Professional Documents
Culture Documents
AHC in NEJM PDF
Uploaded by
iggybauOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AHC in NEJM PDF
Uploaded by
iggybauCopyright:
Available Formats
The
NEW ENGLA ND JOURNAL
of
MEDICINE
Perspective
Accountable Health Communities Addressing Social Needs
through Medicare and Medicaid
Dawn E. Alley, Ph.D., Chisara N. Asomugha, M.D., Patrick H. Conway, M.D., and Darshak M. Sanghavi, M.D.
or decades, experts have described a profound imbalance between public funding of acute medical
care and investments in upstream social and environmental determinants of health.1 By some estimates,
more than 95% of the trillion
dollars spent on health care in
the United States each year funds
direct medical services, even
though 60% of preventable deaths
are rooted in modifiable behaviors
and exposures that occur in the
community.1
Most clinicians are familiar
with the stories behind these
statistics: the child with asthma
whose substandard housing triggers repeated emergency department visits; the patient with repeated visits for severe abdominal
pain caused by her violent home
life; the older adult with diabe-
tes forced to choose between
paying for heat and buying groceries. But in our current system,
patients health-related social
needs frequently remain undetected and unaddressed. Despite
calls for obtaining an expanded
social history at the point of care,2
most health care systems lack the
infrastructure and incentives to
develop comprehensive, systematic screening-and-referral protocols
and relationships with the array
of community service providers
that would be required to address
their patients health-related social needs.
If the rate of preventable hospitalizations among residents of
low-income neighborhoods could
be reduced to the level among
residents of high-income neighborhoods, there would be 500,000
fewer hospitalizations per year.3
As health systems are increasingly
being held accountable for health
outcomes and reducing the cost
of care, they need tools and interventions that address patient and
community factors contributing to
excess utilization. Effective partnerships among medical care,
social services, public health, and
community-based organizations
could improve population health
outcomes, but developing sustainable payment models to support
such partnerships has proved
challenging.4
Some encouraging innovations
n engl j med nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on January 5, 2016. For personal use only. No other uses without permission.
Copyright 2016 Massachusetts Medical Society. All rights reserved.
PERS PE C T IV E
Accountable Health Communities
have emerged. Catalyzed in part
by statewide all-payer deliverysystem reform and the growth of
value-based or shared-risk payment models, some purchasers
and providers of medical care
have found innovative ways to
support high-value communityfocused interventions. For example, Hennepin Health, a countybased Medicaid managed-care
organization in Minnesota, has
reduced emergency department
visits by 9% by using housing
and community service specialists who are part of a tightly integrated medical and social service system. Tracking patients
service utilization across clinical
and human-service systems allows
Hennepin to target upstream interventions so that its patient care
can be more effective (as documented in composite quality metrics of asthma, diabetes, and vascular care); the organization has
improved patients access to social
services and reinvested savings
in a broad range of programs.5
Other examples come from the
Health Care Innovation Awards
granted by the Centers for Medicare and Medicaid Services (CMS);
these awards have supported organizations such Chicago-based
CommunityRx, which generates
prescriptions for community services through an interface linking the patients electronic health
record with a community-resource
database, and the Michigan Public Health Institute Pathways to
Better Health Community Hub
model, in which community health
workers perform a structured assessment of clients health and
social service needs and use
standardized pathways to link
beneficiaries to community resources and track outcomes.
These projects have generated
valuable insights regarding ad2
dressing the social determinants
of health, including the importance of establishing cross-sector
partnerships, building data systems that bridge health and community services, and developing
a workforce to deliver interventions to vulnerable populations.
We still lack expertise, however,
in the best ways of scaling these
approaches across myriad settings;
we remain unsure whether broadbased investments improve health
care utilization and costs; and
we need to develop and test a
template that allows a wide variety of communities to undertake
transformation efforts.
To accelerate the development
of a scalable delivery model for
addressing upstream determinants
of health for Medicare and Medicaid beneficiaries, CMS recently
announced a 5-year, $157 million
program to test a model called
Accountable Health Communities
(AHC). Funded under the auspices
of the CMS Innovation Center,
the test will assess whether systematically identifying and addressing health-related social
needs can reduce health care
costs and utilization among
community-dwelling Medicare and
Medicaid beneficiaries.
The foundation of the AHC
model is universal, comprehensive screening for health-related
social needs including but not
limited to housing needs (e.g.,
homelessness, poor housing quality, inability to pay mortgage or
rent), food insecurity, utility needs
(e.g., difficulty paying utility
bills), interpersonal safety (e.g.,
problems of intimate-partner violence, elder abuse, child maltreatment), and transportation difficulties in all Medicare and
Medicaid beneficiaries who obtain health care at participating
clinical sites. Using the data
gathered through this systematic
screening which form a socialneeds diagnostic snapshot of patients and their community
the AHC model aims to address
these underlying health-related
social needs through three tiers
of approaches, with each tier
linked to a payment method (see
table).
The models design recognizes
that communities needs and capacity vary widely, necessitating a
flexible, tracked approach keyed
to various levels of readiness for
change. The tracks which we
have named Awareness, Assistance, and Alignment were
developed on the basis of growing
evidence that linking high-cost
beneficiaries to social services can
improve health outcomes and reduce costs. Prospective participants in the test, termed bridge
organizations, can be community organizations, local health
departments, managed-care organizations, clinical networks, or
other organizations that can demonstrate that they have strong
relationships with clinical and
community partners.
The AHC model is the first
Innovation Center model designed
specifically to test building community capacity to address the
needs of a geographically defined
population of beneficiaries. Our
test will involve robust evaluation
methods (including randomization at the beneficiary level and
matched comparisons at the community level, which are exempt
from human-subjects review under
the Common Rule), is powered to
detect cost savings associated
with each track, and will have a
qualitative-evaluation component.
To be successful, the AHC
model will have to overcome several challenges that have plagued
earlier efforts to build and evalu-
n engl j med nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on January 5, 2016. For personal use only. No other uses without permission.
Copyright 2016 Massachusetts Medical Society. All rights reserved.
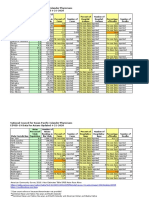
Startup funds ($250,000)
Payments for screening and referral of Medicare
and Medicaid beneficiaries at participating
clinical delivery sites ($2 per person per
year)
Randomization at the beneficiary level
Payment to bridge organi
zation (applicant)
Evaluation strategy
$1 million
$2.57 million
12
Randomization at the beneficiary level
Startup funds ($750,000)
Same payments for screening and referral as in Track 1
Payments for each high-risk beneficiary who elects to
receive community service navigation services
($86 per person per year)
State Medicaid agency; clinical delivery sites; community service providers
Track 3: Alignment
$4.51 million
20
Matched comparison group and matched comparison communities
Same startup funds, payments for screening,
referral, navigation as in Track 2
Annual lump-sum payments to support backbone
organization ($350,000 per year)
All in Track 2 plus backbone organization focused
on community-wide continuous quality-
improvement approach, including an advisory
board that ensures service provision, adequate
capacity to meet needs, and data sharing to
inform a gap analysis
State Medicaid agency; clinical delivery sites; community service providers; local government;
local payers (MA Plans and Medicaid MCOs)
Will a combination of community service navigation (at the individual beneficiary level) and
partner alignment at the community level reduce total cost of care, ED visits, and admissions?
Screening, referral, community service navigation,
plus partner alignment
* Tracks are mutually exclusive; communities will be selected to participate in a single track. ED denotes emergency department, MA Medicare Advantage, and MCO managed-care
organization.
Total funds per awardee
12
Inventory of local community services
All in Track 1 plus intensive community service navi
Universal screening of all Medicare and
gation (in-depth assessment and follow-up until
Medicaid beneficiaries by medical provider
needs are resolved or unresolvable)
Referral to community services with beneficiary
responsible for completing referral
Intervention components
No. of award sites
State Medicaid agency; clinical delivery sites;
community service providers
Required partners
Will providing community service navigation to assist
beneficiaries with overcoming barriers to access to
services reduce total cost of care, ED visits, and
admissions?
Will increasing awareness of community service availability through information dissemination and referral reduce total cost
of care, ED visits, and admissions?
Track 2: Assistance
Screening, referral, plus community service navigation
Question being tested
Track 1: Awareness
Screening and referral only
Intervention
Variable
Key Features of the Accountable Health Community 5-Year Payment-Model Test.*
PE R S PE C T IV E
Accountable Health Communities
ate clinicalcommunity collaborations. First, major gaps exist in
the evidence base needed to inform the selection of screening
items and the collection of data
for detecting health-related social
needs, as highlighted by a recent
report from the Institute of Medicine.2 AHC sites will be required
to select items from a question
bank prepared by CMS in consultation with experts after extensive
review of existing screening items;
however, ensuring that these
questions are reliable for various
delivery modes and patient populations will be a key challenge.
Maintaining a motivated and
skilled stable of community navigators will also be challenging.
Second, community needs and
the quality of resources vary significantly, resulting in a challenging degree of complexity for
a national test. Thats why the
AHC project includes three incremental levels of integration of
care delivery, which can be deployed in multiple settings. The
model permits flexibility in each
track and incorporates extensive
local support and technical assistance to help sites integrate interventions into their workflows.
For example, in addition to the
standard list of social needs that
all participants will try to address, bridge organizations can,
on the basis of community needs
assessment, select additional
needs to target. Sites can also
choose how an intervention is
delivered by mobile device, in
person at clinical sites, or
through home visits depending on the setting (for instance,
whether it is rural or urban). In
the advanced track (Alignment),
CMS will fund a backbone organization that will facilitate data
collection and sharing among all
partners and try to enhance ser-
n engl j med nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on January 5, 2016. For personal use only. No other uses without permission.
Copyright 2016 Massachusetts Medical Society. All rights reserved.
PERS PE C T IV E
Accountable Health Communities
vice capacity, testing the scalability and effectiveness of this backbone structure.
The AHC model reflects a
growing emphasis on population
health in CMS payment policy,
which aims to support a transition from a health care delivery
system to a true health system.
The AHC test will improve our
understanding of whether savings
can materialize when upstream
factors are addressed through
collaboration among stakehold-
ers who are accountable for the
health and health care of their
community.
Disclosure forms provided by the authors
are available with the full text of this article
at NEJM.org.
From the Centers for Medicare and Medicaid
Services, Baltimore.
This article was published on January 5,
2016, at NEJM.org.
1. McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff
(Millwood) 2002;21:78-93.
2. Adler NE, Stead WW. Patients in context
EHR capture of social and behavioral determinants of health. N Engl J Med 2015;372:
698-701.
3. Potentially preventable hospitalizations
United States, 20012009. MMWR Surveill Summ 2013;62:Suppl 3:139-43.
4. Eggleston EM, Finkelstein JA. Finding the
role of health care in population health.
JAMA 2014;311:797-8.
5. Sandberg SF, Erikson C, Owen R, et al.
Hennepin Health: a safety-net accountable
care organization for the expanded Medicaid
population. Health Aff (Millwood) 2014;33:
1975-84.
DOI: 10.1056/NEJMp1512532
Copyright 2016 Massachusetts Medical Society.
n engl j med nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on January 5, 2016. For personal use only. No other uses without permission.
Copyright 2016 Massachusetts Medical Society. All rights reserved.
You might also like
- The Scope and Impact of Mobile HealthDocument12 pagesThe Scope and Impact of Mobile Healthdrestadyumna ChilspiderNo ratings yet
- 1421 McCarthy Triple Aim Overview v2Document12 pages1421 McCarthy Triple Aim Overview v2Ahmed BabaNo ratings yet
- Regional Health Improvement Collaboratives: Overcoming Barriers to Healthcare ReformDocument25 pagesRegional Health Improvement Collaboratives: Overcoming Barriers to Healthcare ReformTimothy Suraj0% (1)
- HealthPartners Case Study: Consumer-Focused Mission and Collaborative ApproachDocument32 pagesHealthPartners Case Study: Consumer-Focused Mission and Collaborative ApproachJyotiGhanchiNo ratings yet
- NACHC 2022 Workforce Survey Full Report 1Document8 pagesNACHC 2022 Workforce Survey Full Report 1Bai Monisa GampongNo ratings yet
- Draft Proposal - Measuring HospitalsDocument24 pagesDraft Proposal - Measuring HospitalsAli H. MhmdNo ratings yet
- News & Notes: Psychiatric Services 66:7, July 2015Document2 pagesNews & Notes: Psychiatric Services 66:7, July 2015Re LzNo ratings yet
- Ramos, Sioco Chapter 25 and 26Document59 pagesRamos, Sioco Chapter 25 and 26DOROTHY ANN SOMBILUNANo ratings yet
- Arnold Ventures Finance Committee Behavioral Health LetterDocument4 pagesArnold Ventures Finance Committee Behavioral Health LetterArnold VenturesNo ratings yet
- Reducing Racial and Ethnic Disparities in Health Care QualityDocument21 pagesReducing Racial and Ethnic Disparities in Health Care QualityIveeh GuillartesNo ratings yet
- High Value Health CareDocument17 pagesHigh Value Health CareSugaintheran MuniandyNo ratings yet
- Health Affairs: For Reprints, Links & Permissions: E-Mail Alerts: To SubscribeDocument11 pagesHealth Affairs: For Reprints, Links & Permissions: E-Mail Alerts: To SubscribeAnnaNo ratings yet
- Module 4 2Document4 pagesModule 4 2api-642701476No ratings yet
- Hsci 6250Document4 pagesHsci 6250api-642711495No ratings yet
- New Technologies Related To Public Health Electronic InformationDocument5 pagesNew Technologies Related To Public Health Electronic InformationRose Lyn Camarista VelascoNo ratings yet
- Health at National and Intl LevelDocument6 pagesHealth at National and Intl Levelshruti singhNo ratings yet
- 2019 LeapfrogToValue PDFDocument57 pages2019 LeapfrogToValue PDFJamey DAVIDSONNo ratings yet
- Discussion 2 - Nursing PerspectivesDocument2 pagesDiscussion 2 - Nursing PerspectivesGabrelle AbalosNo ratings yet
- Adopting Value-Based Care for Universal HealthDocument57 pagesAdopting Value-Based Care for Universal HealthMoss MbuguaNo ratings yet
- Health Affairs: For Reprints, Links & Permissions: E-Mail Alerts: To SubscribeDocument11 pagesHealth Affairs: For Reprints, Links & Permissions: E-Mail Alerts: To Subscribeapi-82483386No ratings yet
- Business Case Study - CompetitionDocument5 pagesBusiness Case Study - CompetitionDarshanShahNo ratings yet
- RWJF Issue BriefDocument4 pagesRWJF Issue BriefiggybauNo ratings yet
- Principles To Guide Health Care TransformationDocument10 pagesPrinciples To Guide Health Care TransformationGFBMGFBLKNGMDSBGFNFHNFHNMHDNo ratings yet
- Warren Lucban Mod4Document3 pagesWarren Lucban Mod4Warren LucbanNo ratings yet
- Hospital FinanceDocument54 pagesHospital FinancePadmanabha Narayan100% (3)
- Milq 054Document28 pagesMilq 054Bassam AlqadasiNo ratings yet
- Community Nursing and Care Continuity LEARNING OUTCOMES After CompletingDocument23 pagesCommunity Nursing and Care Continuity LEARNING OUTCOMES After Completingtwy113100% (1)
- HIS VidDocument8 pagesHIS VidJacqueline HarleNo ratings yet
- Urban-Rural Difference in Satisfaction With Primary Healthcare Services in GhanaDocument9 pagesUrban-Rural Difference in Satisfaction With Primary Healthcare Services in GhanaAyensuaNo ratings yet
- Promoting Competition in Healthcare MarketsDocument40 pagesPromoting Competition in Healthcare Marketspadmanaban manickavelanNo ratings yet
- Reinventing Rural Health Care: A Case Study of Seven Upper Midwest StatesDocument44 pagesReinventing Rural Health Care: A Case Study of Seven Upper Midwest StatesLyndaWaddingtonNo ratings yet
- EpisodeBasedPayment PerspectivesforConsiderationDocument24 pagesEpisodeBasedPayment PerspectivesforConsiderationHazelnutNo ratings yet
- Analysis of Health Care System Initiatives in MA and SF, CA (Function, Cost, Outcome)Document7 pagesAnalysis of Health Care System Initiatives in MA and SF, CA (Function, Cost, Outcome)Wonder LostNo ratings yet
- AHA Patient Centered Medical HomeDocument21 pagesAHA Patient Centered Medical Homein678No ratings yet
- Social Factors Influencing Individual and Population Health - EditedDocument6 pagesSocial Factors Influencing Individual and Population Health - EditedOkoth OluochNo ratings yet
- NRES Thesis - Chapter 1 3Y3-7Document16 pagesNRES Thesis - Chapter 1 3Y3-7acorpuz_4No ratings yet
- Futurescan 2021–2026: Health Care Trends and ImplicationsFrom EverandFuturescan 2021–2026: Health Care Trends and ImplicationsNo ratings yet
- Are Incentives Everything? Payment Mechanisms For Health Care Providers in Developing CountriesDocument21 pagesAre Incentives Everything? Payment Mechanisms For Health Care Providers in Developing CountriesCristhian LarrahondoNo ratings yet
- Jurnal Canada 2Document9 pagesJurnal Canada 2Ikaputri fNo ratings yet
- Turning The Vision of Connected Health Into A RealityDocument14 pagesTurning The Vision of Connected Health Into A RealityCognizant100% (2)
- Cross Roads in Quality 2008Hlth AffairsDocument11 pagesCross Roads in Quality 2008Hlth AffairsVaida BankauskaiteNo ratings yet
- Healthcast The Customisation of Diagnosis Care and Cure-Pwc-2010 PDFDocument58 pagesHealthcast The Customisation of Diagnosis Care and Cure-Pwc-2010 PDFEhli HibreNo ratings yet
- Community HealthDocument4 pagesCommunity HealthJennifer SamsonNo ratings yet
- Policy at The Intersection of Health, Health Care andDocument21 pagesPolicy at The Intersection of Health, Health Care andIsmaNo ratings yet
- Healthcare Inc. A Better Business ModelDocument13 pagesHealthcare Inc. A Better Business ModelrangababNo ratings yet
- Health Policy Brief: Accountable Care OrganizationsDocument6 pagesHealth Policy Brief: Accountable Care Organizationspalak32No ratings yet
- Community As ClientDocument13 pagesCommunity As ClientVirus50% (2)
- Community Based Mental HealthcareDocument4 pagesCommunity Based Mental HealthcarerhiachiNo ratings yet
- Social and Behavior Change and Health System StrengtheningDocument10 pagesSocial and Behavior Change and Health System StrengtheninggilbertoNo ratings yet
- Singer, Judy Qualitative Evaluation of A Community NavajoDocument15 pagesSinger, Judy Qualitative Evaluation of A Community NavajoLuis R HdezNo ratings yet
- Minnesota Hospital Association's Lown Institute ResponseDocument3 pagesMinnesota Hospital Association's Lown Institute ResponseinforumdocsNo ratings yet
- Social Franchising HHPRDocument14 pagesSocial Franchising HHPRZak1717No ratings yet
- Behavioral Health: The Gap in California's Dual Eligible DemonstrationDocument34 pagesBehavioral Health: The Gap in California's Dual Eligible Demonstrationapi-79044486No ratings yet
- 2015 Health Care Providers Outlook: United StatesDocument5 pages2015 Health Care Providers Outlook: United StatesEmma Hinchliffe100% (1)
- Final MCO Working Group ReportDocument77 pagesFinal MCO Working Group ReportShira SchoenbergNo ratings yet
- Questions & Answers - Updated April 12, 2011Document5 pagesQuestions & Answers - Updated April 12, 2011Denilson Oliveira MeloNo ratings yet
- Demand in Health Care AnalysisDocument9 pagesDemand in Health Care AnalysisZewdu MinwuyeletNo ratings yet
- Organizing US Healthcare DeliveryDocument20 pagesOrganizing US Healthcare DeliveryJeffersonNo ratings yet
- Health Care Equity Tool Kit for Developing Winning PolicyDocument25 pagesHealth Care Equity Tool Kit for Developing Winning PolicyDenden Alicias100% (1)
- Hospitals and Community Benefit: New Demands, New ApproachesFrom EverandHospitals and Community Benefit: New Demands, New ApproachesNo ratings yet
- Bostock v. Clayton County, Georgia DecisionDocument119 pagesBostock v. Clayton County, Georgia DecisionNational Content DeskNo ratings yet
- AAFP Letter To Domestic Policy Council 6-10-2020Document3 pagesAAFP Letter To Domestic Policy Council 6-10-2020iggybauNo ratings yet
- Boston Mayor Executive Order 6-12-2020Document3 pagesBoston Mayor Executive Order 6-12-2020iggybauNo ratings yet
- HR 6585 Equitable Data Collection COVID-19Document18 pagesHR 6585 Equitable Data Collection COVID-19iggybauNo ratings yet
- NCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020Document23 pagesNCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020iggybauNo ratings yet
- HR 4004 Social Determinants Accelerator ActDocument18 pagesHR 4004 Social Determinants Accelerator ActiggybauNo ratings yet
- S 3609 Coronavirus Immigrant Families Protection ActDocument17 pagesS 3609 Coronavirus Immigrant Families Protection ActiggybauNo ratings yet
- HR 6763 COVID-19 Racial and Ethnic Disparities Task ForceDocument11 pagesHR 6763 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNo ratings yet
- HR 6437 Coronavirus Immigrant Families Protection AcfDocument16 pagesHR 6437 Coronavirus Immigrant Families Protection AcfiggybauNo ratings yet
- A Bill: in The House of RepresentativesDocument2 pagesA Bill: in The House of RepresentativesiggybauNo ratings yet
- S 3721 COVID-19 Racial and Ethnic Disparities Task ForceDocument11 pagesS 3721 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNo ratings yet
- 7th Circuit Affirming Preliminary Injunction Cook County v. WolfDocument82 pages7th Circuit Affirming Preliminary Injunction Cook County v. WolfiggybauNo ratings yet
- COVID-19 Data For Native Hawaiians and Pacific Islanders UPDATED 4-21-2020 PDFDocument2 pagesCOVID-19 Data For Native Hawaiians and Pacific Islanders UPDATED 4-21-2020 PDFiggybauNo ratings yet
- Doe v. Trump 9th Circuit Denial of Stay of Preliminary InjunctionDocument97 pagesDoe v. Trump 9th Circuit Denial of Stay of Preliminary InjunctioniggybauNo ratings yet
- Milwaukee Board of Supervisors Ordinance 20-174Document9 pagesMilwaukee Board of Supervisors Ordinance 20-174iggybauNo ratings yet
- Physician Association Letter To HHS On Race Ethnicity Language Data and COVID-19Document2 pagesPhysician Association Letter To HHS On Race Ethnicity Language Data and COVID-19iggybauNo ratings yet
- Cook County v. Wolf Denial Motion To Dismiss Equal ProtectionDocument30 pagesCook County v. Wolf Denial Motion To Dismiss Equal ProtectioniggybauNo ratings yet
- COVID 19 FaceCovering 1080x1080 4 SPDocument1 pageCOVID 19 FaceCovering 1080x1080 4 SPiggybauNo ratings yet
- Tri-Caucus Letter To CDC and HHS On Racial and Ethnic DataDocument3 pagesTri-Caucus Letter To CDC and HHS On Racial and Ethnic DataiggybauNo ratings yet
- Doe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationDocument9 pagesDoe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationiggybauNo ratings yet
- Covid-19 Data For Asians Updated 4-21-2020Document2 pagesCovid-19 Data For Asians Updated 4-21-2020iggybauNo ratings yet
- SF StayHome MultiLang Poster 8.5x11 032620Document1 pageSF StayHome MultiLang Poster 8.5x11 032620iggybauNo ratings yet
- Doe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceDocument48 pagesDoe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceiggybauNo ratings yet
- CDC Covid-19 Report FormDocument2 pagesCDC Covid-19 Report FormiggybauNo ratings yet
- WA v. DHS Order On Motion To CompelDocument21 pagesWA v. DHS Order On Motion To CompeliggybauNo ratings yet
- MMMR Covid-19 4-8-2020Document7 pagesMMMR Covid-19 4-8-2020iggybauNo ratings yet
- ND California Order On Motion To CompelDocument31 pagesND California Order On Motion To CompeliggybauNo ratings yet
- Democratic Presidential Candidate Positions On ImmigrationDocument10 pagesDemocratic Presidential Candidate Positions On ImmigrationiggybauNo ratings yet
- Booker-Harris-Warren Letter To HHS Re Racial Disparities in COVID ResponseDocument4 pagesBooker-Harris-Warren Letter To HHS Re Racial Disparities in COVID ResponseStephen LoiaconiNo ratings yet
- Pete Buttigieg Douglass PlanDocument18 pagesPete Buttigieg Douglass PlaniggybauNo ratings yet
- A Review-Formulation of Mouth Dissolving Tablet: International Journal of Pharmaceutical and Clinical ScienceDocument8 pagesA Review-Formulation of Mouth Dissolving Tablet: International Journal of Pharmaceutical and Clinical ScienceSiti Hajar HasyimNo ratings yet
- 2016 8 30 EpiPen LetterDocument8 pages2016 8 30 EpiPen LetterTim TiemannNo ratings yet
- Australian Children Study Sample DesignDocument30 pagesAustralian Children Study Sample Designamri doangNo ratings yet
- Teresa Walters - RN ResumeDocument3 pagesTeresa Walters - RN Resumeapi-581399200No ratings yet
- Individual InsuranceDocument8 pagesIndividual InsuranceBrian AhierNo ratings yet
- Quality Improvement Manager in Northwest Indiana Resume Nancy WulffDocument2 pagesQuality Improvement Manager in Northwest Indiana Resume Nancy WulffNancy WulffNo ratings yet
- AJRR 2016 Annual Report FinalDocument48 pagesAJRR 2016 Annual Report FinalMônica RufinoNo ratings yet
- Medical Coding Fundamentals Study GuideDocument62 pagesMedical Coding Fundamentals Study GuideAaron WallaceNo ratings yet
- AU Tax Refund AmendmentDocument16 pagesAU Tax Refund Amendmentleslie woodsNo ratings yet
- Acs Surgery 2006Document2,184 pagesAcs Surgery 2006allenNo ratings yet
- Trauma Center Feasibility StudyDocument25 pagesTrauma Center Feasibility StudyOakLawnLeaf100% (1)
- Time in The Out Patient Department in Hospital Mba ReportDocument83 pagesTime in The Out Patient Department in Hospital Mba ReportAshutoshSharma100% (1)
- May 3, 2012 - The Federal Crimes Watch DailyDocument13 pagesMay 3, 2012 - The Federal Crimes Watch DailyDouglas McNabbNo ratings yet
- Eysenck Personality QuestionnaireDocument6 pagesEysenck Personality QuestionnaireCimpoies Dragos100% (10)
- Counterfeit Drugs: A Global Threat to Public HealthDocument36 pagesCounterfeit Drugs: A Global Threat to Public Healthreadbooks86100% (1)
- WA Health Fees and Charges ManualDocument136 pagesWA Health Fees and Charges ManualFuadNo ratings yet
- Cream Healthcare Medical Presentation PDFDocument25 pagesCream Healthcare Medical Presentation PDFSusuNo ratings yet
- The Emergency ServicesDocument14 pagesThe Emergency ServicesFUMC ANTIPOLO ER DEPTNo ratings yet
- Compendium 8th EditionDocument251 pagesCompendium 8th EditiondfgNo ratings yet
- Amta 2019 Student Fact Sheet VFDocument2 pagesAmta 2019 Student Fact Sheet VFkingRamos MinistriesNo ratings yet
- Welcome To The 13 Annual Alliance For Aging Golf TournamentDocument48 pagesWelcome To The 13 Annual Alliance For Aging Golf TournamentJoon MoonNo ratings yet
- EHR ImplementationDocument12 pagesEHR Implementations_bouchey100% (2)
- Febmar 08 TCRDocument8 pagesFebmar 08 TCRapi-291864927No ratings yet
- 2019 Annual ReportDocument15 pages2019 Annual ReportLegal CouncilNo ratings yet
- Recovery Help Washington - Resource GuideDocument4 pagesRecovery Help Washington - Resource GuideKING 5 NewsNo ratings yet
- Intradermal Meds ChecklistDocument2 pagesIntradermal Meds ChecklistMonika Sarmiento100% (1)
- Annotated Bibliography 5 SourcesDocument6 pagesAnnotated Bibliography 5 Sourcesapi-355703318No ratings yet
- McKesson Quality EMeasures For ParagonDocument2 pagesMcKesson Quality EMeasures For ParagonrhvenkatNo ratings yet
- An Overview of Standard Operating Procedures (SOPs)Document22 pagesAn Overview of Standard Operating Procedures (SOPs)Urlam Kumar71% (7)
- CM Dr. Kalaignar Insurance SchemeDocument12 pagesCM Dr. Kalaignar Insurance SchemeMeenakshi KhuranaNo ratings yet