of Group A at TI8 Day 2Document5 pagesAnother Spectacular Day For Evil Geniuses Remain at The Top of Group A at TI8 Day 2RanggaNo ratings yet
- Bots decimate Humans in exhibition match as OpenAI Five win series 2-1Document5 pagesBots decimate Humans in exhibition match as OpenAI Five win series 2-1RanggaNo ratings yet
- DAC 2018 Negative Effect Organization Dissipates: Posted by at 08 April 2018 09:45Document2 pagesDAC 2018 Negative Effect Organization Dissipates: Posted by at 08 April 2018 09:45RanggaNo ratings yet
- Wings Gaming Trample EG On Their Way To TI 6 Grand FinalsDocument2 pagesWings Gaming Trample EG On Their Way To TI 6 Grand FinalsRanggaNo ratings yet
- Fnatic Has Made The Choice To 'Temporarily' Remove Pieliedie From The Active Lineup, Replacing Him With Team Coach Adam For Starladder Invitational 5Document1 pageFnatic Has Made The Choice To 'Temporarily' Remove Pieliedie From The Active Lineup, Replacing Him With Team Coach Adam For Starladder Invitational 5RanggaNo ratings yet
- LGD Head To Their First Major Grand Finals at DAC 2018: View Image On TwitterDocument15 pagesLGD Head To Their First Major Grand Finals at DAC 2018: View Image On TwitterRanggaNo ratings yet
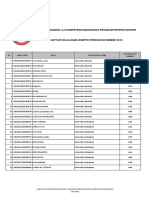
- PANITIA NASIONAL UJI KOMPETENSI MAHASISWA NOV 2016Document63 pagesPANITIA NASIONAL UJI KOMPETENSI MAHASISWA NOV 2016Aci Dwi LestariNo ratings yet
- PGL Open Bucharest - Minor Team Line-Up Has Been DecidedDocument2 pagesPGL Open Bucharest - Minor Team Line-Up Has Been DecidedRanggaNo ratings yet
- OpTic Gaming's path to TI8 after DACDocument4 pagesOpTic Gaming's path to TI8 after DACRanggaNo ratings yet
- Daftar Kelulusan UKMPPD Nov 2016 UPLOAD PDFDocument152 pagesDaftar Kelulusan UKMPPD Nov 2016 UPLOAD PDFRanggaNo ratings yet
- Roster Shuffle: Vega Picks Up FNG, Replaces Solo and NooneDocument1 pageRoster Shuffle: Vega Picks Up FNG, Replaces Solo and NooneRanggaNo ratings yet
- Daftar Kelulusan OSCE Nov 2016 UPLOAD PDFDocument74 pagesDaftar Kelulusan OSCE Nov 2016 UPLOAD PDFfelix_3264_hariantoNo ratings yet
- Wings Gaming Trample EG On Their Way To TI 6 Grand FinalsDocument2 pagesWings Gaming Trample EG On Their Way To TI 6 Grand FinalsRanggaNo ratings yet
- ReDeYe To Host EpicenterDocument1 pageReDeYe To Host EpicenterRanggaNo ratings yet
- DC defeats Fnatic, secures top 3 TI finishDocument3 pagesDC defeats Fnatic, secures top 3 TI finishRanggaNo ratings yet
- Wings Gaming Are The The International 6 Champions!: Game OneDocument3 pagesWings Gaming Are The The International 6 Champions!: Game OneRanggaNo ratings yet
- New BTS Series For SEA and AmericaDocument5 pagesNew BTS Series For SEA and AmericaRanggaNo ratings yet
- Team Empire Returns To ManilaDocument7 pagesTeam Empire Returns To ManilaRanggaNo ratings yet
- DC defeats Fnatic, secures top 3 TI finishDocument3 pagesDC defeats Fnatic, secures top 3 TI finishRanggaNo ratings yet
- DC Throne EG in Dramatic TI6 Lower Finals to Reach Grand FinalsDocument3 pagesDC Throne EG in Dramatic TI6 Lower Finals to Reach Grand FinalsRanggaNo ratings yet
- Newbee Secures Their Spot For Manila MajorDocument2 pagesNewbee Secures Their Spot For Manila MajorRanggaNo ratings yet
- Manila Major SEA Qualifiers - Mineski Are SEA RepresentativesDocument5 pagesManila Major SEA Qualifiers - Mineski Are SEA RepresentativesRanggaNo ratings yet
- Invitation Shanghai MajorDocument3 pagesInvitation Shanghai MajorRanggaNo ratings yet
- Digital Chaos Are The NA Qualifiers Winners For Manila MajorDocument3 pagesDigital Chaos Are The NA Qualifiers Winners For Manila MajorRanggaNo ratings yet
- Eg Invited To The Marstv Dota2 LeagueDocument2 pagesEg Invited To The Marstv Dota2 LeagueRanggaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- PHINMA University of Pangasinan College of Health Sciences Student Nurse Drug ReportDocument2 pagesPHINMA University of Pangasinan College of Health Sciences Student Nurse Drug ReportClaire Madriaga GidoNo ratings yet
- AFRIDarticle2020 Davis StoneDocument6 pagesAFRIDarticle2020 Davis Stonepico 24No ratings yet
- Antipsychotic Prescribing GuidelineDocument26 pagesAntipsychotic Prescribing GuidelineAshraf MullaNo ratings yet
- Asmal Et Al-2013-Cochrane Database of Systematic ReviewsDocument196 pagesAsmal Et Al-2013-Cochrane Database of Systematic ReviewsAngel ArmasNo ratings yet
- QuetiapineDocument3 pagesQuetiapineMichael KuzbytNo ratings yet
- Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment OptionsDocument21 pagesPharmacotherapy of Anxiety Disorders: Current and Emerging Treatment OptionsGabriel Vargas CuadrosNo ratings yet
- APA Draft Schizophrenia Treatment Guideline Dec2019 PDFDocument414 pagesAPA Draft Schizophrenia Treatment Guideline Dec2019 PDFFransiska Yuka JuliaNo ratings yet
- Tabela PDFDocument74 pagesTabela PDFAlexandre SabanyNo ratings yet
- GROUP F Compilation PsychiaFinalDocument20 pagesGROUP F Compilation PsychiaFinalFrancis Raphael PitogoNo ratings yet
- Mood Stabilisers: PsychopharmacologyDocument50 pagesMood Stabilisers: Psychopharmacologymeno321No ratings yet
- Schizoaffective DisordersDocument12 pagesSchizoaffective DisordersDayle Rj Canson Marquez100% (2)
- Fishman Aug 06Document5 pagesFishman Aug 06verghese17No ratings yet
- NCM 117 Psychiatric Nursing MODULE 7Document27 pagesNCM 117 Psychiatric Nursing MODULE 7Meryville JacildoNo ratings yet
- About Psychiatric Drugs Side-EffectsDocument60 pagesAbout Psychiatric Drugs Side-EffectsKarthikeyan Sudarsana BabuNo ratings yet
- Paranoid Schizophrenia Mayo ClinicDocument20 pagesParanoid Schizophrenia Mayo Cliniceinjehl160305No ratings yet
- All MCQs by DR - RoyalDocument19 pagesAll MCQs by DR - RoyalVaqasFarooqiNo ratings yet
- Poster-Proceedings 2016Document441 pagesPoster-Proceedings 2016Ana Rosa González BarrosoNo ratings yet
- Treatment of Psychological DisordersDocument32 pagesTreatment of Psychological Disordersfemfen1225100% (2)
- Trauma Rehabilitation Clinical Guideline: Brain InjuryDocument12 pagesTrauma Rehabilitation Clinical Guideline: Brain InjuryAhmad AliNo ratings yet
- Schizophrenia ReportDocument6 pagesSchizophrenia ReportAnna Reeka AmadorNo ratings yet
- Oman Nursing Student Case Report on Schizophrenia PatientDocument30 pagesOman Nursing Student Case Report on Schizophrenia PatientThe Legend2011100% (2)
- Clozapine Care GuideDocument16 pagesClozapine Care GuideERWIN SUMARDINo ratings yet
- Hesi Psych Study GuideDocument16 pagesHesi Psych Study GuideR100% (17)
- Reviewing Depot Injection Efficacy in The Treatment of SchizophreniaDocument10 pagesReviewing Depot Injection Efficacy in The Treatment of SchizophreniaAnonymous raLgWVyqNo ratings yet
- Soumya Mary 1 Year MSC (N)Document24 pagesSoumya Mary 1 Year MSC (N)Salman HabeebNo ratings yet
- BPD, DiagnosisDocument5 pagesBPD, DiagnosisMArkoNo ratings yet
- AMISULPRIDEDocument26 pagesAMISULPRIDERajmohan VNo ratings yet
- Psychiatry Uworld A4Document133 pagesPsychiatry Uworld A4farheennnahmedNo ratings yet
- PharmacologyDocument84 pagesPharmacologyhenrydycoco100% (1)
- Childhood Disorders & SchizophreniaDocument25 pagesChildhood Disorders & SchizophreniaMaJoy OrdoñezNo ratings yet